Abstract
Study design
Randomized-controlled trial (RCT) with immediate intervention (IMM) and wait-list control (WLC) groups; WLC participants received the intervention during delivery to subsequent cohorts.
Objectives
Investigate the effectiveness and feasibility of a virtually-delivered exercise intervention.
Setting
Home and community.
Methods
A total of 168 middle-aged (49.6 [12.3] years old) men (57%) and women (43%) who lived an average 15.5 (12.3) years with spinal cord injury (SCI) participated. The 16-week program provides users (a) website access with exercise information, resources, and 16 skill-building modules; (b) virtual 60-minute, group-based weekly meetings; and (c) a starter package of exercise equipment. Primary outcomes included subjective physical activity (IPAQ) and objective exercise (Polar A300 wrist-based activity monitor and H7 heart rate strap). Secondary outcomes included fitness indices during a maximal arm crank test, plus self-reported exercise barriers, exercise self-efficacy, and goal-directed thinking.
Results
RCT results indicate significant between group differences in participants’ self-reported weekly time spent in vigorous-intensity PA and goal directed thinking but not for fitness changes. Data combined for IMM and WLC participants from Polar monitoring show participants performed 150 min per week of aerobic exercise plus reported significantly greater time spent in moderate-PA, vigorous-PA, self-efficacy for exercise and nutrition, goal directed thinking, and exercise barriers. Oxygen uptake (V̇O2 peak) and power output (watts max) were the only physiologic measures to demonstrate significant change, with a moderate effect size.
Conclusion
This virtually-delivered program offers a promising approach to increase exercise among those with SCI and may help participants perceive fewer motivational barriers and greater self-efficacy.
Similar content being viewed by others
Rehabilitation professionals have been encouraged [1] to include people with spinal cord injury (SCI) [2,3,4] in the exercise is medicine (EIM) initiative [5, 6] which encourages healthcare professionals to assess physical activity a 5th vital sign [1], along with body temperature, pulse rate, respiration rate, and blood pressure. This approach is in line with 2018 clinical practice guidelines, which identify the heightened risk people with SCI face for cardiometabolic disease [7] and advocate for aggressively promoting lifestyle change.
Physical activity (PA) yields positive effects on fitness, muscle strength, body composition, function, psychological well-being, and quality of life of those with SCI [8,9,10,11,12], yet people with SCI have lower activity levels than those without disability and other disability groups [13, 14]. Studies have examined various approaches to promote home and community-based PA among those with SCI, yet the growing evidence base [15,16,17,18,19,20,21,22,23,24,25] offers limited support for specific strategies or approaches. The paragraphs below summarize this evidence.
In-person and telephone-based programs
Several randomized controlled trials (RCT) have tested multi-component strategies delivered telephonically to promote PA over shorter (6–10 weeks [19, 20, 25], and longer (6–9 months, 23, 24) durations. Strategies include setting goals and self-monitoring, developing a behavioral contract and using rewards [25], providing home exercise equipment [17, 21, 22], staff support [19, 21, 22, 26], and addressing plans to manage barriers [20]. While all increased PA, better outcomes were observed among those provided greater exercise support (equipment [17, 21, 22] and staff support [17, 21, 22, 25]) or paired goal setting [19, 20] with plans to manage barriers [20]. Ma and colleagues reported robust outcomes among participants enrolled in an 8-week, theory-based intervention program [25] that delivered weekly, one-on-one coaching sessions in a flexible manner (in person, Skype, or by phone) and incorporated various behavior change techniques. Participants (n = 14) attended 100% of the weekly sessions; they reported an average increase of 222 weekly minutes in moderate and vigorous PA plus demonstrated significantly improved oxygen uptake (a relative increase of 11.9%) after 8 weeks.
Online programs
Investigators have examined using online platforms over 6–24 weeks, with varied outcomes. An initial feasibility study [27] indicated SCI participants achieved 100% adherence performing 24 home exercise sessions over 8 weeks, yet a subsequent larger trial [24] reported substantially lower adherence. Two features differed between the trials that potentially impacted uptake. Though everyone received a tablet with a custom-designed app that disseminated weekly exercise videos, participants in the larger trial did not receive home exercise equipment nor tele-coaching.
An 8 week RCT investigated a telehealth program where participants received 1-on-1 motivational counseling that included using self-regulation strategies [28, 29]. Participants completed 100% of the counseling sessions and reported larger PA increases than a control group in both leisure time PA (LTPA, absolute increase of 389 vs. 139 min/week) and moderate- and vigorous-intensity PA (MVPA, absolute increase of 140 vs. 88 min/week) at 10 weeks. SCI participants successfully used and positively rated a program where they were paired with a trained peer health coach for 6, 1-on-1 virtual sessions to discuss different health topics [30]. Participants completed 6 sessions over an average of 56 days and reported better health-related self-efficacy, resilience, and health literacy though behavior change was not measured.
Feature preferences
Online programs examined to date deliver some features requested by those with SCI. Pancer and colleagues [31] identified that individuals with SCI reported preferring an online platform that was colorful, easy to navigate, used clear language with pictures and videos, and allowed professionals and peers to interact. Other preferences respondents described were resources such as safety information, tutorials for home-based PA options, managing barriers to activity, inspiring content, risks and benefits, examples of others with SCI being active, plus self-regulation strategies.
The cumulative evidence is encouraging, including participants’ willingness to engage in telephone and online programs, although many yielded lower PA levels than the 150 min recommended by the Physical Activity Guidelines Committee [32, 33] and echoed by the Consortium on Spinal Cord Medicine [7] Notably, these guidelines are higher than SCI-specific evidence-based guidelines that recommend a minimum of 40–90 weekly minutes of moderate to vigorous aerobic exercise for fitness and cardiometabolic health benefits, respectively [34,35,36]. All previous studies provided 1-on-1 support, typically focused on establishing exercise goals, though participants’ reported peer coaches served as sources of support, encouragement, and accountability [30]. This study investigated the effectiveness (based on increased exercise, improved fitness, and better exercise perceptions) and feasibility (based on retention, engagement, and satisfaction) of Workout On Wheels internet intervention (WOWii), an online, evidence- and theory-based PA intervention consisting of 16 weekly modules and group-based virtual sessions.
Methods
Study design and participants
Study procedures were approved by the institution’s IRB (#016–093) and registered on Clinical Trials.gov (NCT03189095). Over 26 months (January 2017-September 2019) participants were recruited into one of 5 successively convened cohorts; for each cohort the PI randomized participants to the immediate intervention (IMM) or wait-list control (WLC) groups using a random number generator. To assure participant identities were concealed, the PI was not involved in screening and received a list containing only the study ID numbers to randomize participants after their screening, but before their baseline assessment. WLC participants were invited to participate in the WOWii program with the subsequent cohort. Exercise maintenance was assessed over 8 weeks following WOWii delivery.
Participants were recruited from the Dallas/Fort Worth (DFW) metropolitan area for the first 2 cohorts via posting fliers within 2 hospital outpatient physiatry offices, distributing fliers across durable medical supply vendors, and through several disability service organizations. Recruitment was expanded across the continental U.S. for cohorts 3 through 5. National recruitment occurred through a rehabilitation hospital in the south and national organizations who serve individuals with SCI, including the Paralyzed Veterans of America, United Spinal, and Facing Disability. Groups distributed emails, fliers, and posted information on their websites.
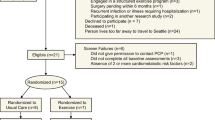
Eligibility criteria included participants: be at least 18 years old; have SCI ≥ 6 months and have sufficient arm movement to perform arm-based exercise; use a wheelchair for mobility ≥50% of the time; able to independently use a computer and navigate a website; have computer/internet access; receive physician signed approval to participate in the exercise study; and not currently meet national PA guidelines of 150 min of moderate-intensity physical activity, based on responses to the 6-item Behavioral Risk Factor Surveillance PA survey [37]. Exclusion criteria included: participating in the pilot study; unable to read the English language (Fig. 1, Consolidated Standards of Reporting Trials diagram [CONSORT]).
The Workout on Wheels internet intervention program
The 16-week WOWii program is founded upon Social Cognitive Theory (SCT) [38] and the Relapse Prevention (RP) model [39]. The four SCT core constructs formally embedded into the WOWii program are self-management, social support, the environment, and self-efficacy. WOWii was translated from a previous trial [40] delivered telephonically via 1-on-1 calls, and detailed elsewhere [41]. WOWii capitalizes upon reciprocal interactions between a person and their physical and social environment by supporting individuals to develop PA self-management skills in a group-based, virtual setting. The program is flexibly designed to meet participants where they are on their exercise journey and thus participants are instructed to progressively increase their weekly exercise based on their activity level at the program’s start. The WOWii program is comprised of 3 core components.
-
(1)
Virtual Intervention Delivery avoids transportation barriers to program participation. WOWii includes website content plus virtual, group-based meetings. The website contains informational resources (exercise and disability laws) plus houses 16 weekly modules on various self-management topics. A staff member leads weekly 60-minute, group-based virtual meetings over Zoom (convened over the noon hour and in the early evening, to maximize participants’ ability to attend) and participants are invited to join a closed Facebook group.
-
(2)
Support linkage. Participants receive support for their efforts to make behavioral changes by the WOWii study staff and other program participants during virtual meetings. The staff leader’s role is to (a) discuss the module topic, which addresses a different behavioral skill weekly and (b) facilitate members’ conversation. Conversations allow participants to support one another’s efforts and share knowledge.
-
(3)
Exercise equipment starter package is provided to each participant to reduce access barriers and enable affordable, home-based PA options. The package contains the three low-cost items: Thera-Bands®, a seated aerobics DVD (developed by the National Center on Health, Physical Activity, and Disability), and pedal exerciser with a tension knob (Drive Medical) to use as a table top arm ergometer.
Outcome measures
Study outcomes were obtained on all participants before, during, immediately following the 16-week WOWii program (4 months), and 2 months after completing WOWii (6 months) to assess maintenance. For the RCT design, WLC participants underwent testing twice before being invited to participate in the WOWii program. The second observation served as post-test data when compared to the IMM group in the RCT. Though for analyses when the IMM and WLC were combined as a group, the second test served as their baseline and their third assessment was then used as their post-test following the WOWii intervention. This study was designed as an effectiveness trial, intended to assess the program’s effectiveness conducted under real-world conditions and we attempted to obtain data from all enrollees for analyses regardless of their level of program participation.
Primary effectiveness outcomes included weekly minutes of aerobic activity derived from objective and self-report records. Aerobic Activity. Subjective time spent in moderate- and vigorous-intensity PA (MPA and VPA) was obtained using the brief 8-item International Physical Activity Questionnaire (IPAQ) [42], which is widely used and captures PA that is done for work, home and yardwork, for transport, recreation, exercise, and sport. We modified the survey questions to include hand cycling among the examples listed for MPA and VPA activities plus added wheeling on the 2 items that refer to walking (e.g., walking or wheeling), similar to others [43, 44]. We followed published scoring rules, including truncating extreme scores [45], though do not report sitting results as all respondents report using a wheelchair at least 50% of the time.
Objective exercise data were based on data derived from a Polar A300 wrist-based activity monitor paired with a Polar H7 chest-based heart rate (HR) strap to assess exercise intensity. Participants were instructed to use the watch to record their aerobic and strength-training exercise sessions and received training (either in person or via a Zoom-based technology training session) on how to record exercise bouts (selecting the activity type, using start/stop button, and saving each exercise session) and synchronize the device via smartphone over Bluetooth or to a computer with a cable. An API transferred Polar data to the WOWii website via account authentication. The API synced the following data fields to the WOWii site for each exercise bout: device ID, date, time, activity type, duration, average HR, and maximum HR. Polar exercise data were displayed on the WOWii site for participants to view their weekly exercise in relation to their established exercise goals. In the RCT, Polar devices were provided to immediate intervention participants and thus, these data are not available to compare between IMM and WLC groups. However, once a WLC participant ended their wait-list period and was invited to participate in the WOWii program, they were then provided a Polar device. Participants’ exercise participation derive from exercise data recording on the Polar watch and synced to the site.
Secondary outcomes included physiologic indices of fitness and self-reported exercise self-efficacy and barriers. Fitness was measured among the DFW sample (n = 56) by conducting a continuous, graded arm crank protocol in a university lab with gas analysis (Ultima CardiO2, MedGraphics St. Paul MN) and 12-ECG monitoring while participants used a Monark Rehab Trainer 881E (Sweden) by assessors blinded to group assignment and not involved with intervention delivery. Oxygen saturation was monitored by a pulse oximeter with a forehead probe. After one-minute warm up at the participant’s preferred cranking speed (typically 40–60 RPM for those with paraplegia and 10–20 RPM for those with tetraplegia), resistance increased at a fixed 5, 10, or 15 watts increment every 2 min. Starting resistance varied based on injury level; those with paraplegia started at 10 watts and those with tetraplegia started at 5 watts. Testing terminated if any one or more of the following were observed: fatigue based on rating of perceived exertion (RPE of >17 on the 6–20 Borg Scale [46]), respiratory exchange ratio >1.15, reaching age-predicted maximal heart rate, exercise intolerance, or the subject requested to stop [47]. Data from the last 30 s of the final stage were used for analysis. Resting blood pressure (BP) and HR were obtained before and after the exercise testing. Body weight was measured using a digital wheelchair scale (SECA model 664) before exercise testing by obtaining the [1] total weight of the person in their wheelchair and then subtracting [2] the wheelchair weight.
Exercise self-efficacy, exercise barriers, and goal directed thinking based on survey responses provided electronically using SurveyGizmo. Self-efficacy was measured with the 28-item Self-Rated Abilities for Health Practices Scale (SRAHP) to assess exercise self-efficacy. Participants rated each item on a 5-point scale from 0 (not at all) to 4 (completely), yielding a total Health Practices score plus 4 subscales scores regarding Exercise, Nutrition, Health Practices, and Psychological Well Being. The SRAHP has demonstrated strong reliability and validity for individuals with and without disabilities [48]. Internal consistency reliability was high among those with disabilities, with a Cronbach’s alpha value of .94 for the total score and .89 for the Exercise subscale score. Exercise barriers were assessed using the 16-item Barriers to Health Adapted for People with Disabilities (BHADP), originally developed to assess general health promotion barriers but all items are relevant to exercise [49]. Participants rated how frequently issues related to caring for their health interfere with activities on a 4-point scale from 1 (never) to 4 (routinely), yielding a total score plus subscale scores for Motivational and External Barriers. The BHADP has high internal consistency (Cronbach’s α = 0.82) and good discriminant validity between individuals with and without disabilities (p < 0.001) [49].
Goal directed thinking was assessed using the 8-item State HOPE Scale (SHS) [50], a measure of perceived capacity to take an action in reaching the goal (Agency subscale) and perception of seeing different routes to achieve the goal (Pathways subscale). Using an 8-point scale from 1 (definitely false) to 8 (definitely true), participants rated how they think about themselves at that moment. The SHS has demonstrated high internal consistency with Cronbach’s alpha values ranging from 0.82–0.95 [50], including among individuals with SCI [51,52,53].
Feasibility included participant retention, engagement, and satisfaction. Retention for the purposes of the effectiveness trial was defined as participating in at least 1 of the 16 virtual sessions and not formally withdrawing. Engagement was measured weekly based on assessing the number of weeks participants (a) attended virtual meetings and (b) completed the online activities to practice the week’s behavioral skill. Satisfaction was assessed by interview (phone or in-person) after the WOWii follow-up period during which participants rated (on a 5-point scale, higher score higher rating) the usefulness and ease of use of all intervention components (website, brief videos, staff-facilitated virtual meetings, conversations with other WOWii members, Polar monitors, etc.) in helping them start and stick with their exercise program. Satisfaction data presented in Appendix 1.
Data analysis for the RCT and for the IMM and WLC groups combined
Analyses for the RCT portion included multilevel modeling, also known as hierarchical linear modeling (HLM), conducted separately for each outcome measure. Models estimated overall group difference across time (i.e., group effect), change over time (4 months; i.e., time effect), and/or group difference in this change (i.e., group-by-time interaction), while accounting for the dependency of observations—i.e., repeated measurements (level 1) within participants (level 2)—and baseline MPA and VPA at 0 month (i.e., covariates). The HLM analysis for the IMM and WLC groups combined examined any changes during [1] the 16-week WOWii program [2], 2 months after the intervention, and [3] the overall 6-month study period. An effect size (Cohen’s d) was calculated for each comparison. Further, ordinary least square (OLS) regression was used to identify the factors that significantly predict exercise participation among potential predictors including time with disability, impairment type, education, exercise barriers, exercise self-efficacy, and goal directed thinking. As a supplementary test for heterogeneity (i.e., moderation) of the intervention feasibility and effectiveness, the analyses were conducted separately for participant subgroups (impairment type: paraplegia or tetraplegia). All analyses were conducted using SAS 9.4.
Statistical power & sample size
Previous WOW study data [40] provided small to moderate effects on aerobic exercise and strength activity (d = 0.38–0.48) and a priori assumption of high attrition (25%) and high correlation (0.50) among repeated measurement. This suggested that a sample of 140 individuals would produce 80% power to test between-group differences as well as changes over time in the combined study sample for the primary outcome measures.
Results
A total of 168 SCI participants enrolled, with 33% (n = 56) from DFW and 67% from across the continental U.S. (n = 112). Participants were middle-aged (49.6 [12.3] years old), mostly non-Hispanic (87%) and White (78%) (Table 1). 57% were male and 52% were married. Participants were highly educated (50.6% earned a bachelor’s degree or higher), 36% were employed, and 61% reported annual family income of < $70,000. Participants lived with SCI for an average of 15.5 (12.3) years; most experienced paraplegia (60%), and most used a manual wheelchair (62%).
RCT results
Participant retention during the RCT phase of the 16-week WOWii program was 79%, (CONSORT diagram Fig. 1). Table 2 shows descriptive statistics of primary and secondary outcome measures, along with observed group differences in 0–4 months change (effect sizes) and mixed modeling results (group-by-time interactions). The group-by-time interaction was significant for self-reported VPA (p < 0.001) indicating greater increases in VPA among IMM participants compared to WLC participants.
Goal directed thinking as reflected on the State Hope Scale also was significant in group-by-time interactions such that IMM participants reported significantly improved perceptions of having control over changes (p < 0.001). Yet, there were no significant group-by-time interactions for other secondary outcomes of exercise barriers, exercise self-efficacy, or for any physiologic outcomes (all p > 0.05).
Combined group results
One-hundred forty-three individuals (85% of the 168 enrolled) initiated the 16-week WOWii program; of these 120 83.9%) completed the 16-week program outcomes and 75% (n = 90/120) completed follow-up assessments 2 months later. During the 2-month maintenance period, participants did not have contact with study staff, although had access to the Facebook group. Fig. 2 depicts program participation for the 143 who initiated the WOWii program based on how many of the 16 weeks they attended the virtual sessions and exercised. The figure shows that nearly everyone (86–100%) participated during the first 3 weeks, yet fewer than half of individuals (44–46%) participated in at least 13 of the 16 program weeks, and 44% engaged in exercise ≥17 of the 24 weeks they were enrolled. Notably, the figure does not solely reflect participants’ discontinued study enrollment as the data also indicate the total number weeks each participant attended a virtual session and the number of weeks each participant exercised. As such, the data reflect that most participants missed one or more weeks of virtual meetings or one or more weeks of exercise, due to conflicts, illness, or other reasons. Fig. 3 indicates the proportion of WOWii participants who were involved in <1 month up to all 4 months of virtual sessions and exercise. The data show that most (44–46%) were involved for all 4 months. Participants’ exercise is detailed in the following paragraphs.
Polar monitoring data show that while everyone (N = 160) received these activity and HR monitors, only 73% (n = 123/143) of those who initiated the WOWii program wore the devices, recorded exercise sessions, and synced the device, which made data visible on the WOWii site. The following data derive from these recorded exercise sessions. Polar data are available for an average of 10.9 (5.1) of the 16 program weeks, though excluding the 15% who synced their Polar watch for less than 4 weeks show that these participants recorded 12.4 (3.9) weeks (n = 105, 85%). During the 8-week maintenance period just over half (n = 70, 58%) synced their Polar device for 5.4 (2.7) weeks. It is unclear whether participants did not exercise weeks when Polar data are not available or, if they simply did not wear the monitor, or not record the sessions.
Polar exercise data for the combined IMM and WLC groups are displayed in Fig. 4. Polar data depict aerobic exercise for 50–78% of the sample across program weeks and 16–28% recorded strength activities using the Polar watch (see n across the X axis for both aerobic and strength data for each of the 24 weeks). Heart rate data are not shown, as the chest monitors were worn about one-third to two-thirds of the time. The figure suggests that as was recommended, the participants spent progressively more time in aerobic exercise over the program weeks, and achieved 150 min of aerobic activity by week 9, a level that was maintained over subsequent weeks. Participants also increased the number of days they engaged in strength activities over the 16-week period. Participants began the program engaging in aerobic exercise an average of less than 3 days a week, which increased to an average of 3 days by week 3 and to more than 3.5 by week 10, which was maintained through the WOWii program. Though it is important to note that the sample size decreased over time and so it is possible that the data reflect activity levels of the most motivated and active participants and the less motivated participants stopped exercising. During the maintenance period, 29–41% of the sample recorded exercise bouts with their Polar monitor; those who captured these exercise sessions continued doing >150 min/week of aerobic exercise for an average of 3.3 days.
The x-axis indicates each of the 24 study weeks, below which the sample size are derived for data regarding aerobic and strength training. The y-axis along the left side of the figure reflects the number of weekly minutes and along the right side the number of days individuals participated in aerobic and strength training.
Table 3 presents combined data for the IMM and WLC groups to portray changes after the 16-week program and 2 months later for primary and secondary outcomes. The changes over the 6-month study period were significant for most self-reported outcomes, with only a few exceptions (time walking/wheeling, and self-efficacy related to Physical Well Being and Health Promotion). Moreover, both after the WOWii program and 2 months later participants reported significantly greater time spent in MPA (time effect p = 0.003 for 0–4 months change and p = 0.011 for 0–6 months change) and VPA (p = 0.010 and p = 0.008, respectively), significantly increased exercise self-efficacy (p = 0.012 and p < 0.001) and nutrition self-efficacy (p = 0.008 and p < 0.001), and goal-directed thinking in terms of perceiving having control over changes (agency; both p < 0.001). Physiologic outcomes measured during fitness testing with the local sample that showed significant change were peak V̇O2 (p = 0.018, 6.1% relative increase) and power output (p = 0.038, 11% absolute increase), both demonstrated a moderate effect size of 0.31 and 0.32, respectively. Analyses of physiologic outcomes by injury level (paraplegic and tetraplegic, see Supplementary Files) indicate the only outcome to significantly differ was HR reserve such that those with tetraplegia demonstrated an average increase of 13 beats per minute (group-by-time interaction p = 0.044) Table 4.
Linear regression results suggested that higher exercise self-efficacy significantly predicted participating in aerobic/strength exercise (using Polar-derived data) (p < 0.05) over the WOWii program when accounting for other factors (time with disability, impairment type, education, exercise barriers, and goal directed thinking).
Feasibility outcomes (engagement and satisfaction). Feasibility data (Fig. 5) were analyzed in terms of (a) efficacy where the denominator was based on all enrollees (n = 168) and (b) effectiveness where the denominator reflects those who remained in the program (n = 133, as 13 people remained in the program, but did not complete post-test assessments). Engagement data based on those who attended at least 1 meeting show they attended an average of 10 of the 16 virtual meetings and completed 12 of the 16 module activities. Attendance averaged 66% across the 16 sessions and participants online activity completion average of 83%. Satisfaction results appear in Appendix 1.
Discussion
This study contributes to the growing evidence base regarding PA and exercise programs for people with SCI. RCT results show the 16-week WOWii program helped intervention participants engage in more VPA and increase their goal-directed thinking in terms of their capacity to take action and seeing various paths to achieve their goals, though there were not measurable between group differences in fitness. Combining data from the IMM and WLC groups after they received the WOWii program revealed similar results. WOWii participants reported significant improvements at both the 4- and 6-month assessment periods for increasing VPA, reporting fewer exercise barriers, greater self-efficacy for exercise and nutrition, plus goal directed thinking. Although participants did not demonstrate significant MPA or VPA increases between post-testing and the 2 month follow-up, they remained more active 2 months after the program than at baseline. Additionally, the data indicate the WOWii program is feasible to deliver. Three-quarters of participants remained in the 16-week program, participants demonstrated good engagement based on attending virtual sessions (averaged 66%) and completing online activities (averaged 83%), plus rated the program as useful (4.2 on a 5-point scale) in helping make behavior changes.
Session attendance is an indicator of the program success. While several studies have reported 100% attendance to sessions [25, 27,28,29]. they were conducted for half as long (8 weeks) and had small sample sizes (<15 participants). At the other end of the spectrum, another study reported that 93% of the sample had poor adherence, based on time engaged in exercise, with 50% non-adherent and 43% had low to suboptimal adherence. While results reported in this study indicate lower attendance than other studies, these data are based on a substantially larger sample -- 168 participants–over a much longer time period -- 16 weeks. Whether using attendance rates based on an intent-to-treat approach with the denominator of the full sample (n = 168) or based on effectiveness analyses using a denominator reflecting those who remain in the program (n = 133) shows a slow decline in attendance from week 1 to week 6, which remained stable over the subsequent 10 weeks. Efficacy-based attendance averaged 57%, attendance averaged 66% for those who did not withdraw and participants’ program engagement, based on completing the weekly online activities averaged 71% (efficacy) to 83% (effectiveness).
These trial results suggest pairing strategies previously demonstrated as successful such as goal setting, self-monitoring, and providing exercise equipment with new features such as providing content online and delivering group-based virtual sessions have the potential to promote high program engagement and exercise participation. The WOWii website was easy to navigate and contained resources, content, plus weekly modules that contained less text and more images and videos that conveyed useful information. Additionally, the weekly group-based virtual meetings offered a platform where participants received both professional and peer support, which are features in line with findings reported by Pancer and colleagues [31].
The WOWii program was designed as a multi-component intervention, yet an important difference between this and other programs is that WOWii was delivered via group-based, virtual sessions whereas others generally provided 1-on-1 telephone-based support. While virtual sessions were led by a study team member, an essential feature of these group meetings was facilitating participants’ conversation. This allowed peers to support one another and share knowledge, which we contend is a crucial feature of the program’s success. Offering the entire program online represents the next generation approach to promote exercise for people living with SCI and has considerable advantages in terms of reach, user control, and cost. Notably, the WOWii program was delivered to participants in the pre-COVID-19 environment. This platform may be even more highly rated since Zoom and other videoconferencing platforms have become a new norm for business and social interactions. Further, as COVID may impact daily life for months to come, this approach for program delivery may yield even greater effects given the likelihood that many are facing greater social isolation during the pandemic.
Limitations. Several limitations are worth noting. First, attrition was higher in the IMM (24%) than the WLC group (10%) over the 16-week trial, though our analytic approach of HLM offers some protection against this bias as it is an Intent-to-Treat approach that uses information from the full sample. The study team encountered difficulties with Polar monitors and API site, which hampered the ability to obtaining all exercise session data. Although Polar allows individuals to hand enter exercise data online, the API does not transfer hand entered data. Thus, sessions in which participants forgot to wear their watch or start/stop the exercise session were missing from the WOWii site, which was a relatively common experience. Our study staff spent tremendous time and effort manually extracting these data from the Polar site to capture those exercise bouts. Another limitation is that the sample represents those in the contemplation and action stages of change and who are more likely to adopt activity given that the screening process required that participants contact the study team. Two other notable limitations are that objective exercise monitoring was only conducted among IMM and thus we do not have objective exercise data from the WLC participants to know if they also increased their exercise participation during the 4-month waiting period. The other notable limitation is our use of the IPAQ for participant reports of weekly MVPA. Though used in other studies with wheelchair users [43, 44], the survey has not been validated for with wheelchair users or SCI samples. Further, study participants reported substantially higher levels of MVPA even before initiating the program than reported in studies that use surveys such as the Physical Activity Recall Assessment for People with Spinal Cord Injury [19, 20, 22, 54, 55]. This difference in reporting may reflect that the IPAQ asks respondents to report the time engaged during employment, while performing house and yardwork, for transport, and in sport and recreation that qualifies as VPA and MPA, which is defined by physical effort and breathing rate. Further, participants’ responses may indicate the fact that inactive individuals with SCI have low fitness levels and performing activities such as housework, yardwork, grocery shopping can yield high levels of physical strain [56], which in turn respondents may count toward the time they report doing these activities. Finally, though combined group analyses revealed significant differences in V̇O2 peak and peak power, the average observed changes were sufficiently small that they may not be clinically meaningful.
Conclusion
The WOWii program is a promising approach to promote home and community-based exercise among those with SCI by facilitating program reach, access to exercise equipment, social support, and eliminating transportation barriers. The 16-week program duration allowed adequate time for participants get to know one another, connect as a group, share their knowledge and experience, and model positive exercise practices. Future research can investigate if similar results can be achieved using a peer-mediated approach.
Data archiving
The datasets generated during and analyzed for the study are available from the corresponding author on request and will be archived at the Interuniversity Consortium for Political and Social Research (ICPSR) by the end of 2022.
References
Cowan RE. Exercise is medicine initiative: physical activity as a vital sign and prescription in adult rehabilitation practice. Arch Phys Med Rehab. 2016;97:S232–S7.
Cowan R, Malone L, Nash M. Exercise is Medicine™: Exercise prescription after SCI to manage cardiovascular disease risk factors. Topics in Spinal Cord Injury. Rehabilitation. 2009;14:69–83.
American College of Sports Medicine (ACSM). Exercise is medicine fact sheet: ACSM; 2012 [February, 2014]. Available from: http://www.exerciseismedicine.org/documents/EIMFactSheet2012_all.pdf.
Sallis RE. Exercise is medicine and physicians need to prescribe it! Br J Sports Med. 2009;43:3–4. https://doi.org/10.1136/bjsm.2008.054825.
U.S. Department of Health and Human Services. Physical activity and health: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34.
Nash MS, Groah SL, Gater DR Jr, Dyson-Hudson TA, Lieberman JA, Myers J, et al. Identification and management of cardiometabolic risk after spinal cord injury: clinical practice guideline for health care providers. Topics in Spinal Cord Injury. Rehabilitation. 2018;24:379–423.
Valent L, Dallmeijer A, Houdijk H, Talsma E, van der Woude L. The effects of upper body exercise on the physical capacity of people with a spinal cord injury: a systematic review. Clin Rehabil. 2007;21:315–30.
Ravenek KE, Ravenek MJ, Hitzig SL, Wolfe DL. Assessing quality of life in relation to physical activity participation in persons with spinal cord injury: a systematic review. Disabil Health J. 2012;5:213–23. https://doi.org/10.1016/j.dhjo.2012.05.005. Epub 2012/10/02; PubMed PMID: 23021731.
van der Scheer JW, Ginis KAM, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Farrow M, Nightingale TE, Maher J, McKay CD, Thompson D, Bilzon JLJ. Effect of Exercise on Cardiometabolic Risk Factors in Adults With Chronic Spinal Cord Injury: a systematic review. Arch Phys Med Rehabil. 2020. Epub 2020/05/24. https://doi.org/10.1016/j.apmr.2020.04.020. PubMed PMID: 32445849.
Tomasone JR, Wesch NN, Ginis KAM, Noreau L. Spinal cord injury, physical activity, and quality of life: a systematic review. Kinesiol Rev. 2013;2:113–29. https://doi.org/10.1123/krj.2.2.113.
van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, Bergen MP, et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil. 2008;89:2094–101. https://doi.org/10.1016/j.apmr.2008.04.024. Epub 2008/11/11 PubMed PMID: 18996237.
Martin Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury Part I: Demographic and injury-related correlates. Arch Phys Med Rehabil. 2010;91:722–8. 10/1016/j.apmr.2009.12.027.
Hiremath SV, Amiri AM, Thapa-Chhetry B, Snethen G, Schmidt-Read M, Ramos-Lamboy M, et al. Mobile health-based physical activity intervention for individuals with spinal cord injury in the community: A pilot study. PLoS ONE. 2019;14:e0223762. Epub 2019/10/16. https://doi.org/10.1371/journal.pone.0223762. PubMed PMID: 31613909; PubMed Central PMCID: PMC6793862.
Nooijen CF, Stam HJ, Bergen MP, Bongers-Janssen HM, Valent L, van Langeveld S, et al. A behavioural intervention increases physical activity in people with subacute spinal cord injury: a randomised trial. J Physiother. 2016;62:35–41. https://doi.org/10.1016/j.jphys.2015.11.003. Epub 2015/12/25; PubMed PMID: 26701155.
Nightingale TE, Rouse PC, Walhin JP, Thompson D, Bilzon JLJ. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99:1998–2006 e1. https://doi.org/10.1016/j.apmr.2018.05.008. Epub 2018/06/15; PubMed PMID: 29902472.
Tomasone JR, Arbour-Nicitopoulos KP, Latimer-Cheung AE, Martin Ginis KA. The relationship between the implementation and effectiveness of a nationwide physical activity telephone counseling service for adults with spinal cord injury. Disabil Rehabil. 2018;40:527–37. https://doi.org/10.1080/09638288.2016.1261415. Epub 2016/12/29; PubMed PMID: 28029067.
Latimer AE, Ginis KAM, Arbour KP. The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: A randomized controlled trial. Rehabil Psychol. 2006;51:273–80. https://doi.org/10.1037/0090-5550.51.4.273. PubMed PMID: WOS:000242144300001.
Arbour-Nicitopoulos KP, Ginis KAM, Latimer AE. Planning, leisure-time physical activity, and coping self-efficacy in persons with spinal cord injury: A randomized controlled trial. Archives of Physical and Medical. Rehabilitation. 2009;90:2003–11. https://doi.org/10.1016/j.apmr.2009.06.019.
Wise HH, Thomas J, Nietert PJ, Brown DD, Sword DO, Diehl N. Home physical activity programs for the promotion of health and wellness in individuals with spinal cord injury. Topics in Spinal Cord Injury. Rehabilitation. 2011;14:122–32.
Bombardier CH, Dyer JR, Burns P, Crane DA, Takahashi MM, Barber J, et al. A tele-health intervention to increase physical fitness in people with spinal cord injury and cardiometabolic disease or risk factors: a pilot randomized controlled trial. Spinal Cord. 2020. Epub 2020/07/23. https://doi.org/10.1038/s41393-020-0523-6. PubMed PMID: 32694748.
Lai B, Wilroy J, Young HJ, Howell J, Rimmer JH, Mehta T, et al. A Mobile App to Promote Adapted Exercise and Social Networking for People With Physical Disabilities: Usability Study. JMIR Form Res. 2019;3:e11689. Epub 2019/03/20. https://doi.org/10.2196/11689. PubMed PMID: 30888325; PubMed Central PMCID: PMC6444218.
Wilroy JD, Lai B, Davlyatov G, Mehta T, Thirumalai M, Rimmer JH. Correlates of adherence in a home-based, self-managed exercise program tailored to wheelchair users with spinal cord injury. Spinal Cord. 2020. Epub 2020/06/17. https://doi.org/10.1038/s41393-020-0497-4. PubMed PMID: 32541883.
Ma JK, West CR, Martin Ginis KA. The effects of a patient and provider co-developed, behavioral physical activity intervention on physical activity, psychosocial predictors, and fitness in individuals with spinal cord injury: a randomized controlled trial. Sports Med. 2019;49:1117–31. https://doi.org/10.1007/s40279-019-01118-5. Epub 2019/05/24; PubMed PMID 31119717.
Ma JK, Cheifetz O, Todd KR, Chebaro C, Phang SH, Shaw RB, et al. Co-development of a physiotherapist-delivered physical activity intervention for adults with spinal cord injury. Spinal Cord. 2020;58:778–86. https://doi.org/10.1038/s41393-020-0422-x. Epub 2020/01/24; PubMed PMID: 31969687.
Lai B, Rimmer J, Barstow B, Jovanov E, Bickel CS. Teleexercise for persons with spinal cord injury: a mixed-methods feasibility case series. JMIR Rehabil Assist Technol. 2016;3:e8. https://doi.org/10.2196/rehab.5524. Epub 2017/06/06; PubMed PMID: 28582252; PubMed Central PMCID: PMC5454561.
Chemtob K, Rocchi M, Arbour-Nicitopoulos K, Kairy D, Fillion B, Sweet SN. Using tele-health to enhance motivation, leisure time physical activity, and quality of life in adults with spinal cord injury: A self-determination theory-based pilot randomized control trial. Psychol Sport Exerc. 2019;43:243–52. https://doi.org/10.1016/j.psychsport.2019.03.008
Rocchi MA, Robichaud Lapointe T, Gainforth HL, Chemtob K, Arbour-Nicitopoulos KP, Kairy D, et al. Delivering a tele-health intervention promoting motivation and leisure-time physical activity among adults with spinal cord injury: an implementation evaluation. Sport, Exercise, and Performance Psychology. 2020. https://doi.org/10.1037/spy0000207.
Allin S, Shepherd J, Thorson T, Tomasone J, Munce S, Linassi G, et al. Web-Based Health Coaching for Spinal Cord Injury: results from a mixed methods feasibility evaluation. JMIR Rehabilitation Assistive Technol. 2020;7:e16351. https://doi.org/10.2196/16351.
Pancer M, Manganaro M, Pace I, Marion P, Gagnon DH, Laramee MT, et al. A web-based physical activity portal for individuals living with a spinal cord injury: qualitative study. JMIR Form Res. 2019;3:e12507. https://doi.org/10.2196/12507. Epub 2019/07/28; PubMed PMID: 31350835.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34. https://doi.org/10.1249/mss.0b013e3180616b27. Epub 2007/09/01; PubMed PMID: 17762377.
Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. Journal of the American Medical Association JAMA. 2018. https://doi.org/10.1001/jama.2018.14854.
Goosey-Tolfrey VL, van der Scheer JW, Lexell J, Clements K, Martin Ginis KA. International SCIEGPG. Development of scientific exercise guidelines for adults with spinal cord injury. Br J Sports Med. 2018;52:1166–7. https://doi.org/10.1136/bjsports-2018-099202. Epub 2018/04/27; PubMed PMID: 29695510.
Martin Ginis KA, Hicks AL, Latimer AE, Warburton DE, Bourne C, Ditor DS, et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord. 2011;49:1088–96.
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21. https://doi.org/10.1038/s41393-017-0017-3. Epub 2017/10/27; PubMed PMID: 29070812.
Centers for Disease Control and Prevention. 2007 Behavioral Risk Factor Surveillance System Questionnaire. 2007.
Bandura A Social foundations of thought and action: Social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
Marlatt GA, Gordon JR. Relapse prevention. Warm Beach, Washington: The Guilford Press; 1985.
Froehlich-Grobe K, Lee J, Aaronson LS, Nary DE, Washburn RA, Little TD. Exercise for everyone: a randomized controlled trial of Project Workout On Wheels in promoting exercise among wheelchair users. Arch Phys Med Rehabil. 2014;95:20–8. https://doi.org/10.1016/j.apmr.2013.07.006.
Cole M, Froehlich-Grobe K, Driver S, Shegog R, McLaughlin J. Website Redesign of a 16-week exercise intervention for people with spinal cord injury by using participatory action research. JMIR Rehabil Assist Technol. 2019;6:e13441. https://doi.org/10.2196/13441.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Saebu M, Sorensen M. Factors associated with physical activity among young adults with a disability. Scand J Med Sci Sports. 2011;21:730–8. https://doi.org/10.1111/j.1600-0838.2010.01097.x. Epub 2010/05/13; PubMed PMID: 20459465.
Bombardier CH, Fann JR, Tate DG, Richards JS, Wilson CS, Warren AM, et al. An exploration of modifiable risk factors for depression after spinal cord injury: which factors should we target? Arch Phys Med Rehabil. 2012;93:775-81. Epub 2012/03/24. https://doi.org/10.1016/j.apmr.2011.12.020. PubMed PMID: 22440484.
IPAQ Core Group. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - Short and Long Forms 2005 [cited 2020 October]. Available from: www.ipaq.ki.se.
Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92–8.
American College of Sports Medicine. ACSM’s exercise testing and prescription (10th Edition). 10th ed. Madeline P, Bayles AMS, editor. Philadelphia, PA: Wolters Kluwer; 2017.
Becker H, Stuifenbergen A, Oh HS, Hall S. Self-rated abilities for health practices: a health self-efficacy measure. Health Values. 1993;17:42–50.
Becker H, Stuifbergen AK, Sands D. Development of a scale to measure barriers to health promotion activities among persons with disabilities. Am J Health Promot. 1991;5:449–54.
Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL. Development and validation of the state hope scale. J Pers Soc Psychol. 1996;70:321–35.
Kennedy P, Evans M, Sandhu N. Psychological adjustment to spinal cord injury: the contribution of coping, hope and cognitive appraisals. Psychol Health Med. 2009;14:17–33. https://doi.org/10.1080/13548500802001801. Epub 2008/12/17; PubMed PMID: 19085309.
Kortte KB, Stevenson JE, Hosey MM, Castillo R, Wegener ST. Hope predicts positive functional role outcomes in acute rehabilitation populations. Rehabil Psychol. 2012;57:248–55. https://doi.org/10.1037/a0029004. Epub 2012/09/06; PubMed PMID: 22946612.
Martz E, Livneh H. Psychosocial adaptation to disability within the context of positive psychology: findings from the literature. J Occup Rehabil. 2016;26:4–12. https://doi.org/10.1007/s10926-015-9598-x. Epub 2015/08/19; PubMed PMID: 26283187.
Ginis KA, Latimer AE, Hicks AL, Craven BC. Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc. 2005;37:1099–111.
Latimer AE, Ginis K, Craven BC, Hicks AL. The physical activity recall assessment for people with spinal cord injury: validity. Med Sci Sports Exerc. 2006;38:208–16.
Janssen TW, van Oers CA, Veeger HE, Hollander AP, van der Woude LH, Rozendal RH. Relationship between physical strain during standardised ADL tasks and physical capacity in men with spinal cord injuries. Paraplegia. 1994;32:844–59. https://doi.org/10.1038/sc.1994.131. Epub 1994/12/01; PubMed PMID: 7708424.
Acknowledgements
The authors would like to thank the individuals who served as focus group members to provide input and guidance in developing the WOWii website and the initial pilot participants who provided important information in shaping the program plus everyone who participated in the WOWii trial. Their time and input were invaluable to our team and we enjoyed getting to know each one of them. The team would also like to acknowledge early study coordinators, Maria Cole, MPH, MSW and Danielle Carlton, MPH who helped launch the study. The content of this paper was developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR; grant number 90IF0091). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS).
Funding
The content of this paper was developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90IF0091). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The content of this paper does not necessarily represent the policy of NIDILRR, ACL, and HHS, and is not endorsed by the Federal Government. The content of this paper was developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR; grant number 90IF0091). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The content of this paper does not necessarily represent the policy of NIDILRR, ACL, and HHS, and is not endorsed by the Federal Government.
Author information
Authors and Affiliations
Contributions
KFG: conceptualized the study design, developed the first full draft of the manuscript. JL: assisted with study conceptualization, conducted all analyses, and wrote the analyses and power sections plus substantially edited text for the results section. CO: assisted with data management, cleaning, and editing various rounds of drafts of the manuscript. AL: assisted with intervention delivery, data entry, Polar data abstraction, plus conducting literature reviews and summarizing new evidence, plus conducting literature reviews and summarizing new evidence. ES: assisted with intervention delivery, data entry, plus analyzing satisfaction data and drafting the text regarding participants satisfaction with the study. SD: assisted with study conceptualization, data interpretation, plus provided substantial contribution to the writing and editing the manuscript drafts. RS: assisted with study conceptualization, data analyses and interpretation, plus provided substantial contribution to the writing and editing the manuscript drafts. SJL: conducted all lab-based testing for fitness measures and weight plus assisted with interpreting results and writing results for the physiologic testing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Froehlich-Grobe, K., Lee, J., Ochoa, C. et al. Effectiveness and feasibility of the workout on wheels internet intervention (WOWii) for individuals with spinal cord injury: a randomized controlled trial. Spinal Cord 60, 862–874 (2022). https://doi.org/10.1038/s41393-022-00787-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00787-w
This article is cited by
-
Qualitative analysis of perceived motivators and barriers to exercise in individuals with spinal cord injury enrolled in an exercise study
Spinal Cord Series and Cases (2022)