Abstract
Study design
Prospective cohort study.
Objectives
To investigate changes in body composition parameters in people with recent spinal cord injury (SCI) during their first inpatient rehabilitation and up to 1 year after discharge and whether those potential changes over time varied between different personal and lesion characteristics groups.
Setting
Rehabilitation center, the Netherlands.
Methods
People with recent SCI (≥18 years; n = 53) were tested around admission (T0) and discharge (T1) of inpatient rehabilitation. A sub-group (n = 19) was measured 1 year after discharge (T2). Personal and lesion characteristics were registered at T0. Anthropometry (height, body mass, body mass index, and waist circumference) was performed at T0, T1, and T2. Bioelectrical impedance analysis (BIA) was measured at T0 and T1.
Results
During inpatient rehabilitation, no significant changes in all body composition parameters were found. During the first year after discharge, body mass index (26.8 kg/m2) significantly increased compared with the level at both admission (25.4 kg/m2; p = 0.01, 95% CI: 0.32–2.52) and discharge (25.1 kg/m2; p = 0.02, 95% CI: 0.26–3.00). People with paraplegia showed an increase in absolute waist circumference (6.5%) compared with people with tetraplegia who showed a net decrease (−5.5%) in the year after discharge (p = 0.047, 95% CI: 0.27–33.62).
Conclusions
A stable body composition during inpatient rehabilitation is followed by an increased BMI in the year after discharge in people with recent SCI. People with paraplegia showed an increase in absolute waist circumference compared with people with tetraplegia who showed a net decrease in the year after discharge.
Similar content being viewed by others
Introduction
Obesity is a common secondary complication in people with spinal cord injury (SCI), predominantly caused by paralyzed muscle atrophy and physical inactivity [1, 2]. These physiological and lifestyle alterations lead to changes in body composition such as an increase in fat mass (FM) and a decrease in lean body mass (LBM), resulting in a significant reduction in total daily energy expenditure and resting energy expenditure [3]. These unfavorable changes combined with the unchanged dietary habits lead to weight gain as time progresses and increase the risk of many obesity-related health problems such as insulin resistance [4], hyperlipidemia [5], cardiovascular diseases [6], and upper-extremity overuse injuries [7]. Previous studies have reported that people with SCI showed up to 12% higher FM% and 14–27% lower resting energy expenditure than able-bodied controls [2, 8]. Crane et al. [9] demonstrated that persons with recent SCI were at the highest risk of weight gain during the first year following rehabilitation. De Groot et al. [10] showed that the percentage of persons with SCI with overweight or obese (body mass index (BMI) ≥ 22 or 25 kg/m2, respectively) increased from 56 to 75% in the first 5 years after injury, with the largest increase in BMI during the first year after discharge. Furthermore, De Groot et al. [10] suggested that based on BMI values, men, persons with paraplegia and older people had more chance of being overweight or obese compared with women, persons with tetraplegia and younger people. Gupta et al. [11] also found that the prevalence of overweight and/or obese (BMI ≥ 25 kg/m2) was higher in people with paraplegia than in those with tetraplegia.
There are several methods to monitor changes in body composition such as measuring BMI and waist circumference (WC), or estimating body composition using bioelectrical impedance analysis (BIA) or dual-energy X-ray absorptiometry (DXA). For clinical purposes, measuring BMI, WC, and BIA is more feasible compared to DXA due to financial and logistical restrictions [12]. Most studies have focused on BMI, WC, FM%, and LBM% in people with SCI after rehabilitation [10, 13,14,15,16,17,18], while only a few studies have investigated body composition during rehabilitation by BIA or DXA [19, 20]. Felleiter et al. [19] found that FM% measured by BIA decreased significantly in the acute phase, but leveled off in the subacute phase during inpatient rehabilitation, suggesting an influence of length of stay during rehabilitation. However, they excluded obese individuals and relatively few (33%) people with tetraplegia were included, which might partly cause the considerably lower FM% (19.9%) of their participants compared to other studies in people with chronic SCI (28–38%) [2, 21]. Singh et al. [20] reported a marked decrease in LBM with an increase in adiposity in a relatively young (mean: 33.3 years, range: 19–60 years) group of people with recent SCI (n = 95) during the first year of SCI using DXA, but unfortunately no follow-up measurements after discharge were performed. Hence, there is a need for body composition data from a more heterogeneous and representative group of people with SCI during and after inpatient rehabilitation. Therefore, in the present study, every patient admitted for the first time to the rehabilitation center was monitored for body composition as a part of regular care. The aim was to investigate changes in body composition, using BMI, WC and BIA outcomes, in people with recent SCI during the first inpatient rehabilitation and up to 1 year after discharge. Furthermore, we investigated whether the alterations in body composition parameters over time varied between different personal characteristics (age and sex) and lesion characteristics (lesion level and motor completeness) groups. Based on previous studies [2, 10, 22], our hypotheses were [1] that people with recent SCI would show a stable body composition during inpatient rehabilitation and a BMI or WC increase during the first year after discharge [2]; that changes in body composition parameters would be affected by personal and lesion characteristics with, men, older people, persons with paraplegia, showing a more increased adiposity than women, younger people, persons with tetraplegia.
Methods
Participants
This study was a part of the AMSterdam Spinal Cord Injury cohort study, which aims to evaluate the treatment on an individual and group level and to study potential outcome determinants. All adults (≥18 years) with recent SCI classified as AIS A-D were eligible to enter the study when admitted for the first inpatient rehabilitation at Reade, center for rehabilitation and rheumatology in Amsterdam, the Netherlands. Exclusion criteria were: (1) SCI due to metastatic cancer with a diminished life expectancy (<1 year), (2) acute severe psychiatric problems, (3) not able to communicate in Dutch or English.
Fifty-three people (25 females) with recent SCI were included. The mean age of the participants was 54.4 (15.7) years and the median time since injury at the admission of inpatient rehabilitation was 23 (17–33) days. Forty-seven percent of the participants had a tetraplegia (tetraplegia: 25 persons; paraplegia: 28 persons) and 25% had a motor complete injury (motor complete injury: 13 persons; motor incomplete injury: 40 persons) (Table 1). This study was approved by the Medical Ethical Committee of Slotervaart Hospital and Reade rehabilitation center. All participants signed an informed consent form before the first test occasion.
Design
Data were collected using standardized procedures within 2 weeks after admission of inpatient rehabilitation (T0), within 2 weeks before discharge (T1) and 1 year after discharge (T2) by trained human movement scientists and physical therapists. Since it was not possible to perform BIA measurements at T2 similarly to T0 and T1, i.e., early morning in bed after an overnight fast, anthropometric measurements were only performed at T2 without an overnight fast on a sub-group of 19 persons. This sub-group was created based on the number of participants that could be measured at T2.
Personal and lesion characteristics
With the median age of 57, younger (≤57 years) and older (>57 years) age groups were defined. Lesion characteristics (level and completeness) were determined by a physiatrist using the AIS criteria [23]. Motor complete (AIS A or B) and motor incomplete injury (AIS C or D) groups were defined while lesion level groups were defined by tetraplegia (lesion ≥T1) and paraplegia (<T1).
Anthropometry
At T0, self-reported height was obtained. Body mass was measured using a wheelchair accessible weighing scale (Henk Maas Scales IND-II, AllScales Europe, Veen, the Netherlands) at T0, T1, and T2. BMI was calculated (body mass (kg)/height (m2)). WC was measured twice (and averaged) after a normal expiration and in supine position with a tension-gated tape measure at the umbilicus level at T0, T1, and T2. A tension-gated tape measure was used to ensure equivalent tape pressure between participants. The adjusted cut-off points of BMI (recommended: BMI < 22 kg/m2; overweight: 22≤BMI < 25 kg/m2; obese: BMI ≥ 25 kg/m2) and WC (recommended: WC < 94 cm; adverse cardiovascular disease (CVD) risk: WC ≥ 94 cm) for people with SCI were used to check the prevalence of overweight/obese individuals and adverse CVD risk at T0, T1 and T2 [17, 24].
Bio-impedance analysis
BIA measurements were scheduled early morning at T0 and T1 when the participants were still in bed after an overnight fast. Caffeine, alcohol intake, and physical exercise were not allowed within 8 h of the measurement. FM% and LBM% were obtained by using a BIA device (Bodystat® 1500MDD, Bodystat Inc, Douglas, UK) with participants’ arms and legs slightly apart. To minimize fluctuations in body fluid distribution, participants were instructed to rest in a supine position for at least 10 min before the measurement started. BIA measurements were performed according to the standard operating procedures from the device’s instruction manual.
Statistical analysis
Data were tested for a normal distribution using QQ-plots, the Kolmogorov–Smirnov test, and the Shapiro–Wilk test and all data were normally distributed. A Chi-squared test was used to determine the differences in prevalence of overweight/obese individuals and adverse CVD risk among all test occasions. Pearson’s correlations identified the relationships between changes in body composition parameters and length of stay between T0 and T1. A paired t-test was used to determine potential differences between T0 and T1 (total group) in BMI, WC, FM%, and LBM%. Repeated measures analysis of variance was used to test the changes in body composition among T0, T1, and T2 in the sub-group and whether changes in body composition parameters between T0 and T1 (total group) as well as T1 and T2 (sub-group) varied between different personal and lesion characteristics groups (interaction effect: group × time). All statistical analyses were performed using SPSS software (version 25, IBM, Somers, NY, USA). A p-value < 0.05 was considered significant. Data are presented as mean (SD).
Results
Table 1 shows the baseline (T0) characteristics of the total group (n = 53) and sub-group (n = 19). At T0, the prevalence of overweight/obese individuals was 78% while the prevalence of adverse CVD risk was 51%. When using BMI and WC cut-off points, no significant changes were found in prevalence between T0, T1 and among T0, T1, T2 (Fig. 1). Also, no significant changes over time were found in prevalence between the different personal and lesion characteristics groups.
Percentage of participants in the three BMI groups between a T0 and T1 (n = 53) and b T0, T1, and T2 (n = 19) and percentage of participants in the two WC groups between c T0 and T1 (n = 53) and d T0, T1 and T2 (n = 19) according to adjusted cut-off points of BMI and WC for people with SCI. BMI body mass index, WC waist circumference, CVD cardiovascular disease.
Figure 2 illustrates the individual changes in BMI, WC, FM%, and LBM% in the groups of tetraplegia and paraplegia. No significant changes in BMI, WC, FM%, and LBM% or interaction effects (group × time) during inpatient rehabilitation were found (Table 2).
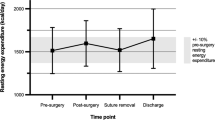
Figure 3a shows that BMI increased significantly in the sub-group during the first year after discharge (26.8 kg/m2) compared with the level at both admission (25.4 kg/m2; p = 0.01, 95% CI: 0.32–2.52) and discharge (25.1 kg/m2; p = 0.02, 95% CI: 0.26–3.00). In contrast, no significant change was found in WC during the first year after discharge, but an interaction effect indicated that people with paraplegia (6.5%) showed a significantly larger increase in absolute WC than people with tetraplegia who showed a net decrease (−5.5%; p = 0.047, 95% CI: 0.27–33.62; (Fig. 3b)). Table 3 shows the changes in BMI and WC among T0, T1, and T2 in the sub-group.
Changes in a BMI and changes in b WC in the whole group and in different age (Age ≤ 57, Age > 57), lesion level (Tetraplegia, Paraplegia) groups from T0 to T2. BMI body mass index, WC waist circumference. Error bars in a, b belong to the whole group. a *Significant change in BMI between T0 and T2, p < 0.05 **Significant change in BMI between T1 and T2, p < 0.05. b *Significant difference in WC between age groups, p < 0.05 **Significant interaction effect in WC between lesion level groups during T1 and T2, p < 0.05.
Discussion
During inpatient rehabilitation
According to the BMI and WC cut-off points, the percentage of overweight/obese individuals and those who were at risk of CVD did not show a significant change during inpatient rehabilitation, which was also found in a previous Dutch study [10]. This quite stable BMI during inpatient rehabilitation might be explained by a more active lifestyle due to therapy and imposed meals [22]. Since BMI does not distinguish between FM and LBM [24], BIA outcomes (FM% and LBM%) were investigated. Also, no significant changes were identified in the absolute body composition parameters (BMI, WC, FM%, and LBM%) during inpatient rehabilitation, similar to Felleiter’s study [19]. However, they scheduled more measurements during inpatient rehabilitation and found that FM% gradually decreased at the early stages after the injury (2–14 weeks), but then nearly returned to the level at admission in the following weeks until the end of rehabilitation (14–26 weeks). Our stable body composition during inpatient rehabilitation seems to be inconsistent with some other studies [20, 25]. Wilmet et al. [25] found that lower-limb LBM already started to decrease during the first few weeks after injury and this decrease occurred rapidly in people with acute SCI after the first 15 weeks post injury. This period was longer than our inpatient rehabilitation (median: 8 weeks), which could be the reason for not finding significant changes in body composition. In contrast, Wilmet et al. also found that LBM in the arms increased by 30% after the first 6 months indicating different changes in body composition between paralyzed and unaffected parts [25]. In future studies, possible changes in body composition should, therefore, be measured segmentally. Singh et al. [20] reported a significant decrease in LBM below the level of injury and a significant increase in FM% in all regions in people during the first year after injury. This might be explained by their longer study period during rehabilitation (12 months) and that they only included people with motor complete injury [20], while people with motor incomplete injuries can have a smaller decrease in LBM below the lesion level [2]. Finally, no significant changes in body composition were found between different personal and lesion groups during inpatient rehabilitation, which is in line with a previous study in people with chronic SCI [2].
Since the prevalence of overweight/obese individuals was 78% (based on adjusted BMI cut-off points for people with SCI) and 55% (based on BMI cut-off points for general population) at T0, and the median time since injury was only 23 days, we hypothesize that most of these participants were already overweight or obese at the time of SCI. Moreover, studies have showed that early onset of a reduction in body mass can be found in people with SCI because of hypercatabolism and reduced appetite during the first 4 weeks after injury [26, 27]. Thus, there might be more participants with higher premorbid levels of obesity at the time of SCI. However, even though people were already qualified as overweight or obese, body mass gain could still increase the risk status of their obesity-related health problems. According to the World Health Organization (WHO) classification of BMI for the general population, the increased risk is a continuum with increasing BMI and the risk status increases from moderate to very high between the range of 25–40 kg/m2 [28]. A previous study showed that two of every three persons who have SCI were likely obese and appear at risk for the metabolic consequences of obesity [1]. This highlighted the importance of managing obesity after SCI.
During the first year after discharge
The percentage of overweight/obese individuals increased from 63 to 79% in the first year after discharge, which is supported by previous observations [10], indicating that, even though 10–15 years have passed since the study of De Groot et al. [10], the problem of an increase in BMI still exists in the first year after discharge. Useful and effective methods to counteract the unfavorable trend of body composition such as dietary management and exercise prescription during that challenging period are still urgently needed. In contrast, WC did not significantly change, indicating that the increase in body mass is not around the abdominal segment. These contradicting results remain unfortunately unexplained since we were not able to obtain FM% and LBM% in our sub-group. Future studies should collect those parameters and utilize segmental measurements to analyze lean and adipose tissue in specific regions. After discharge, people with paraplegia had a considerably larger increase in WC than those with tetraplegia, who even showed a tendency towards a decrease. A speculative reason could be that people with paraplegia have the ability to use both arms for daily activities (e.g. do groceries and approach food by themselves), giving them increased independence to eat freely in daily life [11], suggesting that the food intake affects the energy balance more in people with paraplegia than the higher levels of physical activity and significantly higher rates of basal energy expenditure compared to those with tetraplegia [29, 30]. Besides the individual difference in energy balance between participants with tetraplegia and paraplegia, there might be multiple factors that could play a role in weight management such as e.g., living situation, economical status [31]. This makes weight management a multivariable and complex issue.
During inpatient rehabilitation, our dieticians provided dietary advice mainly about calorie and protein intake to every participant within the first week of admission. Depending on the seriousness of the situation, follow-up appointments were scheduled at least once every 2 weeks until participants were satisfied with the treatment and reached their personal goals such as losing weight, gaining muscle, or gaining weight. So the stable body composition during inpatient rehabilitation might be explained by the given dietary advice from dieticians. However, future studies should record the dietary advice in detail to investigate whether it could have any effect on body composition during inpatient rehabilitation. After returning home, people with SCI might start with a lifestyle without the control of nutritional intake and without the motivation of being physically active [19, 32], resulting in a rapid increase in body mass.
Strengths and limitations
Our study has some strengths and weaknesses. One of the strengths is that changes in body composition were measured over the less commonly studied subacute phase after SCI. More importantly, no specific inclusion criteria were applied contributing to a heterogeneous and more representative group of participants. The use of self-reported height was an inherent weakness of the BMI calculation. The BIA only provided whole-body but not segmental body composition, disallowing distinguishing the changes in body composition between paralyzed and unaffected parts. The BMI and WC results at 1 year after discharge are somewhat unsupported since no BIA outcomes were available and due to the relatively small sample size. However, the follow-up measurement in the sub-group was of great importance to identify the negative changes in body composition after rehabilitation. Furthermore, alterations in body composition might be different at various stages as shown between 2–14 weeks post injury and 14–26 weeks post injury by Felleiter et al. [19]. Although we did not find any relationship between changes in body composition and length of stay between T0 and T1, potential changes in body composition at specific stages might be concealed. Moreover, it might be valuable to register medication use at each measurement since a change in medication use, such as diabetic medications, can have an impact on the change in body mass.
Future directions
For future studies, segmental measurement of body composition is essential to detect the changes between paralyzed and unaffected parts and studies with a larger sample are needed to evaluate our findings during the first year after discharge. Other anthropometrics such as hip circumference could be beneficial. Also, it could be valuable to gain insight into changes in body composition in different phases during inpatient rehabilitation. Furthermore, it is very important to measure nutritional variables and activity levels and provide timely intervention regarding diet, exercises and education to control the risk of body mass and FM gain in both the inpatient and outpatient phases. Both rehabilitation professionals and people with SCI should be aware of the importance of controlling body composition after the patient leaves the acute inpatient rehabilitation setting.
Conclusions
People with subacute SCI did not show significant changes in body composition during inpatient rehabilitation and changes in body composition were not significantly related to personal and lesion characteristics. However, BMI increased significantly during the first year after discharge and people with paraplegia showed a larger increase in WC compared to people with tetraplegia who showed a net decrease.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gater DR Jr. Obesity after spinal cord injury. Phys Med Rehabil Clin N. Am. 2007;18:333–51.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr., Waters RL, et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95:2398–407.
Tanhoffer RA, Tanhoffer AIP, Raymond J, Hills AP, Davis GM. Exercise, energy expenditure, and body composition in people with spinal cord injury. J Phys Act Health. 2014;11:1393–400.
Bauman WA, Adkins RH, Spungen AM, Waters RL. The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord. 1999;37:765–71.
Maki K, Briones E, Langbein W, Inman-Felton A, Nemchausky B, Welch M, et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Spinal Cord. 1995;33:102.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. 2005;43:408–16.
van Drongelen S, de Groot S, Veeger HE, Angenot EL, Dallmeijer AJ, Post MW, et al. Upper extremity musculoskeletal pain during and after rehabilitation in wheelchair-using persons with a spinal cord injury. Spinal Cord. 2006;44:152–9.
Broad EM, Newsome LJ, Dew DA, Barfield JP. Measured and predicted resting energy expenditure in wheelchair rugby athletes. J Spinal Cord Med. 2020;43:388–97.
Crane DA, Little JW, Burns SP. Weight gain following spinal cord injury: a pilot study. J Spinal Cord Med. 2011;34:227–32.
de Groot S, Post MWM, Postma K, Sluis TA, van der Woude LHV. Prospective analysis of body mass index during and up to 5 years after discharge from inpatient spinal cord injury rehabilitation. J Rehabil Med. 2010;42:922–8.
Gupta N, White KT, Sandford PR. Body mass index in spinal cord injury - a retrospective study. Spinal Cord. 2006;44:92–4.
Willems A, Paulson TA, Keil M, Brooke-Wavell K, Goosey-Tolfrey VL. Dual-energy X-ray absorptiometry, skinfold thickness, and waist circumference for assessing body composition in ambulant and non-ambulant wheelchair games players. Front Physiol. 2015;6:356.
Cirnigliaro CM, La Fountaine MF, Emmons R, Kirshblum SC, Asselin P, Spungen AM, et al. Prediction of limb lean tissue mass from bioimpedance spectroscopy in persons with chronic spinal cord injury. J Spinal Cord Med. 2013;36:443–53.
Gorgey AS, Dolbow DR, Gater DR Jr. A model of prediction and cross-validation of fat-free mass in men with motor complete spinal cord injury. Arch Phys Med Rehabil. 2012;93:1240–5.
Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G. Body composition assessment in spinal cord injury subjects. Acta Diabetol. 2003;40:S183–6.
Mojtahedi MC, Valentine RJ, Evans EM. Body composition assessment in athletes with spinal cord injury: comparison of field methods with dual-energy X-ray absorptiometry. Spinal Cord. 2009;47:698–704.
Ravensbergen HJC, Lear SA, Claydon VE. Waist circumference is the best index for obesity-related cardiovascular disease risk in individuals with spinal cord injury. J Neurotraum. 2014;31:292–300.
Spungen AM, Bauman WA, Wang J, Pierson RN Jr. Measurement of body fat in individuals with tetraplegia: a comparison of eight clinical methods. Paraplegia 1995;33:402–8.
Felleiter P, Krebs J, Haeberli Y, Schmid W, Tesini S, Perret C. Post-traumatic changes in energy expenditure and body composition in patients with acute spinal cord injury. J Rehabil Med. 2017;49:579–84.
Singh R, Rohilla RK, Saini G, Kaur K. Longitudinal study of body composition in spinal cord injury patients. Indian J Orthop. 2014;48:168–77.
Gorgey AS, Caudill C, Sistrun S, Khalil RE, Gill R, Castillo T, et al. Frequency of dietary recalls, nutritional assessment, and body composition assessment in men with chronic spinal cord injury. Arch Phys Med Rehabil. 2015;96:1646–53.
de Groot S, Post MW, Hoekstra T, Valent LJ, Faber WX, van der Woude LH. Trajectories in the course of body mass index after spinal cord injury. Arch Phys Med Rehabil. 2014;95:1083–92.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Laughton GE, Buchholz AC, Martin Ginis KA, Goy RE, Group SSR. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord. 2009;47:757–62.
Wilmet E, Ismail AA, Heilporn A, Welraeds D, Bergmann P. Longitudinal study of the bone mineral content and of soft tissue composition after spinal cord section. Paraplegia. 1995;33:674–7.
Laven GT, Huang CT, DeVivo MJ, Stover SL, Kuhlemeier KV, Fine PR. Nutritional status during the acute stage of spinal cord injury. Arch Phys Med Rehabil. 1989;70:277–82.
Rodriguez DJ, Benzel EC, Clevenger FW. The metabolic response to spinal cord injury. Spinal Cord. 1997;35:599–604.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Mollinger LA, Spurr GB, el Ghatit AZ, Barboriak JJ, Rooney CB, Davidoff DD, et al. Daily energy expenditure and basal metabolic rates of patients with spinal cord injury. Arch Phys Med Rehabil. 1985;66:420–6.
Mc Cormack K, Carty A, Coughlan G, Crowe L, Caulfield B. The effects of a neuromuscular electrical stimulation training intervention on physiological measures in a spinal cord injured male: a case study. Physiother Pract Res. 2010;31:30–5.
Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8:402–24.
van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, Bergen MP, et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil. 2008;89:2094–101.
Acknowledgements
We thank the rehabilitation center Reade in Amsterdam which have contributed to the organization of measurements. We appreciate the cooperation of all the participants.
Author information
Authors and Affiliations
Contributions
SDG conceived the study. SR, WA, and LVO recruited participants and collected the data. YM, SDG, and TJ interpreted the data. YM drafted the paper. YM, SDG, and TJ revised the paper and all authors approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Medical Ethical Committee of Slotervaart Hospital and Reade rehabilitation center.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, Y., de Groot, S., Romviel, S. et al. Changes in body composition during and after inpatient rehabilitation in people with recent spinal cord injury. Spinal Cord Ser Cases 7, 88 (2021). https://doi.org/10.1038/s41394-021-00446-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00446-x
This article is cited by
-
Obesity in wheelchair users with long-standing spinal cord injury: prevalence and associations with time since injury and physical activity
Spinal Cord (2024)
-
Bilateral tibial fractures associated with powered exoskeleton use in complete spinal cord injury – a case report & literature review
Spinal Cord Series and Cases (2024)
-
Monitoring outcome measures for cardiometabolic disease during rehabilitation and follow-up in people with spinal cord injury
Spinal Cord (2024)
-
Risk constellation of hospital acquired pressure injuries in patients with a spinal cord injury/ disorder - focus on time since spinal cord injury/ disorder and patients’ age
Spinal Cord (2023)