Abstract
Study design
Validation cross-sectional study.
Objectives
To develop and assess the psychometric properties of two instruments based on the middle-range theory of self-care in chronic illness: the Self-Care in Spinal Cord Injuries Inventory (SC-SCII) and the Self-Care Self-Efficacy Scale in Spinal Cord Injuries (SCSES-SCI).
Setting
Multicenter study in five spinal units across Italy and Ireland.
Methods
Instrument development was based on self-care behaviours identified in the scientific literature. Behaviours were grouped into four dimensions during a consensus conference: self-care maintenance, self-care monitoring, self-care management and self-care self-efficacy. Sixty-seven items were subsequently generated based on these dimensions. A multidisciplinary group of 40 experts evaluated content validity. Dimensionality of the final items was tested by confirmatory factor analyses (CFA) with a sample of 318 participants. Internal consistency and test–retest reliability were evaluated for each dimension. Construct validity was assessed using correlations between items and scoring differences amongst participants with more severe conditions and secondary complications.
Results
Content validity of the SC-SCII and SCSES-SCI was satisfactory for thirty-five of the previously generated items, which were further refined. CFA showed comparative fit indexes ranging from 0.94 to 0.97 and root mean square errors of approximation from 0.03 to 0.07. Internal consistency ranged from 0.71 to 0.85, and intraclass correlation coefficients were higher than 0.70. Correlations among dimensions were moderate, and the theoretical hypotheses formulated when designing the instruments were largely confirmed.
Conclusions
The SC-SCII and the SCSES-SCI represent valid and reliable theoretically-grounded instruments to assess self-care in people with spinal cord injury.
Similar content being viewed by others
Introduction
People with spinal cord injuries (SCI) face a wide range of limitations in everyday life activities, social relationships, participation, education and employment opportunities [1]. Furthermore, SCI survivors are at increased risk for physical and psychological secondary conditions (SCs) that may affect their independence, quality of life and long-term health [2]. As SCI results in changes in autonomic function and in level of independence, it is essential that people with SCI take primary responsibility for their own care, often relying on caregivers or assistants [3]. Thus, similarly to individuals with other chronic diseases, SCI survivors need to acquire and incorporate specific self-care behaviours into their daily routines throughout their lives, in order to manage their condition and prevent SCs [4, 5]. Good self-care behaviours are effective in improving well-being in individuals with chronic diseases [6, 7]. Thus, it is crucial to regularly assess the level of self-care performed by SCI survivors in order to provide targeted interventions to support the incorporation of such behaviours in daily life.
Rating scales previously developed for an SCI population only partly assessed the self-care concept by focusing on the functional perspective without a sound theoretical grounding [8, 9]. The widely used Spinal Cord Independence Measure (SCIM) assesses functional independence in feeding, bathing, dressing and grooming; while the Functional Independence Measure focuses on eating, grooming, bathing, dressing and toileting. The Self-Care Assessment Tool (SCAT), developed for people with SCI below C7, focuses on medication management, transfers, skin care and continence and lacks a consistent psychometric evaluation [10]. Existing scales assessing self-care behaviours have a poor psychometric and theoretical underpinning [11], thereby emphasising the need for sound, evidence-based instruments.
To address these limitations, a novel tool assessing self-care behaviours in SCI, the Self-Care in Spinal Cord Injury Index (SC-SCII), was developed and tested. The SC-SCII was derived from the middle-range theory of self-care of chronic illness [12]. Middle-range theories in nursing focus on a narrow dimension of a phenomenon in order to guide interventions and everyday practice. Accordingly, self-care is defined as a process performed in ill and healthy states, aimed at maintaining health through health promoting practices and management of health. Based on the theory, self-care consists of three core concepts: self-care maintenance, focused on the need for individuals with chronic illness of ensuring continued physical health and psychological well-being; self-care monitoring, carried out to detect health status modifications; and self-care management, related to behaviours performed by people with a chronic illness to respond to signs and symptoms actively. Self-care concepts, and self-care scales, based on the middle-range theory, are described in several chronic conditions, including heart failure [13], diabetes [14] and chronic obstructive pulmonary disease [15]. A Self-Care Self-Efficacy Scale in SCI (SCSES-SCI), was also developed to assess self-care-related self-efficacy, and particularly, the confidence of individuals with SCI in performing self-care behaviours [12]. This scale was developed to address the lack of a specific instrument measuring self-care self-efficacy in SCI, given evidence indicating the value of self-efficacy in predicting self-care behaviours performed by people with diabetes and heart failure [16, 17].
This study seeks to develop and test the psychometric properties of these two instruments measuring self-care behaviours and self-care-related self-efficacy in individuals with SCI.
Methods
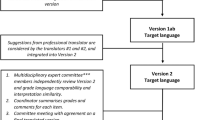
The SC-SCII and the SCSES-SCI were developed and tested through a three-phase process. Firstly, domains and items were generated and discussed in a Consensus Conference of experts. Content validity of identified items was subsequently assessed and face validity tested in a pilot study. Finally, the psychometric properties of the developed instruments were assessed in a multicentre, cross-sectional study.
Instrument development
Firstly, quantitative and qualitative evidence relating to self-care and SCI was analysed to identify behaviours performed by individuals with SCI. In September 2017, the self-care behaviours derived from the literature (Supplementary Material Table S1) were presented to a Consensus Conference of eleven healthcare professionals (HCPs) and three individuals with SCI. HCPs encompassed disciplines involved in SCI rehabilitation (physical medicine, urology, physical therapy, occupational therapy, nursing, psychology and social work) with a median experience of working with SCI of 16 years (range 7–32). People with SCI had complete tetraplegia, complete paraplegia, and incomplete tetraplegia and a median of 7 years (range 4–9 years) lived experience of SCI.
The expert group assessed and organised the presented behaviours to mirror the structure of the middle-range theory of self-care of chronic illness [12]: self-care maintenance (subdivided into skin care, continence care, social participation, and health and social promotion); self-care monitoring (subdivided into SCI-specific and SCI non-specific); and self-care management behaviours (subdivided into autonomous and consulting). The development of the SCSES-SCI followed an analogous process that focused on self-efficacy behaviours (subdivided into health maintenance and symptom monitoring). Behaviours were formulated in item form through a structured, open-ended discussion. Each item had to reach unanimity to be included. This process succeeded in reducing 284 behaviours, grouped into 40 categories, to 67 items.
The items generated during this process were translated from Italian to English under the supervision of the author of the middle-range theory of self-care. At the conclusion of phase one, both scales were available in Italian and English. The SC-SCII consisted of 57 items further subdivided into three scales; Self-Care Maintenance (33 items); Self-Care Monitoring (13 items); Self-Care Management (11 items). The SCSES-SCI consisted of 10 items.
Content and face validity
A multidisciplinary team of experts including 20 HCPs and 20 individuals with SCI from Europe and USA assessed the content validity of the SC-SCII and SCSES-SCI. Items were independently assessed for relevance and comprehensibility using a 5-point Likert scale (0 = not consistent; 5 = strongly consistent). In addition, experts were asked to recommend other relevant self-care behaviours if not listed. A total of 35 items reached a satisfactory content validity (>0.78), while 32 items that did not attain a satisfactory value were removed. No new items were added. The final versions of the instruments contained 12 items for the Self-Care Maintenance Scale, 8 for the Self-Care Monitoring Scale, 8 for the Self-Care Management Scale and 7 for the SCSES-SCI.
Items were refined and scored using a 5-point rating scale (0 = never; 5 = always), indicating the frequency with which behaviours are performed. A “not applicable” option was added for the Self-Care Maintenance Scale items, to accommodate differing SCI clinical manifestations. To mirror the instruments based on the middle-range theory [13, 14, 18, 19], two items were added to the Self-Care Monitoring scale to check occurrence of symptoms and promptness in identifying them as SCI-related symptoms (0 = not recognised; 5 = quickly recognised). In addition, an item was added to the Self-Care Management Scale to determine if the treatment used contributed to the respondent’s feeling better (0 = anything done; 5 = very sure). To facilitate comparisons between instruments with a different number of items, scoring for the self-care and self-efficacy scales is determined by standardising the sum of the items’ score to 100. Higher scores show better self-care.
Face validity was assessed in a pilot study evaluating time for completion, comprehensibility and clarity of the instruments. Data from 20 people with SCI, not subsequently included in the final study, attained a face validity of 9.2/10 (0 = not comprehensible; 10 = very comprehensible). The average time for completion was 11 min.
The SC-SCII and SCSES-SCI (Supplementary Material Table S2) were deemed appropriate to be psychometrically tested to evaluate their structural validity, internal consistency, test–retest reliability and construct validity.
Participants
Dimensionality and internal consistency testing require a minimum of seven respondents for each item of the scale [20]. As each scale had been validated independently, at least 84 respondents were needed. However, in this study, we included 320 respondents to ensure diverse clinical conditions and sociodemographic characteristics. Between March 2018 and October 2019, a consecutive sample of people with SCI was enroled during their follow-up appointments in one northern Italian SCI rehabilitation centre, in two central Italian centres and in one southern Italian centre. Participants were also recruited in Ireland. Inclusion criteria were as follows: (1) traumatic or non-traumatic SCI with an (2) American Spinal Injury Association Impairment (ASIA) Scale A to D classification, (3) discharged at least 6 months from rehabilitation and (4) aged ≥18. People with documented cognitive disorders or mixed diagnoses (e.g. brain injury) were excluded.
Procedure
Participants completed a set of self-report measures in a private space to ensure confidentiality. Administration time ranged from 15 to 30 min. Data collected were as follows:
-
A purposefully designed questionnaire gathered sociodemographic (gender, marital status, education, employment, cohabitation, number of children, healthcare utilisation and caregiver presence) and clinical (level of SCI—tetraplegia/paraplegia, completeness—complete/incomplete and traumatic or non-traumatic aetiology) data.
-
The Modified Barthel Index (MBI) was used to evaluate functional independence [21]. This 10-item mono-dimensional scale describes the functioning of individuals in activities of daily living, with a total score from 0 (total dependence) to 100 (independence).
-
Self-Care and Self-care self-efficacy were evaluated using the SC-SCII and SCSES-SCI.
-
SCs were assessed with the Italian version of the Spinal Cord Injury Secondary Conditions Scale (SCI-SCS) [22]. This 15-item instrument measures the occurrence of the most common physical, SCI-related complications in the previous 3 months. Each item provides a score from 0 (absence) to 3 (chronic), with a total attainable score of 45.
Data analysis
The clinical and sociodemographic characteristics of participants, together with the results of administered questionnaires were presented as means, standard deviations and frequencies. Missing data were evaluated at the variable and item level, deleting them pairwise if clinical or sociodemographic and handling them with maximum likelihood estimation if represented on the self-care scales.
The dimensionality of the SC-SCII and SCSES-SCI was measured prior to estimating reliability [23]. As the instruments were theory-based, the structural validity of each of the three scales composing the SC-SCII and SCSES-SCI was tested by a confirmatory factor analysis (CFA). Factor loadings ≥0.30 were considered adequate. A robust maximum likelihood method for parameter estimation was applied, as the items were not normally distributed. Model fit was determined using X2 statistics, comparative fit index (CFI), Tucker and Lewis index (TLI), root mean square error of approximation (RMSEA) and standardised root mean square residual (SRMR). The goodness-of-fit was evaluated using the CFI and TLI with values of 0.90–0.95 indicating acceptable fit, and values >0.95 indicating a good model fit; RMSEA values ≤0.05 indicating a good model fit, 0.05–0.08 a moderate fit; values of SRMR ≤0.08 showing good fit. The X2 statistic was not applied in interpreting model fit as affected by sample size.
The reliability and validity of the SC-SCII and SCSES-SCI were evaluated. Internal consistency was assessed by calculating Cronbach’s α coefficient and omega coefficient to consider scales’ multidimensionality. Values ≥0.70 were considered satisfactory. To assess the stability of the instruments, the test–retest reliability was calculated on a subgroup of 50 participants to whom the scales were re-administered within 2 weeks. The intraclass correlation coefficient (ICC) was calculated for the scores of each scale. An ICC = 0.80 was considered adequate with two repeated measures [20]. An ICC ≥0.70 was considered acceptable.
Since no other instruments evaluating self-care are available in the literature, criterion validity could not be assessed. Construct validity was verified based on several hypotheses. Firstly, we hypothesised that individuals with tetraplegia, complete lesions, higher functional dependence and more SCs would have higher self-care scores, as increased impact of health conditions motivates increased self-care [24]. Moderate correlations amongst the three self-care scales were hypothesised, as they represent interrelated, albeit distinct aspects, of the self-care construct [12], already demonstrated in other self-care instruments [14, 15, 25]. Finally, as self-efficacy has been shown to be a predictor of self-care [16, 17], a moderate correlation between the SCSES-SCI and the self-care scales was predicted. Correlation was calculated using the Pearson’s product moment correlation coefficients, considering values of 0.10–0.29 as small, 0.30–0.49 as moderate and ≥0.50 as strong [26].
The differences among the SC-SCII mean scores obtained from individuals with SCI who differed in the recognised clinical measures were evaluated using T tests for independent groups. Non-dichotomised variables were converted as follows: MBI (total or severe dependency if ≤60 and moderate or slight dependency if >60) and SCI-SCS (low and high based on median value).
The level of significance was set at ≤0.05. Statistical analyses were performed using SPSS Version 27 (IBM, Armonk, NY) except for CFA, which was performed using Mplus Version 8.1 [27].
Results
Of the 320 participants with SCI, 318 (99%) completed the SC-SCII and the SCSES-SCI (Table 1). Data from two participants who completed less than 50% of the administered set of instruments were excluded. The majority of respondents were male (n = 228; 71.7%), had a traumatic injury (n = 237; 75.7%), paraplegia (n = 207; 65.7%) and were more than 3 years post injury (n = 236; 74.2%). The mean age was 50.5 years (SD = 14.73). Most participants had a complete injury (n = 165; 52.1%) and moderate or slight dependency (n = 203; 63.8%). Joint and muscle pain (n = 194; 61.0%), spasticity (n = 188; 59.1%), and urinary tract infections (n = 171; 53.8%), were the most frequently reported chronic or occasional SCs with a median SCI-SCS total score of 17.
Self-care maintenance scale
The scale was constructed to include four dimensions; skin care, such as performing pressure relief at regular intervals or transferring avoiding impact or friction; continence care, such as using an efficient method for bladder and bowel management; social participation, such as maintaining social activities and sexuality; and health promotion, such as attending regular follow-up visits or getting information on available social and health services.
The model goodness-of-fit indices (Table 2) were good: X2 = 67.2, p = 0.03, CFI = 0.97, TLI = 0.96, RMSEA = 0.03 (90% CI [0.01–0.05]), p = 0.89, SRMR = 0.04. Factor loadings ranged from 0.31 to 0.89 and were statistically significant (Table 3).
The Cronbach’s α coefficient for the entire scale was 0.71, while the omega coefficient was 0.72. The ICC coefficient for the total score was 0.89 (95% CI [0.77–0.96]).
Self-care monitoring scale
The scale was constructed to include two dimensions; behaviours focussed on SCI-specific symptom monitoring, such as inspecting the skin for redness or changes in the urine colour or smell; and non-SCI-specific symptom monitoring, such as checking weight changes or medication side-effects.
The model goodness-of-fit indices (Table 2) were good: X2 = 30.8, p = 0.04, CFI = 0.97, TLI = 0.95, RMSEA = 0.04 (90% CI [0.01–0.07]), p = 0.59, SRMR = 0.04. Factor loadings ranged from 0.44 to 0.72 and were statistically significant (Table 3).
The Cronbach’s α coefficient for the entire scale was 0.76, while the omega coefficient was 0.77. The ICC coefficient for the total score was 0.87 (95% CI [0.69–0.94]).
Self-care management scale
The scale was constructed to include two dimensions; autonomous behaviours, such as taking medications to relieve specific signs and symptoms or changing fluid intake; and consulting behaviours, such as asking a caregiver to help with signs and symptoms or searching the internet to get information.
The model goodness-of-fit indices (Table 2) were acceptable: X2 = 33.4, p = 0.01, CFI = 0.94, TLI = 0.90, RMSEA = 0.05 (90% CI [0.02–0.08]), p = 0.41, SRMR = 0.04. Such values were obtained after the correlation of errors between two items belonging to the consulting behaviours dimension. Factor loadings ranged from 0.36 to 0.80 and were statistically significant (Table 3).
The Cronbach’s α coefficient for the entire scale was 0.69, while the omega coefficient was 0.71. The ICC coefficient for the total score was 0.91 (95% CI [0.81–0.96]).
Self-care self-efficacy scale
The scale was constructed to include two dimensions, behaviours related to confidence in adhering to self-care maintenance and management behaviours, such as following HCPs’ advice or doing something to relieve symptoms; and confidence in adhering to symptom monitoring behaviours, such as recognising changes in health status or evaluating the importance of symptoms.
The model goodness-of-fit indices (Table 2) were acceptable: X2 = 34.6, p < 0.001, CFI = 0.95, TLI = 0.92, RMSEA = 0.07 (90% CI [0.04–0.10]), p = 0.63, SRMR = 0.03. Factor loadings ranged from 0.45 to 0.79 and were statistically significant (Table 3).
The Cronbach’s α coefficient for the entire scale was 0.84, while the omega coefficient was 0.85. The ICC coefficient for the SCSES-SCI was 0.86 (95% CI [0.69–0.94]).
Construct validity
The three self-care scales were moderately correlated with each other and each of them was moderately correlated with the SCSES-SCI (Table 4). Participants with complete injuries had higher scores on the Self-Care Maintenance Scale, while those with tetraplegia, total or severe dependency and more SCs reported higher scores on the Self-Care Management Scale. In contrast to study hypotheses, scores on the Self-Care Maintenance Scale were higher in people with paraplegia, moderate or slight dependency and fewer SCs.
Discussion
This study aimed to develop and evaluate the psychometric properties of two novel instruments evaluating self-efficacy and the three theoretical dimensions of self-care. This represents a first attempt to apply the middle-range theory of self-care of chronic illness to SCI, thereby providing a solid theoretical underpinning for the SC-SCII.
The self-care behaviours included in the SC-SCII differ from those included in previously developed instruments extensively used in SCI [8,9,10]. In contrast to a functional perspective, the self-care behaviours in the three dimensions of this newly developed instrument focus on the maintenance and promotion of health in individuals with SCI. This focus is consistent with the prevention of the most common SCs and integrates the social and participation domains, which combine to ensure well-being amongst this population [3, 28, 29]. Moreover, self-care monitoring behaviours are considered as an intensive, complex and time-consuming activity for people with SCI [3], involving recognising body signals or sensations, which is a crucial component of the decision-making process that individuals engage in when performing self-care [12, 30]. This decision-making process leads people with SCI to actively engage in behaviours, either independently or in consultation with HCPs, caregivers, or other sources [3], directed towards managing their health in response to specific signs and symptoms [12, 30]. It can encourage SCI survivors to integrate self-care activities into the more functional focus of rehabilitation. In this respect, functional assessment should remain a cornerstone for HCPs in the field of SCI, which must not be questioned in favour of focusing exclusively on self-care. Instead, the tools developed in this study could constitute practical means of broadening the range of outcomes to be assessed for people with SCI by incorporating the evaluation of the level of self-care together with the functional assessment.
The theoretical hypotheses formulated when designing the SC-SCII were largely confirmed. More extensive self-care monitoring and self-care management behaviours were reported by individuals with tetraplegia, complete injuries, higher dependency, and more SCs, indicating that the scales can accurately reflect an increase in self-care behaviours in people with severe clinical conditions. Conversely, self-maintenance behaviours are not influenced by injury level, functional independence and the presence of SCs. Inconsistencies in carrying out self-care maintenance behaviours has been demonstrated in previous studies, indicating that it represents a multifaceted dimension of illness and consequently of self-care [12, 14]. People with a more severe chronic illness usually perform more self-care behaviours [14, 15, 31], suggesting that those with the most severe health conditions and higher disease-related symptoms, as is the case in complete injuries, had an increased need to focus on self-care. Given the differences between SCI and other chronic illnesses with a progressive trajectory, it is likely that more self-maintenance behaviours are performed by SCI survivors with greater independence and ability to participate, in order to prevent the occurrence of SCs. The support of a caregiver following SCI rehabilitation might indicate that individuals with less independence perform less self-maintenance behaviours, relying on the caregivers’ contribution to self-care [32]. Further studies are required to evaluate these possibilities. According to the middle-range theory of self-care, the three self-care scales are related, showing that they are interrelated expressions of the same general construct [12].
This study developed and tested the SCSES-SCI. This instrument encapsulates two factors describing confidence in maintaining and managing SCI and monitoring of symptoms. The effectiveness of this concept in predicting self-care among people with chronic illness [16, 17] has been demonstrated, thus suggesting the need to assess its application to SCI survivors. If this association is demonstrated in people with SCI, interventions addressing confidence should be considered viable options to enhance self-care in this population.
The three self-care scales and the SCSES-SCI demonstrated reliability. All scales reached an adequate internal coherence for such multidimensional instruments. All instruments showed acceptable stability. Moreover, they were considered readable and easy to use, implying that they are applicable in clinical practice and do not represent a burden for individuals with SCI or for HCPs.
This study has some limitations. Recruitment took place during follow-up visits, and therefore participants consisted of those accessing outpatient clinics following SCs and may not be representative of a community-dwelling SCI population. The sample was mainly composed of people with paraplegia, traumatic SCI and moderate dependency, thereby excluding the full range of self-care behaviours that might be performed by individuals with more severe conditions. Nevertheless, the inclusion of a considerable number of participants from five centres in two European countries may have reduced these limitations. Further testing with a broader sample of people with SCI in different contexts is desirable to confirm the psychometric properties of the instruments. Moreover, as the responsiveness of the SC-SCII and SCSES-SCI, or the ability to detect change over time, was not tested, several longitudinal studies in which interventions to promote self-care are needed to assess changes over time of this construct and its effect on clinical outcomes of SCI.
Conclusion
The SC-SCII is a 38-item instrument, developed to assess self-care in people with SCI, based on the middle-range theory of self-care of chronic illness. The questionnaire comprises three distinct scales reflecting the dimensions described by the theory from which it was inspired. In addition, the SCI-SCSES represents a 7-item scale developed to evaluate self-care self-efficacy, which showed a meaningful effect on self-care in chronic illness. The study findings support the psychometric properties of these instruments in a large sample of people with SCI from Italy and Ireland. Such tools can represent a valid and reliable resource to corroborate the functional assessment with the self-care activities performed by people with SCI to maintain, monitor and manage their condition. Further testing in different populations and an evaluation of SC-SCII and SCI-SCSES in identifying the impact of self-care on clinical and psychological outcomes is recommended, as they may represent valuable tools to guide HCPs in planning appropriate interventions for individuals with SCI.
Data availability
The datasets generated and analysed during this study are available from the corresponding author on request.
References
World Health Organisation. International classification of functioning, disability and health: ICF. Geneva: World Health Organisation; 2001.
Gabbe BJ, Nunn A. Profile and costs of secondary conditions resulting in emergency department presentations and readmission to hospital following traumatic spinal cord injury. Injury. 2016;47:1847–55.
Conti A, Clari M, Kangasniemi M, Martin B, Borraccino A, Campagna S. What self-care behaviours are essential for people with spinal cord injury? A systematic review and meta-synthesis. Disabil Rehabil. 2020;0:1–16.
Matter B, Feinberg M, Schomer K, Harniss M, Brown P, Johnson K. Information needs of people with spinal cord injuries. J Spinal Cord Med. 2009;32:545–54.
Conti A, Dimonte V, Rizzi A, Clari M, Mozzone S, Garrino L, et al. Barriers and facilitators of education provided during rehabilitation of people with spinal cord injuries: a qualitative description. Plos ONE. 2020;15:e0240600.
Ditewig JB, Blok H, Havers J, van Veenendaal H. Effectiveness of self-management interventions on mortality, hospital readmissions, chronic heart failure hospitalization rate and quality of life in patients with chronic heart failure: a systematic review. Patient Educ Couns. 2010;78:297–315.
Ausili D, Bulgheroni M, Ballatore P, Specchia C, Ajdini A, Bezze S, et al. Self-care, quality of life and clinical outcomes of type 2 diabetes patients: an observational cross-sectional study. Acta Diabetol. 2017;54:1001–8.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM—spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6.
Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the Functional Independence Measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74:531–6.
McFarland SM, Sasser L, Boss BJ, Dickerson JL, Stelling JD. Self-care assessment tool for spinal cord injured persons. SCI Nurs. 1992;9:111–6.
Clari M, Matarese M, Alvaro R, Piredda M, De Marinis MG. Measurement properties of instruments evaluating self-care and related concepts in people with chronic obstructive pulmonary disease: a systematic review. Heart Lung J Acute Crit Care. 2016;45:441–8.
Riegel B, Jaarsma T, Strömberg A. A middle-range theory of self-care of chronic illness. Adv Nurs Sci. 2012;35:194.
Riegel B, Barbaranelli C, Carlson B, Sethares KA, Daus M, Moser DK, et al. Psychometric testing of the revised self-care of heart failure index. J Cardiovasc Nurs. 2019;34:183–92.
Ausili D, Barbaranelli C, Rossi E, Rebora P, Fabrizi D, Coghi C, et al. Development and psychometric testing of a theory-based tool to measure self-care in diabetes patients: the Self-Care of Diabetes Inventory. BMC Endocr Disord. 2017;17:66.
Matarese M, Clari M, De Marinis MG, Barbaranelli C, Ivziku D, Piredda M, et al. The self-care in chronic obstructive pulmonary disease inventory: development and psychometric evaluation. Eval Health Prof. 2020;43:50–62.
Caruso R, Rebora P, Dellafiore F, Fabrizi D, Riegel B, Ausili D, et al. Clinical and socio-demographic determinants of inadequate self-care in adults with type 1 diabetes mellitus: the leading role of self-care confidence. Acta Diabetol. 2019;56:151–61.
Vellone E, Pancani L, Greco A, Steca P, Riegel B. Self-care confidence may be more important than cognition to influence self-care behaviors in adults with heart failure: testing a mediation model. Int J Nurs Stud. 2016;60:191–9.
Dickson VV, Lee C, Yehle KS, Abel WM, Riegel B. Psychometric testing of the self-care of hypertension inventory. J Cardiovasc Nurs. 2017;32:431–8.
Vaughan Dickson V, Lee CS, Yehle KS, Mola A, Faulkner KM, Riegel B. Psychometric testing of the self-care of coronary heart disease inventory (SC-CHDI). Res Nurs Health. 2017;40:15–22.
De Vet HCW, Terwee CB, Mokkink LB, Knol DL. Measurement in medicine: a practical guide. Cambridge, England: Cambridge University Press; 2011.
Galeoto G, Lauta A, Palumbo A, Castiglia S, Mollica R, Santilli V, et al. The Barthel Index: Italian translation. Adapt Valid Int J Neurol Neurother. 2015;2:1–7.
Conti A, Clari M, Arese S, Bandini B, Cavallaro L, Mozzone S, et al. Validation and psychometric evaluation of the Italian version of the Spinal Cord Injury Secondary Conditions Scale. Spinal Cord. 2020;58:496–503.
Barbaranelli C, Lee CS, Vellone E, Riegel B. The problem with Cronbach’s Alpha: comment on Sijtsma and Van der Ark (2015). Nurs Res. 2015;64:140–5.
Riegel B, Jaarsma T, Lee CS, Strömberg A. Integrating symptoms into the middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2019;42:206–15.
Riegel B, Barbaranelli C, Sethares KA, Daus M, Moser DK, Miller JL, et al. Development and initial testing of the self-care of chronic illness inventory. J Adv Nurs. 2018;74:2465–76.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988.
Muthén LK, Muthén BO. Mplus user’s guide (8th ed.). Los Angeles, CA: Author; 1998.
Wang Y, Zhao X, Xie H. Quality of life and its predictors in people with traumatic spinal cord injury in mainland China. Spinal Cord. 2019;57:739–46.
Gross-Hemmi MH, Fekete C, Post MWM, Scheel-Sailer A, Schwegler U, Brinkhof MWG. Detecting subgroups in social participation among individuals living with spinal cord injury: a longitudinal analysis of community survey data. Spinal Cord. 2021;59:419–28.
Riegel B, Dickson VV, Faulkner KM. The situation-specific theory of heart failure self-care: revised and updated. J Cardiovasc Nurs. 2016;31:226–35.
Dickson VV, Buck H, Riegel B. A qualitative meta-analysis of heart failure self-care practices among individuals with multiple comorbid conditions. J Card Fail. 2011;17:413–9.
Vellone E, Riegel B, Alvaro R. A situation-specific theory of caregiver contributions to heart failure self-care. J Cardiovasc Nurs. 2019;34:166–73.
Acknowledgements
Sincere thanks go to Prof. Barbara Riegel for her supervision during the process of constructing the instrument and the methodological support provided during the design of the study protocol. Moreover, we wish to thank the participants and the staff at the Spinal Cord Injury Units of Città della Salute e della Scienza University Hospital of Torino, Careggi Hospital of Firenze, IRRCS Fondazione Santa Lucia of Roma, Cannizzaro Hospital of Catania, and the National Rehabilitation Hospital of Dublin. Particularly, we would like to acknowledge Silvia Mozzone, Simona Frigerio, Patrizia Maitan, Eva Wallace, Sara Arese, Marco Tommasini, Vittoria Parolai, and Stefano Gatta for their contribution in the data collection and accomplishment of this project.
Author information
Authors and Affiliations
Contributions
AC was responsible for designing and writing the study protocol, and for submitting the study to the ethical committee. He was also responsible for writing the article, collaborating with recruiting centres, and interpreting results. EV, VD, and SC were responsible for designing and writing the study protocol and provided feedback on the article draft. GS, MN, BB, and AB were responsible for recruiting the participants and managing the data. MC was responsible for the database managing, analyzing data, and interpreting the results. MC and MN contributed to writing the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval (Resolution no. CS2/596, March 13, 2018) was granted by the Città della Salute e della Scienza di Torino, Mauriziano Hospital, ASL TO1 Research Ethics Committee, Turin, Italy. All recruitment centres gave their authorisation for participation in the study. Furthermore, all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed. Participants provided written, informed consent, and anonymity was maintained throughout the research process.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Conti, A., Campagna, S., Nolan, M. et al. Self-care in spinal cord injuries inventory (SC-SCII) and self-care self-efficacy scale in spinal cord injuries (SCSES-SCI): development and psychometric properties. Spinal Cord 59, 1240–1246 (2021). https://doi.org/10.1038/s41393-021-00702-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00702-9