Abstract
Study design
Systematic review and meta-analysis.
Objectives
To identify, critically appraise, and synthesize research findings on non-sensate versus sensate flaps among individuals with spinal cord disease and pelvic pressure ulcers, with pressure ulcer recurrence as primary outcome.
Methods
PubMed, EMBASE, and Cochrane CENTRAL were screened for relevant studies. Data on surgical characteristics, ulcer recurrence, and sensory outcomes were retrieved and tabulated. Risk of bias was assessed with MINORS. The level of evidence was evaluated with GRADE. Meta-analysis was performed when possible.
Results
Meta-analysis of 1794 non-sensate locoregional reconstructions indicated a recurrence rate of 34% within several years (95% CI, 27–42). Twenty-one articles provided data on 75 sensate reconstructions, performed in 74 individuals. Meta-analysis of the sensate reconstructions indicated a recurrence rate of 1% (95% CI, 0–8). Sensate reconstructions were not associated with an increase of wound complications (19%; 95% CI, 7–40) compared with non-sensate ones (34%; 95% CI, 27–42). A very low level of evidence was determined with use of GRADE.
Conclusion
Although of a very low-level, the present evidence suggests that restoration of sensory innervation may be an effective intervention for the prevention of pressure ulcer recurrence among individuals with spinal cord disease. A prospective RCT is needed to confirm or refute the results of this systematic review.
Similar content being viewed by others
Introduction
Every year, between 250,000 and 500,000 people suffer develop spinal cord disease (SCD) [1]. Because SCD results in loss of innervation, individuals with SCD become prone to ulcer formation [2, 3]. It is estimated that over 33% of persons with SCD suffers from a pressure ulcer at this moment [4, 5]. In one-eighth of individuals with SCD, pressure ulcers are listed as the cause of death [6].
The goal of pressure ulcer reconstruction is to improve quality of life and to prevent wound complications such as osteomyelitis, sepsis, and fluid and protein loss through the wound. Because most ulcers occur in proximity of the pelvis, locoregional flaps from the hip or thigh are the current standard of care [7,8,9]. Long-term studies continue to reveal high pressure ulcer recurrence rates of over 50% [8, 10,11,12,13]. Some authors have put forward that flaps harvested from non-sensate tissue may not address what seems to be the essence of the dilemma: the lack of sensory innervation in the tissue at risk [2, 14,15,16,17].
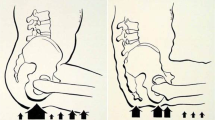
In response, plastic surgeons have set out to restore pelvic sensory innervation by means of several surgical techniques. In low-level lesions such as those caudal to L4/L5, anterior thigh innervation is preserved. In these individuals, pedicled transpositions of sensate anterior thigh tissue to non-sensate risk sites such as the sacrum are possible. In people with high-level lesions, sensory innervation can be restored through microsurgical coaptation between a flap and a sensory nerve located cranial to the level of injury. Examples of such reconstructions are presented in Fig. 1.
Multiple reports on the preventive potential of restoration of sensation exist, but have been dispersed over time and had small sample sizes. At present, a systematic analysis of the evidence on this topic is lacking. The aim of this systematic review is therefore to provide a systematic and meta-analytic comparison of sensate with non-sensate reconstructions for the prevention of pressure ulcer recurrence among individuals with SCD. We hypothesize that sensate reconstructions prevent pressure ulcer recurrence better.
Methods
The report of this systematic review was drafted in concordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18]. As this study concerns a literature review, no ethical approval was required. No review protocol for this meta-analysis was published or registered before this study was undertaken.
Study selection
A clinical librarian was consulted on the search strategy. PubMed, EMBASE and Cochrane Library CENTRAL databases were searched up to November 11th, 2019 with terms relating to pressure ulcers, SCDs, and flap reconstructions, including medical subject headings (MeSH) terms. The search strategy did not use any restrictions. The search strategy is provided as Supplementary Appendix S1. Titles, abstracts, and full-texts were screened by two reviewers (PRZ and RWAV) independently, based on predefined inclusion criteria. Full-texts were only assessed after their abstracts were deemed to be of interest.
Eligibility criteria
Non-sensate flap studies were included if they had over 20 months of follow-up, a sample size of over 20 individuals with SCD, and reported on pressure ulcer recurrence as an outcome. Because the goal of our study was to provide a comprehensive overview of the evidence on sensate reconstructions for the prevention of pressure ulcers among individuals with SCD, and the rarity of sensate reconstructions, we utilized different criteria for the selection of sensate reconstructions reports: these were included as long as they described sensate reconstructions and reported on pressure ulcer recurrence as an outcome, irrespective of sample size. We excluded articles in languages other than English, Dutch, French or German, animal studies, duplicates, conference abstracts and articles without original data. Reference lists of included articles were searched for articles of potential relevance.
Outcomes
Our primary outcome was pressure ulcer recurrence of flaps that were reported to be vital after transfer in case of non-sensate flaps, and vital and sensate in case of sensate flaps.
Pressure ulcer recurrence was defined as a pressure ulcer occurring within the tissue of a previous reconstruction. Additional outcomes of importance included the presence of any postoperative surgical complications and the sensory outcomes of the sensate flaps as reported by individual studies, for example whether a flap developed wound dehiscence or had an intact perception of pain after transfer.
Data extraction
Two reviewers (RWAV and PRZ) extracted data independently in predefined evidence tables. Discrepancies were resolved through discussion. Data collected included: study design, number of individuals, gender, age, type of SCD, ulcer details from before reconstruction (size, location, and history), flap type, amount of stages, re-innervation technique, donor nerve and vessels, recipient nerve and vessels, timing of reconstruction, length of follow-up, pressure ulcer recurrence, modalities used for sensory assessment, and sensory outcomes.
Assessment of risk of bias and level of evidence
As we estimated that many articles would be single-armed reports of surgical results, we chose the MINORS (Methodological index for non-randomized studies) Tool for risk of bias evaluation [19]. Strengths of this tool include that it has been developed specifically for use in surgical systematic reviews, has been validated, and can be used for assessment of single-arm reports as well as comparative studies. Two reviewers critically appraised each study independently, and reached a final verdict through discussion (PRZ and RWAV). The body of evidence was graded using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Working Group guidelines [20].
Statistical analysis
Because we anticipated that we would predominantly identify single-armed observational studies, a meta-analysis of singular proportions was planned using the ‘metaprop’ function and random-effects in RStudio software [21]. I2 was used to quantify heterogeneity. Because we encountered only zero values for sensate flap recurrence, and multiplication with zero results in computational error, we added one hypothetical study with a recurrence in order to be able to perform meta-analysis [22].
Results
Systematic review
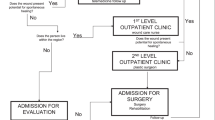
The systematic search retrieved 2301 records. Review of the reference lists of included articles identified one additional record of interest. After deduplication, 1474 records were screened, of which 1401 were excluded based on title and abstract. Seventy-three full text articles were assessed for eligibility, of which 34 were excluded (reasons are presented in Fig. 2) and 39 were included. The references of the identified articles are presented as Supplementary Appendix S2.
Study characteristics
We identified 8 case reports and 13 case series on sensate flaps, and 19 retrospective non-sensate flap cohort studies. Risk of bias assessments of every study are presented as Supplementary Tables S1 and S2.
Risk of bias and level of evidence
As the evidence on sensate reconstructions consisted of small case series and case reports only, their results were judged to be very prone to bias. We did not detect any studies designed with the specific aim to compare sensate with non-sensate flaps. The comparison of the outcomes of sensate and non-sensate flaps in this review was therefore indirect in nature, which was based on a very low level of evidence. An overview of the rating process with supporting explanations is provided in Supplementary Table S3.
Surgical characteristics of the non-sensate reconstructions
An overview of non-sensate locoregional flap types is presented in Supplementary Table S4. All non-sensate reconstructions were performed with use of single-staged, locoregional, pedicled flaps, except for the study by Di Caprio et al. (138 of 1794 flaps, 7.7%). Di Caprio et al used tissue expanders to increase flap size and decrease tension, where they also created the possibility of repeating the procedure in case of recurrence. Rubayi et al. performed a simultaneous Girdlestone procedure during reconstruction to remove pressure points and allow for easier closure. None of the non-sensate flap transfers involved microsurgery. Meta-analysis of the non-sensate flap transfers indicated that 34% developed postoperative wound complications (95% CI, 27–42, 1784 flaps). A forest plot is presented as Supplementary Fig. S1.
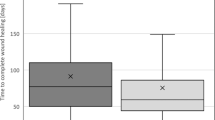
Pressure ulcer recurrence after locoregional reconstruction with non-sensate tissue
An overview of the reports on non-sensate locoregional reconstructions is presented as Supplementary Table S4 (1794 reconstructions in total). The mean length of follow-up of these studies varied from 20 to 62 months. Meta-analysis indicated that overall, 34% (95% CI, 27–42) of non-sensate flaps develops pressure ulcer recurrence within several years. A forest plot is presented in Fig. 3. Fasciocutaneous and musculocutaneous flaps displayed a similar incidence of pressure ulcer recurrence of 22% (95% CI, 18–27, 326 flaps) and 18% (95% CI, 8–36, 190 flaps).
Surgical characteristics of the sensate flap transfers
Ten of 86 (12%) sensate flap transfers, performed in 86 individuals, were unsuccessful because of flap failure (2 cases) or loss of sensation (8 cases) after transfer. Most sensate reconstructions were performed with pedicled flaps harvested from sensate thigh tissue of individuals with a low level SCD (66 of 86 flaps, 77%, performed in 64 individuals). The most frequently used flap was a sensate pedicled tensor fascia latae flap (39 of 86 flaps, 45%, performed in 38 individuals). Thirteen flaps (15%) involved a delay procedure, performed in 13 individuals. Eleven flaps involved microsurgery (11 individuals). A free sensate plantar foot flap was the most commonly used free flap, performed in nine individuals. Meta-analysis indicated that 19% of the sensate reconstructions developed postoperative wound complications (95% CI, 7–40, 54 flaps performed in 53 individuals). A forest plot is presented as Supplementary Fig. S3. A detailed summary of the surgical characteristics of the sensate reconstructions is presented as Table 2 (SCD level, flap type, donor and recipient nerves and vessels, required stages, postoperative wound complications).
Pressure ulcer recurrence after restoration of sensory innervation
We identified the results of 74 individuals with SCD in whom pelvic sensation had been restored through surgery. None of the sensate reconstructions developed pressure ulcer recurrence (0 of 75 flaps, 0%). Meta-analysis (including the hypothetical cohort with one recurrence) indicated a pressure ulcer recurrence rate of 1% (95% CI, 0–8). A forest plot is presented as Supplementary Fig. S2. Fifteen of 21 reports had a mean follow-up of over 24 months. In the report with the longest follow-up period, Thomson et al. describe the results of four persons with SCD who received sensate pedicled fasciocutaneous thigh flaps. Whereas these individuals worked as administrative secretaries and were chair-bound for at least 8 h a day, all remained free of pressure ulcer recurrence despite a follow-up of 9–18 years. The patient and pressure ulcer characteristics, pressure ulcer recurrence rates, and MINORS scores of the sensate reconstruction reports are presented as Table 1.
Sensory outcomes of the sensate reconstructions
Studies assessed sensory outcomes of the transferred flaps with the following modalities: pain perception, pressure discomfort, Semmes-Weinstein monofilament testing, perception of soft touch, vibration perception, hot/cold discrimination, two-point discrimination, static/moving discrimination, pressure/pinch discrimination, discrimination of different objects, dermatomal somatosensory-evoked potentials, bromophenol blue sweat testing, and histology. Nine of 11 free flaps were reported to regain protective sensation. Goldberg et al. demonstrated that sensation could be restored even in free flaps harvested distal to the spinal cord lesion 21 years after the occurrence of SCD. Goldberg and Küntscher et al. confirmed viable sensory nerve fibers to be present in free flaps, with use of histological biopsy. Sekiguchi et al. demonstrated that sensory nerve coaptation seems to restore autonomic nervous system function, as they objectively confirmed that their flaps could produce sweat (which is mediated by the autonomous nervous system). A summary of the sensory outcomes is presented in Supplementary Table S5. The surgical characteristics of these flaps are reported in Table 2.
Discussion
With a recurrence rate of 34% within several years (95% CI, 27–42, 1794 flaps), our meta-analysis indicates that in individuals with SCD, non-sensate locoregional reconstructions are associated with a substantial risk of pressure ulcer recurrence. The available data indicates that surgical restoration of sensory innervation is very effective at preventing pressure ulcer recurrence among individuals with SCD, with a recurrence rate of 1% (95% CI, 0–8). Still, because the sensate reconstruction evidence consists of a small number of case reports and case series, it should be kept in mind that these comparisons are at risk of severe publication bias. Estimating the actual extent of publication bias remains troublesome and whether sensate reconstructions are truly superior to non-sensate locoregional flaps thus continues to be relatively uncertain.
Despite ongoing advances in flap design, long-term studies continue to reveal high rates of pressure ulcer recurrence after use of non-sensate tissue flaps. Repeated recurrences can lead to a shortage of local tissue, increasing the complexity of reconstructive procedures. Several authors therefore characterize non-sensate reconstructions as a symptomatic treatment that does not address underlying pathology [14, 16], and some even question whether flap reconstruction is appropriate because of the substantial risk of pressure ulcer recurrence. Whereas current research seems to focus on minimizing donor-site morbidity such as through the design of perforator flaps, these flaps will continue to be non-sensate when harvested from non-sensate tissue. It seems unlikely that such flap designs will increase flap durability. In concordance with this notion, a previous meta-analysis did not detect significant differences between musculocutaneous, fasciocutaneous and perforator flaps [23]. As can be seen in Table 1, many of the individuals who received sensate reconstructions had a prior history of multiple recurrences after reconstructions with use of non-sensate, locoregional tissue. After receiving a sensate reconstruction, all of them remained free of pressure ulcer recurrence. This suggests that sensate reconstructions have the potential to disrupt the frequent cycle of recurrence after recurrence in this challenging patient population. The rarity of pressure ulcers among patients with intact sensation can be seen as indirect evidence to support this notion.
A drawback of sensate reconstructions is their increased surgical complexity, such as the need for microsurgery in cases with a high-level SCD. Assessment of the possibility of a sensate reconstruction should therefore include an assessment of the required surgical complexity, compared to its perceived benefits. Yet, when sensate reconstructions are shown to decrease the need for future reconstructions because of recurrence, this will likely also be shown to result in considerable cost benefits, compensating for the costs associated with surgical restoration of sensation.
The strengths of our study include a comprehensive systematic review of the literature, assessment of risk of bias and level of evidence, and meta-analysis of the available data on both non-sensate (1794 flaps) and sensate reconstructions (75 flaps). Still, our review has several limitations. All studies included were retrospective in nature, and most had limited sample sizes and unknown selection bias. Once more, it should be kept in mind that systematic reviews such as this meta-analysis are vulnerable to publication bias, as positive results are more likely to be published [24]. Likewise, it is also difficult to estimate the influence of confounding factors such as appropriate use of preventive medical devices, skeletal protuberances, and patients’ individual psychosocial status. In addition, because of the sparsity of literature on sensate flaps for this indication, our review used different criteria for the accrual of data on sensate compared to non-sensate flaps, potentially introducing selection bias. Another limitation to our study is that we did not include studies published in languages other than English, Dutch, French, and German; journals in other languages may have contained additional studies of interest. In this review, we investigated the outcomes of flaps, which are nested within persons. In some cases, multiple flaps were nested within a person. Because we mainly analyzed the data on a flap level, this may introduce bias.
This review indicates that restoration of sensory innervation may be effective in preventing pressure ulcer recurrence in individuals with SCD. Future studies should therefore not only focus on minimizing donor-site morbidity such as through use of perforator flaps, but should also explore ways to improve flap durability, with surgical restoration of sensory innervation as an example. Ideally, a RCT that includes recruiting consecutive individuals with SCD and a pressure ulcer, appropriate long-term follow-up, and cost-effectiveness analysis should be performed to confirm or refute the results of this systematic review.
Individuals presenting with SCD and a pressure ulcer should receive a physical exam in order to delineate the extent of their sensory innervation. This is important because although low-level SCDs are relatively rare; it may be possible to perform sensate pedicled reconstructions in these patients, avoiding the need for microsurgery. Nerve blocks can be used to delineate the neural territory of specific nerves before transfer [25]. Because of significant variations between patients in the extent of SCD, dermatomes, and sensory nerve neural territories, the design of sensate flaps should be guided by such examinations. Microsurgical restoration of sensory innervation should be considered in persons with high-level injuries who are relatively young and healthy. Multiple reports indicated that even when free flaps are harvested distal to the level of SCD, sensory recovery can be expected. Although reconstructive techniques may continue to evolve, prevention continues to be better than cure as it avoids the need for complex surgeries. Adequate use of pressure ulcer preventive technologies and protocols should therefore continue to be a top priority among clinicians and researchers.
Conclusion
Pressure ulcer recurrence continues to be a significant issue for individuals with SCD who receive locoregional reconstructions with use of non-sensate tissue. Although associated with increased surgical complexity, the literature indicates that restoration of sensory innervation may be very effective at preventing pressure ulcer recurrence. Still, the evidence on sensate reconstructions is of a very low quality level and at considerable risk of publication bias, and whether sensate reconstructions are superior to non-sensate locoregional flaps thus continues to be uncertain.
References
WHO. International Perspectives on Spinal Cord Injury. Geneva, Switzerland: WHO; 2013.
Kruger EA, Pires M, Ngann Y, Sterling M, Rubayi S. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013;36:572–85.
Zwanenburg PR, Backer SFM, Obdeijn MC, Lapid O, Gans SL, Boermeester MA. A Systematic Review and Meta-Analysis of the Pressure-Induced Vasodilation Phenomenon and Its Role in the Pathophysiology of Ulcers. Plast Reconstr Surg. 2019;144:669e–81e.
Chen Y, Devivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86:1208–13.
Cowan LJ, Ahn H, Flores M, Yarrow J, Barks LS, Garvan C, et al. Pressure Ulcer Prevalence by Level of Paralysis in Patients With Spinal Cord Injury in Long-term Care. Adv Ski Wound Care. 2019;32:122–30.
Dinsdale SM. Decubitus ulcers: role of pressure and friction in causation. Arch Phys Med Rehabil. 1974;55:147–52.
Larson JD, Altman AM, Bentz ML, Larson DL. Pressure ulcers and perineal reconstruction. Plast Reconstr Surg. 2014;133:39e–48e.
Relander M, Palmer B. Recurrence of surgically treated pressure sores. Scand J Plast Reconstr Surg Hand Surg. 1988;22:89–92.
Ricci JA, Bayer LR, Orgill DP. Evidence-Based Medicine: the Evaluation and Treatment of Pressure Injuries. Plast Reconstr Surg. 2017;139:275e–86e.
Schryvers OI, Stranc MF, Nance PW. Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil. 2000;81:1556–62.
Tavakoli K, Rutkowski S, Cope C, Hassall M, Barnett R, Richards M, et al. Recurrence rates of ischial sores in para- and tetraplegics treated with hamstring flaps: an 8-year study. Br J Plast Surg. 1999;52:476–9.
Disa JJ, Carlton JM, Goldberg NH. Efficacy of operative cure in pressure sore patients. Plast Reconstr Surg. 1992;89:272–8.
Mehta A, Baker TA, Shoup M, Brownson K, Amde S, Doren E, et al. Biplanar flap reconstruction for pressure ulcers: experience in patients with immobility from chronic spinal cord injuries. Am J Surg. 2012;203:303–6. Discussion 6–7.
Posma AN. The innervated tensor fasciae latae flap in patients with meningomyelocele. Ann Plast Surg. 1988;21:594–6.
Cochran JH Jr, Edstrom LE, Dibbell DG. Usefulness of the innervated tensor fascia lata flap in paraplegic patients. Ann Plast Surg. 1981;7:286–8.
Dibbell DG. Use of a long island flap to bring sensation to the sacral area in young paraplegics. Plast Reconstr Surg. 1974;54:220–3.
Dibbell DG, McCraw JB, Edstrom LE. Providing useful and protective sensibility to the sitting area in patients with meningomyelocele. Plast Reconstr Surg. 1979;64:796–9.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–6.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Schwarzer G metaprop - meta-analysis of single proportions. https://www.rdocumentation.org/packages/meta/versions/4.9-2/topics/metaprop.
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Commun Health. 2013;67:974–8.
Sameem M, Au M, Wood T, Farrokhyar F, Mahoney J. A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg. 2012;130:67e–77e.
Kicinski M, Springate DA, Kontopantelis E. Publication bias in meta-analyses from the Cochrane Database of Systematic Reviews. Stat Med. 2015;34:2781–93.
Santanelli Di Pompeo F, Longo B, Pagnoni M, Laporta R. Sensate anterolateral thigh perforator flap for ischiatic sores reconstruction in meningomyelocele patients. Microsurgery 2014;35:279–83.
Acknowledgements
We want to thank our clinical librarian Faridi van Etten-Jamaludin for her help constructing the search strategy. We want to thank our statisticians Susan van Dieren and Rebecca Holman for their advice on how to approach statistical analysis and present the data.
Funding
Sponsors did not have any influence in the study design, in the collection, analysis and interpretation of data; in the writing of the paper; and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the design of the study and interpretation of data and helped draft the final paper, and revised it critically in equal measure as a group effort. All authors approve the final version to be published and agree to be accountable for all aspects of the work related to its accuracy and integrity. PRZ also formulated the first concept for this paper and its methodology, constructed the search strategy together with a clinical librarian, performed the systematic review, helped with data extraction, risk of bias assessment and OHAT assessment of the body of evidence, and helped with the construction of the tables, created the figures and illustrations, and devised the initial outlines of the paper. RWAV also performed the systematic review as a second reviewer and helped with data extraction and risk of bias and body of evidence assessment and constructed the tables. OL and MCO also provided their clinical perspective as plastic surgeons. Professor MAB also acted as study supervisor.
Corresponding author
Ethics declarations
Conflict of interest
MAB reports institutional grants from J&J/Ethicon, Acelity/KCI, Allergan/LifeCell, Ipsen, Baxter, Mylan, Bard, and is advisory board member of J&J/Ethicon, Acelity/KCI, Bard, and Allergan/LifeCell, for research and expertize outside the submitted work. The authors declare that there are no conflicts of interest related to this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zwanenburg, P.R., Verdijk, R.W.A., Lapid, O. et al. A Systematic review and meta-analysis of sensate versus non-sensate flaps for the prevention of pressure ulcer recurrence among individuals with spinal cord disease. Spinal Cord 59, 463–473 (2021). https://doi.org/10.1038/s41393-020-00590-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00590-5