Abstract
Study design
Prospective, multicenter, longitudinal cohort study.
Objectives
To describe female-male differences in first-line urological management during spinal cord injury (SCI) rehabilitation.
Setting
Inpatient specialized post-acute SCI rehabilitation in Switzerland.
Methods
Data on bladder storage medication (antimuscarinic and beta-3 agonist) use, suprapubic catheter placement, demographic and SCI characteristics was collected within 40 days of SCI and at rehabilitation discharge from May 2013–September 2021. Prevalence and indicators of bladder storage medication and suprapubic catheter use at discharge were investigated with sex-stratified descriptive and logistic regression analyses.
Results
In 748 patients (219 females, 29%), bladder storage medication use at discharge had a prevalence of 24% (95% CI: 18–29%) for females and 30% (95% CI: 26–34%) for males and was indicated by cervical AIS grade A, B, C and traumatic SCI in both sexes. Thoracic AIS grade A, B, C SCI (males), and lumbar/sacral AIS grade A, B, C SCI (females) predicted higher odds of bladder storage medication use (SCI characteristic*sex interaction, p < 0.01). Prevalence of suprapubic catheter use at discharge was 22% (95% CI: 17–28%) for females and 17% (95% CI: 14–20%) for males. Suprapubic catheter use was indicated by cervical AIS grade A, B, C SCI, and age >60 in both sexes. Females with thoracic grade A, B, C SCI tended to have higher odds of suprapubic catheter use (SCI characteristic*sex interaction, p = 0.013).
Conclusions
We identified sex differences in urological management especially in persons with AIS grade C or higher sub-cervical SCI. There is scope for well-powered, female-specific research in SCI in order to understand the underlying mechanisms and support patient-tailored management.
Similar content being viewed by others
Introduction
Women account for a growing proportion of the persons with acute spinal cord injury (SCI), especially in the oldest age groups [1,2,3]. In elderly populations, some of the dominant causes of SCI include low-level falls leading to traumatic SCI (TSCI) [1, 3, 4], and degenerative processes and diseases leading to non-traumatic SCI (NTSCI) [2, 3]. Although gender-specific considerations should be incorporated into most aspects of SCI management [5], they may particularly concern the urological domain, given the substantial physiological and anatomical differences in the lower urinary tract (LUT) between sexes [6]. Indeed, the neuro-urology guidelines do make female-specific recommendations in the cases where relevant evidence is present [7], but to this point, much of the urological research in SCI has been conducted in predominantly male populations [8], that are also often small and heterogeneous [9]. Following, when optimizing urological management, the transferability of majority-male results to the female SCI population is uncertain. The body of evidence addressing sex differences is even further limited in the context of management during inpatient post-acute SCI rehabilitation.
Two critical management issues in the context of SCI rehabilitation [10], potentially requiring a female-specific tailoring, include the use of antimuscarinic medications for neurogenic detrusor overactivity (NDO) and storage symptoms, as well as catheterization to promote complete bladder emptying. There is high-level evidence recommending the use of antimuscarinic medications as first-line treatment for patients with NDO [11, 12], but muscarinic receptor expression in the LUT has been shown to differ between the sexes, potentially resulting in differential responses to medications, and divergent management outcomes [13]. The evidence base regarding catheterization is more developed, there are reports that females are at higher risk than males for using an indwelling catheter at discharge from rehabilitation, as opposed to intermittent self-catheterization [14, 15]. The objective of this study is to describe differences in first-line LUT management between females and males during SCI rehabilitation in order to evaluate the scope for sex-specific research in neuro-urological management. The specific aims include: (1) to describe the prevalence of bladder storage medication and bladder emptying method stratified according to sex and SCI characteristics; (2) to evaluate whether predictors of bladder storage medication and suprapubic catheter use differ between sexes.
Methods
Study design, setting, and participants
This study utilizes data from the prospective, longitudinal Swiss Spinal Cord Injury (SwiSCI) Inception Cohort, reported in detail elsewhere [16]. Participants were Swiss residents, age 16 or older, undergoing inpatient specialized post-acute SCI rehabilitation at one of the four specialized SCI centers in Switzerland from May 2013 to September 2021. Exclusion criteria were: acute SCI in the context of palliative care, SCI attributable to a congenital condition, or presence of a neurodegenerative disorder. During the study period, 49% consented to undergoing SwiSCI-specific data collection (study data set, SDS), 42% of the participants consented only to use of routine data from the clinical record, and 9% did not consent to any data collection. Data collection occurred at up to four time points during the inpatient rehabilitation stay: at discharge (0–15 days before discharge), and 28 days (time frame: 16–40 days), 84 days (70–98 days), 168 days (150–186 days) after SCI. This study focuses on the patient status at discharge. For the current study, patients with missing information on SCI characteristics (completeness, neurological level) were excluded (n = 9), as were persons who died during rehabilitation or shortly after discharge to a hospital (n = 12), as well as one person admitted for a second SCI. Ethical approvals were obtained from all responsible ethics committees (Ethics Committee Northwest and Central Switzerland (EKNZ) 100/13, Ethics Committee Lucerne (LU) 12090; Ethics Committee Zurich (KEK Zurich) 2013-0249; Ethics Committee Valais (CE Valais) 032/13).
Neuro-urological management
All participating rehabilitation centers adopt a patient-tailored bladder management approach that is based on the European Urology Association Guidelines on Neuro-Urology [7]. In brief, the therapeutic strategy aims to preserve and promote both upper and LUT function, and treatment decisions are based on urodynamic investigation. Indications for bladder storage medication include: presence of NDO, urinary incontinence episodes resulting from NDO, and low bladder capacity. Refractory bladder storage symptoms are treated with intradetrusor onabotulinumtoxinA injections as a second-line treatment. Intermittent self-catheterization is the preferred bladder emptying method for persons who are unable to achieve complete bladder emptying via spontaneous voiding. Suprapubic catheters are utilized when intermittent self-catheterization is not feasible—especially in persons with upper extremity impairments [7, 15, 17].
Study measures
Urological management
Urological management data was extracted from the clinical record for SDS participants within 40 days after SCI and at discharge from rehabilitation, based on the International Spinal Cord Society (ISCoS) LUT Function Basic Data Set [18]. This data set contains information on LUT surgeries, including the last performed dates for suprapubic catheter insertion and intradetrusor onabotulinumtoxinA injections, as well as information on bladder emptying method. Data on medication usage were extracted from the clinical record reflecting status during a 1-week period at each data collection time point. Based on expert input, use of bladder storage medication was defined as any of the following medications: the antimuscarinics oxybutynin, tolterodine, solifenacin, trospium chloride, darifenacin, fesoterodine, and the beta-3 agonist mirabegron.
Routine clinical data, neurological assessment and functional independence
Routine data extracted from the clinical record included: demographic information (sex, age), characteristics of the rehabilitation stay (rehabilitation center, dates of admission and discharge), and SCI history (etiology—TSCI or NTSCI, date of SCI diagnosis). Neurological condition was evaluated using the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) assessment (neurological level, American Spinal Injury Association Impairment Scale (AIS) Grade) [19]. Functional independence was assessed using the Spinal Cord Independence Measure III [20], and was used here to provide contextual information regarding female-male differences at baseline.
Modeling considerations
As this study was targeting population-level inference on the role of biological sex as an indicator of urological management, the models for both bladder storage medication and suprapubic catheter use included the potential predictors age, neurological level, AIS grade, SCI etiology, and rehabilitation center.
Statistical analyses
All continuous variables were tested for normality and found to have non-normal distributions, so non-parametric tests (Kruskal–Wallis) were used in univariable baseline descriptions of the study population. Chi-squared tests were applied to categorical variables in the corresponding analyses. Binomial exact confidence intervals (CIs) are reported with proportions. Sampling bias was evaluated, and inverse probability weights (IPWs) were used to correct for differences in study participation identified between the SDS and the source population in all regression analyses (Supplement 1). Logistic regression analyses stratified on sex were used to generate weighted prevalence predictions for the use of bladder storage medication and suprapubic catheters at the time of discharge, as well as to identify the predictors of the respective outcomes. Models including both sexes were then run to confirm the findings of the stratified analyses. Age was divided into categories according to ISCoS [21] (16–30, 31–45, 46–60, 61–75, 76 or older). A combined variable for neurological level and AIS grade, “SCI severity” was employed: Cervical AIS A, B, C; Thoracic AIS A, B, C; Lumbar/Sacral AIS A, B, C, all AIS D/E as model testing indicated that it was the categorization that best accounted for interactions between AIS grade and neurological level, and additionally was in line with ISCoS reporting recommendations [21]. When age was included as a continuous variable, linearity was tested using multivariable fractional polynomial models, and a variable with a cubic transformation was employed in the final analysis.
Because SCI characteristics have been shown to stabilize during the course of the first year [22], for descriptive and logistic regression analyses, missing data from the baseline ISNCSCI assessment (n = 48, 6%) were addressed using a next observation carried backwards approach. Likewise, for cases missing ISNCSCI data at discharge (n = 52, 7%), a last observation carried forward approach was used. In variables with more than two categories, significance testing was first performed via global Wald tests, and in case there was a joint effect of all categories, post hoc Wald tests were performed to investigate the relationships between each set of categories. All p values based on post hoc testing presented here are Bonferroni-adjusted to account for multiple testing. Analyses were performed in Stata statistical software, version 16.1 for Windows (StataCorp LLC: College Station, TX, USA).
Results
Out of the 748 participants admitted to rehabilitation for acute SCI from May 2013 to September 2021, 219 (29%) were female. Females were more likely to have an NTSCI, a shorter length of stay, as well as higher functional independence scores than men, 61% of females had an AIS D SCI as opposed to 53% of males. There were also differences in sex distributions between centers (Table 1). A relationship between age and sex was not identified when age was analyzed as a continuous variable. Sampling bias was identified with multivariable logistic regression analysis, the SDS population tended to have a younger age, lower proportion of females, and earlier admission to rehabilitation. Additionally, participation varied among rehabilitation centers (Supplement 1). The median (quartile 1 (Q1)–quartile 3 (Q3)) time to discharge from rehabilitation was 159 (93–224) days, or 5.3 (3.1–7.5) months after SCI.
Bladder storage medications were used by 28% (95% CI: 25–31%) (n = 204) of the population at discharge (2% missing data at discharge) (Table S2), 25% of whom (n = 52) used mirabegron. In both sexes, the majority of the persons with a lumbar SCI that used a bladder storage medication had a neurological level of L1 or L2, and bladder storage medication was not used at all in persons with sacral SCI. Further information on bladder storage medication use during rehabilitation is provided in the Supplementary Material (Supplement 2, Table S2). A total of 21 patients (3% of the population), had intradetrusor onabotulinumtoxinA injections before being discharged from rehabilitation, and 13 of these patients were using bladder storage medications at the time of discharge.
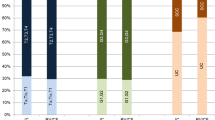
At discharge, females (23%, 95% CI: 17–29%) tended to use bladder storage medication less frequently than males (30%, 95% CI: 26–34%) in sex-stratified univariable analysis (Table S2). See Fig. 1 for the distribution of bladder storage medication use stratified according to sex and SCI characteristics. The adjusted weighted prevalence of bladder storage medication use in females was 24% (95% CI: 18–29%) and in males it was 30% (95% CI: 26–34%). SCI severity was a predictor of bladder storage medication use in both females and males (global p < 0.01, both groups) in stratified regression analyses. Additionally, for both groups SCI etiology was a potential predictor of bladder storage medication usage at discharge, the adjusted odds ratio (aOR) for NTSCI vs. TSCI for females: 0.50 (95% CI: 0.22–1.12); for males: aOR NTSCI 0.40 (95% CI: 0.24–0.66). In both sexes, cervical AIS grade A, B, C SCI was a potential predictor of bladder storage medication use, aOR vs. AIS D/E grades for females: aOR 6.91 (95% CI: 1.40–34.01, post hoc p = 0.14); for males: aOR 4.59 (95% CI: 2.51–8.40, post hoc p < 0.0001) (Table 2). However, in females, odds of bladder storage medication use at discharge were also higher in the lumbar/sacral A, B, C group (aOR 4.82 (95% CI: 1.69–13.77, post hoc p = 0.018), but not in the thoracic group. A post hoc test comparing cervical and lumbar/sacral AIS A, B, C SCI with thoracic AIS A, B, C and all AIS D indicated that these two groupings differed from each other p < 0.0001. In males, thoracic AIS A, B, C SCI aOR: 3.75 (95% CI: 2.26–6.22, post hoc p < 0.0001) was also a predictor of bladder storage medication use, with a post hoc test comparing cervical and thoracic AIS A, B, C SCI to the lumbar/sacral and all D groups indicating that the two categories differed from each other, p < 0.0001. In an analysis of bladder storage medication use combining both females and males the interaction between sex and SCI severity was statistically significant (p < 0.01), further supporting the findings from the stratified analyses (Fig. 2).
When SCI characteristics were not available, they were taken from the closest available time point after the very acute period. Other bladder emptying method refers to reflex triggering, bladder expression, and urinary diversion. AIS American Spinal Injury Association (ASIA) Impairment Scale, C cervical, IC intermittent catheter, IDW indwelling catheter L lumbar, S sacral, T thoracic.
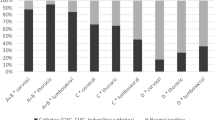
Predictions are from a logistic regression analysis with use of bladder storage medication at discharge coded as “1”. This model included females and males together with an interaction between sex and SCI severity (p < 0.01), and was also was adjusted for age, SCI etiology and rehabilitation center.
The most common bladder emptying method at discharge was spontaneous voiding (42%, 95% CI: 39–46%), followed by intermittent catheterization (37%, 95% CI: 34–41%) (4% missing bladder emptying data at discharge). Prevalence of suprapubic catheter use at discharge was 16% (95% CI: 13–19%) (n = 115) (Table S3). The overall distribution of bladder emptying method at discharge stratified according to sex and SCI characteristics is visualized in Fig. 1. Further information on suprapubic catheter use during rehabilitation is available in the Supplementary Material (Supplement 2, Table S3). In sex-stratified univariable analysis, 19% (95% CI: 14–25%) of females, and 15% (95% CI: 12–18%) of males used suprapubic catheters. Females with cervical (83%, 95% CI: 52–98) and thoracic (29%, 95% CI: 14–48) AIS grade A, B, C SCI, tended to use suprapubic catheters more frequently at discharge than males (cervical 48%, 95% CI: 35–61; thoracic 7%, 95% CI: 3–14) (Table S3). In adjusted analyses stratified on sex, females had a weighted prevalence of suprapubic catheter use of 22% (95% CI: 17–28%), while in males the weighted prevalence was 17% (95% CI: 14–20%). Age >60 (post hoc p < 0.001, both sexes), and cervical AIS A, B, C SCI (post hoc p < 0.001, both sexes) were predictors of suprapubic catheter use in both females and males (Table 3). Females with a thoracic AIS grade A, B, C SCI also had higher odds of suprapubic catheter use compared to persons with AIS D SCI, aOR 5.11 (95% CI: 1.27–20.62, post hoc p = 0.12). In agreement with the findings of the sex-stratified analyses, there was an interaction between sex and SCI severity in combined analysis, p = 0.013. Predicted probabilities of suprapubic catheter use according to sex, age, and SCI severity are shown in Fig. 3. At discharge, 44 persons (38%) who used a suprapubic catheter also used bladder storage medication, 30 of whom (68%) had a cervical SCI. Sixteen of the dual bladder storage medication and suprapubic catheter users were female, of whom 9 (56%) had a cervical SCI.
Predictions are from a logistic regression analysis with use of a suprapubic catheter at discharge coded as “1”. This model included females and males together with age as a continuous variable that was transformed to account for non-linearity, and was also was adjusted for rehabilitation center and SCI etiology. For readability, female and male predictions were graphed separately. The interaction between sex, SCI severity and transformed age is statistically significant (p < 0.0001). The color version of this figure (available online) also contains 95% confidence intervals.
Discussion
In this study we examined the sex-specific prevalence and indicators of bladder storage medication and suprapubic catheters use during SCI rehabilitation. Cervical AIS grade A, B, C SCI and TSCI were predictors of bladder storage medication use in both females and males, however thoracic AIS grade A, B, C SCI was only a predictor for males, and lumbar AIS grade A, B, C SCI was only a predictor for females. Age >60 and cervical AIS grade A, B, C SCI were predictors of suprapubic catheter use in both sexes, while thoracic AIS grade A, B, C SCI was tentatively an additional predictor of suprapubic catheter use in females.
The current results indicate that female-male differences in the use of bladder storage medication during SCI rehabilitation mainly occur in relation to SCI characteristics despite substantial sex differences in the anatomy and physiology of the LUT, such as shorter urethral length in females, presence of the prostate in males, as well as differing pelvic floor physiology and distribution of muscarinic receptor subtypes [13]. The tendency toward females using less bladder storage medication in unadjusted analyses might be at least partially attributable to the fact that the female population also had a higher prevalence of NTSCI. To the best of our knowledge, there are no existing studies investigating the relationship between sex and the usage of bladder storage medication during the rehabilitation period to serve as a basis for comparison. The evidence regarding differences in the prevalence of bladder storage medication use in females and males in the community setting is also scarce, although there was one study that did not find female-male differences in a population where 63% of the participants used antimuscarinics [23]. Based on the proposed mechanism for NDO, we had expected that the prevalence of bladder storage medication use might be lower in the group with lumbar SCI compared to groups with higher neurological levels, as in the lumbar groups the sympathetic innervation that relaxes the bladder could be at least partially spared [24, 25]. While this pattern was evident in the male population at the time of discharge, it was not observed in females. One possible explanation is that suprapubic catheter use could be reducing some of the need for bladder storage medication in females with thoracic AIS grade A, B, C SCI [14], but this hypothesis could not be tested with the available information in this data set. In order to understand the factors underlying the current results, further research which utilizes information from urodynamics investigation and also includes a large female population is necessary.
Reports from the literature have indicated that females are expected to have a higher prevalence of suprapubic catheter use than males [14, 15, 17], and this trend could also be observed in the present population, especially in the younger age groups. Previously proposed explanations for the higher rates of suprapubic catheter insertion in women include less straightforward access to the urethra, transferring difficulties [14, 15], which along with other factors, could lead to a suprapubic catheter allowing women to have more independence [8]. In a community setting, the time required for catheterization through the urethra tended to be substantially longer for a small sample of women who were overweight or who required caregiver support [26], indicating that the suprapubic catheter might be the more convenient option for some [8]. A final factor identified in the community setting, “lack of sitting balance” was more commonly cited by females than males as an explanation of inability to perform intermittent catheterization independently [27], and this might also provide a suggestion as to why thoracic AIS grade A,B,C SCI is tentatively a female-specific predictor of suprapubic catheter use in the present study. As sitting balance represents a potentially modifiable factor, this would also represent a route for further intervention if this relationship can be definitively established. The other risk factors identified in both sexes, in particular older age [3] and cervical SCI also are in agreement with the existing body of evidence [14, 15].
Secondary findings of this study include additional factors associated with bladder storage medication and suprapubic catheter use in both sexes. The relationship between SCI etiology and antimuscarinic use has not been directly addressed before in the literature. Our previous findings from this cohort have shown that there is a higher comorbidity load in the NTSCI population [10], so concerns about interactions and side effects such as constipation and potential cognitive impact, might explain some of the hesitancy to prescribe bladder storage medication to persons with NTSCI [12, 28]. To fully investigate this hypothesis, as for other domains in the SCI field [9], further investigation is needed, in the form of well-designed population-based cohort studies capturing the full spectrum of comorbidities before SCI as well as secondary health conditions in this population.
A strength of this descriptive study is its representativeness, as it utilizes data from a population-based cohort that covers all of the specialized post-acute SCI rehabilitation centers in Switzerland. Furthermore, the use of inverse probability weighting minimized the potential for sampling bias. The present epidemiological inference may well apply to other high-income settings, although it remains to be seen whether local policy differences regarding length of rehabilitation stay and thereby the time to discharge affect the transferability of these study findings. Differences in referral patterns between countries and their respective healthcare systems might also affect the applicability of results to other settings. In the context of TSCI in Switzerland, it has previously been shown that women, the elderly and persons with lumbar and sacral lesions are less likely to be enrolled by the SwiSCI cohort [29]. This study is also performed in a population with a comparatively large number of female participants, making it well-powered for the SCI context, nevertheless, the CIs in adjusted analyses in the oldest age groups, females with cervical AIS grade A, B, C SCI, and both sexes with lumbar and sacral A, B, C SCI are still quite wide, indicating that there is still a relatively high degree of uncertainty in these groups. Further, although missing data in the predictor variables (SCI characteristics) was addressed by utilizing information from other time points, the relationships identified here could be subject to bias if there is a relationship between the predictor variables and missingness of data in the outcome variables. Additional limitations to the potential of this data set to support analyses targeted at causal inference or evaluation of treatment effectiveness included lack of parameters regarding cognitive function, patient motivation, diagnostic examinations (i.e., urodynamics investigation), and pre-existing urological conditions such as pelvic floor dysfunction or prostatic outlet obstruction.
Conclusions
Our findings indicate a scope for female-specific research, in particular to understand potential mechanisms underlying the management differences between sexes in persons with AIS grade C or higher sub-cervical SCI. Although there may be considerable clinical expertise in how to manage NLUTD in women with SCI, this information needs to be systematically documented. A well-powered female-specific study, probably requiring an international effort, could help to identify potential targets of intervention and also to support patient-tailored management and female-specific guideline recommendations.
Data availability
Owing to our commitment to SwiSCI study participants and their privacy, data sets generated during the current study are not made publicly available. The SwiSCI study center requires, on behalf of the SwiSCI Study Group, contact prior to any planned data usage (contact@swisci.ch).
References
Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 2014;52:97–109.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M. Effects on age on spinal cord lesion patients’ rehabilitation. Spinal Cord. 2003;41:457–64.
Chamberlain JD, Deriaz O, Hund-Georgiadis M, Meier S, Scheel-Sailer A, Schubert M, et al. Epidemiology and contemporary risk profile of traumatic spinal cord injury in Switzerland. Inj Epidemiol. 2015;2:28.
Slocum C, Halloran M, Unser C. A primary care provider’s guide to clinical needs of women with spinal cord injury. Top Spinal Cord Inj Rehabil. 2020;26:166–71.
Abelson B, Sun D, Que L, Nebel RA, Baker D, Popiel P, et al. Sex differences in lower urinary tract biology and physiology. Biol Sex Differ. 2018;9:45.
Groen J, Pannek J, Castro Diaz D, Del Popolo G, Gross T, Hamid R, et al. Summary of European Association of Urology (EAU) guidelines on neuro-urology. Eur Urol. 2016;69:324–33.
Teplitsky S, Murphy A, Shenot PJ. Knowledge gaps in urologic care of female spinal cord injury patients. Curr Urol Rep. 2019;20:21.
Dvorak MF, Cheng CL, Fallah N, Santos A, Atkins D, Humphreys S, et al. Spinal cord injury clinical registries: improving care across the SCI care continuum by identifying knowledge gaps. J Neurotrauma. 2017;34:2924–33.
Anderson CE, Birkhäuser V, Jordan X, Liechti MD, Luca E, Möhr S, et al. Urological management at discharge from acute spinal cord injury rehabilitation: a descriptive analysis from a population-based prospective cohort. Eur Urol Open Sci. 2022;38:1–9.
Welk B, Schneider MP, Thavaseelan J, Traini LR, Curt A, Kessler TM, et al. Early urological care of patients with spinal cord injury. World J Urol. 2018;36:1537–44.
Madersbacher H, Murtz G, Stohrer M. Neurogenic detrusor overactivity in adults: a review on efficacy, tolerability and safety of oral antimuscarinics. Spinal Cord. 2013;51:432–41.
Hartigan SM, Dmochowski RR. Gender specific pharmacokinetic and pharmacodynamic considerations for antimuscarinic drugs for overactive bladder treatment. Expert Opin Drug Metab Toxicol. 2020;16:103–10.
Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ, et al. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010;184:213–7.
Zlatev DV, Shem K, Elliott CS. How many spinal cord injury patients can catheterize their own bladder? The epidemiology of upper extremity function as it affects bladder management. Spinal Cord. 2016;54:287–91.
Fekete C, Gurtner B, Kunz S, Gemperli A, Gmünder HP, Hund-Georgiadis M, et al. Inception cohort of the Swiss Spinal Cord Injury Cohort Study (SwiSCI): design, participant characteristics, response rates and non-response. J Rehabil Med. 2021;53:jrm00159.
Krebs J, Wöllner J, Rademacher F, Pannek J. Bladder management in individuals with spinal cord injury or disease during and after primary rehabilitation: a retrospective cohort study. World J Urol. 2022;40:1737–42.
Biering-Sorensen F, Kennelly M, Kessler TM, Linsenmeyer T, Pannek J, Vogel L, et al. International spinal cord injury lower urinary tract function basic data set (version 2.0). Spinal Cord Ser Cases. 2018;4:60.
ASI Association. International standards for neurological classification of spinal cord injury (ISNCSCI). Richmond, VA, USA: American Spinal Injury Association; 2019.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
DeVivo MJ, Biering-Sorensen F, New P, Chen Y. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord. 2011;49:596–9.
Zariffa J, Kramer JL, Fawcett JW, Lammertse DP, Blight AR, Guest J, et al. Characterization of neurological recovery following traumatic sensorimotor complete thoracic spinal cord injury. Spinal Cord. 2011;49:463–71.
Yıldız N, Akkoç Y, Erhan B, Gündüz B, Yılmaz B, Alaca R, et al. Neurogenic bladder in patients with traumatic spinal cord injury: treatment and follow-up. Spinal Cord. 2014;52:462–7.
Miyazato M, Kadekawa K, Kitta T, Wada N, Shimizu N, de Groat WC, et al. New frontiers of basic science research in neurogenic lower urinary tract dysfunction. Urol Clin North Am. 2017;44:491–505.
Sahai A, Cortes E, Seth J, Khan MS, Panicker J, Kelleher C, et al. Neurogenic detrusor overactivity in patients with spinal cord injury: evaluation and management. Curr Urol Rep. 2011;12:404–12.
Velaer KN, Welk B, Ginsberg D, Myers J, Shem K, Elliott C, et al. Time burden of bladder management in individuals with spinal cord injury. Top Spinal Cord Inj Rehabil. 2021;27:83–91.
Yılmaz B, Akkoç Y, Alaca R, Erhan B, Gündüz B, Yıldız N, et al. Intermittent catheterization in patients with traumatic spinal cord injury: obstacles, worries, level of satisfaction. Spinal Cord. 2014;52:826–30.
Duong V, Iwamoto A, Pennycuff J, Kudish B, Iglesia C. A systematic review of neurocognitive dysfunction with overactive bladder medications. Int Urogynecol J. 2021;32:2693–702.
Chamberlain JD, Ronca E, Brinkhof MW. Estimating the incidence of traumatic spinal cord injuries in Switzerland: Using administrative data to identify potential coverage error in a cohort study. Swiss Med Wkly. 2017;147:w14430.
Acknowledgements
First of all, we thank all of the SwiSCI study participants for their invaluable contribution to this research. Additionally, we thank the SwiSCI Steering Committee with its members Xavier Jordan, Fabienne Reynard (Clinique Romande de Réadaptation, Sion); Michael Baumberger, NN (Swiss Paraplegic Center, Nottwil); Armin Curt, Martin Schubert (Balgrist University Hospital, Zürich); Margret Hund-Georgiadis, NN (REHAB Basel, Basel); Laurent Prince (Swiss Paraplegic Association, Nottwil); Heidi Hanselmann (Swiss Paraplegic Foundation, Nottwil); Daniel Joggi (Representative of persons with SCI); Mirjana Bosnjakovic (Parahelp, Nottwil); Mirjam Brach, Gerold Stucki (Swiss Paraplegic Research, Nottwil); Armin Gemperli (SwiSCI Coordination Group at Swiss Paraplegic Research, Nottwil).
Funding
This work was financially supported by the Swiss National Science Foundation (SNSF, 33IC30_179644). The funding body did not play a role in the design of the study, the analysis and interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
CEA, VB, TMK, and MWGB were responsible for the design and conceptualization of the study. Statistical analysis was performed by CEA and MWGB. CEA, VB, MDL, XJ, EL, SM, JP, TMK, and MWGB analyzed and interpreted the data. The manuscript was drafted by CEA, with the support of VB, TMK, and MWGB. All authors provided critical feedback on the manuscript regarding important intellectual content, and provided their approval on the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was granted by all responsible ethics committees: Ethics Committee Northwest and Central Switzerland (EKNZ) 100/13, Ethics Committee Lucerne (LU) 12090; Ethics Committee Zurich (KEK Zurich) 2013-0249; Ethics Committee Valais (CE Valais) 032/13). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anderson, C.E., Birkhäuser, V., Liechti, M.D. et al. Sex differences in urological management during spinal cord injury rehabilitation: results from a prospective multicenter longitudinal cohort study. Spinal Cord 61, 43–50 (2023). https://doi.org/10.1038/s41393-022-00860-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00860-4