Abstract
Background
Spinal gout is uncommon. The clinical manifestations of spinal gout are not characteristic. Huge tophi can invade the vertebral joints and protrude into the spinal canal, even causing spinal canal stenosis, which may result in irreparable spinal cord injury. Therefore, early diagnosis and treatment is very important. Summarizing the imaging features of spinal gout may help clinicians with an early diagnosis and promptly intervention.
Study design
Retrospective case series.
Objectives
To describe the findings from computed tomography (CT) images of spinal gout, including the tophi location, growth pattern, involvement of adjacent joints, and differentiation from other spinal lesions.
Methods
We analyzed CT images from the atlantoaxial joint and lumbar spine in 17 cases with spinal gout.
Results
17 cases had tophi as high-density masses. 14 (82.4%) cases involved lumbar facet joints, including 7(41.2%)cases involving single vertebral facet joints and 7(41.2%) cases involving multiple vertebral facets. CT imaging showed bone resorption and erosion of the facet joints, as well as narrowing of the joint space. The other three cases (17.6%) involved the atlantoaxial joint, showing a high-density mass around the odontoid process with bone resorption and invasion under the articular surface. One case was secondary to a pathological fracture. Four cases (23.6%) showed a huge mass protruding into the spinal canal where the nerve root was compressed, and even spinal cord injury, leading to serious lower back pain symptomatic of brachial plexus or sciatic nerve compression, and even affected the motor function of lower limbs.
Conclusions
In cases with gouty arthritis involving the axial spine, the lower lumbar spine is mainly involved, high-density tophi grow forward and backward around the facet joints, CT image shows bone resorption, erosion of facet joints, and narrowing of the joint space. With atlantoaxial joint involvement, there was evidence of bone resorption combined with joint.
Similar content being viewed by others
Introduction
Gout is a rheumatic metabolic disease associated with hyperuricemia which causes uric acid deposition and may result in gouty arthritis, uric acid nephropathy, and kidney stones. The incidence rate of gout in China is increasing gradually. Worldwide, patients tend to be younger and the incidence rate in coastal areas or economically developed areas is higher, mostly due to the different dietary patterns [1, 2]. Clinical cases are divided into the acute, intermittent, and chronic phases.
Gouty arthritis is a metabolic disease. Due to the high level of uric acid in the blood, sodium urate crystals deposit in the bone joints, causing a local inflammatory reaction and bone tissue destruction. The pathological basis of gouty arthritis is the formation of a gout stone, which is manifested as nodular gout stones, often occurring in the foot, ankle, knee, and other wedge joints [3]. Gouty arthritis in the spine is rare [4]. In this study, computed tomography (CT) imaging data from 17 individuals with spinal gout mainly involving the lumbar facet joint and atlantoaxial joint were collected and analyzed to describe the clinical manifestations of the disease.
Methods
Cases
Seventeen individuals diagnosed with axial gout receiving CT imaging between January 2012 and December 2020 were included. All 17 cases were adult males. In total, 14 cases (82.4%) involved the lumbar facet joint, 2 cases (11.8%) involved both lumbar facet and atlantoaxial joints, and 1 case (5.9%) involved the atlantoaxial joint. The ages of the participants ranged from 23 to 85 years old.
Data collection
CT imaging data and clinical data of all cases were collected, including uric acid levels, pathological results or past medical history to confirm that they had gout. All cases received CT examinations.
Scanning method
To scan, a “GE BrightSpeed 16 CT System or Siemens Definition AS 64 CT System was used. The scanning slice thickness was 2 mm and the interval was 2 mm. After scanning, the original image was post-processed and multiplanar reconstruction of the coronal and sagittal planes was performed. The reconstruction slice thickness and interval were 2 mm.
Imaging studies
All images were independently analyzed by two radiologists with more than 10 years of clinical experience. The specific imaging evaluation parameters include the location, size, shape, and characteristics of the tophi, degree of bone erosion under the articular surface, presence of secondary pathological fractures, spinal stenosis.
Results
In total, 17 cases were diagnosed with gout by a clinical, laboratory, or pathological examination. Of these, 11 cases had surgical and pathological evidence of gout stones in the spine or other parts of the body. Among the other cases, 4 cases had typical gout appearing in the joints and other parts of the body diagnosed by X-ray or B-ultrasound (not including CT or MRI). The remaining 2 cases had a history of chronic gout lasting for several years. All cases received CT examination, of which 9 cases also received X-ray or magnetic resonance imaging (MRI) examination of other joints, which confirmed the existence of gouty arthritis.
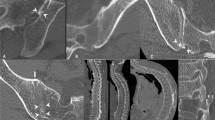
CT images in 17 cases showed the tophi as high-density masses. 14 (82.4%) cases involved lumbar facet joints, including 7 (41.2%) cases involving single vertebral facet joints and 7 (41.2%) cases involving multiple vertebral facets. CT imaging showed bone resorption and erosion of the facet joints, as well as narrowing of the joint space.The other 3 cases (17.6%) involved the atlantoaxial joint, showed high-density tophi around the odontoid process with bone resorption and invasion under the articular surface (Fig. 1). One case was secondary to a pathological fracture. In 4 cases (23.6%), the huge tophi protruding into the spinal canal where the nerve root was compressed, and even spinal cord injury, leading to serious lower back pain symptomatic of brachial plexus or sciatic nerve compression, and even affected the motor function of lower limbs (Fig. 2).
Discussion
This study aimed to analyze CT imaging data from 17 individuals with spinal gout mainly involving the lumbar facet joint and atlantoaxial joint to describe the clinical manifestations of the disease. Our results indicate that most gouty deposits involved the lumbar facet joints.
It is known that limb joints are the most frequently involved joints in gouty arthritis, including the first toe metatarsal, cuneiform, ankle, knee, wrist, and elbow joints, for example. Gouty arthritis usually involves monoarticular. In this group of cases, seven patients involved multiple vertebral facets.The pathological basis of this disease is the deposition of urate in the joint or bursa, which can lead to inflammation of the surrounding soft tissue and slowly erode the surface of the bone, from the outside to the inside, leading to bone absorption and destruction. Individuals with gouty arthritis usually experience pain and limited activity because of inflammation and bone marrow edema in diseased joints [5,6,7,8].
The cases presented herein mainly involved the facet joints. Spinal stenosis caused by tophi led to compression of nerve roots and resulted in numbness of limbs in some cases. The tophi shows a huge mass in few cases, invades the spinal canal and compresses the spinal cord, resulting in spinal cord injury, which needs surgical resection. Gouty arthritis that occurred in the atlantoaxial joint because of the deposition of tophi, resulted in atlantoaxial space stenosis. At the same time, despite facet joint or atlantoaxial joint involvement, when there was inflammation on the articular surface, the cases experienced pain in that joint. Previously, it was thought that gouty arthritis of the axial spine was rare [8], but one recent study [9] reports that gouty arthritis involving the axial spine is more common than previously thought. We need early detection and treatment to avoid spinal canal stenosis, nerve compression or spinal cord injury caused by spinal gout, because spinal cord injury is often difficult to recover.
Gout is mainly diagnosed by clinical symptoms, laboratory results, and image findings. In 1977, the American Rheumatic Society established the classification standard of gout. First, the diagnosis of gout must be based on the presence of urate crystals in the synovial fluid or urate crystals in the tophi confirmed by chemical assay or seen via microscope. In addition to clinical and laboratory findings, gout can be classified by the asymmetric intra-articular swelling or non-erosive subcortical bone cysts confirmed by X-ray, which reflects the importance of imaging in the diagnosis of gout.
We based our consensus for diagnostic criteria on domestic and foreign gout-related disease guidelines which link key clinical indicators such as high blood uric acid levels, urate deposition, and inflammatory reaction, with the development of gout [10]. In 2015 [11], the American College of Rheumatology and the European Anti-rheumatic League jointly developed a classification system for gout, which reinforces the importance of imaging in diagnosis. Specifically, the identification of urate deposits in joints or bursae by dual-energy CT and ultrasound and identification of gouty bone lesions by x-ray plain film are included. The classification system also suggests that a non-invasive diagnosis of gout can be achieved by combining clinical symptoms, uric acid level, and image findings. Domestic and foreign researchers have pointed out that dual-energy CT can more accurately detect urate deposition in the joint area due to the composition of urate which has a high imaging sensitivity [12, 13]. Studies that compared results of ultrasound with those of CT and MRI [14] found that CT findings were highly consistent with the pathologic anatomy in the evaluation of tophus and bone destruction [15]. However, most of the imaging studies on gouty arthritis focus on the large joints of the upper and lower limbs, while the imaging findings of cristae gout are less known, appearing mostly in case reports. The results of this study are similar to those of Zhi [16] Ming [17], however, the disadvantage is that we included only plain spiral CT instead of dual-energy CT. For further analysis of tophus, this needs to be supplemented in future work.
Spinal gout mainly involved the facet joints and atlantoaxial joints in the present study. Image findings showed that bone resorption occurred under the articular surface, accompanied by high-density tophi around the joint, which are characteristic imaging manifestations. In this group of cases, 14 cases involving lumbar facet joints, with different sizes of gout stones. The images showed high-density urate mass around the facet joints, due to the urate mainly deposited in the articular cartilage or synovium. The synovium is located at the edge of the facet and there are synovial folds between facets. The tophi develop behind the facet at first and then it forms forward and backward around the facet. Spinal gout is usually induced by facet joint inflammation due to bursitis and then develops into gouty arthritis. Some scholars suggest that the most common occurrence is in the lumbar spine in cases of spinal gout [18]. In the spine, the lumbar spine is the most load-bearing region, and spinal gout affects the facet joints of L4/5 or L5/S1 most commonly [19]. Some research suggests that the cause of gouty arthritis in the lower lumbar facet joint may be related to blood supply disorders and low pH value [20, 21]. This group of cases involving multiple joints showed that tophi involving the right facet was more serious than that on the left, and the bone resorption under the right facet was more obvious than that on the left. This may be because most people move their right limb more frequently than their left limb.
In the present study, three cases of atlantoaxial joint involvement showed high-density tophi around the odontoid process, accompanied by bone absorption under the atlantoaxial joint surface. Two cases had been living with gout for decades accompanied by serious gouty arthritis in many joints and subcutaneous extensive gout nodules. The bone resorption in other areas with gouty arthritis was more serious than that in the atlantoaxial joint, and the tophi were more extensive. We assume that atlantoaxial gouty arthritis may appear later compared to gout in other areas, however, the number of cases in this group is small and the results cannot be statistically analyzed.
In this group, four cases of tophi showed a huge mass, three cases involved the lumbar facet joint, one case involved the atlantoaxial joint, with obvious bone absorption and erosion of the involved joints, a pressed nerve root, and a narrowed neurocanal,and even spinal cord compression in some cases. All the cases were young men (23–39 years old) All of them experience acute attacks of neck pain, as well as lower back and shoulder pain. They all experienced rapid development of their symptoms. The imaging finding in each case was a high-density huge mass, which can easily be misdiagnosed as a chondrogenic tumor. The differential characteristics for gout are that the huge mass develops forward and backward around the facet joint, there is no obvious soft tissue mass around the huge mass, and the muscle is compressed. Combined with the laboratory findings of the case, correct diagnoses are possible.
Rheumatoid arthritis is one possible differential diagnosis in the present cases. Rheumatoid arthritis mainly occurs in middle-aged women, which is characterized by multiple and nonspecific chronic arthritis. This is different from gouty arthritis as it usually involves bilateral symmetrical joints, most often involving the small joints of the hands and feet. Rheumatoid arthritis involving the atlantoaxial joint results in bone resorption of the atlantoaxial joint without tophi. Differential diagnosis can be made in combination with the laboratory results and clinical manifestations of the patien, such as positive rheumatoid factor, increased erythrocyte sedimentation rate, and stiffness of the affected joint.
In addition, gout can be misdiagnosed as degenerative osteoarthritis of the spine. Degenerative osteoarthritis of the spine usually occurs in middle-aged and elderly patients, and there are usually severe degenerative changes of the spine, including degenerative changes of facet joints and intervertebral discs. Degenerative osteoarthritis involving the facet joint usually presents as a narrowing of the facet joint space, bone hyperplasia, sclerosis under the articular surface, formation of marginal osteophytes, usually without bone absorption under the articular surface, and no tophi around the joint. Combined with the overall condition of the patient’s spine, a differential diagnosis can be made.
In the study by Martins [11], it is pointed out that hyperuricemia without treatment may cause spinal tophi deposition. Therefore, the primary treatment of spinal gouty arthritis is to reduce the concentration of uric acid and take analgesic drugs to relieve the symptoms associated with lower back pain [9], as well as dietary intervention. In order to avoid severe paraplegia, early surgical intervention to relieve the numbness and weakness of limbs caused by the compression of tophi is recommended. However, there are also some patients without nerve compression or low back pain. These patients need combined imaging and laboratory examination to make the correct diagnosis and treatment to avoid future symptoms [22,23,24,25,26,27,28].
There are some limitations of this study to consider. There were a small number of cases for the analysis, and only three cases involving the atlantoaxial joint. Therefore, more data are needed to explore the imaging parameters for diagnosis. With future studies to understand the imaging features, combined with the differential diagnosis features of other lesions, we can improve the accuracy of imaging diagnosis, provide advice and basis for early clinical treatment, and avoid more serious consequences caused by delayed treatment.
Conclusions
The clinical manifestations of spine gout are not reliably characteristic. The main manifestations are pain caused by arthritis of the affected area or symptoms caused by nerve compression by tophi. However, CT imaging manifestations of spine gout have certain reliable characteristics. The results from this group of cases suggest that spine gout initially involves the lower lumbar spine, the high-density mass accumulates forward and backward around the facet joints, and that it is accompanied by bone absorption and erosion under the facet joints. Huge tophi can protrude into the spinal canal, causing spinal canal stenosis and even spinal cord compression, resulting in irreparable spinal cord injury. Therefore, early diagnosis and treatment is very important. Further, when the atlantoaxial joint is involved, the bone absorption combined with tophi is evident. Combined with the laboratory findings, we can distinguish the diagnosis from rheumatoid arthritis.
Data availability
All data were uploaded and saved in our hospital. If necessary, you can contact the corresponding author for accessived.
References
Gong Y, Su X. 2016 Chinese guideline for gout diagnosis and treatment. Chin J Intern Med. 2016;55:892–9.
Li L, Zhu X, Dai Y, Lin H, Dai R. Expert group of multidisciplinary consensus on diagnosis and treatment of hyperuricemia related diseases. Chinese multidisciplinary expert consensus on diagnosis and treatment of hyperuricemia related diseases. Chin J Intern Med. 2017;56:235–48.
Kumar R, Khalsa DD, Carmody JB. Serum uric acid and hyperuricemia in U.S. adolescents: 40-year trends. Clin Exp Rheumatol. 2016;34:S22–S23.
Wei C, Yu S, Guo Y. Imaging findings of spinal gouty arthritis. M M I Monthly. 2020;29:1005–8.
Konatalapalli RM, Demarco PJ, Jelinek JS, Murphey M. Gibson Michael. Gout in the axial skeleton. J Rheumatol. 2009;36:609–13.
Konatalapalli RM, Lumezanu E, Jelinek JS, Murphey MD, Wang H, Weinstein A. Correlates of axial gout: a cross-sectional study. J Rheumatol. 2012;39:1445–9.
Wells AF, MacDonald PA, Chefo S, Jackson RL. African American patients with gout: efficacy and safety of febuxostat vs. allopurinol. BMC Musculoskelet Disord. 2012;13:13–15.
Lumezanu E, Konatalapalli R, Weinstein A. Axial (Spinal) Gout, Current Rheumatology Reports. 2012.14:161–4.
Leventhal LJ, Levin RW, Bomalaski JS. Peripheral arthrocentesis in the work-up of acute low back pain. Arch Phys Med Rehabil. 1990;71:253–4.
Zhu C-C, Yang Q. Advances in imaging study of gouty arthritis. Chin J Med Imaging. 2020;28:156–60.
de Mello FM, Helito PVP, Bordalo-Rodrigues M, et al. Axial gout is frequently associated with the presence of current tophi, although not with spinal symptoms. Spine. 2014;39:1531–6.
Baer AN, Kurano T, Thakur UJ, Thawait GK, Fuld MK, Maynard JW, et al. Dual-energy computed tomography has limited sensitivity for non-tophaceous gout: a comparison study with tophaceous gout. BMC MusculoskeletDisord. 2016;17:91.
Qian X, Yang Z, Jiang Y, Xiao Z. Application of single-source dual-energy CT scanning and single-energy spectrum imaging in the diagnosis of Gout nodules. Chin J CT MRI. 2021;19:154–155+171.
Liu D. Ultrasonographic features of gouty arthritis compared with CT and MRI. Chin J CT MRI. 2020;18:150–2.
Bongartz T, Glazebrook KN, KavrosSJ, Murthy NS, Merry SP, Franz WB, et al. Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis. 2015;74:1072–7.
Ren ZQ, HE SH, ZHANG XF. Lumbar spondylolisthesis combined with unilateral facet joint rheumatoid deposition:a case report and literature review. J Spinal Surg. 2020;18:213–6.
Du M, Song Z, Liu R, Wang J. A case of ankylosing spondylitis combined with Crista Gout and Literature Review. Rheumatism Arthritis. 2020;9:41–3.
Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D, et al. 2015 gout classification criteria: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2015;67:2557–68.
Jin HJ, Son ES, Kim DH. The Frequency of Axial Deposition in Korean Patients With Gout at a Tertiary Spine Center. Original Res. 2020;7:339–45.
Bonaldi VM, Duong H, Starr MR, Sarazin L, Richardson J. Tophaceous gout of the lumbar spine mimicking an epidural abscess: MR features. AJNR Am J Neuroradiol. 1996;17:1949–52.
Yu J, Li Q, Lin J, Wang J. One case of lumbar facet gout stone and literature review. Hainan Med. 2013;24:759–60.
Tan X, Pu T, Liu J, Xu X. Diagnosis and treatment of gouty lumbar spinal stenosis. J Clin Orthopedics. 2016;19:552–4.
Dhote R, Roux FX, Bachmeyer C, Tudoret L, Daumas DC, Christoforov B. Extradural spinal tophaceous gout: evolution with medical treatment. Clin Exp Rheumatol. 1997;15:421–3.
Duprez TP, Malghem J, Vande Berg BC, Noel HM, Munting EA, Maldague BE. Gout in the cervical spine: MR pattern mimicking diskovertebral infection. Am J Neuroradiol. 1996;17:151–3.
Jacobs SR, Edeiken J, Rubin B, DeHoratius RJ. Medically reversible quadriparesis in tophaceous gout. Arch Phys Med Rehabil. 1985;66:188–90.
Koskoff TD, Morris LE, Lubic LG. Paraplegia as a complication of gout. JAMA 1953;152:37–8.
St George E, Hillier CE, Hatfield R. Spinal cord compression: an unusual neurological complication of gout. Rheumatology 2001;40:711–2.
Van de Laar MAFJ, Van Soesbergen RM, Matricali B. Tophaceous gout of the cervical spine without peripheral tophi. Arthritis Rheum. 1987;30:237–8.
Author information
Authors and Affiliations
Contributions
YY and YG contributed to the conception and design of the study, Conceptualization, Methodology, Data curation. YY wrote the paper. SY supervised the research. BZ collected the data. All authors contributed to the critical revision of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
As the retrospective nature of the study, patient consent was waived.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, Y., Guo, Y., Yu, S. et al. CT image findings of spinal gout. Spinal Cord 60, 722–725 (2022). https://doi.org/10.1038/s41393-022-00773-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00773-2