Abstract
In May 2023, a disclaimer posted on ClinicalTrials.gov dismisses accountability for the accuracy of registered information. For spinal cord injury, inconsistencies in intervention classification, phase designation, and lack of study protocols and results threaten the integrity of the database and put users at risk. An investment in what the resource should be rather than what it is not will give it the authority commensurate with the requirements for its regulatory use and informed decision-making for prospective trial participants.
Similar content being viewed by others
Main text
Clinical trial registration on ClinicalTrials.gov is required for trials under the jurisdiction of the Food and Drug Administration (FDA), those funded by the NIH, and trial results published in journals under the umbrella of the International Committee of Medical Journal Editors (ICMJE). If registration is mandatory, then curation to ensure accurate reporting is necessary. On May 25, 2023, the United States National Library of Medicine at the National Institutes of Health (NIH) posted a disclaimer on ClinicalTrials.gov effectively disowning accountability for errors or omissions of data uploaded to its site. It states:
“The U.S. government does not review or approve the safety or science of all studies listed on this website. The study sponsor or investigator submits information about their study to ClinicalTrials.gov and is responsible for the safety, science, and accuracy of any study they list.” (ClinicalTrials.gov)
The stated purpose of the ClinicalTrials.gov database, “… is to provide information about clinical research studies to the public, researchers, and health care professionals”, combined with the new disclaimer is paradoxical to its efforts to “support laws, regulations, and policies that require sponsors and investigators to publicly share information about clinical trials, including results”. Rather than addressing areas for improvement through monitoring or a standardized approval process, the May update trivializes the information ClinicalTrials.gov professes to offer, undermines regulatory and publication requirements, and is offensive to all who rely on it.
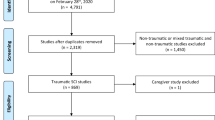
Significant gaps in the ClinicalTrials.gov database have been documented in the past [1]. We are particularly concerned about clinical trials for people living with spinal cord injury (SCI) for whom biomedical innovation is regularly featured in news media, and who may turn to the database for scientific details and opportunities for enrollment in trials themselves. Each year, the life-altering condition of SCI affects between 250,000 and 500,000 people worldwide [2]; with life-time healthcare costs ranging from US$1.3–5.8 million in North America [3], creating a dire unsolved need for effective, population-wide interventions.
The lack of oversight and enforcement permits inconsistencies and incomplete information to be posted on the database. Medically vulnerable participants are left to decipher variances in definitions, such as the timing of interventions. For example, the recorded timeframe for acute injuries spans a few hours to a few months post-injury (e.g., NCT02260713, NCT04331405, NCT01694927), and for chronic injuries ranges 5 to 18 months and in some cases 20 years (NCT01005615). Some entries do not define the time window of recruitment at all. While a lack of consensus on timing definitions may mirror the research literature where a surgical intervention can define acute as <24 h and a biological intervention as <12 h, we could not determine any such trend from our examination of over 400 studies.
While the labeling of interventions for some trials are correct, such as TCA Cellular Therapy (USA) NCT01162915 transfer of bone marrow derived stem cells for the treatment of SCI, others are inconsistent. Some stem cells trials may be categorized as a drug, genetic, or procedural intervention (Table 1) rather than the biological one that it is. Trials with Botox/Botulin toxin A are categorized as both as a biological intervention and as a drug intervention. Stem cells are unequivocally a biological product and should be categorized as such.
The Not Applicable Phase category, defined as “trials without FDA-defined phases, including trials of devices or behavioral interventions” presents further ambiguity. It accounts for a majority of SCI clinical trial studies [1]. However, there is a lack of clarity about what type of intervention qualifies for a Not Applicable Phase study versus Phase I, or if a successful trial in the Not Applicable Phase moves to a Phase I or to directly a Phase IV designation. Two biomaterial scaffolds that are in trials illustrate this concern: one is registered in the Not Applicable Phase and categorized as a device; the other is registered in Phase II and categorized as a biological intervention (Table 2). This opacity in the categorization of intervention or phase is a serious barrier to scientific reliability and accountability.
The FDA calls for mandatory reporting of results and study protocols to ClinicalTrials.gov for applicable clinical trials [4], yet the majority of completed trials do not have results posted on the database [1] and the recent disclaimer further nullifies this requirement. The absence of published results pertaining to reported adverse events is a critical barrier to informed decision-making. Uncurated and vague criteria such as leaving undefined exclusion criteria to investigator discretion pose ethical challenges to transparency and inclusivity.
SCI trials are suspended, terminated, or withdrawn due to low enrollment numbers [5, 6]. People living with SCI rely heavily on online sources for information and the trustworthiness of available information is second only to interest [7]. Both are compromised when information is poor or inaccurate, creating a void that can be filled by unscrupulous sources leading to misinformation and mistrust in science. This is a violation of any code of ethics governing research, and ultimately will translate to hesitation to take up interventions that are brought to market. A SCI specific clinical trial database (https://scitrialsfinder.net/trials) has been created to meet the needs of the community. If every patient group had to resort to hosting its own trials tracking site, the proliferation of inefficiencies, inaccuracies, and dubiety would be extraordinary.
Vague wording in the 2013 amendments to the Declaration of Helsinki creates ambiguity around the responsible party for ensuring post-trial access in low- and middle-income countries demonstrating a further waning from ethical principles meant to protect vulnerable participants [8]. The FDA does not require compliance with the Declaration of Helsinki for protocols under their jurisdiction but implemented overseas. Although post-trial access is normally identified in the consent protocols, listing them on the ClinicalTrials.gov database would significantly enhance transparency.
Oversight and enforcement of registered studies is essential for the reliability and utility of the ClinicalTrials.gov database, and accountability for the accuracy and completeness of study information is vital to fulfilling its purpose. Clear definitions and consistency across the type of interventions and categorization of trial phase will provide clarity and reliability of available information; monitored transparency about adverse events will bring new research to improve the quality-of-life of people living with SCI, clinical outcomes, and addressing the related economic burden of SCI (Table 3).
Although we acknowledge that reviewing the safety and science of all studies is a high bar to reach, oversight for consistency and standardization in terminology and categorization of an intervention is a must for the database to fulfill its stated purpose. Rather than hiding behind a disclaimer, an investment in Clinicaltrials.gov that is commensurate with the gravitas of the requirements for engaging with it will empower contributors, revive the usefulness of this important resource, and support the autonomy and decision-making of trial participants.
References
Dietz VA, Roberts N, Knox K, Moore S, Pitonak M, Barr C, et al. Fighting for recovery on multiple fronts: the past, present, and future of clinical trials for spinal cord injury. Front Cell Neurosci. 2022;16:977679.
World Health Organization. (2013, November 19) Spinal cord injury. Accessed 31 Jul 2023.
National Spinal Cord Injury Statistical Centre. (2022) Traumatic spinal cord injury facts and figures at a glance. Accessed 1 Aug 2023.
National Institutes of Health DpoHaHS. Clinical trials registration and results information submission. Final rule. Fed Regist. 2016;81:64981–5157.
Lee RS, Noonan VK, Batke J, Ghag A, Paquette SJ, Boyd MC, et al. Feasibility of patient recruitment into clinical trials of experimental treatments for acute spinal cord injury. J Clin Neurosci. 2012;19:1338–43.
Blight AR, Hsieh J, Curt A, Fawcett JW, Guest JD, Kleitman N, et al. The challenge of recruitment for neurotherapeutic clinical trials in spinal cord injury. Spinal Cord. 2019;57:348–59.
Farrehi C, Pazzi C, Capron M, Anderson K, Richardson B, Stillman M. How individuals with spinal cord injury in the United States access and assess information about experimental therapies and clinical trials: results of a clinical survey. Spinal Cord Ser Cases. 2020;6:103.
Hellmann F, Bernabe RC, Homedes N. Post-trial provisions in the declaration of Helsinki: a watered-down principle that needs to be strengthened. J R Soc Med 2022;115:420–3.
Acknowledgements
Dr. Judy Illes is Distinguished University Scholar, and UBC Distinguished Scholar in Neuroethics supported by the North Family Foundation. Wolfram Tetzlaff is a Professor and Principal Investigator at ICORD, a UBC centre for spinal cord injury research. The authors acknowledge the contribution of Neuroethics Canada team members to this project.
Funding
Government of Canada New Frontiers in Research Fund (NFRF), NFRFT-2020-00238.
Author information
Authors and Affiliations
Contributions
TAB: conceptualization and design of study and methodology, data analysis, manuscript writing; WT, JI: consultation on study-design and data interpretation, manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barretto, T.A., Tetzlaff, W. & Illes, J. Ethics and accountability for clinical trials. Spinal Cord 62, 192–194 (2024). https://doi.org/10.1038/s41393-024-00980-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-024-00980-z