Abstract
Study design
Cohort study.
Objectives
To evaluate the association between residential living location and health outcomes, environmental barriers, quality of life, and healthcare utilization patterns after traumatic spinal cord injury (tSCI).
Setting
Community setting, Atlantic Canada.
Methods
An ambispective study of data collected on a subset of individuals enrolled in the Rick Hansen Spinal Cord Injury Registry (RHSCIR) from 2012 to 2018. Outcomes were analyzed using two measures of rurality: postal codes at community follow-up (rural versus urban) and residential travel distance to the nearest RHSCIR facility (>100 km versus ≤100 km). Outcomes studied included the Craig Hospital Inventory of Environmental Factors-Short Form (CHIEF-SF), Short Form-36 Version 2 (SF36v2), Life Satisfaction Questionnaire (LISAT-11), Spinal Cord Independence Measure (SCIM), secondary health complications and healthcare utilization patterns. Outcomes were assessed 9 to 24 months post-discharge from initial hospitalization.
Results
104 participants were studied, 21 rural and 83 urban based on postal codes at community follow-up. 59 participants lived more than 100 km away from the nearest RHSCIR facility, while 45 participants lived within 100 km. Individuals from urban area codes reported a greater magnitude of perceived barriers on the policies and work/school subscales of the CHIEF-SF. No differences in function, quality of life, and healthcare utilization patterns according to the measures of rurality were observed. Individuals living >100 km from the nearest RHSCIR facility reported greater rates of sexual dysfunction.
Conclusions
Despite differences in environmental barriers, individuals from urban and rural locations in Eastern Canada reported similar health outcomes and quality of life after tSCI.
Similar content being viewed by others
Introduction
The International Classification of Function framework from the World Health Organization (WHO) emphasizes how function and health are a dynamic interplay between impairments, environmental factors and personal factors [1]. The impairments that result from traumatic spinal cord injury (tSCI) may have different effects on individuals, depending on their geographic area of residence.
Individuals with tSCI have multi-system impairments, which can include spasticity, neuropathic pain, heterotopic ossification, muscle weakness and immobility, neurogenic bowel and bladder, autonomic instability, pressure ulcers, sublesional osteoporosis, and impaired cough and ventilatory function [2]. As a result of these impairments, individuals with tSCI report a greater use of inpatient and outpatient healthcare services compared to persons without tSCI [3]. Individuals with tSCI also have unique activity limitations and participation restrictions that require a comprehensive, collaborative healthcare approach. The ability to access these services may vary according to geographic setting. Utilization of inpatient and outpatient services has been noted to be inversely correlated with travel distance to healthcare facilities [4]. Despite this correlation, there is little research evaluating the impact of rurality and healthcare utilization patterns on overall health outcomes after tSCI. Research to date on health outcomes after SCI has primarily focused on the effect of age, gender and injury-related factors, rather than on environmental markers such as rurality and distance to nearest healthcare facility [5].
In addition, there has been a paucity of research evaluating the influence of rural versus urban living location on perceived environmental barriers in patients with tSCI, and how that relates to health outcomes, healthcare utilization patterns and life satisfaction [6]. The ability to participate in meaningful life roles and activities after tSCI is affected by environmental factors, including the accessibility of the natural and built environment, social support networks (e.g., personal care assistance, peer mentors), public transportation systems, governmental policies and community attitudes towards disability and reintegration [6,7,8,9]. A greater magnitude of environmental barriers has been shown to be predictive of physical and mental health after SCI [10]. Although environmental barriers have been correlated with injury characteristics and sociodemographic variables such as household income and income inequality, there is little research examining the correlation between rurality and environmental barriers after tSCI [11].
Given these issues, the purpose of this study was to determine whether there is a difference in environmental barriers and health outcomes between rural and urban individuals with tSCI from Atlantic Canada. This is a region of Eastern Canada, which compromises four provinces and has a population of approximately 2.3 million people. As the region primarily consists of sparsely populated communities with a limited number of tertiary medical centers and thus, residents have varied access to specialized tSCI care, we would expect environmental barriers to be greatest for individuals from rural locations. The primary outcome of the study is to evaluate whether environmental barriers, health, and quality of life outcomes differ based on rural versus urban location, in addition to distance from RHSCIR centers. The secondary objectives are to evaluate if persons with tSCI are moving closer to regions with densely populated areas, and to determine if longer travel distances to tertiary SCI healthcare facilities are associated with reduced healthcare utilization.
Methods
Data sources and study population
This study utilized data from the Rick Hansen Spinal Cord Injury Registry (RHSCIR) from patients admitted to one of three acute SCI hospitals or to one of three SCI rehabilitation centers within Atlantic Canada between 2012 and 2018 [12]. RHSCIR is a national prospective registry of adult persons with a new tSCI admitted to one of eighteen acute and twelve rehabilitation facilities across Canada [11]. All participating facilities have local ethics approval prior to enrolling patients. The registry maintains a minimal data set on all individuals with tSCI, in addition to an expanded data set and community follow-up (CFU) for those who provide informed consent [12, 13]. Individuals were included in this study if they provided consent to CFU, had CFU data collected between 9- and 24-months post-discharge from inpatient care, survived their initial hospitalization, lived within Atlantic Canada at CFU, and provided their postal code at discharge.
Rural and urban setting
The definition of rural and urban varies in the literature, however, it is generally accepted that rural refers to both population density and distance from a densely populated area [14]. Statistics Canada defines an urban population center as an area with a population of at least 1,000 persons and a density of 400 or more people per square kilometer [6]. Across the country regions not satisfying the urban criteria are defined as rural and are uniformly identified by the number “0” in the second digit of the postal code. Using this definition, study participants were grouped into rural and urban cohorts based on the residential postal code at CFU.
Distance from specialized SCI center
Outcomes were evaluated according to travel distance from residential address to the nearest RHSCIR facility. These data were obtained by calculating the driving distance for each participant from their residential postal code at CFU to the nearest RHSCIR facility. The distance was calculated by inputting this information into Google Maps and selecting the option of departing at 12:00 am using the shortest calculated distance. There is limited research to define a cut-off travel distance that is known to affect patient health outcomes or healthcare utilization patterns. This value was chosen based on research by Canale et al. that investigated cancer-related outcomes in British Columbia [14]. The hypothesis is that patients, family members or caregivers are willing to travel 100 km or less to receive medical care, as it represents a manageable driving time of 60 min or less. Participants were divided into two groups: those living >100 km from the nearest RHSCIR facility, and those living ≤100 km from the nearest RHSCIR facility. Primary outcomes and healthcare utilization patterns were compared between these two groups.
Demographic and injury characteristics
Information that was included from the RHSCIR dataset for the purpose of this study included: sex, age at injury, comorbidities (based on the Charlston Comorbidity Index), education level, employment status, marital status, living setting, compensation status (disability insurance/workers compensation/none), mechanism of injury, neurological injury severity by the American Spinal Injury Association (ASIA) Impairment Scale (AIS) (AIS A, B, C, D, E), and neurological injury level (cervical, C1–C8; thoracolumbar, T1 and below) derived from the International Standards for Neurological Classification of SCI examination [15].
Primary outcome
The primary outcome was to evaluate environmental barriers, health outcomes, and secondary health complications according to rurality and travel distance to the nearest RHSCIR facility. Outcome data were evaluated using several validated questionnaires from the extended RHSCIR dataset at CFU. Environmental barriers were assessed using the Craig Hospital Inventory of Environmental Factors-Short Form (CHIEF-SF). The CHIEF-SF assesses the impact of physical, social, and political barriers on activity participation [16]. The mean CHIEF-SF score was calculated in addition to the mean scores of the five subscales, which include policy, physical/structural, work/school, attitudes/support and services/assistance barriers. Scores are the product of the frequency score (from never = 0 to daily = 4) and the magnitude of impact score (little problem = 1, big problem = 2). A greater score indicates greater severity of environmental barriers. Health outcomes were explored by using the Medical Outcomes Study 36-Item Short Form-36 Version 2 (SF36v2), the Life Satisfaction Questionnaire 11 (LISAT-11), the Functional Independence Measure (FIM), and the Spinal Cord Independence Measure (SCIM). The SF36v2 assesses health status and can be reported as a profile of eight health domains: physical functioning, role limitations due to physical health problems, bodily pain, general health, vitality, social functioning, role limitations related to emotional problem and mental health [17]. It can also be reported as two summary scores, the Physical and Mental Component Scores (PCS and MCS), which were done in this study. A lower score is associated with more disability. The LISAT-11 is an eleven-item measure of quality of life and satisfaction regarding important life domains: vocational, financial and leisure situations, contacts with friends, sexual life, self-care management, family life, partner relationships and physical and psychological health [18]. Higher scores indicate greater life satisfaction. The FIM assesses independence with 13 motor and 5 cognitive tasks, with each task graded on a scale from 1 (total assistance) to 7 (complete independence) [19]. The SCIM evaluates independence with self-care, respiration and sphincter management and mobility [20]. Higher FIM and SCIM scores are associated with greater independence. RHSCIR also tracks secondary health complications related to SCI. The complications that were compared between groups with respect to the secondary outcomes were: autonomic dysreflexia, deep vein thrombosis, depression, pressure injury, sexual dysfunction, spasticity, and urinary tract infections (UTI). These conditions were chosen based on the study by Glennie et al., as these complications could require specialized care that may not be available in rural locations [6].
Secondary outcomes
The secondary outcomes were to evaluate if persons with tSCI are moving closer to regions with densely populated areas, and to determine the relationship between travel distances to RHSCIR facilities and healthcare utilization patterns. The postal codes at discharge and CFU were compared to determine if any participant moved from one living setting to another between discharge and CFU. The expanded RHSCIR dataset was used to evaluate healthcare utilization patterns. The patterns that were compared between groups based on distance to nearest RHSCIR facility included re-hospitalization, types of healthcare visits (e.g., family physician, physical medicine and rehabilitation specialist, spine surgeon, allied health professionals), and patient-reported access and barriers to healthcare.
Statistical analysis
Descriptive statistics were generated for all baseline demographic and injury variables. Student t-tests (normal) or Wilcoxon two–sample tests (non-normal) were used to compare continuous variables and chi-square tests for categorical variables. Unadjusted bivariate analysis was performed to compare participants living in rural vs urban settings post-discharge, and to compare participants according to distance to nearest RHSCIR facility. All analyses were carried out using SAS STAT 12.1 version 9.4 (SAS Institute, Cary NC.). A p-value of less than 0.05 was considered statistically significant. Sensitivity analysis was performed to compare the study cohort with the participants who had no CFU to determine if there is any potential bias in the cohort.
Results
Demographic data according to rural versus urban population density
From 2012-2018, 340 patients were admitted to Atlantic Canada RHSCIR sites (Fig. 1). In total, 104 participants with CFU at 9–24 months were included in the study. 21 participants lived in rural postal codes at CFU, and 83 lived in urban postal codes. 59 participants lived more than 100 km away from the nearest RHSCIR facility, while 45 participants lived within 100 km. There were no significant differences in age at injury, sex, comorbidity count, employment status, education level, marital status, living setting, living set-up (i.e., home alone versus with home with family/friends), and compensation type when comparing participants according to rural and urban postal codes, and according to distance to the nearest tertiary care facility (Table 1). Individuals who lived more than 100 km away from the nearest RHSCIR facility were less likely to be discharged home, as compared to those who lived within 100 km. Nearly 20% of participants in the “>100 km” group were discharged to another hospital after leaving the RHSCIR facility. This is consistent with patients who live far from the treating facility being repatriated to their local hospital where final discharge destination is arranged. There was no association between discharge destination and postal codes.
There were no significant differences in mechanism of injury or neurological injury severity (AIS) at admission and discharge according to postal code and travel distance (Table 2). There were no differences in neurological level of injury at admission and discharge according to urban versus rural postal codes. Neurological level of injury at admission and discharge were significantly different according to travel distance. Neurological diagnosis at discharge was significantly different according to travel distance, but not according to postal codes.
Sensitivity analysis comparing the study cohort with the participants with no CFU showed that the group with no CFU had significantly more females (35% vs 15%, p = 0.004), fewer were employed (46% vs 70%, p = 0.003), and fewer were married or in common law (40% vs. 61%, p = 0.01).
Primary and secondary outcomes according to rural versus urban population density
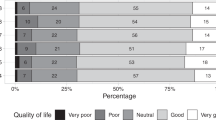
Participants living in urban settings after 9–24 months of CFU reported greater environmental barriers than those residing in rural locations in the policies (0.34 ± 0.69 vs. 0.05 ± 0.22) and work/school subscales (0.28 ± 0.79 vs 0 ± 0) of the CHIEF-SF (Table 3). There were no significant differences in the SF36v2, FIM, SCIM, or LISAT-11 scores when comparing patient groups during CFU (Table 3). There were no significant differences between groups when comparing the secondary health complications of autonomic dysreflexia, deep vein thrombosis, depression, pressure injuries, spasticity, sexual dysfunction, or urinary tract infections (Table 3). There were no differences in healthcare utilization patterns between groups, including re-hospitalization, and visits to family physicians, spine surgeons, physiatrists, and allied health professionals (Table 4, Fig. 2a). Barriers to healthcare utilization were similar between groups, with the main issue being related to waiting time and lack of available services (Table 4).
Primary and secondary outcomes according to distance to closest RHSCIR facility
The outcomes at CFU, including CHIEF-SF, LISAT-11, SF36, FIM, SCIM, and secondary health complications, were not significantly different according to travel distance to the nearest RHSCIR facility (Table 3). Individuals living >100 km from the nearest RHSCIR facility were more likely to report sexual dysfunction after injury. There were no differences in healthcare utilization patterns between groups, including re-hospitalization, access and barriers to healthcare and visits to family physicians, spine surgeons, physiatrists, and allied health professionals (Table 4, Fig. 2b). Barriers to healthcare utilization were similar between groups, with the main issue being related to waiting time and lack of available services (Table 4).
Patient migration
No participants migrated from an urban to rural setting or from a rural to urban setting between time of discharge and CFU.
Discussion
In this study, two measures of rurality—postal code at CFU and travel distance to the nearest RHSCIR facility—were used to evaluate environmental barriers, health outcomes and healthcare utilization patterns after tSCI. There were similar health outcomes between individuals from rural and urban postal codes and between individuals who lived >100 km or ≤100 km from the nearest RHSCIR facility, based on measurements of function (FIM, SCIM), quality of life (LISAT-11), health status (SF36), medical complications and healthcare utilization patterns. The only difference was those individuals living more than 100 km away from the nearest tertiary care facility were more likely to report sexual dysfunction after tSCI. This may reflect the neurological level of injury and not the impact of rurality, as individuals in this group were more likely to have complete paraplegia.
Goodridge et al. reported that most SCI participants from rural areas in the province of Saskatchewan, Canada, valued the benefits of living in rural settings and described that their decision to remain in a rural location post-discharge was often not supported by their healthcare provider. It was perceived that individuals with disabilities from rural areas could have worse health outcomes, as there may be limited access to recreational activities, medical care providers and work/school opportunities. There appears to be a growing amount of evidence to suggest that SCI patients from rural areas can have similar—and sometimes better health outcomes—as compared to their urban counterparts. This may be related to the protective effects of a tight-knit community and to the accessibility of open rather than built-up environments [21]. Glennie et al. found that mental health outcomes were better in individuals with tSCI from rural areas in British Columbia, as compared to those living in urban settings and those who migrated from rural to urban settings [6]. A large study of 1454 individuals with tSCI in New Jersey and Alabama reported that life satisfaction was greatest in rural communities [22]. These trends may not be unique to the SCI population: an evaluation of 1200 Canadian neighborhoods and communities found that populations exceeding 50,000 people reported less life satisfaction than smaller communities, despite having lower rates of unemployment and higher incomes [23].
A strong foundation of social support is essential for promoting mental and physical health, community re-integration and functional independence after tSCI [7]. Social relationships with friends, colleagues, and family members are an important motivating factor to participate in community life following SCI [7]. The protective effect of social relationships could explain the benefits of remaining in one’s community after injury. Glennie et al. found that patients who migrated from rural to urban settings after discharge reported worse health outcomes [6]. The transition of moving is disruptive and can interfere with support networks. This may explain the benefits of living in either rural or urban locations in Atlantic Canada, and why patients did not migrate between urban and rural settings after community follow-up.
The similarities in outcomes of health and function according to measures of rurality may also have been related to comparable access to outpatient care. There were no differences in healthcare visitations to physicians and allied health professionals during CFU when participants were stratified according to postal code or travel distance after discharge. There have been a limited number of studies that have looked at healthcare utilization patterns according to travel distances. Bell et al. found that longer travel distances were inversely related with physician and physiotherapist visits [24]. In our study, there were no differences between the “≤100 km” and “>100 km” groups with respect to physician and allied health professional visits during community follow-up. However, travel distance was to the nearest RHSCIR facility, so it may not necessarily reflect the location of care. Ronca et al. found that individuals who had to travel more than 69 min to a tertiary SCI center were more likely to forgo specialist care in exchange for more generalist local care [25]. In our study, there were similar rates of specialist care (e.g., spine surgeon, physical medicine and rehabilitation specialist, urologist) with a cut-off travel distance of 100 km, which corresponds to a travel time of ~60 min. However, a limitation of our study was that we did not record the number of visits for each provider. Individuals from rural settings may have achieved similar health outcomes by visiting physicians and allied health professionals a different number of times. Guilcher et al. reported a mean number of physician visits of 29.7 for traumatic SCI during the first year after inpatient rehabilitation [26]. There were different patterns of utilization according to rurality, with those living in an urban setting more likely to have 30 or more physician visits and 20 or more specialist visits, while those living in a rural environment were more likely to have two or more ED visits. Munce et al. also found that patients from rural locations were more likely to visit the emergency department for their healthcare needs [27]. As a result, there may have been differences in healthcare utilization patterns that were not captured with the RHSCIR dataset used in this study. In addition, we only looked at healthcare visitations within the first 9–24 months post-discharge; it is possible that the demand for healthcare may have changed and diverged between groups the longer individuals lived in their communities.
We also demonstrated that participants with tSCI in Atlantic Canada experience relatively similar environmental barriers and difficulties accessing care according to geographical area of residence, which may have contributed to similar health and functional outcomes. The main challenges for obtaining care included a lack of available services, lack of information to access these services, and lengthy waiting times. The issue of waiting times has been previously identified as a major concern in SCI-related care in a qualitative study by Goodridge et al. [21]. Although there were some services that were well-accessed by participants, there were some services that appear to be underutilized. Less than 5% of participants had access to a vocational counselor, despite 65% being employed prior to their injury. Only one person visited a peer support person, which is discouraging as the availability of peer support after SCI discharge has been highlighted as an important resource for maintaining health and wellness [21]. Only one person visited a sexual health clinician in the first year of community follow-up, despite approximately half of participants reporting sexual dysfunction in the last 12 months.
Individuals from rural and urban living locations perceived the most environmental barriers within the physical/structural subscale of the CHIEF-SF. This finding has been recognized in three previous studies on tSCI [6, 8, 10]. Participants from rural and urban postal codes reported scores of 1.79 and 1.93, respectively on the physical/structural subscale. These scores are higher than those reported in non-disabled populations (0.39 ± 0.60) by Whiteneck et al., suggesting a common barrier to individuals with tSCI [16]. Holliday and Kurl identified an accessibility gap within Canada, which respondents attributed to older buildings which are harder to renovate, the expensive costs of creating accessible environments, the lack of general understanding about what accessibility entails, the lack of importance given to accessible designs during construction, and the lack of governmental enforcement [28]. These factors are most related to the built environment and may explain the magnitude of barriers identified within the physical/structural subscale of the CHIEF-SF. Cao et al. reported that the physical/structural and services/assistance subscales of the CHIEF-SF were most predictive of mental and physical health after SCI [10]. This may explain the health outcomes in our study, as these subscales were similar between urban and rural cohorts and between those living “≤100 km” and “>100 km” from the nearest RHSCIR facility. As well, previous research has suggested that scores on the CHIEF-SF may account for only 4% and 10% of the variation in participation and life satisfaction measures [8].
Individuals with tSCI from urban postal codes in Atlantic Canada experienced more environmental barriers than those from rural locations with respect to the CHIEF-SF subscales of work/school and policies. These same findings were not replicated using travel distance as a marker of rurality. High population density, outdated infrastructure, poor urban planning and a built-up environment with obstacles such as stairs, curbs, and sidewalks may pose unique challenges to individuals with tSCI from urban areas [28]. These factors may have contributed to the differences in the policies subscale scores, as the policy barriers may have been more apparent in a built-up, urban environment. In addition, individuals from rural postal codes reported no barriers within the work/school subscale. It is unclear why this was the case. There were no differences in rates of employment pre- and post-injury according to postal codes at discharge.
Glennie et al. compared environmental barriers and health outcomes between rural and urban participants in British Columbia [6]. They concluded that urban participants reported fewer perceived environmental barriers, particularly with respect to the physical/structural and services/assistance subscales. It is unclear why there may be differences in perceived barriers between rural and urban patients from Atlantic Canada and British Columbia, but this may relate to differences in climate and injury characteristics. In our study, individuals from urban areas were more likely to have a cervical neurological level of injury at discharge, which was not the case in the study by Glennie et al. It has been shown that individuals with disability reduce their community participation when exposed to snowy and cold weather [29]. This may be less of a factor in British Columbia, as the province has a much milder climate during the winter months than Atlantic Canada, particularly in major cities such as Vancouver and Victoria.
Limitations
There are several limitations to this study. As the RHSCIR data set depends on participant recall, there is the possibility of recall bias and incompleteness of the information gathered. There were some incomplete data fields on the CFU related to demographics and health outcomes for some participants. In addition to the incomplete data fields, missing postal codes contributed to a high number of patients from the RHSCIR data set that were not eligible for the study, which could have contributed to non-response bias. The use of any existing data set such as RHSCIR limits the number of potential outcome variables. For example, healthcare utilization is only documented according to whether a person has seen a healthcare specialist or not, and does not record the number of visits. In addition, we did not explore whether healthcare visits were conducted by telehealth or through in-person assessments. It is possible that telehealth services may have had an impact on the ability of rural individuals to access specialized care. Although this is a multi-center study, it is based on a regional data set, so the results may not be generalizable to other populations. The lack of qualitative data and open-ended responses may have limited our ability to fully understand the details of the barriers perceived.
In addition, a rural location was defined according to postal code, as this is how rurality is defined through Statistics Canada. Any location with a population less than 1000 persons and a density of less than 400 or more people per square kilometre is considered rural and is identified by a zero as the second digit of the postal code. There are limitations to this definition, as an urban postal code in this study included any population center above 1000 people. In Canada, any area that is not rural can be classified as either a small population center (1000–29,999 people), medium population center (30,000–99,999 people) or large population center (100,000 or more people). This distinction was not made in this study, in line with previous work by Glennie et al. [6] in British Columbia, Canada. This does represent a limitation, as small to medium population centers could have different economic, demographic, and living conditions than those experienced in larger centers. It is for these limitations that outcomes and barriers were explored according to travel distance.
The results were analyzed using a travel distance cut-off of 100 km, based on research by Canales et al. [14]. The manuscript used a cut-off value, rather than an interval scale measure, to have two dichotomous measures of geography (travel distance and postal codes). This represents a limitation of the study, as environmental barriers, health outcomes and healthcare utilization patterns may have differed over a range of travel distances, rather than over a set cut-off point.
This research involved several statistical comparisons. Less than 5% of all the statistical tests met criteria for statistical significance. It is possible that those tests which met statistical significance were incidental rather than clinically meaningful findings, as it is expected that around 5 percent of findings are incidental when an alpha value of 0.05 is used.
Conclusion
Individuals from urban area codes in Atlantic Canada reported a greater magnitude of perceived barriers on the policies and work/school subscales of the CHIEF-SF. No differences in function, quality of life, and healthcare utilization patterns were seen when analyzing individuals according to rural versus urban area codes, and according to travel distance to the nearest RHSCIR facility. Individuals living >100 km from the nearest RHSCIR facility reported greater rates of sexual dysfunction. Although this suggests that living location may not have an impact on outcomes after tSCI in Atlantic Canada, it is possible that different measures of geography may have yielded different results. As this study only explored outcomes within a 9-to-24-month community follow-up period, future research should explore longer time periods after tSCI. Travel distance and rurality may have a greater influence on life satisfaction, community participation, and healthcare utilization patterns as individuals age with tSCI. In addition, future research should explore how the availability of independent transportation affects health outcomes after tSCI, as this may have a greater impact on accessing health services than travel distance or rurality. With the emphasis on telerehabilitation stronger than ever during the COVID-19 pandemic, future research on healthcare utilization should explore differences in telerehabilitation services, and whether these are being optimized for both rural and urban individuals.
Data availability
The data analyzed during this study is available for access from the corresponding author upon appropriate request. Data sharing will be regulated via the RHSCIR Data Use and Disclosure Policy.
References
World Health Organization. International classification of functioning, disability and health: ICF. 2001.
Bloemen-Vrencken JHA, De Witte LP, Post MWM. Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation. Spinal Cord. 2005;43:462–75.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42:513–25.
LaVela SL, Smith B, Weaver FM, Miskevics SA. Geographical proximity and health care utilization in veterans with SCI&D in the USA. Soc Sci Med. 2004;59:2387–99.
Gary KW, Cao Y, Burns SP, McDonald SD, Krause JS. Employment, health outcomes, and life satisfaction after spinal cord injury: comparison of veterans and nonveterans. Spinal Cord. 2020;58:3–10.
Glennie RA, Batke J, Fallah N, Cheng CL, Rivers CS, Noonan VK, et al. Rural and urban living in persons with spinal cord injury and comparing environmental barriers, their health, and quality-of-life outcomes. J Neurotrauma. 2017;34:2877–82.
Barclay L, McDonald R, Lentin P. Social and community participation following spinal cord injury: a critical review. Int J Rehabil Res. 2015;38:1–19.
Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1793–803.
Cobb JE, Leblond J, Dumont FS, Noreau L. Perceived influence of intrinsic/extrinsic factors on participation in life activities after spinal cord injury. Disabil Health J 2018;11:583–90.
Cao Y, Walker EA, Krause JS. Environmental barriers and subjective health among people with chronic spinal cord injury: a cohort study. J Spinal Cord Med. 2015;38:526–31.
Reinhardt JD, Middleton J, Bökel A, Kovindha A, Kyriakides A, Hajjioui A, et al. Environmental barriers experienced by people with spinal cord injury across 22 countries: results from a cross-sectional survey. Arch Phys Med Rehabil. 2020;101:2144–56.
Noonan VK, Kwon BK, Soril L, Fehlings MG, Hurlbert RJ, Townson A, et al. The Rick Hansen Spinal Cord Injury Registry (RHSCIR): a national patient-registry. Spinal Cord. 2012;50:22–27.
Noreau L, Cobb J, Bélanger LM, Dvorak MF, Leblond J, Noonan VK. Development and assessment of a community follow-up questionnaire for the Rick Hansen Spinal Cord Injury Registry. Arch Phys Med Rehabil. 2013;94:1753–65.
Canale TD, Cho H, Cheung WY. A population-based analysis of urban-rural disparities in advanced pancreatic cancer management and outcomes. Med Oncol. 2018;35:116.
Waring WP, Biering-Sorensen F, Burns S, Donovan W, Graves G, Jha A, et al. 2009 Review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med. 2010;33:346–52.
Whiteneck GG, Harrison-Felix CL, Mellick DC, Brooks CA, Charlifue SB, Gerhart KA. Quantifying environmental factors: a measure of physical, attitudinal, service, productivity, and policy barriers. Arch Phys Med Rehabil. 2004;85:1324–35.
Forchheimer M, McAweene MTD. Use of the SF-36 among persons with spinal cord injury. Am J Phys Med Rehabil. 2004;83:390–5.
Post MW, Van Leeuwen CM, Van Koppenhagen CF, De Groot S. Validity of the life satisfaction questions, the life satisfaction questionnaire, and the satisfaction with life scale in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93:1832–7.
Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM-spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6.
Goodridge D, Rogers M, Klassen L, Jeffery B, Knox K, Rohatinsky N, et al. Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil. 2015;37:1401–10.
Botticello AL, Chen Y, Cao Y, Tulsky DS. Do communities matter after rehabilitation? The effect of socioeconomic and urban stratification on well-being after spinal cord injury. Arch Phys Med Rehabil. 2011;92:464–71.
Helliwell JF, Shiplett H, Barrington-Leigh CP. How happy are your neighbours? Variation in life satisfaction among 1200 Canadian neighbourhoods and communities. PLoS One. 2019;14:e0210091.
Bell N, Kidanie T, Cai B, Krause JS. Geographic variation in outpatient health care service utilization after spinal cord injury. Arch Phys Med Rehabil. 2017;98:341–6.
Ronca E, Scheel-Sailer A, Koch HG, Essig S, Brach M, Munzel N, Gemperli A. Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J Spinal Cord Med. 2020;43:111–21.
Guilcher SJT, Munce SEP, Couris CM, Fung K, Craven BC, Verrier M, et al. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord. 2010;48:45–50.
Munce SEP, Guilcher SJT, Couris CM, Fung K, Craven BC, Verrier M, et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord. 2009;47:470–6.
Holliday I, Kurl S. Angus Reid Institute. Disability in Canada: does closing the accessibility gap literally start from the ground up? http://angusreid.org/wp-content/uploads/2016/12/2016.12.02-RHF-disability.pdf. 2016. Accessed 10 Feb 2022.
Borisoff JF, Ripat J, Chan F. Seasonal patterns of community participation and mobility of wheelchair users over an entire year. Arch Phy Med Rehabil. 2018;99:1553–60.
Acknowledgements
We would like to acknowledge those individuals who consented to participate in this study. The authors would also like to thank the RHSCIR network and all the participating local RHSCIR sites: Nova Scotia Rehabilitation Centre, QEII Health Sciences Centre, Saint John Regional Hospital, Stan Cassidy Centre for Rehabilitation, St. John’s Health Sciences Centre, and L.A. Miller Rehabilitation Centre. Data for this research/project was collected using the Global Research Platform http://www.rhigrp.net/. Neurology data for this research/project was cleaned using the Praxis ISNCSCI Algorithm http://www.isncscialgorithm.com/. The Rick Hansen Spinal Cord Injury Registry and this work are supported by funding from the Praxis Spinal Cord Institute, Health Canada, Pacific Economic Development Canada (PacifiCan), and the Governments of Alberta, British Columbia, Manitoba, and Ontario. For more information about RHSCIR, please visit www.praxisinstitute.org. Authors DW, MC, CLC, and SH are employed by Praxis. All participating RHSCIR centers receive funding for general local data collection. No additional funding was received to prepare this manuscript.
Author information
Authors and Affiliations
Contributions
AW, SM, PB, DW, MC, CLC, SH, CO, NA, AE, and SC helped designed the study. Authors DW, MC, CLC, SH conducted the data analysis. All authors contributed to the interpretation of the data. AW drafted the manuscript. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All participating RHSCIR centers have and maintain Research Ethics Board approval for collection and national sharing of research data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Whelan, A., McVeigh, S., Barker, P. et al. The effect of rurality and distance from care on health outcomes, environmental barriers, and healthcare utilization patterns in persons with traumatic spinal cord injury. Spinal Cord 61, 399–408 (2023). https://doi.org/10.1038/s41393-023-00898-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00898-y