Abstract
Study design
Cross-sectional study.
Objectives
To describe the socio-demographics, injury characteristics, prevalence of shoulder and neck symptoms, weekly participation in leisure time physical activity (LTPA) and quality of life (QoL) of individuals with spinal cord injury in Denmark (SCI).
Setting
Nation-wide community survey, Denmark.
Methods
Individuals with SCI for >2 years were included from three SCI rehabilitation departments. Questionnaire data regarding socio-demographic details, SCI injury characteristics, medical history, shoulder and neck symptoms, LTPA and QoL were collected.
Results
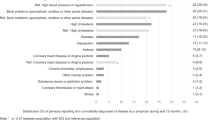
Of 2454 potential participants, 1517 (62%) responded to the survey (mean age = 56.2, SD 16.1, 37% female, 42% tetraplegia, 23% complete SCI, mean time since injury = 16.9, SD 13.5). 75% used some form of assistive mobility device. Responders and non-responders showed no sex or injury type/severity differences. Shoulder and neck symptoms within the past 3 months were reported by 63 and 67% respectively, with 51% reporting shoulder symptoms within the past week. Among those with symptoms, 61% had experienced shoulder symptoms and 56% neck symptoms, for more than 30 days during the previous 3 months. Symptoms often prevented participants from performing their usual activities (due to shoulder symptoms 46%, neck symptoms 41%).
Conclusions
A high prevalence of self-reported shoulder and neck symptoms was found, which may limit physical function and social activities. We succeeded in generating the Danish Spinal Cord Injury Shoulder (DanSCIS) dataset, which comprised a substantial proportion of Danish adults with SCI. Future studies using data from this cohort will investigate patterns and associations between shoulder/neck symptoms, use of assistive mobility devices, LTPA and QoL.
Similar content being viewed by others
Introduction
Around 3,000 individuals living in Denmark (population 5.8 million) have a spinal cord injury (SCI), with an annual incidence of 10–15 cases per million inhabitants for traumatic SCI and non-traumatic SCI respectively [1]. In individuals with SCI, chronic pain, including shoulder pain, is very common, prevalence estimates of shoulder pain vary between 30 and 73% [2, 3], i.e., up to three times the point prevalence for shoulder pain in the general population [4].
The etiology of musculoskeletal shoulder pain in individuals with SCI is multifactorial, where individual factors, such as sex, age and level of SCI [2, 3], as well as shoulder loading from physical and daily life activities [5, 6] have been reported as some of the possible risk factors. But, physical activity (PA) may also improve shoulder symptoms, general health and quality of life (QoL) [7, 8].
The large variation in prevalence estimates and the uncertainty of risk factors for shoulder pain may be due to different study approaches, such as study design, setting, recruitment strategy, and generally small sample sizes [2, 9,10,11,12]. One large cross-sectional observational study (n = 1549) reported on prevalence of shoulder pain the past week (36%), and did not find an association between shoulder pain and PA level, although it did not include detailed information on the amount and intensity levels of the PA that was carried out. Additionally, QoL and information on qualitative descriptors of pain were not reported [3]. The latter is assumed to be a relevant aspect for both diagnosis and treatment. Both among individuals with SCI and in the general population, shoulder pain is associated with co-occurring pain at other body sites, primarily in the neck, but also elsewhere in the upper extremity. Therefore, addressing neck symptoms is of further relevance [13, 14].
Generally, there is lack of knowledge about the extent and characteristics of shoulder symptoms, including limitations in performing usual activities, and associations with weekly participation in PA (amount, intensity) and QoL, which are important information for optimizing diagnostics, rehabilitation, injury prevention strategies and policy-making. Before proceeding to analytical studies, in this descriptive paper, we detail the design, recruitment procedures, data collection, and assessment tools for the nation-wide cross-sectional ‘Danish Spinal Cord Injury Shoulder Cohort (DanSCIS)'. Part of investigating this population’s representativeness is to report and compare the results of socio-demographics with similar populations, the SCI injury characteristics and the main self-reported outcome measures. Therefore, the objectives of this paper were to describe the socio-demographics and SCI injury characteristics, and to report the prevalence of shoulder and neck symptoms, overall weekly participation in leisure time PA (LTPA) (amount, intensity) and QoL of individuals with SCI.
Methods
Study design
The study is a mixed-mode [15], cross-sectional, observational study of individuals with SCI living in Denmark. Reporting of the study follows the STROBE guidelines (STrengthening the Reporting of OBservational studies in Epidemiology) [16].
Study population
For the last 30 years, SCI rehabilitation in Denmark has been considered a highly specialized function for patients with newly acquired SCI. Study participants were Danish individuals with SCI registered in the patient registry databases at one of the following clinics: (1) Department for Spinal Cord Injuries, Rigshospitalet; (2) Spinal Cord Injury Centre of Western Denmark, Viborg Regional Hospital; and (3) Specialist, Rehabilitation Centre, Rødovre. Clinics 1 and 2 are the two national hospitals offering health care to individuals with SCI. Clinic 3 is a private rehabilitation centre with public funding, offering health care to individuals with polio and various types of physical injuries including SCI.
Inclusion criteria
Individuals with SCI (traumatic event (e.g., traffic accident, fall) or non-traumatic events (e.g., infection, tumors)), who sought health care for SCI-related problems within the past 3 years at the involved clinics, were 18 years or older, and able to understand spoken and written Danish were included in the study.
Exclusion criteria
We excluded individuals who were less than 2 years post SCI, in order to minimize influence of the immediate consequences of the SCI from cognitive, emotional and social factors on self-reported symptoms as seen in the acute state. In addition, individuals were excluded if they had other severe neurological disorders (e.g., stroke or traumatic brain disease/injury) causing a cognitive disorder, or severe degenerative diseases.
Patient registry databases
Patient registry databases at the three recruitment clinics were used to extract civil registration numbers (CPR) (a unique government-issued identification number for all residents), contact information and SCI injury characteristics. The registry databases contain patient-specific information regarding examination, treatment and rehabilitation. The time period for data extraction was from the inception of each patient registry database (~1990) to 2016 (December). Registration number duplicates were eliminated and the most recent contact information was used to contact potential participants.
Data collection and variables
A personalized cover letter was developed with inspiration from Dillman et al. [15], containing a short description of the study, how the potential participant was identified, what the data would be used for, and information regarding confidentiality. Lastly, the cover letter was accompanied by instructions on how to fill out a web-based questionnaire. The cover letter, the instructions and the electronic questionnaire were pilot-tested by both clinical experts and individuals with SCI and the process led to revisions of the invitation letter regarding wording, project information and the inclusion of institutional logos. In the web-based questionnaire, corrections of wording/typing errors were made, and additional explanations were added to the following items: socio-demographic characteristics, PA, and medicine intake for preventing/treating shoulder pain. Additionally, shaded diagrams defining the shoulder and neck areas were added to questions related to shoulder and neck symptoms.
The web-based questionnaire included the following validated questionnaires: Standardized Nordic Questionnaire (SNQ) for shoulder and neck symptoms [17], Wheelchair User’s Shoulder Pain Index (WUSPI) for targeting activity limitation resulting from shoulder pain [18, 19], McGill Pain Questionnaire (MPQ) for assessing the intensity and quality of pain [20] (results will be presented in a subsequent publication). LTPA Questionnaire for people with SCI (LTPAQ-SCI) [21], International SCI QoL Basic Data Set [22] and International Spinal Cord Injury Socio-demographic Data Set [23]. In addition to the validated questionnaires listed above, the DanSCIS questionnaire included questions on use of medication for prevention and/or treatments for shoulder pain within the past 3 years (results will be presented in a subsequent publication), and types of assistive mobility devices for use during walking (walkers, crutches, canes or other), additional questions for individuals using wheelchairs (results will be presented in a subsequent publication), included duration of wheelchair use, number of wheelchair transfers per day, car driving, type of automobile, history of shoulder symptoms, and the presence of hand and elbow dysfunction were included [24]. In total, the questionnaire consisted of 84 questions in eight electronic pages, estimated to take between 15 and 20 min to complete. During pilot testing, participants were asked how long time it took to fill in the questionnaire. As an alternative to the web-based questionnaire, it was possible to complete a 12-page paper-based questionnaire, if requested (see supplementary material Appendix 1 for a full presentation of the cover letter, instructions and questionnaire used).
Information about the study and the motivation to participate was given through advertisements in relevant consumer magazines, self-advocacy organizations and relevant homepages/social media.
Before mailing the cover letter, the contact list extracted from the three recruitment clinics was validated against the Civil Registration System regarding current living status (i.e., alive, deceased, or emigrated). Afterwards, all potential participants received a cover letter containing instructions and a personal code for the web-based questionnaire. If the potential participants had not returned their questionnaire within 3 weeks from the initial posting, a reminder, including the cover letter containing the code for the web-based questionnaire, was resent. If there was no response within 6 weeks, a second reminder was sent via a secured digital post, ‘e-Boks', which is a Danish Public Digital Post, for public authorities to send digital messages. One-week later, the third reminder was mailed to the participant’s home address, including the initial cover letter containing the code for the web-based questionnaire and the paper-based questionnaire along with a stamped return envelope.
The data collection occurred between May 2017 to August 2017 (10 weeks).
Standardized Nordic Questionnaire (SNQ)
The SNQ includes a general section that extracts musculoskeletal health information for each part of the body, and a specific section focusing on the lower back and neck/shoulders [17]. For the current study, we used six of the 17 neck/shoulder questions from the specific section. A shaded diagram of the body defining the neck and shoulder areas on a body image was added to the questionnaire. Using the diagram, the study participants answered either ‘Yes' or ‘No' to, ‘Have you had any presence of musculoskeletal symptoms, in one or both shoulders, within the past 3 months?' (Item was mandatory). If answering affirmatively, they were asked three additional questions; (1) ‘For how many days have you had these symptoms within the past 3 months?' with the response categories of ‘1–7 days', ‘8–30 days', ‘More than 30 days' or ‘Every day'; (2) ‘Have your symptoms prevented you from performing your usual activities (at home/outside the home)?' with response categories of either ‘Yes' or ‘No'; and lastly (3) ‘Have you had shoulder symptoms at any time during the past 7 days?' with response categories of either ‘Yes' or ‘No'.
For neck symptoms, the study participants were asked two questions; (1) ‘For how many days have you had these symptoms within the past 3 months?' ('0 days', ‘1–7 days', ‘8–30 days', ‘More than 30 days' or ‘Every day'), and (2) ‘Have your symptoms prevented you from performing your usual activities (at home/outside the home)?' ('Yes' or ‘No') [17]. The SNQ has previously been shown to be a reliable and feasible screening and surveillance tool in able-bodied that can assist medical examinations [25, 26]. The SNQ instrument assesses 12-month symptom prevalence. For this study, a 3-month prevalence was used to assess chronic symptoms.
Leisure Time Physical Activity Questionnaire for people with Spinal Cord Injury (LTPAQ-SCI)
Participation in LTPA was assessed by the LTPAQ-SCI asking study participants about PA performed within the past 7 days as follows: ‘During the last 7 days, on how many days did you do mild/moderate/heavy intensity LTPA?' and ‘On those days, how many minutes did you usually spend doing mild/moderate/heavy intensity LTPA?' [21]. The LTPAQ-SCI was scored by calculating the mean number of minutes per day of LTPA performed at mild, moderate, and heavy intensities, and a total LTPA score was calculated by summing minutes per day of activity across the three intensities. Furthermore, participants were asked about which PA they were mostly involved in. Evidence has been provided of the reliability and criterion validity of the LTPAQ-SCI as a brief measure of LTPA performed by people with SCI [21]. For reference of maximum values of relevant weekly minutes of LTPA activity, we used results from a previous study on athletes with SCI [27]. Before calculating total score, less than 30 responses were excluded. A Danish version of the LTPAQ-SCI has been translated and cross-culturally adapted based on recommended guidelines, in collaboration with the developers [28].
International Spinal Cord Injury Quality of Life Basic Data Set
QoL was measured by the International SCI QoL Basic Data Set, consisting of three items regarding satisfaction with overall QoL, satisfaction with physical health, and satisfaction with psychological health for the past 4 weeks [29], which has a good construct and convergent validity for individuals with SCI [22]. Participants were asked: ‘Thinking about your own life and personal circumstances, how satisfied are you with your life as a whole (physical health, psychological health (emotions and moods)) in the past 4 weeks?' All three items are rated on a numeric rating scale (NRS) from 0 (completely dissatisfied) to 10 (completely satisfied).
International Spinal Cord Injury Socio-demographic Data Set and injury characteristics
Socio-demographic status was assessed by questions concerning age, sex, marital status, household composition, years of formal education and primary occupation [23]. SCI etiology, severity (impairment/completeness), and time since injury were selected as indicators of SCI characteristics. SCI etiology was classified into ‘traumatic/non-traumatic', impairment was classified into ‘paraplegia/tetraplegia', and injury completeness was classified into ‘incomplete/complete'. The dichotomized variable on impairment was merged, with a self-reported variable on their level of SCI injury (cervical, thoracic, lumbar or sacral injury), to calculate a combined self-reported/medical record-based variable. Responses of a ‘cervical injury’ were categorized as ‘tetraplegia', and the remaining responses as ‘paraplegia'. In this process, we found a relative low number of incongruences (n = 134). When this occurred, information from the medical record was used. Information on impairment and completeness, were drawn from medical registrations of neurological level of injury, and classifications based on the American Spinal Injury Association Impairment Scale [30].
Supplementary questions
The use of assistive mobility devices was assessed by the following items: ‘Do you use a wheelchair?' ('Yes' or ‘No') (Item was mandatory), and if yes, they were asked; ‘Which type of wheelchair?', ('manual wheelchair', ‘electrical wheelchair' or ‘both'). Furthermore, participants were asked: ‘Do you use one or more assistive devices for walking?' ('Yes' or ‘No'), if answering affirmatively, participants could select: ‘walkers', ‘crutches', ‘canes' or ‘other'. Participants were allowed to choose more than one response option.
Data quality control
All data were coded and recorded in REDCap (Research Electronic Data Capture system). Data were imported to the SPSS Statistics version 24.0 for Windows (IBM, Armonk, NY) to create a database which is stored at the Open Patient data Explorative Network, Odense University Hospital/Department of Clinical Research. A quality control process, including range checks and ensuring accurate data importing and data transfers, was carried out. Information from the paper-based questionnaires was assessed by double data entry into the REDCap system to ensure uniformity of the variables and to minimize data entry errors. Any discrepancies and decisions made were documented and subsequently corrected. When the quality control process and data cleaning were completed, the database was locked. There were no requirements for number of required responses to be included in the dataset.
Statistical analysis
Continuous variables were tested for normality (Shapiro Wilk test, histogram and quantile-quantile (Q-Q plots)). Descriptive statistics (number of observations, percentages, mean and standard deviation (SD), median (interquartile range, IQR)(Q3 = 75th percentile - Q1 = 25th percentile)) were used to describe socio-demographic status, injury characteristics, shoulder and neck symptoms, LTPA and QoL. The variables on use of assistive mobility device were grouped into the following categories; ‘Walking without assistive devices', ‘Walking with assistive devices', ‘Manual wheelchair', ‘Electric wheelchair', ‘Both manual and electric wheelchair'. For the purpose of the analysis, the number of days of shoulder and neck symptoms was grouped into 30 days or less, or more than 30 days. Additionally, neck symptoms for 0 days, 1 day or more were grouped into ‘No' and ‘Yes', respectively. Despite non-normal distributions, the variables on LTPA are presented in both median and mean, to allow for better comparisons with other studies. Item-response rates are presented as the number of observations and percentages relative to the total number of included participants. Differences between responders and non-responders were analyzed with an Independent t test or χ2 test, where appropriate. All statistical tests were two-tailed, the level of significance was set at p < 0.05.
Ethics
An advisory board of patient and expert representatives were actively involved in the preparation of the patient recruitment materials, pre-testing of the questionnaire, and will be part of the knowledge dissemination process. Informed consent to participate according to the Declaration of Helsinki [31] was presumed, based on a returned questionnaire.
Results
Participants
After exclusion of double registrations within and between hospitals/centers (n = 486), 2670 potential participants were initially identified based on the inclusion criteria. In all, 216 were ineligible, therefore 2454 individuals were invited to participate in the study, and the total number of respondents included in the analysis was 1517, resulting in a response rate of 62%. Details of response, participation and exclusion are presented in Fig. 1. The paper-based questionnaire was filled out by 239 participants (15%).
Socio-demographic status and injury characteristics
All but three of the demographic and SCI characteristic response rates were above 94%: etiology (85%), completeness of injury (69%), and time since injury (77%) (Table 1). Mean age of all participants was 56.2 years (ranged from 18 to 97 (Table 1)). Sixteen participants were above the age of 80. The mean level of years of formal education was 12.5 (ranged 7–26 years, not shown in table), and mean time since injury was 16.9 years (ranged from 2 to 85 years). Due to the level of missing values in the American Spinal Injury Association (ASIA) Impairment Scale (AIS) grade and our primary interest in being able to divide participants according to level of injury, we report level of injury and the AIS grade separately. The included participants had traumatic SCI (52%), paraplegia (58%), and incomplete SCI (77%). The majority of the participants used some form of assistive mobility device (n = 1139; 75%), while 25% were able to walk without assistive devices. Using a manual wheelchair was the dominant assistive device, although for a proportion of the participants, wheelchair use was combined with another assistive mobility device.
Shoulder and neck symptoms
The majority of items had response rates of more than 94%, whereas the LTPA had lower response rates (76–83%) (Table 2). Of all the participants, shoulder and neck symptoms within the past 3 months were reported by 63 and 67%, respectively, with 51% reporting shoulder symptoms within the past week (Table 2). Among those with symptoms, 61 and 56% had experienced shoulder and neck symptoms respectively, for more than 30 days during the previous 3 months. More than half of the participants with symptoms (56%) reported both shoulder and neck symptoms within the past 3 months.
Symptoms often prevented participants from performing their usual activities at home or outside the home (shoulder symptoms 46%, neck symptoms 41%). On average, the current level of symptoms on the Numeric Pain Rating Scale (NPRS) corresponded to moderate pain (~4 out of 10) for both shoulder and neck.
Leisure time physical activity
Weekly amount of LTPA ranged between 0 and 6235 min/week (Table 2) with only 26 individuals presenting with total LTPAQ scores above 3000 min/week. Generally, the participants performed LTPA at mild intensities, for the majority of the time (median 180 (IQR 380) min/week), and slightly over 10% of the participants reported no LTPA whatsoever. The weekly total score of LTPA at combined moderate/hard intensity was mean 259.37, median 120.0 (IQR 360) min/week (not shown in Table 2).
Quality of life
Reporting of general QoL (overall well-being) and satisfaction with psychological health averaged ~6.5 out of a maximum of 10, while satisfaction with physical health was somewhat lower at 5.4 (Table 2).
Comparison of responders and non-responders
The results include the five respondents who self-selected to participate in the study (Fig. 1). Responders (1517) and non-responders (942) showed no differences regarding sex, level of SCI (tetraplegia/paraplegia), and severity of injury (complete/incomplete), but the responders were on average 4 years older, with longer time since injury (≈ 2 years), and had less often experienced a traumatic injury (≈ 6%) (Table 3).
Discussion
We described the clinical database sources, design, questionnaire development, participant recruitment/response rate, and data quality checks for the population-based DanSCIS dataset. Further, based on socio-demographic factors and injury characteristics, we succeeded in recruiting a substantial proportion of the Danish target population of adults with long-standing SCI (n ≈ 3000) (response-rate of 62%). Participants reported a high prevalence of shoulder and neck symptoms (63 to 67%, past 3 months), as well as variations in weekly amounts of LTPA.
The current socio-demographics and injury characteristics appear to be similar to those reported in studies from other countries on SCI populations [1, 3, 32,33,34,35,36,37,38]. However, for some studies, the sample sizes were relatively small, and the populations were sometimes restricted to include individuals with a traumatic injury or paraplegia only, making them less comparable with the general SCI population [9, 32,33,34, 38]. Socio-demographics of the DanSCIS (age, sex) are broadly in line with a recent Swiss SCI community cross-sectional study (n = 1549) (age 56.2 ± 16 vs. 52.3 ± 15, sex 37% vs. 39%) [3], although, our DanSCIS dataset had a smaller proportion of individuals with complete SCI than the Swiss study (23% vs. 42%). The high proportion of incomplete injuries in the DanSCIS study (77%) is in line with previous findings from a Danish specialized rehabilitation hospital (~70%) [37], the Norwegian Spinal Cord Injury Registry (NorSCIR) (86%) and the Nordic Spinal Cord Injury Registry (NordicSCIR) (~80%) [36, 39]. Furthermore, additional results on socio-demographic status (marital and occupational status) are comparable to those of SCI individuals involved in an Irish study [35].
Our findings of high prevalence and severity of self-reported shoulder and neck symptoms are similar to a previous study from Turner and colleagues, where 76% of a mixed SCI population reported upper extremity pain after their SCI. Additionally, pain was experienced over a period of 75 days in the past 3 months and participants were restricted from usual activities for ~18% of the time [13]. The one-week prevalence of shoulder symptoms reported in the current study is somewhat higher than previously found in a comparable study (51% vs. 39%) [3], and our findings on three-month prevalence of neck symptoms (67%) is also higher than previously reported (33%) [13]. This could be due to a higher proportion of tetraplegic individuals included in this study (42% vs. 30%). Additionally, the discrepancies observed may be due to study sizes, differences in populations included and the methodologies used. On the whole, studies showed shoulder and neck symptom prevalence’s which are higher than the able-bodied population (1-month prevalence 17–31% and 15–41%, respectively) [4, 40].
The results on LTPA suggest a very large variation among the participants, and both the mean scores of individual LTPA intensities (mild, moderate, hard) and the total LTPA score, are higher than previously found [41, 42], although somewhat closer to the results from the SwiSCI cohort study [42]. Differences in the methodology used to assess LTPA and the inclusion of SCI populations at different functional levels may account for the different study results. In our study, 25% of the participants were able to walk without assistive devices, which is higher than previously reported [41, 42]. In contrast to the study by Ginis and colleagues, information on LTPA included in the current study and in the SwiSCI cohort study [42] were self-reported, which may have introduced an overestimation of the LTPA level, especially for mild and moderate intensities.
The quality of life scores from the DanSCIS study were consistent with previous studies, showing scores between 5.5 and 7.1, with the lowest score for physical health [35, 43].
Previous literature points towards a negative association between shoulder and neck pain and QoL [44, 45]. Furthermore, few studies have examined the associations between physical activity and shoulder symptoms in SCI and results are equivocal to whether physical activity is a possible risk or preventive factor [5, 46, 47]. Multivariable analyses are needed to further investigate the associations between shoulder symptoms, use of assistive devices for mobility, quality of life and physical activity.
In this survey, a mixed-mode design was used, combining contact delivery modes and different modes of data collection. This design is attractive, due to the possibility of reducing overall study costs, and due to the potential to reach different types of participants [48]. It was therefore expected that this design would potentially decrease both coverage errors and non-response errors, hence increasing response rate and overall representation of the final sample. However, a mixed-mode design may introduce bias by using different modes [15]. Even though considerations were put into the current design phase in order to avoid mode bias (by replicating the mode design from the web-based to the paper-based mode), we cannot exclude the possibility that the type of mode had an influence on the answers provided. Apart from the items related to wheelchair usage and 3 months prevalence of shoulder symptoms, survey questions were not mandatory. This methodological decision has presumably led to a greater amount of missing values in the measurement scales, where total scores are calculated, such as the LTPAQ-SCI scale, although a mandatory answer to all survey questions could also have entailed some participants leaving the survey due to an unwillingness to provide answers. The DanSCIS survey is the first study of its size to include the LTPAQ-SCI as a self-report measure. To the authors’ knowledge, no guidelines exist on how to calculate summary scores of LTPAQ-SCI, when missing data occur, nor are we familiar with any recommendations on data-cleaning rules, as provided for other SCI relevant measurements, e.g., socio-demographic variables [23]. The 62% response rate is somewhat higher compared to cross-sectional studies of similar sizes within this population, with response rates ranging from 41 to 49% [3, 32, 33, 35, 49]. Participants were somewhat older than non-responders and had sustained their injuries for a longer period of time. Moreover, a difference between responders and non-responders was found in their cause of injury, which may introduce a potential bias, but the clinical relevance of that difference is questionable. The similarity between groups in sex, injury level and completeness, points towards a representative population of adults with long-term SCI. For future studies, we recommend the use of a mixed-mode design to increase response rates and a discussion about the survey question requirements regarding measurement scales from where a total score is derived, in order to avoid missing data.
Strengths and limitations
We may have missed participants if, for some reason, they had not visited the outpatient clinics at the Danish SCI rehabilitations hospital departments over the 3-year period as expected, or had not been referred to a specialized rehabilitation center at all. Although this could affect the sample size, we expect our invitation to participate in the DanSCIS study accessed the majority of the Danish SCI population. Currently, no reliable estimate of the prevalent SCI population in Denmark exists, although previous results point to an approximate prevalence of about 3000 individuals [1]. Due to limitations of the electronic databases/registry systems, it was not possible to preclude individuals fulfilling exclusion criteria, such as additional neurological diagnoses with a cognitive disorder, or severe degenerative diseases. However, the survey included specific questions, which provided the possibility of identifying these respondents. We did not include information about other health problems the individual may be experiencing (e.g., urinary tract problems, spasticity and contractures), although we are quite aware that these aspects are of great importance for the overall physical and mental health of individuals with SCI. We wanted the survey to have the minimum number of questions possible to answer our research questions to maximize our response rate. The strengths of this study are the use of a mixed-mode design, inclusion of selected validated datasets and questionnaires, as well as the inclusion of a large and representative population. We thereby fulfilled important general quality criteria, for surveying associations between shoulder symptoms, LTPA and QoL for people with SCI in Denmark.
Conclusion
In conclusion, we have provided a thorough description of clinical database sources, design, questionnaire development, participant recruitment/response rate, and data quality checks for the population-based DanSCIS dataset. We succeeded in collecting socio-demographics, SCI injury characteristics and self-reported outcome measures on a substantial proportion of Danish adults with long-term SCI. Future studies using data from this cohort will investigate patterns and associations between shoulder/neck symptoms, use of assistive mobility devices, LTPA and QoL. A high prevalence of self-reported shoulder and neck symptoms was found and weekly LTPA and QoL varied greatly. Overall, the number of minutes of LTPA performed at heavy intensity weekly was limited.
Data availability
Unidentifiable data may be available upon request and approval from the Danish Data Protection Agency.
References
Biering-Sørensen F. Behandling og (genop) træning. Ugeskr Laege. 2001;163:2766.
Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, Part I: epidemiology, etiology, and pathomechanics. J Spinal Cord Med. 2003;27:4–17.
Bossuyt FM, Arnet U, Brinkhof MWG, Eriks-Hoogland I, Lay V, Muller R, et al. Shoulder pain in the Swiss spinal cord injury community: prevalence and associated factors. Disabil Rehabil. 2018;40:798–805.
Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33:73–81.
Akbar M, Brunner M, Ewerbeck V, Wiedenhöfer B, Grieser T, Bruckner T, et al. Do overhead sports increase risk for rotator cuff tears in wheelchair users? Arch Phys Med Rehabil. 2015;96:484–8.
Ferrero G, Mijno E, Actis MV, Zampa A, Ratto N, Arpaia A, et al. Risk factors for shoulder pain in patients with spinal cord injury: a multicenter study. Musculoskelet Surg. 2015;99:S53–56.
Kljajić D, Eminović F, Dopsaj M, Pavlović D, Arsić S, Otašević J. The impact of sports activities on quality of life of persons with a spinal cord injury. Zdr Varst. 2016;55:104–11.
Fullerton HD, Borckardt JJ, Alfano AP. Shoulder pain: a comparison of wheelchair athletes and nonathletic wheelchair users. Med Sci Sports Exerc. 2003;35:1958–61.
Alm M, Saraste H, Norrbrink C. Shoulder pain in persons with thoracic spinal cord injury: prevalence and characteristics. J Rehabil Med. 2008;40:277–83.
Gironda RJ, Clark M, Neugaard B, Nelson A. Upper limb pain in anational sample of veterans with paraplegia. J Spinal Cord Med. 2004;27:120–7.
Mulroy SJ, Hatchett P, Eberly VJ, Haubert LL, Conners S, Requejo PS. Shoulder strength and physical activity predictors of shoulder pain in people with paraplegia from spinal injury: prospective cohort study. Phys Ther. 2015;95:1027–38.
Kentar Y, Zastrow R, Bradley H, Brunner M, Pepke W, Bruckner T, et al. Prevalence of upper extremity pain in a population of people with paraplegia. Spinal Cord. 2018;56:695–703.
Turner JA, Cardenas DD, Warms CA, McClellan CB. Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil. 2001;82:501–9.
Hartvigsen J, Davidsen M, Hestbaek L, Sogaard K, Roos EM. Patterns of musculoskeletal pain in the population: a latent class analysis using a nationally representative interviewer-based survey of 4817 Danes. Eur J Pain. 2013;17:452–60.
Dillman DA, Smyth JD, Christian LM. Internet, phone, mail, and mixed-mode surveys: the tailored design method. Hobroken, New Jersey: John Wiley & Sons; 2014.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Erg. 1987;18:233–7.
Curtis KA, Roach KE, Applegate EB, Amar T, Benbow CS, Genecco TD, et al. Reliability and validity of the wheelchair user’s shoulder pain index (WUSPI). Spinal Cord. 1995;33:595–601.
Salisbury S, Nitz J, Souvlis T. Shoulder pain following tetraplegia: a follow-up study 2–4 years after injury. Spinal Cord. 2006;44:723.
Main CJ. Pain assessment in context: a state of the science review of the McGill pain questionnaire 40 years on. Pain. 2016;157:1387–99.
Ginis KAM, Phang SH, Latimer AE, Arbour-Nicitopoulos KP. Reliability and validity tests of the leisure time physical activity questionnaire for people with spinal cord injury. Arch Phys Med Rehabil. 2012;93:677–82.
Post MWM, Forchheimer MB, Charlifue S, D’Andrea Greve JM, New PW, Tate DG. Reproducibility of the international spinal cord injury quality of life basic data set: an international psychometric study. Spinal Cord. 2019;57:992–8.
Chen Y, Charlifue S, Noonan V, New P, Gururaj G, Katoh S, et al. International Spinal Cord Injury Socio-Demographic Basic Data Set (Version 1.0) – 2020.01.15. https://www.iscos.org.uk/international-sci-socio-demographic-data-sets.
Samuelsson K, Tropp H, Gerdle B. Shoulder pain and its consequences in paraplegic spinal cord-injured, wheelchair users. Spinal Cord. 2004;42:41.
Ohlsson K, Attewell RG, Johnsson B, Ahlm A, Skerfving S. An assessment of neck and upper extremity disorders by questionnaire and clinical examination. Ergonomics. 1994;37:891–7.
Palmer K, Smith G, Kellingray S, Cooper C. Repeatability and validity of an upper limb and neck discomfort questionnaire: the utility of the standardized Nordic questionnaire. Occup Med. 1999;49:171–5.
Juul-Kristensen B, Bech C, Liaghat B, Cools AM, Olsen HB, Søgaard K, et al. Assessment of shoulder rotation strength, muscle co-activation and shoulder pain in tetraplegic wheelchair athletes - a methodological study. J Spinal Cord Med. 2020. https://doi.org/10.1080/10790268.2020.1803659. [Epub ahead of print].
Larsen CM, Juul-Kristensen B. Final report on Leisure Time Physical Activity Questionnaire for People with Spinal Cord Injury (LTPAQ-SCI) outcome questionnaire: Translation and Cross-Cultural Adaptation of the Danish Version. Odense, Denmark, 2017 (Avaliable upon request).
Charlifue S, Post MWM, Biering-Sorensen F, Catz A, Dijkers M, Geyh S, et al. International spinal cord injury quality of life basic data set. Spinal Cord. 2012;9:672–5.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
World Medical A. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Andresen S, Biering-Sørensen F, Hagen E, Nielsen J, Bach F, Finnerup N. Pain, spasticity and quality of life in individuals with traumatic spinal cord injury in Denmark. Spinal Cord. 2016;54:973
Andresen SR, Biering-Sørensen F, Hagen EM, Nielsen JF, Bach FW, Finnerup NB. Cannabis use in persons with traumatic spinal cord injury in Denmark. J Rehabil Med. 2017;49:152–60.
Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A. Swiss national community survey of functioning after spinal cord injury: protocol, characteristics of participants and determinants of non-response. J Rehabil Med. 2016;48:120–30.
Burke D, Lennon O, Fullen BM. Quality of life after spinal cord injury: The impact of pain. Eur J Pain. 2018;22:1662–72.
Halvorsen A, Pettersen AL. NorSCIR Årsrapport for 2016 med plan for forbedringstiltak. Trondheim: Nasjonalt registersekretariat; 2017.
Regionshuset. Rygmarvsskadebehandling- og rehabilitering i Vestdanmark. Viborg: Region Midt; 2010.
Halvorsen A, Pettersen A, Nilsen S, Halle KK, Schaanning EE, Rekand TJSc. Epidemiology of traumatic spinal cord injury in Norway in 2012–2016: a registry-based cross-sectional study. Spinal Cord. 2019;57:331–8.
Halvorsen A, Pettersen AL. NordicSCIR Årsrapport 2018. Trondheim: Nasjonalt registersekretariat; 2019.
Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15:834–48.
Ginis KA, Arbour-Nicitopoulos KP, Latimer AE, Buchholz AC, Bray SR, Craven BC, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part II: activity types, intensities, and durations. Arch Phys Med Rehabil. 2010;91:729–33.
Rauch A, Hinrichs T, Oberhauser C, Cieza A, Group SS. Do people with spinal cord injury meet the WHO recommendations on physical activity? Int J Public Health. 2016;61:17–27.
Post M, Adriaansen JJ, Charlifue S, Biering-Sørensen F, van Asbeck F. Good validity of the international spinal cord injury quality of life basic data set. Spinal Cord. 2016;54:314.
Silvestri J. Effects of chronic shoulder pain on quality of life and occupational engagement in the population with chronic spinal cord injury: preparing for the best outcomes with occupational therapy. Disabil Rehabil. 2017;39:82–90.
Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1309–15.
Gutierrez DD, Thompson L, Kemp B, Mulroy SJ. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med. 2007;30:251–5.
Medina G, Jesus C, Ferreira D, Pacheco E, Beraldo G, de Franca Urquiza F, et al. Is sport practice a risk factor for shoulder injuries in tetraplegic individuals? Spinal Cord. 2015;53:461.
De Leeuw ED. To mix or not to mix data collection modes in surveys. J Stat. 2005;21:233–55.
Heutink M, Post MW, Wollaars MM, van Asbeck FW. Chronic spinal cord injury pain: pharmacological and non-pharmacological treatments and treatment effectiveness. Disabil Rehabil. 2011;33:433–40.
Acknowledgements
We would like to acknowledge the Department for Spinal Cord Injuries, Rigshospitalet; the Spinal Cord Injury Centre of Western Denmark, Viborg Regional Hospital; and the Specialized Hospital for Polio and Accident Victims for their collaboration and their operational help in recruiting the sample. Furthermore, we would like to acknowledge the study reference group for their valuable inputs.
Funding
This work was funded by grants from the Danish Society of Polio and Accident Victims; the Danish Physiotherapy Research Foundation, the Jascha Foundation and the Vanføre Foundation.
Author information
Authors and Affiliations
Contributions
CML was responsible for the design and completion of the present study. BJK, HK, JH, LHF, EB, LØ and FBS provided support regarding design considerations, as well as, critical feedback on manuscript content. HK and FBS further provided support in data collection at their respective hospital clinics. EB provided statistical support for the analyses. Finally, CML was responsible for all analyses and for finalizing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Ethics approval was obtained from the Danish Data Protection Agency (journal nr. 15/95635) and the Danish Health and Medicines Authority (journal nr. 3-3013-1472/1).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Larsen, C.M., Juul-Kristensen, B., Kasch, H. et al. The Danish Spinal Cord Injury Shoulder (DanSCIS) cohort: methodology and primary results. Spinal Cord 59, 821–831 (2021). https://doi.org/10.1038/s41393-020-00594-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00594-1
This article is cited by
-
Monitoring outcome measures for cardiometabolic disease during rehabilitation and follow-up in people with spinal cord injury
Spinal Cord (2024)
-
Effect of pelvic laparoscopic implantation of neuroprosthesis in spinal cord injured subjects: a 1-year prospective randomized controlled study
Spinal Cord (2022)
-
Treatment of shoulder pain in people with spinal cord injury who use manual wheelchairs: a systematic review and meta-analysis
Spinal Cord (2022)
-
Does the Danish version of the Spinal Cord Lesion-related Coping Strategies Questionnaire measure what we think it measures? A triangulated mixed-methods validation approach
Spinal Cord (2022)