Abstract
Study design
Participant-blinded comparative pre-post randomized controlled trial.
Objective
To evaluate the effects of virtual soccer game on balance, gait function, and kick speed in individuals with spinal cord injuries.
Setting
Forty participants with incomplete spinal cord injury (SCI) were included.
Methods
The participants were randomized into either an experimental group (EG) or a control group for treatment 3 days/week over 4 weeks. The clinical outcomes included the results of the chair stand test (CST), timed up-and-go (TUG) test, and 10 m walking test (10MWT). The virtual reality (VR) content outcome measure was kick speed.
Results
The independent t-test results indicated that the participants in the EG exhibited superior performances in the CST, TUG test, 10MWT, and kick speed test (all P < 0.05).
Conclusions
Our results provide novel, promising clinical evidence that VR rehabilitation improves both dynamic and static balance and reduces the risk of falls in patients with incomplete SCI of Asia impairment scale grades C–D.
Similar content being viewed by others
Introduction
The number of people living with spinal cord injury (SCI) worldwide is increasing owing to the development of transportation systems and industries. The incidence of SCI and injury patterns vary considerably across world regions in relation to resource levels; geographic, demographic, and socioeconomic factors; and changes occurring due to the aging of populations, with increased injuries due to falls and non-traumatic causes [1]. Sitting or standing balance and gait impairments resulting from losses of sensation and muscle strength in parts of the body below the level of the injury due to loss of motor function are considered major causes of decreased quality of life in people with SCI [2,3,4]. Trunk control is essential to the arm and leg movements of neurologically normal individuals [5]. However, individuals with SCI lose their ability to activate the trunk muscles related to arm and leg movements. The level (and extent) of injury indicates the deficit in trunk control coordination, which in turn affects trunk stability and maximum hand reach distance but may not necessarily affect other arm movement patterns such as those in wheelchair propulsion. This results in the compensatory action of the quadriceps muscles to support trunk function or even replace the role of the trunk during walking or standing [6]. Therefore, quadriceps muscle training rehabilitation can enhance the walking and balance functions of individuals with incomplete SCI. Previous studies showed that strengthening the quadriceps, hamstring and gluteus muscles of individuals with SCI are effective for enhancing their walking and balance functions [7]. To activate the quadriceps muscles of patients with SCI, electrical stimulation at a frequency of ~20 Hz is typically applied [8]. However, the consequent physiological changes of the quadriceps muscles result in increased resistance to fatigue with training or frequency of electrical stimulation [8].
To mitigate the inherent problems of conventional physiotherapy, innovative user and computer interactive training systems designed to provide repetitive, task-specific, and motivative exercises were developed using virtual reality (VR) technology [9, 10]. Therefore, intrinsic motivation is especially important for individuals with SCI to better understand the necessity of rehabilitation and achieve rehabilitation goals. VR systems reduce risks and provide patients the opportunity to safely experience activities that they would not otherwise experience in real life [11, 12]. To compensate for patients’ inability to participate in such experiences in real life, VR, a computer-generated three-dimensional artificial environment that simulates reality, is used. VR allows users to have various experiences intuitively by creating an illusion in a virtual space through the interaction between the computer and the user [13]. Furthermore, the auditory and visual effects of VR content can deeply immerse and intrigue patients [14].
In a previous study, Villiger et al. observed that after 4 weeks of VR, pain intensity and measures of balance, endurance, motor skill, and independence showed improvements in 14 individuals with incomplete SCI [15]. In the present study, VR content was proposed to minimize the intervention of therapists and allow patients with incomplete SCI to voluntarily participate in rehabilitation processes by applying game elements that motivate them as tools for triggering behavioral change [16, 17]. The specific aim of the present study was to examine the effects of VR rehabilitation on dynamic and static balance and the risk of falls, and the effects of VR content on outcomes in patients with incomplete SCI.
Methods
Participants
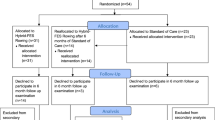
A total of 40 participants with incomplete SCI were recruited from a SCI rehabilitation support center in Gyeonggi, Korea. The participants were randomly classified into an experimental group (EG) and a control group (CG). Each group was composed of 20 participants and received interventions. The study was approved by the university Institutional Review Board (IRB No. 2020-03-004-002) before any activities related to the study were started. The present study had a randomized, single-blinded experimental design where patients were randomly assigned to either the control or EG through a random allocation sequence method using the Excel program. To reduce or eliminate the experimental biases associated with the participants’ expectations, experimental information that might affect the participants was masked until the completion of the experiment. The inclusion criteria were as follows: (1) chronic, clinically incomplete SCI (time since injury > 1 year); (2) C5 to C7 SCI and manual muscle test (MMT) grade > 3 for quadriceps muscle strength; (3) no knee range-of-motion (ROM) limitation; (4) motor-incomplete SCI (grade C or D) classified according to the International Standards for Asia Impairment Scale; (5) lower extremity weight-bearing (standing and/or walking) as part of the typical activities of daily living and medical clearance to participate; (6) patients who can perform the 10MWT at least twice; and (7) lower extremity motor score ≥ 20. The exclusion criteria were (1) surgery in the last 6 months, (2) musculoskeletal disorders such as bone fracture or contracture, (3) bone instability (non-consolidated fractures, unstable spinal column, or severe osteoporosis requiring treatment with bisphosphonates), or (4) other neurodegenerative disorders (e.g., amyotrophic lateral sclerosis or Parkinson’s disease).
Interventions
The participants in both groups received 12 sessions of a 30 min therapy 3 days/week for 4 weeks in their homes. Evaluations using the MMT, chair stand test (CST), timed up-and-go (TUG) test, 10 m walk test (10MWT), and ROM test were performed before and after each session. A physical therapist (CP) performed the MMT and ROM test in each participant for seven lower limb muscle groups (hip flexors/extensors/abductors, knee flexors/extensors, ankle dorsiflexors, and plantar flexors) in standardized patient positions [18]. The MMT was used to determine the knee extensor strength in the standard MMT position, which is sitting on a chair while actively extending the knee. The performance in each test was rated between grade 0 (no movement and contraction) and grade 5 (full ROM against gravity with maximal resistance). The participants in the EG underwent rehabilitation while sitting in a wheelchair and wearing a head-mounted display (HMD) and input devices that recognize lower limb motions in both legs. Audiovisual signals were delivered to the participants via the sound effects in the VR content. The participants were asked to lift their legs as they received the signals, which were delivered to them with every approaching virtual ball. According to the participant’s condition for 30 min, knee extension exercises must be performed 20 times, that is, 10 times for each leg in random order.
By contrast, the participants in the CG underwent rehabilitation without the VR content. They underwent rehabilitation while sitting in a wheelchair and wearing input devices that recognize lower limb motions. The exercise program for the participants in the CG included lowering the leg immediately after extending the knee and lowering the leg after extending the knee and holding it for at least 3 s as indicated by a certified physical therapist. These movements were repeated ten times, with two sets for each leg. The devices that the participants wore on their legs were used to collect the data for the study (Fig. 1).
Chair stand test
The CST was used to examine stability and balance control during a pattern of repeated sit-to-stand movements. The participants sat on an armless chair, with their arms on the sides, their back upright, 90° hip flexion, and their feet flat on the floor at 10 cm behind the knees. Then, they were instructed to stand up with the hips and knees in full extension and sit down five times as quickly and safely as they could without using the arms. In this test, the time from the command “Go!” until the participant’s back touched the backrest of the chair on the fifth repetition was recorded [19, 20]. The reliability and validity of the CST was well established in a previous study [21].
Timed up-and-go test
The TUG test was used to examine the risk of falls. It was started by having the participant sit back in a chair. Then, the participant rose from the chair, walked 3 m, turned around, walked back to the chair, and sat down. The time taken by the participant to complete the test was measured, and participants who took <10 s to complete the task were classified as normal, whereas those who took 10–20 s to complete the task were classified as somewhat mobile, and those who required >20 s were classified as individuals in urgent need of caregiver help [19, 20, 22]. The TUG test, which is a valid measure that correlates well with the Berg Balance Scale, safety in community ambulation, and 10MWT.
Ten-meter walk test
The 10MWT is a performance measure used to assess walking speed in meters per second over a short distance. It can be used to determine functional mobility, gait, and vestibular function [19, 23, 24].
Creation of the VR content
Users of the VR content performed motions while seated in a wheelchair by using a HMD, input devices that recognize lower limb motion, and a base station than recognizes user motions. The base stations detected the VR users’ locations and allowed them to navigate and communicate with their avatars in the virtual world. If the user made motions and these motions were recognized by the base station, their avatar made exactly the same motions in the virtual world; as a result, users could become more immersed in the virtual activity.
In the VR content created for the rehabilitation, two kinds of balls, a soccer ball and an iron ball, approached the participant. Special approaches to design were adopted for these balls. Whereas the soccer ball was designed to make one want to kick the ball, the iron ball was designed to make one want to avoid it by lifting a foot. No explanation was required to elicit these feelings from the participants. In the VR content, 20 balls rolled toward the participant over a maximum of period of 1 min. Specifically, ten balls rolled toward the left foot, and another ten rolled toward the right foot, in random order and at random times. For each foot, eight soccer balls and two iron balls were allocated. The participants gained one point for each virtual soccer ball they kicked but lost one point if they failed to raise their foot within 3 s of the ball’s arrival. Conversely, the participants gained one point for each iron ball they avoided by lifting their leg within 3 s of the iron ball’s arrival and holding that leg in the air for 3 s. They lost one point for each iron ball they failed to avoid (Fig. 2).
Development of an input device that recognizes lower limb motions
An Arduino microcontroller and two gyroscopes formed an input device that recognizes lower limb motions and was used in the study. The input devices were attached to the participant’s tibia, located 5 cm above each malleolus on the inner side and parallel to the gyroscopes. The gyroscopes were used as data-collecting instruments that interacted with the VR content by using serial communication. The data on the location of each lower limb were updated at a speed of 1 ms. Therefore, the data on both lower limbs were received at a speed of 2 ms. In addition, the data were transmitted in real time at 500 Hz. The avatar’s motions in VR were embodied in accordance with the data received from the input devices. To complete the task with their avatars, the participants must move their lower extremities on both sides.
Kick speed
The participants performed knee extension by kicking a ball toward the displayed lines. For each hit, the participant received a score reward. This exercise required the participants to tilt the lower leg and thus trained knee extension without direct measurement of the knee angle. To minimize the learning effect between the EG and the CG, the kick speed measurement test was used with VR content different from that used in the training during the VR intervention in the EG.
Statistical analysis
All results are shown as mean and standard deviation. Under the assumption of a normal distribution, all continuous variables were analyzed using the Kolmogorov–Smirnov test. The paired and independent t-tests were used to compare data within and between the groups, respectively. A power analysis was performed using G*Power (Franz Faul, University of Kiel, Kiel, Germany) to calculate the minimum sample size required (N = 36), on the basis of the findings of our pilot study. To achieve a power of 0.80 and an effect size of 0.69, a sample size of 30 was required, calculated from a pilot study of four subjects by using a partial η2 value of 21 at a significance level of 0.05. In addition, the independent t-test was used to determine all the changes associated with the use of each measure. The statistical analysis was performed using SPSS 25.0 for Windows (SPSS Inc., Chicago, IL, USA). The data were trimmed because of the presence of an outlier and missing data. In addition, the differences between the two groups were quantified, and the actual significance levels of the variables were measured using the effect size.
Results
The participants’ characteristics are shown in Table 1. In the two groups, the participants’ quadriceps muscle strengths, heights, and ages were determined to analyze the homogeneity of variances between them. Test results with P values > 0.05 demonstrated group homogeneity.
Clinical outcomes
Chair stand test
The independent t-test results showed significantly greater decreases in CST times (P < 0.05) and greater difference between pre- and post-intervention in the EG than in the CG, which suggests improved static balance in the participants with incomplete SCI in the EG. The observed effect size (Cohen’s d = 0.71) can be classified as large (Table 2).
TUG test
The independent t-test result showed significantly greater decreases in the TUG test time (P < 0.05) and greater difference between pre- and post-intervention in the EG than in CG, indicating a greater decrease in the risk of falls. The observed effect size (Cohen’s d = 0.42) can be classified as medium (Table 3).
Ten-meter walking test
The independent t-test result showed significantly improved 10MWT scores (P < 0.05) and greater difference between pre- and post-intervention in the EG than in the CG, indicating a greater increase in dynamic balance. The observed effect size (Cohen’s d = 0.61) can be classified as medium (Table 4).
VR content outcomes
Kick speed
The increase in kick speed gained by the participants in the EG and CG during the time that they used the VR content for exercise was significant (P < 0.05). The Fig. 3 shows that the difference between pre- and post-intervention was greater in the EG than in the CG. A statistically significant difference was found between the two groups in terms of the effect of the intervention between the EG and the CG. The observed effect size (Cohen’s d = 0.307) can be classified as small (Fig. 3), which suggests a greater increase in the velocity of the lower limb movement in the EG than in the CG.
Discussion
According to the results of the tests conducted after the interventions, the performances of the participants in both the EG and CG improved in each category compared with their performances before the intervention. However, a statistically significant difference was found between the EG and the CG. The present randomized controlled study is the first clinical study to highlight the positive effects of a VR intervention on static and dynamic balance and kick speed. We can conclude that rehabilitation programs that use VR content could be used to create an environment in which participants can independently undergo rehabilitation with less help from rehabilitation therapists, as such programs improve quadriceps muscle function and ultimately lead to improvement in patients’ performance in activities of daily living, similarly to rehabilitation programs that use verbal directions from therapists. The overall muscle strength and coordination improvements of the quadriceps muscles might have allowed patients with SCI to walk faster and gain stability (10MWT and balance scale improvement) [15, 25].
During exercise using the VR content, the participants in the EG were provided with audiovisual stimuli that made them feel as though they were in an environment in which balls were rolling toward them. By contrast, the patients in the CG received minimal help from experts and exercised while following verbal directions that were given to guarantee their safety. Thus, the results can be interpreted such that the difference between the groups was due to differences in the level of immersion and the audiovisual stimuli provided by the VR system. VR technologies provide users with specific stimuli that contribute to the creation of an environment that attracts users and helps them concentrate without distractions. Intrinsic and extrinsic motivational mechanisms are also provided by VR technologies [26]. Furthermore, an immersive and interactive VR system prompts users to develop their imagination. Therefore, this treatment method enables patients to concentrate on their treatment longer than they could when traditional treatments are used [27].
According to the study by Sternad [28], limitations that arise from more complicated technical challenges can be overcome with virtual environments because they permit experimenters to control the physics of an object so that it can be rendered and confined exactly to the variables and parameters under analysis. In addition, the result of a brainwave test using VR technologies showed increased activation of the posterior cingulate cortex, which is involved in emotions such as joy and interest [28]. Virtual environments improve one’s motor abilities by activating motor areas [29], which leads to extraordinarily increased activation of brain regions associated with sensory perception [29]. VR has been found to be effective in relieving depression in participants with SCI and in motivating them to express their emotions comfortably [29]. In addition, VR training improves balance, spatial orientation capacity, and motor skills by activating the prefrontal, parietal, and motor cortices and other cortical networks and by inducing the reorganization of neurons in the cerebral cortex [29]. Studies have found that VR increased the oxygen levels in the prefrontal cortex during a series of gradual balance trainings [26]. A multimodal sensory stimulus causes neural bombing on the damaged spinal cord to elicit neurophysiological and structural reorganizations of the relevant pathways [30, 31].
The VR content used in this study was developed to reduce the role of the therapist in rehabilitation processes for participants with incomplete SCI. The content induced the active participation of the participants in rehabilitation exercises, which improved quadriceps muscle performance and patient performance in activities of daily living [28]. In this study, the effects of the virtual environment on psychological aspects and the differences in performance levels in rehabilitation processes that resulted from these effects were not thoroughly investigated because the testing conducted in the study mainly focused on improvements in quadriceps femoris muscle performance and patient performance in activities of daily living after the intervention. In previous review studies, all the studies that analyzed the effects of VR interventions on functional performance and balance obtained significant results in outcome measures. It should be emphasized that the positive results obtained in the present study could have an impact on clinical neurorehabilitation, as the participants with SCI usually presented severe limitations in their participation and performance of activities of daily living. Furthermore, the inclusion of VR interventions in clinical practice could improve patient motivation and treatment adherence and performance in different activities in safe virtual environments and provide feedback and task-oriented training [32, 33]. However, psychological factors, which affect the level of immersion of participants with incomplete SCI in virtual environments, and their effects have not been sufficiently studied. Therefore, additional studies are required to analyze the rehabilitation process using VR content and psychological factors. In addition, if methods such as electromyography were adopted, differences in the level of quadriceps muscle activation and the effects of VR content on patient rehabilitation could be better understood. VR is a useful tool for health-care providers to assess and provide health services to their patients, but its application as a therapeutic tool for patients with incomplete SCI of International Standards for Neurological Classification of SCI grade C to D is still limited.
Several limitations of the present research should be considered in future investigations. One of the main limitations is that although we extensively measured the patients’ performance parameters in the CST, TUG test, and 10MWT, the underpinning mechanism of neuroplasticity changes was not investigated because of the lack of quantitative measuring equipment for assessing neuroplasticity. Future studies should develop advanced imaging tools for measuring VR-induced neuroplasticity changes during and after VR training in participants with SCI. Another limitation is that although the present results are promising, they should be interpreted with caution when extrapolating the present findings to clinical practice and to the management of patients with SCI undergoing rehabilitation because of the small sample size. Nevertheless, the results of our effect size analyses and the accumulated results of the VR rehabilitation in the participants with SCI indicate that consistent use of VR intervention demonstrated advantageous effects on gait, balance, and kick speed. In addition, further clinical research is warranted to investigate possible multifactorial interventions for cardiopulmonary function, depression, and motor function in patients with SCI.
Conclusion
This clinical research study demonstrated that VR rehabilitation was more effective than rehabilitation without VR content for improving balance, gait function, and kick speed in the participants who were recovering from incomplete SCI. The present results provide clinical evidence-based insights into the utilization of VR technology to maximize the recovery of the balance, gait function, and kick speed of patients with incomplete SCI during neurorehabilitation.
Data availability
The datasets generated and/or analyzed in the present study are available from the corresponding author on reasonable request.
References
Thompson C, Mutch J, Parent S, Mac-Thiong JM. The changing demographics of traumatic spinal cord injury: an 11-year study of 831 patients. J Spinal Cord Med. 2015;38:214–23.
Serra-Ano P, Pellicer-Chenoll M, Garcia-Masso X, Brizuela G, Garcia-Lucerga C, Gonzalez LM. Sitting balance and limits of stability in persons with paraplegia. Spinal Cord. 2013;51:267–72.
Raab K, Krakow K, Tripp F, Jung M. Effects of training with the ReWalk exoskeleton on quality of life in incomplete spinal cord injury: a single case study. Spinal Cord Ser Cases. 2016;2:15025.
Sliwinski MM, Akselrad G, Alla V, Buan V, Kimberlin E. Community exercise programing and its potential influence on quality of life and functional reach for individuals with spinal cord injury. J Spinal Cord Med. 2020;43:358–63.
Milosevic M, Masani K, Kuipers MJ, Rahouni H, Verrier MC, McConville MV, et al. Trunk control impairment is responsible for postural instability during quiet sitting in individuals with cervical spinal cord injury. Clin Biomech (Bristol, Avon). 2015;30:507–12.
Gorassini MA, Norton JA, Nevett-Duchcherer J, Roy FD, Yang JF. Changes in locomotor muscle activity after treadmill training in subjects with incomplete spinal cord injury. J Neurophysiol. 2009;101:969–79.
Crozier KS, Cheng LL, Graziani V, Zorn G, Herbison G, Ditunno JF. Spinal cord injury: prognosis for ambulation based on quadriceps recovery. Paraplegia. 1992;30:762–7.
Gerrits HL, de Hann A, Sargeant AJ, Dallmeijer A, Hopman MT. Altered contractile properties of the quadriceps muscle in people with spinal cord injury following functional electrical stimulated cycle training. Spinal Cord. 2000;38:214–23.
Levin MF, Weiss PL, Keshner EA. Emergence of virtual reality as a tool for upper limb rehabilitation: incorporation of motor control and motor learning principles. Phys Ther. 2015;95:415–25.
Shin JH, Ryu H, Jang SH. A task-specific interactive game-based virtual reality rehabilitation system for patients with stroke: a usability test and two clinical experiments. J Neuroeng Rehabil. 2014;11:1–10.
Kizony R, Raz L, Katz N, Weingarden H, Weiss PK. Video-capture virtual reality system for patients with paraplegic spinal cord injury. J Rehabil Res Dev. 2005;42:595–608.
Villiger M, Bohli D, Kiper D, Pyk P, Spillmann J, Meilick B, et al. Virtual reality–augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabil Neural Repair. 2013;27:675–83.
Miguel-Rubio AD, Rubio MD, Salazar A, Camacho R, Lucena-Anton D. Effectiveness of virtual reality on functional performance after spinal cord injury: A systematic review and meta-analysis of randomized controlled trials. J Clin Med. 2020;9:2065.
Alashram AR, Padua E, Hammash AK, Lombardo M, Annino G. Effectiveness of virtual reality on balance ability in individuals with incomplete spinal cord injury: a systematic review. J Clin Neurosci. 2020;72:322–7.
Villiger M, Bohli D, Kiper D, Pyk P, Spillmann J, Meilick B, et al. Virtual reality-augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabil Neural Repair. 2013;27:675–83.
Putz C, Alt CD, Wagner B, Gantz S, Gerner HJ, Weidner N, et al. MR defecography detects pelvic floor dysfunction in participants with chronic complete spinal cord injury. Spinal Cord. 2020;58:203–10.
Weiss PL, Rand D, Katz N, Kizony R. Video capture virtual reality as a flexible and effective rehabilitation tool. J Neuroeng Rehabil. 2004;1:12.
Kendall FP, McCreary EK, Provance P, Rodgers M, Romani W. Muscles: Testing and function, with posture and pain (Kendall, Muscles). 2005.
An YS, Jeong HY, Lee WJ, Park CH, Cho JD. Virtual reality rehabilitation contents for improving quadriceps muscle strength in patient with incomplete spinal cord injury: a case study. KSDS Conf Proc. 2019;5:144–9.
Poncumhak P, Saengsuwan J, Kamruecha W, Amatachaya S. Reliability and validity of three functional tests in ambulatory patients with spinal cord injury. Spinal Cord. 2013;51:214–7.
Khuna L, Thaweewannakij T, Wattanapan P, Amatachaya P, Amatachaya S. Five times sit-to-stand test for ambulatory individuals with spinal cord injury: a psychometric study on the effects of arm placements. Spinal Cord. 2020;58:356–64.
Podsiadlo D, Richardson S. The timed “up&go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8.
Bloem BR, Marinus J, Almeida Q, Dibble L, Nieuwboer A, Post B, et al. Measurement instruments to assess posture, gait, and balance in P arkinson’s disease: Critique and recommendations. Mov Disord. 2016;31:1342–55.
Amatachaya S, Naewla S, Srisim K, Arrayawichanon P, Siritaratiwat W. Concurrent validity of the 10-meter walk test as compared with the 6-minute walk test in patients with spinal cord injury at various levels of ability. Spinal Cord. 2014;52:333–6.
Kim CM, Eng JJ, Whittaker MW. Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord. 2004;42:156–62.
Howard MC. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput Hum Behav. 2017;70:317–27.
Baumgartner T, Valko L, Esslen M, Jancke L. Neural correlate of spatial presence in an arousing and noninteractive virtual reality: an EEG and psychophysiology study. Cyberpsychol Behav. 2006;9:30–45.
Sternad D. From theoretical analysis to clinical assessment and intervention: three interactive motor skills in a virtual environment. 2015 International Conference on Virtual Rehabilitation (ICVR). IEEE; 2015:265–72. https://doi.org/10.1109/ICVR.2015.7358579.
Prasad S, Aikat R, Labani S, Khanna N. Efficacy of virtual reality in upper limb rehabilitation in patients with spinal cord injury: a pilot randomized controlled trial. Asian Spine J. 2018;12:927.
Taylor DM, Schwartz AB. Using virtual reality to test the feasibility of controlling an upper limb FES system directly from multiunit activity in the motor cortex. In Proceedings of the 6th Annual IFESS Conference: 2001 June 16–20; Cleveland. 2001:132–4.
Jang SH, You SH, Hallett M, Cho YW, Park CM, Cho SH, et al. Cortical reorganization and associated functional motor recovery after virtual reality in patients with chronic stroke: an experimenter-blind preliminary study. Arch Phys Med Rehabil. 2005;86:2218–23.
Khurana M, Walia S, Noohu MM. Study on the Effectiveness of Virtual Reality Game-Based Training on Balance and Functional Performance in Individuals with Paraplegia. Top Spinal Cord Inj Rehabil. 2017;23:263–70.
Miguel-Rubio AD, Rubio MD, Salazar A, Moral-Munoz JA, Requena F, Camacho R, et al. Is Virtual Reality Effective for Balance Recovery in Patients with Spinal Cord Injury? A Systematic Review and Meta-Analysis. J Clin Med. 2020;9:2861.
Author information
Authors and Affiliations
Contributions
CP and YA were involved in the study design; performed the analysis; and wrote and revised the paper. YA performed the experiments and collected and analyzed data. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
An, Y., Park, C. The effects of virtual soccer game on balance, gait function, and kick speed in chronic incomplete spinal cord injury: a randomized controlled trial. Spinal Cord 60, 504–509 (2022). https://doi.org/10.1038/s41393-021-00745-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00745-y