Abstract
Study design
Qualitative exploratory study.
Objectives
To explore the lived experience of SCI caregivers, with a focus on the challenges of their role.
Setting
Caregivers of people with SCI living in the community in Switzerland.
Methods
Data were collected through semi-structured interviews. Thematic analysis was performed.
Results
The sample included 22 participants (16 women, 15 life partners) with a mean age of 61 years who had been caregivers for an average of 18 years. Caregiving in SCI seemed to be characterized by two phases. The first phase was relatively short and was central to becoming a caregiver; it was marked by challenges related to adjusting to the role of caregiver (e.g., dealing with shock, feeling unprepared). The second phase is lifelong and is characterized by a number of recurrent challenges related to balancing caregiving and personal life (e.g., having to prioritize caregiving over personal wishes, negotiating tasks and workload). Challenges related to lacking appropriate housing, facing financial uncertainty and dealing with bureaucracy were noted during both phases. Caregivers had to deal with these challenges to stay in step with life changes and newly emerging needs.
Conclusions
Informal caregivers have a major role in supporting people with SCI. But their needs are not static. Any strategy to empower them has to adapt to an evolving role characterized by multiple tasks and challenges. A functional relationship between caregivers and care recipients is based on the recognition of their individualities and the different phases of adaptation, which is also an enriching process.
Similar content being viewed by others
Introduction
A spinal cord injury (SCI) changes a person’s life overnight, requiring them to relearn the most basic tasks. People with a SCI who do not achieve complete independence rely on support to manage their condition and carry out daily activities. This support contributes to their quality of life and ability to participate in society and is often provided by family members [1]. Moreover, caregivers provide support not only for mobility and household chores, but also for respiratory care, body care, bowel and bladder management, and eating and drinking [2, 3]
Research in the field of other chronic conditions, such as cancer, Alzheimer’s disease, and Parkinson’s disease, shows that caregiving often disrupts the life of the caregiver, including their professional, social, and familial relationships [1, 4,5,6]. Furthermore, studies have reported the perceived impact that the role of caregiving has on a caregiver’s life (e.g., caregiver burden) [7, 8].
In the context of SCI, recent reviews of the literature have reported caregivers having high levels of burden, depression and anxiety, physical symptoms, and reduced life satisfaction, as well as feelings of isolation and a loss of identity [9, 10]. This might be due to the fact that, unlike caregiving in other conditions, caregiving in SCI can last decades, as the life expectancy of people with SCI has increased, and these caregivers often take on the role in early-middle age [9, 11].
Caregiving is an evolving experience that is shaped by an interplay of contextual and relational factors. To better support caregivers, it is necessary to identify the challenges they encounter in caring for a loved one and assess the appropriateness of the healthcare system’s response to their needs [12]. This study will explore the lived experience of SCI caregivers, with a focus on the challenges that they face over time. While research in the field of SCI has emphasized the caregiver burden (e.g., predictors, impact on health) [3, 13, 14], this study looks at the evolution of the role of caregiver as experienced by those in this position.
Methods
Study design, sampling, and recruitment
This qualitative exploratory study is part of a larger project about informal caregivers of people with SCI in Switzerland. The project included a quantitative study [2] and a qualitative study with a subgroup of participants. Overall, the latter aimed to identify targets for the empowerment of informal caregivers in terms of support, information services and self‐management resources. Some of its findings are presented in this manuscript.
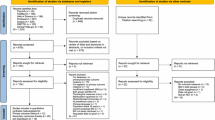
To recruit participants, we contacted the people with SCI included in the address lists of the national longitudinal survey (Swiss Spinal Cord Injury Cohort Study) [15, 16], cross-referenced with the membership database of the Swiss Paraplegic Association and patient databases of the four SCI-specialized clinics in Switzerland. Those with SCI were asked to give the enclosed survey to their primary family caregiver. The caregivers who completed the survey (N = 717) could indicate in the informed consent form their availability to take part in an interview.
All the caregivers who indicated in the survey, their availability to take part in an interview, were considered potential participants. Among them, we recruited a purposive sample of participants for this study. The participants fulfilled the following inclusion criteria: being >18 years of age, speaking an official Swiss language (French, German, or Italian) fluently, providing at least 10 h per week of care to a family member with SCI who has been a wheelchair user for at least 4 years, and perceiving either a high or low burden in relation to caregiving. This information was retrieved from the survey. To capture a wide range of perspectives on SCI caregiving, we also considered factors that might affect the experience of caregiving [17,18,19,20] such as gender and age (for caregiver and care recipient), linguistic region, relationship between caregiver and care recipient (partner, parent, adult child), financial expenditures due to caregiving, and number of years of caregiving.
The potential participants were contacted via phone or via email, depending on the contact method that they indicated as preferred in the survey. We tried to join 34 caregivers, of which 22 actually participated in the study. We stopped trying to recruit a potential participant after having called three times at different times of the day or after having sent two reminders without answer.
Participation in the study was voluntary, and written consent was obtained from all interviewees. During the first contact, the researcher would quickly present the aim of the study and what the participation consisted of. If the person showed an interest in participating, the study information and a copy of the informed consent were sent home. Later on, the interview was scheduled. The day of the interview, the researcher would remind the most important issues linked to the declaration of informed consent and the interviewee would sign the document.
Data collection
Data were collected through audio-recorded semi-structured interviews. The interview guide was developed by CZ and revised in collaboration with the research team. The questions explored the experiences of caregiving and their evolution over time. Knowing from the literature that caregiving can be a disruptive event and that caregivers often reported negative outcomes, we included questions that covered these aspects. In addition, and in line with other scientific literature, we asked questions to uncover the positive aspects of caregiving, as well as resources and strategies that caregivers put into place. The main questions of the interview guide are presented in Table 1. The questions would guide the conversation but there was the opportunity to follow-up on issues raised by the participants.
Three pilot interviews were conducted to test the interview guide after which no major changes were made, but the wording was improved. The pilot interviews were therefore included in the analysis.
The first author and a trained research assistant (NL) conducted all interviews in the interviewees’ preferred language (German, French, or Italian) and in a location of their choosing (i.e., home, workplace, bar). The interviewers kept a field diary in which they took notes of initial analysis thoughts, interpretations, and questions as well as of feelings during the interviews and first impressions. The interviewers also discussed issues emerged in the conduction of the interviews (e.g., how to best support a caregiver who is crying, how to deal with the own emotions).
Data analysis
The interviews lasted an average of 70 min (±SD = 33), were transcribed verbatim and analyzed following the principles of thematic analysis [21]. The analysis included both a deductive and an inductive phase: The first author (CZ) conducted the first deductive coding of six interviews and JA and NL of each three interviews. The three researchers met then to compare the coding and solve disagreement. A similar procedure was followed for the inductive coding. The data of each theme were constantly compared to ensure their homogeneity as well as their distinctiveness from other themes. Thematic saturation was reached.
To ensure trustworthiness, the researchers involved in the analysis documented their personal reflections on the data and had regular informal peer debriefings. They also performed investigator triangulation (e.g., by checking preliminary findings and interpretations against the raw data) to reduce researcher bias. They kept track of their discussions on themes, labeling, etc. to remember how and why decisions were made.
The interviews were analyzed in their original language, and excerpts were translated only for the purpose of scientific publications. The software MAXQDA™ (Release 12.2.0) was used to organize and store the data.
More details are presented in the Supplementary file 1.
Results
The final sample included 22 participants (16 women) with a mean age of 61 years (±SD = 10.4) who had been caregivers for an average of 18 years (±SD = 13.5). The majority of the participants were the life partners (n = 15) of the care recipient. Participants’ characteristics are presented in Table 2.
The analysis indicated that the experience of SCI caregiving had two phases. The first phase covered the period in which the family member became a caregiver. In most cases, this happened after the patient’s discharge from their first rehabilitation. However, in some cases, caregiving began later (e.g., partners met after SCI onset and became caregivers once they moved in together). The second phase began after a new routine had been arranged.
Many participants claimed the beginning of caregiving was a “natural” consequence of the relationship they had with the care recipient, anchored in social norms (e.g., a wife is expected to take care of her husband) and an expectation of reciprocity (i.e., she/he would have done it for me) (illustrative quotes are presented in Table 3, Q1). In their views, being a caregiver was a part of their duties as a mother or life partner (Q2) and some explained that helping was part of their nature or personality (Q3). Among the reasons mentioned for having become caregivers, the participants often referred to a desire to protect the family privacy and to avoid dependence on homecare providers (Q4). However, in other cases, it was the concurrence of certain life circumstances (e.g., being unemployed and a nurse by training when the accident happened); expressions like “I slipped into it” stressed the accidental way the caregiving began (Q5). Other reasons for “slipping into caregiving” were not finding any appropriate assisted living facility or the expectation of the injured person to be assisted by the family member (Q6).
Despite the different ways in which the participants described the beginning of caregiving, they seemed to have experienced a number of similar challenges. The first phase was characterized by specific challenges that seemed to mirror how the caregiving started: unexpected and disruptive. Dealing with these challenges allowed the family member to embed the caregiver role into their life. The second phase was marked by recurrent challenges and subsequent adjustments. In the following, we provide an in-depth exploration of the challenges that characterize the lifelong process of becoming and being a caregiver (Fig. 1).
Challenges related to adjusting to the role as caregiver
Dealing with the shock
In situations in which the care recipient and caregiver already had a relationship before SCI onset (e.g., parent–child, partners), the analysis highlighted that the caregiver had to deal with shock and realize that the disability was permanent. The participants reported that during the acute rehabilitation phase they had to understand what happened, manage their expectations for recovery, and start coming to terms with the situation (Q7).
Feeling unprepared
The participants reported a lack of information, training, and guidance (Q8). When looking back, some interviewees stated that the focus was always on the person with SCI and resented a lack of support in preparing them for a “lifetime job” as a caregiver (Q9).
Adapting life and habits
Becoming a caregiver required adaptations in many domains: professional life (e.g., reducing working time), social life (e.g., less time for friends and hobbies), and family life (e.g., moving because the house could not be adapted) (Q10). Even in the cases of caregivers who took on the task years after SCI onset, there was a need to adapt their lives to the new situation (Q11). Adapting their lives and habits gave rise to new routines, which were often fixed and based around the needs of the care recipient (e.g., self-management activities such as emptying the bladder or laying down to prevent pressure injuries) (Q12).
Challenges related to housing, bureaucracy, and financial issues
Lacking appropriate housing
Housing for people with SCI are lacking, in particular for young people, for whom neither nursing homes nor assisted living facilities for individuals with learning disabilities are adequate solutions (Q13). Moreover, caregivers who had started to feel the consequences of ageing wondered about who would take on caregiving when they are no longer able to provide the needed care. This worry especially affected caregivers whose care recipient was not accustomed to receiving assistance from homecare providers (Q14). In some cases, this worry was reinforced by bad experiences with nursing care facilities (Q15).
Dealing with bureaucracy
Several participants mentioned the challenges of dealing with the bureaucracy of insurance providers. They mostly complained about the complexity of the reimbursement system (Q16) or the strict rules (e.g., reimbursement for psychological support) (Q17). Some interviewees also stressed how mentally exhausting the process of applying for reimbursement or allowances could be (Q18).
Facing financial uncertainty
The participants reported that the often very long procedures to define disability benefits left families in limbo and facing financial uncertainty. The situation could be more or less difficult, depending on their financial situation prior to SCI onset and the caregiver’s work situation. Among the participants facing financial difficulty, some decided to continue working even after reaching official retirement age. Among those who were in a comfortable situation, some expressed worry for the future (Q19).
Challenges related to finding a balance between caregiving and personal life
Having to prioritize caregiving over personal wishes
Some participants acknowledged that caregiving required sacrifice in terms of personal aspirations and freedom (Q20). Some interviewees stated that they had to give up vocational retraining or new professional experiences because these were not compatible with their caregiver role (Q21). Several others reported having to refuse invitations or give up activities when these did not fit with their caregiving schedule. Many caregivers acknowledged that caregiving affected their ability to make spontaneous plans (Q22).
Negotiating tasks and workload
Some caregivers described how they negotiated their workload and tasks (Q23). For example, the fear of mixing the roles of partner and caregiver led to a clear division of tasks: personal care (e.g., bowel management) was delegated to homecare providers, while the partner took on assistance (e.g., mobility). The analysis highlighted that this negotiation is an iterative process and can be triggered by several factors; for example, caregivers might realize that the situation is not sustainable anymore because of ageing, other commitments, or unclear role boundaries (e.g., being caregiver, life partner, and working partner), or care recipients might develop new needs that require new arrangements (Q24).
Finding time for themselves
Caregiving was often perceived as a full-time job, and a major challenge for caregivers was to find time for themselves (Q25). With good organization, it was possible to create free time, but such organization could be demanding. Some caregivers stressed that an activity had to be worthwhile; otherwise, the planning effort exceeded the pleasure (Q26). Furthermore, in many cases this would require the care recipient to accept external support, which was often undesired (Q27).
Discussion
This study found that SCI caregiving most often begins unexpectedly and is characterized by two phases. The first phase is relatively short and central to becoming a caregiver, and it is marked by challenges related to adjusting to the role of caregiver and embedding this in their lives. The second phase, which is lifelong, is characterized by a number of recurrent challenges related to finding a balance between caregiving and personal life. The challenges related to housing, bureaucracy, and financial issues take place in both phases. Caregivers have to deal with these challenges to stay apprised of life changes (e.g., retirement) and newly emerging needs (e.g., how to deal with ageing in SCI).
These finding have two major implications. First, by describing how family members become caregivers, a time point in which vulnerable caregivers can be identified is suggested. Second, by describing the challenges and their timing, inputs for developing tailored programs and assessing the adequacy of the services available are provided.
In relation to the first point, the “birth” of a caregiver offers the earliest opportunity to identify people in need of support. Indeed, as past research has documented, becoming a caregiver is a turning point in one’s life trajectory [22], and for relatives, it seems to be less a matter of choice than a matter of responsibility and reciprocity [23, 24]. Considering that feelings of control in caregiving relate to caregivers’ wellbeing and that the decision to become a caregiver is an indicator of control [25], caregivers who choose to take on caregiving might experience higher levels of control than caregivers who “slipped into it”. In addition, research has shown that less control in caregiving is associated with a lower household income, a lower subjective social position, and a higher objective caregiver burden [25]. Thus, it might be important to assess these factors to identify vulnerable caregivers in a timely manner.
The moment a person becomes a caregiver is a turning point. However, our findings indicate that being a caregiver is more a process than a state. Consequently, caregivers have to find resources throughout their lives to assist the care recipient without jeopardizing their own well-being. In line with earlier research [3, 26, 27], we believe that routine need-and-outcome assessments may be useful. In practice, rehabilitation clinics could offer a “caregiver checkup” in tandem with the checkup offered to the people with SCI. This is in accordance with Chan [28], who stressed the importance of considering a caregiver and care recipient as a single unit to promote understanding and preparedness post discharge.
During the “caregiver checkup”, caregivers could be screened with regard to the challenges they may be facing and the care recipient’s health status and functional independence, as these are associated with caregiver outcomes [29, 30]. Such support might not only benefit caregivers, it could also positively influence the care recipient and the relationship between the two [13, 31]. Furthermore, positive caregiver outcomes would ensure the caregiving is sustainable, thereby contributing greatly to the healthcare system.
The findings of this study might also provide an opportunity to check if the services available support caregivers in addressing the challenges they encounter over time. While adjusting to their new role, caregivers often feel unprepared and struggle with shock. Therefore, the effectiveness of educational programs in increasing caregivers’ confidence and competence in providing safe and effective care could be evaluated, as could the services addressing distress [32, 33]. Similarly, the adequacy of services to support caregivers in dealing with challenges linked to housing, bureaucracy, financial issues, and balancing caregiving and personal life needs to be assessed. In Switzerland, several services (e.g., homecare providers, respite care) are available, but their use is limited and dependent on the characteristics of both the caregiver and the care recipient [2, 34]. In about half of all cases, there seems to be no need of these services; however, sometimes costs, limited flexibility and care receiver’s rejection of external assistance are barriers to using these services [2].
Furthermore, our findings suggest that the timing of existing services should be considered. Indeed, a limitation is that most of these services, including caregiver education, are offered during or shortly after discharge from acute care or rehabilitation [35]. For educational programs this is problematic, as receiving too much information at once or at the wrong time might not be helpful [36] (p.153). Hence, we endorse the suggestion of Graf and colleagues [26] to offer support at different points in time. Based on the results of a “caregiver checkup”, rehabilitation clinics could identify caregivers in need and direct them to the appropriate services or provide them with tailored information. Linking caregivers to resources would help them find the appropriate support when it was most needed. In this regard, the introduction of case management programs could also help; in a recent study in Switzerland nearly half of the respondents reported that their need for case management was at best partially fulfilled [37].
This study has some methodological limitations. First, it relied on the memories of participants, who were reporting their (often very long) caregiving experiences. Prospective longitudinal studies could further explore the specific challenges of caregiving directly after first rehabilitation; however, the fact that saturation was reached supports the existence of several shared challenges. Second, the composition of our sample did not allow for performing comparisons among groups (e.g., caregivers with different relationships with the care recipient, male vs female caregivers). It is nonetheless important to notice that in Switzerland caregivers of people with SCI are mostly life partners and female [2], as in our sample. Finally, some of the challenges presented in this article might be specific to the Swiss context.
Conclusion
The findings of this study suggest that SCI caregivers go through two phases and that their lives are characterized by continuous adjustment to the ever-evolving role of caregiver. Furthermore, describing how family members become caregivers and the challenges they face over time might help improve the societal response to SCI by developing tailored interventions aimed at equipping caregivers with the necessary knowledge and skills. This will not only benefit caregivers, it is also likely to have a positive impact on the care recipient and the relationship between the two. Caring for caregivers is a way of giving back to these family members who support the healthcare system with their often invisible, but extremely valuable, work.
Data archiving
The transcripts of the interviews analyzed in the current study are available from the corresponding author on request. Transcripts will be provided in the original language (mostly German).
References
Smith EM, Boucher N, Miller WC.Caregiving services in spinal cord injury: a systematic review of the literature.Spinal Cord. 2016;54:562–9.
Gemperli A, Rubinelli S, Zanini C, Huang J, Brach M, Pacheco et al. Family caregivers of persons with spinal cord injury. J of Rehabilit Med. (in press).
Post M, Bloemen J, De Witte L. Burden of support for partner of persons with spinal cord injuries. Spinal Cord. 2005;43:311–9.
Houldin AD. A qualitative study of caregivers’ experiences with newly diagnosed advanced colorectal cancer. Oncol Nurs forum. 2007;34:323–30.
Grimmer K, Moss J, Falco J. Becoming a carer for an elderly person after discharge from an acute hospital admission. The Internet J of Allied Health Sci and Prac. 2004;2:1–8.
Silva-Smith AL. Restructuring life: preparing for and beginning a new caregiving role. J Fam Nurs. 2007;13:99–116.
Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108:23–7.
Brewin A. The quality of life of carers of patients with severe lung disease. Br J Nurs. 2004;13:906–12.
Lynch J, Cahalan R. The impact of spinal cord injury on the quality of life of primary family caregivers: a literature review. Spinal Cord. 2017;55:964–78.
Baker A, Barker S, Sampson A, Martin C. Caregiver outcomes and interventions: a systematic scoping review of the traumatic brain injury and spinal cord injury literature. Clin Rehabil. 2017;31:45–60.
Savic G, DeVivo M, Frankel H, Jamous M, Soni B, Charlifue S. Long-term survival after traumatic spinal cord injury: a 70-year British study. Spinal Cord. 2017;55:651–8.
International perspectives on spinal cord injury. World Health Organization & The International Spinal Cord Injury Society 2013.
Tough H, Brinkhof MW, Siegrist J, Fekete C. Subjective caregiver burden and caregiver satisfaction: the role of partner relationship quality and reciprocity. Arch Phys Med Rehabil. 2017;98:2042–51. Epub 2017/03/14
Fekete C, Tough H, Siegrist J, Brinkhof MW. Health impact of objective burden, subjective burden and positive aspects of caregiving: an observational study among caregivers in Switzerland. BMJ Open. 2017;7:e017369. Epub 2017/12/25
Post MW, Brinkhof MW, von Elm E, Boldt C, Brach M, Fekete C, et al. Design of the Swiss spinal cord injury cohort study. Am J Phys Med Rehabil. 2011;90:5–16.
Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A. Swiss national community survey on functioning after spinal cord injury: Protocol, characteristics of participants and determinants of non-response. J Rehabil Med. 2016;48:120–30.
Lai DWL. Effect of financial costs on caregiving burden of family caregivers of older adults. SAGE Open. 2012;2:2158244012470467.
Hu X, Dolansky MA, Zhang F, Qu M. Factors associated with the caregiver burden among family caregivers of patients with heart failure in southwest China. Nurs Health Sci. 2016;18:105–12.
Saunders MM. Factors associated with caregiver burden in heart failure family caregivers. West J Nurs Res. 2008;30:943–59.
Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA 2014;311:1052–60.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101.
Mandelbaum DG. The study of life history: gandhi. Curr Anthropol. 1973;14:177–206.
Pertl MM, Sooknarine-Rajpatty A, Brennan S, Robertson IH, Lawlor BA. Caregiver choice and caregiver outcomes: a longitudinal study of Irish spousal dementia caregivers. Front Psychol. 2019;10:1801. Epub 2019/08/29
Schulz R, Beach SR, Cook TB, Martire LM, Tomlinson JM, Monin JK. Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging Ment Health. 2012;16:712–21.
Fekete C, Tough H, Brinkhof MWG, Siegrist J. Does well-being suffer when control in productive activities is low? A dyadic longitudinal analysis in the disability setting. J Psychosom Res. 2019;122:13–23. Epub 2019/05/28
Graf R, LeLaurin J, Schmitzberger M, Freytes IM, Orozco T, Dang S, et al. The stroke caregiving trajectory in relation to caregiver depressive symptoms, burden, and intervention outcomes. Top Stroke Rehabilitation. 2017;24:488–95.
Stucki G, Bickenbach J. The implementation challenge and the learning health system for SCI initiative. Am J Phys Med Rehabil. 2017;96:S55–s60. Epub 2017/01/07
Chan RCK. How does spinal cord injury affect marital relationship? A story from both sides of the couple. Disabil rehabilitation. 2000;22:764–75.
Springate BA, Tremont G. Dimensions of caregiver burden in dementia: impact of demographic, mood, and care recipient variables. Am J Geriatr Psychiatry. 2014;22:294–300.
Lu N, Liu J, Lou VWQ. Exploring the reciprocal relationship between caregiver burden and the functional health of frail older adults in China: a cross-lag analysis. Geriatr Nurs. 2016;37:19–24.
Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller EL, et al. Evidence for stroke family caregiver and dyad interventions: a statement for healthcare professionals from the American Heart Association and American Stroke Association. Stroke 2014;45:2836–52. Epub 2014/07/19
Reinhard S, Given B, Petlick N, Bemis A. Supporting family caregivers in providing care. In: Hughes R, editor. patient safety and quality: an evidence-based handbook for nurses. Rockville: Agency for Healthcare Research and Quality 2008.
Chien LY, Chu H, Guo JL, Liao YM, Chang LI, Chen CH, et al. Caregiver support groups in patients with dementia: a meta-analysis. Int J Geriatr psychiatry. 2011;26:1089–98. Epub 2011/02/11
Huang J, Pacheco Barzallo D, Rubinelli S, Münzel N, Brach M, Gemperli A. What influences the use of professional home care for individuals with spinal cord injury? A cross-sectional study on family caregivers. Spinal Cord. 2019;57:924–32.
Visser-Meily A, van Heugten C, Post M, Schepers V, Lindeman E. Intervention studies for caregivers of stroke survivors: a critical review. Patient Educ counseling. 2005;56:257–67. Epub 2005/02/22
Coon DW, Gallagher-Thompson D, Thompson LW. Innovative interventions to reduce dementia caregiver distress: a clinical guide. New York: Springer; 2003. P.
Trezzini B, Brach M, Post M, Gemperli A. Prevalence of and factors associated with expressed and unmet service needs reported by persons with spinal cord injury living in the community. Spinal Cord. 2019;57:490–500. Epub 2019/01/31
Acknowledgements
We would like to express our gratitude to the Swiss National Science Foundation for funding this project as well as to the participants for their time and engagement. We also acknowledge the team of the Informal Care Project for their support and Natalie Lustenberger (NL) for her commitment and rigor in the recruitment and data collection as well as in the transcription of the interviews. We are grateful to Lisa Adey, who carefully checked the translation of all quotes from the interviews. Thank you also to the SwiSCI Steering Committee with its members Xavier Jordan, Fabienne Reynard (Clinique Romande de Réadaptation, Sion); Michael Baumberger, Hans Peter Gmünder (Swiss Paraplegic Center, Nottwil); Armin Curt, Martin Schubert (University Clinic Balgrist, Zürich); Margret Hund-Georgiadis, Kerstin Hug (REHAB Basel, Basel); Laurent Prince (Swiss Paraplegic Association, Nottwil); Heidi Hanselmann (Swiss Paraplegic Foundation, Nottwil); Daniel Joggi (Representative of persons with SCI); Nadja Münzel (Parahelp, Nottwil); Mirjam Brach, Gerold Stucki (Swiss Paraplegic Research, Nottwil); Armin Gemperli (SwiSCI Coordination Group at Swiss Paraplegic Research, Nottwil).
Funding
This project was supported by the Swiss National Science Foundation [grant number: 160158]. Open Access funding provided by Universität Luzern.
Author information
Authors and Affiliations
Contributions
CZ was involved in the design of the study, supervised data collection, conducted data analysis and interpreted the findings, was responsible for drafting, revising, and finalizing the manuscript for submission. JA was involved in interpreting the findings, drawing implications for practice as well as in drafting, revising, and finalizing the manuscript for submission. SR developed the study protocol and contributed to revising the manuscript. AG and MB developed the study protocol, provided feedback, and approved the manuscript draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical treatment of human volunteers were followed throughout the study. The Ethics Committee of Northeast and Central Switzerland claimed no jurisdiction because no health-related data were collected. All participants have signed a written consent form.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zanini, C., Amann, J., Brach, M. et al. The challenges characterizing the lived experience of caregiving. A qualitative study in the field of spinal cord injury. Spinal Cord 59, 493–503 (2021). https://doi.org/10.1038/s41393-021-00618-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00618-4
This article is cited by
-
Exploring caregivers’ perceptions of community-based service requirements of patients with spinal cord injury: a qualitative study
BMC Primary Care (2023)
-
A qualitative exploration of the dynamics of guilt experience in family cancer caregivers
Supportive Care in Cancer (2023)
-
Perception of facing life's challenges in patients with spinal cord injury in Iran: a qualitative study
BMC Psychology (2022)
-
Self-Efficacy and Psychological Well-Being of Family Caregivers of Persons with Spinal Cord Injury
Psychological Studies (2022)