Abstract
Study design
Retrospective, cross-sectional study.
Objectives
To investigate prevalence, types, and severity of fecal incontinence (FI) and constipation in adults with spina bifida (SB), in relation to self-perception and help-seeking, and to compare findings to data from a general population reference group.
Setting
University Medical Center Groningen (UMCG), the Netherlands.
Methods
The 294 adults with SB registered at UMCG in 2017 were invited to participate. The Groningen Defecation and Fecal Continence Questionnaire was used to assess functional outcomes for FI and constipation using Rome IV criteria. Vaizey (for FI) and Agachan (for constipation) scores were determined. Socio-demographic factors and self-perception of bowel-related problems were recorded through the questionnaire. Data were compared with an age and sex matched reference group.
Results
The completed questionnaires of 112 (38%) responding participants were analyzed. FI and constipation were more prevalent in the study group (35% and 45%, respectively) than in the reference group (8.9% and 22%, respectively). In general, in participants with SB aperta (SBA; n = 75), FI was more severe than in participants with SB occulta (SBO; n = 37). However, severity of FI was higher in SBO participants than in the SBA group after the age of 61. Bowel problems in adults with SB were associated with worse self-perception regarding health.
Conclusions
In adults with SB, anorectal dysfunction is often present and severe. Older persons with SBO experience more severe FI than in early age. Bowel problems should systematically and more adequately be addressed and controlled throughout adulthood in both the spina bifida groups.
Similar content being viewed by others
Introduction
Spina bifida (SB) is a congenital defect caused by the incomplete closure of the neural tube during embryonic development [1]. Persons with spina bifida frequently experience a broad range of problems including bowel dysfunction such as fecal incontinence (FI), constipation, or both [2, 3]. Currently, the examination of persons with SB who present with bowel problems is often limited to FI and/or constipation, while the distribution of the different types of FI, the symptoms associated with constipation, the severity, and duration of bowel problems in these persons are unknown.
Furthermore, bowel problems are usually studied in the SB group as a whole, rather than distinguishing between SB aperta (SBA) and SB occulta (SBO) [3], or in only one of these SB subgroups. Of note, frequently SBO is reported as the clinically mild type of SB and SBA as the more severe type [2]. Consequently, one might assume that persons with SBA suffer more severe forms of anorectal dysfunction than persons with SBO, or that the symptoms associated with bowel problems differ between these two subgroups. In children, SBA is mainly associated with FI, and SBO with constipation [2, 4]. Adults with SBA regard FI as a problem more often than do those with SBO [2]. This finding might be related to the type and/or severity of FI. The symptomatic differences as well as the severity regarding fecal problems between spina bifida aperta and occulta have not been comprehensively investigated. The associations between the type of bowel problem and its severity in cohorts of adult with SB, including the subgroups SBA and SBO, remain unclear and have to date not been compared to the general population without SB.
To date, predictors of the presence, types, and severity of bowel dysfunction in SB have not been determined. Although a relationship between neurological impairment and bowel problems seems obvious in persons with SB, this association is not supported by current literature. Brochard and colleagues found no association between bowel dysfunction and the neurological level of the lesion, nor with the presence of hydrocephalus, agenesis of the corpus callosum, or Chiari malformation. Instead, obesity, urological disorders, and altered stool consistency appear to be major factors related to bowel dysfunction [3]. From a neurological perspective the association of bowel and bladder dysfunction seems logical. One might expect that urinary incontinence might predict the presence of bowel problems, such as FI and/or constipation. This matter has, however, not yet been settled for persons with either SBA or SBO.
In the general population, demographic factors such as age and sex are known to be related to bowel dysfunction [5]. Generally, women tend to be more prone to constipation than men and its prevalence decreases with age, while the prevalence of FI does not change with increasing age [5]. It has been reported that in persons with SB these demographic factors are also associated with the prevalence of bowel problems [2], but the relationship with the severity and type of SB is unclear. Seeing that SBA and SBO have different pathophysiological backgrounds, the type of SB may be associated with different symptoms and severity. Therefore, the predictive value of certain factors may differ between these two groups, and if true, general predictive statements should be avoided.
The primary aim of our study was to assess FI and constipation in adults with SB with regard to prevalence, subtypes, symptoms, and severity, and to compare these data with a reference group from the general Dutch population. Our secondary aim was to investigate whether factors such as the type of SB and certain demographic factors are related to the severity of FI and constipation in these persons. We also aimed to study the association of urinary incontinence as a possible predictor of bowel dysfunction. Finally, we evaluated associations between the types of SB and socio-emotional factors, including self-perception, adjustment to daily activities, and help-seeking.
Methods
Study design
This retrospective, cross-sectional cohort study was conducted at the Anorectal Physiology Laboratory (AFC) in cooperation with the Spina Bifida Team of University Medical Center Groningen (UMCG), the Netherlands.
Participants
We approached all adults with SB of 18 years and older, who were registered at UMCG, to participate. In 2017, we sent a letter of invitation to participate in the study to those persons who were alive at the time and who lived in the Netherlands. Non responders were sent a reminder letter once. After receiving their written informed consent, we sent them the validated Groningen Defecation and Fecal Continence (DeFeC) questionnaire, either on paper or digitally [6]. We excluded persons with a bowel stoma.
Controls
The control group consisted of adults from the general Dutch population who had participated in an earlier survey [6]. Originally, the group consisted of 1259 adult respondents who were described in general terms by Meinds and colleagues [6]. One of these respondents was excluded before matching on account of reportedly having SB.
Propensity score matching of the study and control groups was conducted in a 1:2 ratio based on age and sex. This sample constituted the reference group for the study.
Assessment of participants’ medical history
Participants’ medical history was collected from the medical files. It included type of SB, presence of hydrocephalus, having had detethering surgery or not, neurological level of dysfunction (classification based on neurological symptoms), and using clean intermittent catheterization (CIC).
Assessment of defecation disorders
Using the Groningen DeFeC questionnaire, we defined FI as the recurrent, uncontrolled passage of fecal material at least several times a month for the past 6 months, in accordance with the Rome IV criteria for functional FI [7]. We determined the severity of FI by calculating the Vaizey incontinence score on a of 0–24 point scale, with 0 indicating complete continence and 24 indicating complete incontinence. The Vaizey incontinence score consists of four items including incontinence for solid stool, for liquid stool and for flatus, and lifestyle alterations, which are summarized over four weeks. For each item, a score from 0 to 4 can be given, depending on the frequency. Additionally, either 0 or 2 points are given for the need to wear a pad or plug, use of constipating medication and the lack of ability to defer defecation for >15 min. The sum of these scores results in the total score, which ranges from 0 (continence), to 24 (complete incontinence). The DeFeC questionnaire contains questions regarding the aforementioned symptoms, and answers regarding the symptoms were used to calculate the scores [8].
Additionally, we distinguished the following subtypes of FI: soiling, solid FI, liquid FI, and urge FI. Soiling is the accidental passage of small, coin-sized amounts of fecal material that only stain the underwear. Solid and liquid FI is the accidental passage of large amounts of either solid or liquid feces, in the absence of urge sensation. Urge FI is either being unable to reach a toilet in time to prevent FI while feeling a strong urge to defecate, having to hurry to the toilet to prevent FI, or the inability to postpone defecation for more than 5 min after feeling the urge to defecate.
Constipation was defined in accordance with the Rome IV criteria for functional constipation [9]. To count as constipation a participant should have experienced at least two of the following symptoms during at least 25% of defecations in the last 3 months: straining, hard or lumpy stools, sensation of incomplete evacuation, sensation of anorectal obstruction, using manual maneuvers to assist in defecation, or fewer than three bowel movements a week. In addition to these symptoms, loose stools should rarely be present without the use of laxatives. The severity of constipation was determined by calculating the Agachan score on a 0–30 point scale, with 0 indicating no constipation and 30 indicating severe constipation. In case of the Agachan score, 0–4 points can be scored for frequency of bowel movements, minutes needed to sit on the toilet to defecate, painful evacuation, feeling incomplete evacuation, unsuccessful attempts for evacuation per 24 h, abdominal pain and duration of constipation and between 0 and 2 points for type of assistance [10].
Assessment of urinary incontinence
The DeFeC questionnaire also provides information on urinary incontinence (UI). We define UI as any involuntary leakage of urine during the past 6 months in accordance with the definition of the International Continence Society (ICS) [11].
Assessment of socio-emotional factors
Socio-emotional factors were assessed through answers to the DeFeC questionnaires. These include health-perception, help-seeking behavior and coping mechanisms through daily adjustments.
Statistical analysis
Continuous variables were not normally distributed and are therefore reported as median (25% and 75% percentiles). We used non-parametric test to analyze these variables. The Mann–Whitney U test was used to compare the continuous variables, while Spearman’s correlation was used to analyze the correlation between these continuous variables. To compare dichotomous variables, we used the chi-square test. We calculated the odds ratios (ORs) using regression analysis. We considered P ≤ 0.05 as statistically significant. Statistical analyses were performed using SPSS®, Version 24.0 for Windows® (IBM, Armonk, New York, USA).
Ethical approval
The study was approved by the Medical Ethical Committee of University Medical Center Groningen, the Netherlands. All participants had given their written informed consent.
Results
Patient characteristics
Of the 294 adults who had been invited to participate, 149 gave their informed consent. Subsequently, we asked them to fill out the Groningen DeFeC questionnaire [7]. The questionnaire was completed by 113 patients, which represented a response rate of 38.4%. We had to exclude one person with a bowel stoma. Thirty-one participants received and filled out the questionnaire on paper, the other 81 participants did so digitally.
Out of the 112 adults with SB included for analysis, 35 (31%) were men, 75 (67%) had SBA and 37 (33%) had SBO. Participants’ median age was 40 (27–50) years. The non-responder group did not significantly differ from the responders with respect to age and the percentages of SBA versus SBO patients. In Table 1 we present further clinical information on the participants, including enemas and/or the use of laxatives, colonic washouts, and CIC.
The group of persons with SB who had used colonic washouts, was younger than the group who did not use these (median age 29 years (23–40) versus 43 (30–55; p < 0.001)). The median age of persons using and not using laxatives or enemas, was not significantly different (36 years (27–50) versus 42 (28–51), p = 0.662).
The reference group consisted of 224 age and sex matched adults. We also list their characteristics in Table 1.
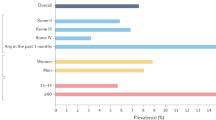
Prevalence and types of fecal incontinence
The prevalence of FI was higher in persons with SB than in the reference group, viz. 35% versus 8.9%, (OR, 5.5, 95% CI, 3.0–10.0, p < 0.001) (Fig. 1A). Multivariable analysis, in which we corrected for body mass index, urinary incontinence, colonic washouts, and laxatives and/or enemas, showed that the odds ratio for FI in persons with SB was 3.3 (95% CI, 1.6–6.8, p < 0.001) (Table 2).
In persons with SB, FI was significantly associated with a previously performed detethering (p = 0.011). In contrast, FI was associated with neither type of SB, nor urinary incontinence, nor with other factors frequently associated with this dysfunction, as specified in Table 2.
Although the prevalence of FI was not significantly higher in persons with SBA than in persons with SBO, we did observe that the distribution of different types of FI was different. Only soiling had a comparable prevalence in both the types of SB (Fig. 1A). Interestingly, FI in combination with constipation was present in the study group more often than in the reference group (p < 0.001), and in persons with SBA more often than in those with SBO (p = 0.022).
Prevalence and symptoms of constipation
In general, constipation was significantly more prevalent in the study group than in the reference group, viz. 45% versus 22%, (OR 2.9, 95% CI, 1.8–4.7, p < 0.001) (Fig. 1B). In the multivariable analysis, however, corrected for urinary incontinence and use of laxatives and/or enemas, persons with SB are not more likely to have constipation (OR 1.2, 95% CI, 0.56–2.5, p = 0.657) (Table 3).
Univariable analysis performed within the study group indicated that constipation was associated with SBA (p = 0.028), with increasing age (p = 0.036), and with the use of laxatives and/or enemas (p < 0.001). In the multivariable analysis adjusted for age and use of laxatives and/or enemas, the association between constipation and type of SB was no longer statistically significant (p = 0.093).
The association of UI with constipation in the general population (OR 2.1, 95% CI, 1.1–4.0, p = 0.026) was not found in persons with SB (p = 0.866). The prevalence of the different symptoms of constipation was not significantly related to the type of SB (Fig. 1B). Nevertheless, we did observe that persons with SBA used their hands to support defecation more often than those with SBO (43% versus 27%). Constipated persons with SBA used laxatives and/or enemas more often than persons with SBO (OR 5.6, 95% CI, 2.0–16, p = 0.001) (Table 3) and yet they still experienced having hard stools more frequently (40% versus 30%) (Fig. 1B).
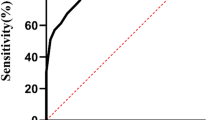
Severity fecal incontinence and constipation
In line with our expectation, both FI and constipation were more severe in persons with SB than in the general population, as was substantiated by significantly higher Vaizey and Agachan scores. Moreover, persons SBA experienced more severe FI and constipation than those with SBO (Fig. 2A, B).
Comparison of the (A) Vaizey score and (B) Agachan score between the reference group, the total spina bifida (SB) group, the spina bifida occulta (SBO) group, and the spina bifida aperta (SBA) group. Correlation of the Vaizey score and age in persons from (C) the SBA group, (D) persons from the SBO group, (E) in the reference group, and (F) in all the groups investigated. G Duration of defecation disorders in all the groups.
Although the severity of FI was similar in persons with SBA and SBO, it was more severe in older persons with SBO, as seen by the positive correlation between age and the Vaizey score (rho = 0.59, p < 0.001), which was not found in persons with SBA (Fig. 2C, D). Persons with SBO and who were older than 61 years, experienced more severe constipation than persons with SBA of the same age (Fig. 2F). In the reference group too, age and severity of FI were not correlated (Fig. 2E).
Interestingly, 34% of the persons with SBA had experienced bowel problems for 10-20 years or even longer, compared to 12% of persons with SBO for a similar timespan (Fig. 2G).
The severity of FI was not associated with UI (data not shown). There was no association between severity of constipation and UI and any of the aforementioned factors (data not shown).
Association between bowel dysfunction and socio-emotional factors
Persons with SB discussed their FI significantly more often with others than did members of the reference group (p = 0.014, Fig. 3A). Persons with SBA and SBO qualified their health in relation to bowel function significantly worse than the general population (Fig. 3B). The association between constipation and self-perception of health in relation to bowel function was significant in persons with SB (p < 0.001). We found no such association for FI (p = 0.223).
A With whom participants/respondents discussed their defecation disorders. B Qualification of one’s own health regarding defecation. C Prevalence of adjusting daily activities on account of defecation disorders. Abbreviations: SB persons with spina bifida, SBO persons with spina bifida occulta, SBA persons with spina bifida aperta.
Similarly, the prevalence of daily adjustments to FI was higher in the study group than in the reference group (40% versus 18%, p = 0.006), without a clear difference between persons with SBO and those with SBA (30% versus 44%) (Fig. 3C).
There was a significant association between a hydrocephalus and the educational level of persons with SB (p = 0.002). There was, however, no significant association between FI and either the presence of hydrocephalus or educational level (p = 0.621 and p = 0.467, respectively).
Other factors related to bowel dysfunction
In our cohort, 10 (8.9%) persons with SB had no neurological deficit, where one of these 10 persons had a meningomyelocele, two had meningocele, and the remaining seven persons had SBO. Of these ten patients without neurological deficit, three experienced FI (one having meningomyelocele and two spina bifida occulta) and four experienced constipation (one having meningocele and one myelomeningocele). These 10 patients had significantly lower FI severity as indicated by the Vaizey scores (median 3.5 (1.8–8.8) versus 8 (4–11), p = 0.039) than the rest of the patient group, but they had similar constipation severity, as indicated by comparable Agachan scores (median 4 (2–7.8) versus 4.5 (2–9.3), p = 0.459).
In our cohort 22 (20%) persons with SB reported using anticholinergic medication for bladder dysfunction. There was no association between the medication use and either FI or constipation.
Discussion
In this study we show that FI is highly prevalent in adults with SB, and more severe than in the general population. Although the prevalence of FI in persons with SBO and those with SBA is comparable, it is more severe in the latter. Moreover, severity of FI is correlated with increasing age in persons with SBO, but not in those with SBA.
Constipation is also more prevalent and more severe in persons with SB than in the general population. Although persons with SBO are less likely to suffer from constipation than persons with SBA, persons in the SBO group still tend to be constipated more often than the general population.
We know from previous studies that persons with SB experience defecation disorders and our findings corroborate the previous studies [2, 3]. Such findings, however, based only on the prevalence of these problems in a certain patient cohort, do not illustrate their real magnitude. Because we know that bowel problems also occur in the general population, we found it important to compare the patient cohort to the general Dutch population. Such a comparison was possible because we screened both the general Dutch population and this cohort of persons with SB using the Groningen DeFeC questionnaire [5]. The prevalence of bowel dysfunction in our SB cohort was lower than in a previous study [3]. This may be the result of the difference in study design and the use of different criteria for FI and constipation. Brochard and colleagues used multiple criteria for these conditions including the Neurogenic Bowel Dysfunction Score, aimed specifically at neurogenic causes of bowel dysfunction [11]. We used the Rome IV criteria for functional FI and constipation to compare it to the general population where these causes might be less prevalent.
When considering the different types of SB separately, in general bowel dysfunction in the SBO group is less prominent than in persons with SBA. Nevertheless, the prevalence of FI and constipation is higher in both, the SBO and SBA, subgroups when compared to the reference group. Interestingly, the severity of FI in persons with SBA is equally distributed along respondents with different age, while in persons with SBO the severity of FI is higher in older respondents than in younger. Importantly, persons with SBO older than 60 years have more severe FI than persons with SBA. Of note, persons with SBA reported having bowel problems for 10–20 years approximately four times more often than persons with SBO. Moreover, persons with SBA reported experiencing bowel problems for more than 20 years approximately two times more often than persons with SBO. By contrast, persons with SBO reported having bowel problems for the last year approximately four times more often than persons with SBA. It seems thus, that persons with SBO develop fecal problems at later age that SBA. This in turn, indicates that development of fecal problems in people with SBA and SBO has a different dynamic and maybe even a different pathophysiological cause. This finding advocates our choice to analyze the bowel problems in SBA and SBO separately.
One might think that the more severe FI found by us in the older people with SBO could result from the fact that use of colon-washouts in persons with SB to prevent FI has only become a common practice in the last 15–20 years. However, if this was true, then the same effect should be observed in persons with SBA, unless fecal problems had been underestimated especially in persons with SBO, which could eventually lead to undertreatment.
This observation provides a clinically relevant argument that not only persons with SBA, but also those with SBO, require regular medical consultation for screening of bowel functions and recommending adequate treatment, such as colonic washouts, pharmacological treatment, or perhaps pelvic floor physiotherapy. Further physiological research, preferably in the form of a longitudinal study, should be conducted to assess the efficacy of these therapies in persons with SB. Furthermore, we also show that although the prevalence of constipation is not associated with age in persons with SBO, it is lower in older persons with SBA and in the general population than in the younger generation. Perhaps this was caused by better coping strategies developed with increasing age or perhaps by the same unknown mechanism that may contribute to the increased severity of FI in older persons with SBO.
Finally, although we found an association between the prevalence and severity of FI and constipation, and urinary incontinence in the reference group, we did not find such an association in either the total SB group or in the SBO and SBA subgroups. On account of the high number of participants using CIC, we corrected this outcome for such cofactors using multivariable regression analysis. No significant association was found. These association differences between the study and reference groups might indicate that these problems involve different pathophysiological mechanisms in persons with SB than in the general population. In other words, urinary incontinence seems not to be a predictor of bowel dysfunction in persons with SB. The Groningen DeFeC questionnaire, however, only contains a limited number of questions regarding urinary problems. These allowed us to use the ICS definition of urinary incontinence to determine whether there is a urinary problem [12], but they do not provide sufficient information to describe their magnitude and severity. Moreover, since information on CIC was acquired through medical files instead of the questionnaire, we cannot be sure that participants were using CIC or were using it properly at the time of filling out the questionnaire. The data on CIC in the medical files was often missing in these persons who are not systematically seen at our center anymore. We consider this a limitation of our study.
Because we only included persons who were registered at our hospital, it is possible that we included persons with the most severe forms of SB, which may have led to selection bias such as for instance overestimation of the prevalence of fecal problems. This counts especially for persons with SBO, who may even go undiagnosed for bowel dysfunctions on account of the generally milder symptoms. Additionally, it is possible that only persons with more severe complaints responded to our invitation and filled out the DeFeC questionnaire. It may have resulted in a selection bias.
Another limitation of this study is the relatively low response rate. This might be caused by the fact that for this study we had invited all the persons who had ever been registered at our hospital as having SB. This cohort however includes persons who do and do not undergo regular controls at our hospital. Usually persons with SB who are not under control of the medical specialist have no or less severe symptoms, and this might contribute to decreased motivation to participate in this study.
Defecation problems have considerable impact on the lives of persons with SB. More than 40% of the participants in this study reported having to adjust their daily activities to cope with their problems and more than half of these persons qualify their general health regarding defecation as moderate or worse. Bowel dysfunction therefore remains a problem in persons with SB, even though it can be treated. Despite difference in prevalence of bowel dysfunction between the SBA and SBO subgroups, the percentage of persons who consider their bowel function as poor is comparable between these two groups. Interestingly, despite these problems many persons with SB do regard their health situation as good or reasonable, suggesting effective coping mechanisms and unawareness of possible treatment strategies. This has also been observed before in people with bowel dysfunction in the general population [5].
Intellectual disability of persons with SB, occurring more frequently in those with hydrocephalus [13], might influence the ability to master continence techniques. Although the DeFeC questionnaire does not contain questions on the cognitive capabilities, it does contain information about educational level, which we show to be associated with hydrocephalus. In our cohort however neither hydrocephalus nor education level are associated with being fecal incontinent.
This study clearly indicates that many adults with SB suffer from bowel dysfunction, also at older ages, and therefore, regular medical consultation that focuses on bowel dysfunction should be continued to provide adequate treatment if necessary. Treatment options for bowel dysfunction frequently include use of laxatives, colonic washouts and pelvic floor physiotherapy. Future studies should determine which treatments are most effective for each different cause of bowel dysfunction in these patients.
Conclusion
The prevalence and magnitude of bowel problems, including FI and constipation, is considerably higher in persons with SB than in the general population. Although persons with SBA suffer from bowel problems more often than SBO, older persons with SBO experience more severe FI than in early age. Urinary incontinence should not be considered a predictor of bowel dysfunction in persons with SB. Our findings indicate the need for regular screening of bowel functions in both adults with SBA or SBO, so that they can receive proper care, if necessary. Bowel problems should systematically and more adequately be addressed and controlled throughout adulthood in both the spina bifida groups.
Data availability
Additional data is available from the corresponding author on reasonable request.
References
Verhoef M, Lurvink M, Barf HA, Post MWM, Van Asbeck FWA, Gooskens RHJM, et al. High prevalence of incontinence among young adults with spina bifida: Description, prediction and problem perception. Spinal Cord. 2005;43:331–40.
Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM, et al. Spina bifida. Nat Rev Dis Prim. 2015;1:15007.
Brochard C, Peyronnet B, Dariel A, Ménard H, Manunta A, Ropert A, et al. Bowel dysfunction related to spina bifida: keep it simple. Dis Colon Rectum. 2017;60:1209–14.
van Meegdenburg MM, Heineman E, Broens PMA. Pudendal neuropathy alone results in urge incontinence rather than in complete fecal incontinence. Dis Colon Rectum. 2015;58:1186–93.
Meinds RJ, van Meegdenburg MM, Trzpis M, Broens PM. On the prevalence of constipation and fecal incontinence, and their co-occurrence, in the Netherlands. Int J Colorectal Dis. 2017;32:475–83.
Meinds RJ, Timmerman MEW, van Meegdenburg MM, Trzpis M, Broens PMA. Reproducibility, feasibility and validity of the Groningen Defecation and Fecal Continence Questionnaires. Scand J Gastroenterol. 2018;53:790–6.
Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, et al. Bowel disorders. Gastroenterology.2016;S0016-5085:00222–5.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut.1999;44:77–80.
Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, et al. Functional anorectal disorders. Gastroenterology.2016;S0016-5085:00175–X 10.1053.
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39:681–5.
Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord. 2006;44:625–31.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology.2003;61:37–49.
Alimi Y, Iwanaga J, Oskouian RJ, Loukas M, Tubbs RS. Intelligence quotient in patients with myelomeningocele: a review. Cureus.2018;10:e3137.
Acknowledgements
The authors acknowledge E. Visser, PhD of RoQua (Routine Outcome and Quality Assessment) for helping to process the data of the questionnaires. We also thank all participants who took part in this study.
Author information
Authors and Affiliations
Contributions
NW collected participants’ data, analysed the data, interpreted the results and wrote the manuscript. FH collected the participants’ data. GJFJ Bos and OFB provided feedback during this process. MT helped interpreting results and provided feedback on the manuscript. PMAB was the principal investigator of the study and helped interpreting results and provided feedback on the manuscript. All authors participated in designing and providing feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the research committee of University Medical Center Groningen, the Netherlands (MCG (METc 2016.162). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Wild, N., Herrmann, F., Bos, G.J.F.J. et al. Anorectal dysfunction in adults with spina bifida and associated socio-emotional factors—a retrospective, cross-sectional cohort study. Spinal Cord 60, 679–686 (2022). https://doi.org/10.1038/s41393-022-00754-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00754-5