Abstract
Study design
Longitudinal community survey.
Objectives
To determine subgroups in social participation of individuals living with spinal cord injury (SCI).
Setting
Community.
Methods
Data were collected in 2012 and 2017 as part of the community survey of the Swiss Spinal Cord Injury cohort. Participation was assessed using the 33-item Utrecht Scale of Evaluation of Rehabilitation-Participation evaluating frequency of, restrictions in and satisfaction with productive, leisure, and social activities. Linear mixed-effects model trees were used to distinguish subgroups in participation associated with sociodemographic and lesion characteristics.
Results
In all, 3079 observations were used for the analysis, of which 1549 originated from Survey 2012, 1530 from Survey 2017, and 761 from both surveys. Participants were mostly male (2012: 71.5%; 2017: 71.2%), aged on average 50 years (2012: 52.3; 2017: 56.5), with an incomplete paraplegia (2012: 37.5%; 2017: 41.8%) of traumatic origin (2012: 84.7%; 2017: 79.3%). There was limited within-person variation in participation over the 5-year period. Participation varied with age, SCI severity, education, financial strain, number of self-reported health conditions (SHCs), and disability pension level. Among modifiable parameters, the number of SHCs and disability pension level emerged as the most frequent partitioning variables, while education was most informative for participation in productive, leisure, and social activities.
Conclusions
Long-term rehabilitation management and clinical practice should target people most prone to decreased participation in major life domains. Our study indicates that the alleviation of SHCs, engagement in further education, or adjusting disability pension level are promising areas to improve participation of persons living with SCI.
Similar content being viewed by others
Introduction
Fulfilling participation in major life domains such as social and cultural activities and work is a key indicator of successful rehabilitation [1, 2], and its positive impact on health and well-being has been repeatedly shown for different populations including persons living with spinal cord injury (SCI) [3, 4]. Yet, variation in participation of persons with SCI is still poorly understood. Most of the evidence is cross-sectional in nature [1], while rehabilitation management is dependent on prognostic or causal information, which can only be reliably inferred from longitudinal data. This was demonstrated in a study that analyzed both cross-sectional and longitudinal effects of age and time since injury on, e.g., social integration [5]. Specifically, social integration showed a negative association with age group between individuals, while a positive association with age was found within individuals.
Existing longitudinal studies in SCI showed a mixed pattern of favorable and unfavorable changes in social participation over the life-span [5,6,7,8,9,10,11]. While daily activities inside and outside the home, such as personal care, doing housework, or going out, and mobility tended to decrease over time [6, 8, 9], there is conflicting evidence as to the frequency of and satisfaction with social participation and integration, and employment [5,6,7,8, 10]. These conflicting results may be attributed to different participation measurement instruments or analysis techniques. Moreover, it is often unclear to what extent the population under study was representative of the respective SCI community [6, 7, 11].
Sociodemographic (e.g., age, gender, financial restrictions, or education) and SCI characteristics (e.g., SCI severity), as well as medical and environmental factors (e.g., social support), have been repeatedly reported in relation to participation outcomes [1, 5, 6, 10, 11]. However, hardly any of these prospective studies looked at the interactive effects of multiple participant characteristics on social participation while accounting for between- and within-person differences. For example, only one study tested participant characteristics (e.g., age at injury, AIS categories, income, and domestic situation (i.e., living alone)) in interaction with time since SCI on the outcomes subjective community integration and autonomy in participation [11], and results of only two studies [5, 11] were accounted for within-person (longitudinal effects) and between-person variation (cross-sectional effects). Thus, there is insufficient evidence for the identification of persons in most urgent need of participation-oriented interventions in counseling, long-term follow-up, and individual goal setting in rehabilitation.
The present study makes use of longitudinal, population-based survey data to identify subgroups in major life domains of participation among community-dwelling individuals with SCI in Switzerland. Specifically, we explored determinants of within- and between-person variation in (1) overall participation frequency, experienced restrictions in participation due to a person’s health condition and satisfaction with participation; and (2) within the frequency domain of participation we further explored determinants of productive, leisure, and social activities.
Methods
Study design
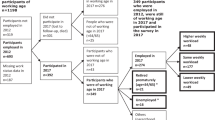
We used data from the first and second Swiss Spinal Cord Injury (SwiSCI) community survey (subsequently referred to as Survey 2012 and Survey 2017). The design, recruitment, and eligibility criteria of Survey 2012 and 2017 are detailed elsewhere [12, 13]. In brief, Survey 2012 was conducted between 9/2011 and 3/2013 and Survey 2017 between 3/2017 and 3/2018. Participants were recruited through all four Swiss specialized SCI rehabilitation centers, the Swiss Paraplegic Association and ParaHelp, the specialized home care institution for individuals with SCI in Switzerland. In Survey 2012, the sampling frame covered ~50% of the total Swiss adult SCI population and 49.3% of this sample responded to the survey [12], and in Survey 2017 the sampling frame covered ~65% of the total Swiss adult SCI population and 38.6% of this sample responded to the survey [13]. The questionnaires of Survey 2012 and 2017 included items on body functions and structures, activities and participation, environmental and personal factors, lesion characteristics as well as participants’ appraisal of health and well-being and are available online.Footnote 1
Ethical approval was sought for Survey 2012 and 2017, and all participants gave their informed consent.
Participants
Inclusion and exclusion criteria were per study protocol. SwiSCI included Swiss residents 16 or older years who had a chronic traumatic or nontraumatic SCI. Excluded were persons with SCI due to congenital conditions, neurodegenerative disorders, or Guillain–Barré syndrome [12, 13].
Measures
Participation was measured with the Utrecht Scale of Evaluation of Rehabilitation-Participation (USER-Participation) that comprises 32 items in three scales: frequency, restrictions, and satisfaction [14]. The frequency scale (11 items) assesses the hours or occasions spent on productive, leisure, and social activities and ranges from none at all/never to 36 h or more/19 times or more. The restrictions scale (11 items) assesses experienced restrictions on vocational, mobility, leisure, and social activities due to one’s health condition and item scores range from 0 (not possible at all) to 3 (no difficulty at all). The satisfaction scale (ten items) measures satisfaction with vocational, mobility, leisure, and social activities; item scores range from 0 (not satisfied at all) to 5 (very satisfied). To assure linear metric properties for use in regression tree analysis, Rasch transformed scores were used for the restrictions and satisfaction scales of Survey 2012 and 2017. The scores range from 0 to 100 with higher scores representing better participation (higher frequency, less restrictions, and higher satisfaction). A Rasch analysis of the frequency scale is not warranted [15]. As different productive activities, such as pursuing paid work, doing housework, and volunteering work, cannot be performed simultaneously, this renders the scaling of associated frequencies into a single dimension conceptually meaningless. The frequency scale is further divided into three subscales summing the items of the productive, leisure, and social activities, which are converted to a 0–100 scale [16]. Currently, there is no consensus regarding clinically important cut-off scores that can guide policy and interventions with the goal of improving participation across the life domains. With a pragmatic distribution-based criterion of 0.5 standard deviation in the respective USER-Participation scales, we consider a 9–10 points difference in participation scale scores as clinically important. The USER-Participation’s validity, test-retest reliability, and responsiveness in rehabilitation settings were satisfactory [14, 17, 18]. Supplementary File 1 contains all questions of the USER-Participation.
Based on theoretical assumptions and literature [1], a set of modifiable and non-modifiable determinants was included into the models. Non-modifiable determinants were gender, age in years, injury severity (incomplete paraplegia; complete paraplegia; incomplete tetraplegia; complete tetraplegia), years since injury, and SCI etiology (traumatic/nontraumatic). Injury severity was either derived from patient records (if available) or based on self-report. If derived from patient records, AIS A was defined as complete lesion vs. AIS B C D as incomplete. Modifiable determinants were marital status (yes/no married/in partnership), financial strain (yes/no), years of education, and number of self-reported health conditions (SHCs) self-rated as chronic or significant. For the number of SHCs, 14 items of the SCI secondary conditions scale [19] and one item reflecting sleep problems were selected and dichotomized (0 = no, mild/infrequent or moderate/occasional problem; 1 = chronic/significant problem; a sum score reflecting the number of SHCs of chronic/significant level was computed). Supplementary File 1 contains all questions of the SCI secondary conditions scale. Financial strain was assessed by the question “Did you experience financial difficulties that restricted your everyday life (participation) over the past four weeks?” A dichotomous variable was created out of the four response categories (no = not applicable, no influence, vs. yes = made my life a little harder, made my life a lot harder). The participants’ disability pension level (i.e., full pension, 3/4 pension, 1/2 pension, 1/4 pension, no pension) was added as a policy level determinant.
Data analysis
To identify groups at risk of low social participation, linear mixed-effects model (LMM) trees were calculated for the frequency, restrictions, and satisfaction scales and the frequency subscales of the USER-Participation [20]. A key feature of the LMM tree algorithm is that it facilitates the detection of subgroups that may be conditional on observations within a hierarchical, nested (i.e., repeated observations nested within individuals) data structure. This hierarchical structuring may inform social and health policy by accentuating possible intervention strategies that are expected to have the greatest leverage in improving participation in specific subgroups. We refrained from traditional mixed effect models because these models assume a common parametric form for the population mean structure that may not be appropriate within the heterogeneous SCI population, i.e., the assumption of a common parametric form will obscure meaningful subgroup differences and hence may lead to erroneous inferences [21]. Moreover, by partitioning the data set with respect to a number of determinants, better-fitting models in each final subgroup (also called terminal nodes) can be employed. The LMM tree algorithm was described in detail by Fokkema et al. [20], and a thorough description and evaluation of the algorithm can be found in Supplementary File 2. In brief, LMM trees use both model-based recursive partitioning and traditional linear mixed models to “grow” a tree of which each detected subgroup in the terminal node is associated with separate locally fixed-effect regression coefficients of the resulting partitioning, while keeping the random effects, which are derived through a mixed-effects model, constant throughout the tree [20, 22]. Survey year was the determinant for the locally node-specific fixed-effect model and person ID was specified as determinant of the global random effect, thus deriving random intercepts across persons. Finally, the set of potential partitioning variables (i.e., the determinants) for growing the tree was used to assess within- and between-person variation in evaluating the tree and generating subgroups. The size of the LMM trees is determined by the model instability significance test during partitioning. To avoid overfitting, we additionally set the maximum depth of the tree to five nodes with a reasonable minimal size of n = 250 for any inner (i.e., where the branches of the tree split into “inner or child nodes”) or terminal node (i.e., the final identified subgroups in the tree). The result of the partitioning can be presented as a regression tree with locally fixed effects models in each of the terminal nodes. Inner nodes indicating partitioning of the data set and corresponding p values from the model instability tests (Bonferroni corrected and with the significance level set to alpha = 0.05) are graphically displayed in the resulting trees. For terminal nodes a boxplot of the observed values is provided as well as mean-centered fitted values. Finally, corresponding intraclass correlations (ICC) are reported. ICC is a measure of the proportion of the total variance in the outcome variables that is accounted for by between-person variation. List-wise deletion was applied for cases with missing data in a determinant. All analyses were performed with Stata 14.2 (StataCorp) and the glmertree package (version 0.2–2) in R Studio (R Core Team 2020) [23].
Results
In total, 3079 observations (n = 1549 for Survey 2012; n = 1530 for Survey 2017 of which n = 761 of people who participated in both surveys) were used in the analysis. Table 1 details the sample characteristics. The majority of the participants were male, with incomplete paraplegia of traumatic origin. Participants were on average in their 50s, had 14 years of education, and had been living for over 15 years with SCI. The number of SHCs of a chronic or severe nature was on average two. The distribution of the values of the USER-P scales and of the frequency subscales was similar across surveys.
Determinants of within- and between-person variations in participation
Figure 1 shows the LMM tree for USER-Participation frequency scale. Between survey years, frequency scores showed small within-person variation (the fixed effects of survey year ranged from −1.7 to 1.9 points, Table 2). For the frequency of participation, the algorithm identified seven subgroups. Age, pension level, education, and number of SHCs best explained between-person variation in frequency of participation. A 12.0 points difference was found between the subgroups with the lowest and highest scores on the USER-Participation frequency scale (Table 2). The lowest frequency scores (node 13, estimated score: 29.0) were reported by persons aged 65 years or more and those with a full disability pension (node 12, estimated score: 30.3; node 11, estimated score 32.7). The highest scores were found for persons aged 41 years or less and with more than 14 years of education and without a full disability pension (node 8, estimated score: 41.0). The corresponding ICC indicates that 51.9% of variance in USER-Participation frequency scores was explained by between-person differences.
Between survey years, estimates of perceived restrictions ranged from −1.4 to 4.2 points (Fig. 2). Between-person variation in perceived participation restrictions was associated with number of SHCs, injury severity, financial strain, and age, resulting in six subgroups. The most extensive restrictions were perceived by persons with more than 1 SHCs and tetraplegia (node 11, estimated score: 57.4, Table 2). That subgroup had a 17.6 points difference compared with persons with less or equal than 1 SHC and with an incomplete lesion, i.e., those who reported the fewest restrictions (node 3, estimated score: 75.0). Between-person differences explained 69.1% (ICC) of the variation in the USER-Participation restriction scores.
Within-person variation was small with estimates of satisfaction scores ranging from −0.6 to 3.9 points between survey years (Fig. 1 of Supplementary File 3). Number of SHCs, financial strain, injury severity, and disability pension level explained between-person variation in satisfaction with participation best. Persons with more than two SHCs and with financial strain reported the lowest satisfaction (node 11, estimated score: 45.3, Table 2) and had a 16.2 and 13.6 points difference compared with persons without SHCs and with incomplete paraplegia, i.e., the subgroup with the highest satisfaction scores (node 4, estimated score: 61.5) and those with complete paraplegia and incomplete or complete tetraplegia (node 5, estimated score: 58.9). Between-person differences explained 51.4% (ICC) of the variation in the USER-Participation satisfaction scores.
Between survey years, within-person variation was minimal with estimates of productive activities ranging from −0.4 to 1.7 points (Table 2). Lower scores for productive activities were found in individuals aged 65 or older (node 9, estimated score: 14.1) and among younger individuals with a full disability pension (node 8, estimated score: 17.7). These subgroups had a 12.9 and 16.5 points difference compared with persons with the highest productive activities scores, namely, those aged 64 or younger, with at most two SHCs and with the lowest (none, 1/4) disability pension levels (node 5, estimated score: 30.6, Fig. 2 of Supplementary File 3). Between-person differences explained 42.8% (ICC) of the variation in the productive activities scores.
Estimates of leisure activities ranged from −0.2 to −7.1 points between survey years (Fig. 3 of Supplementary File 3 and Table 2). Between-person variation in reported frequency of leisure activities was associated with education and financial strain. Persons with <11 years of education had 5.1 points less on the frequency of leisure activities subscale (node 2, estimated score: 37.9) compared with persons with more than 13 years of education and no financial strain had higher participation in leisure activities (node 6, estimated score: 47.9, node 6). Between-person differences explained 45.2% (ICC) of variation in the leisure activities scores.
Finally, estimates of social activities ranged from −3.5 to 1.8 points between survey years, and between-person variation on that subscale was associated with education and age (Fig. 4 of Supplementary File 3). Persons with <12 years of education and aged 54 years or older had the lowest participation in social activities (node 5, estimated score: 43.3, Table 2) with a 13.3 points difference compared with persons with more than 13 years of education and aged 40 years or younger, i.e., those with the highest participation in social activities (node 8, estimated score: 56.5). Between-person differences explained 53.2% of variation in the social activities scores.
Discussion
This study identified subgroups of individuals who have low social participation. Participation showed limited within-person variation over a period of 5 years. A minor improvement was documented for perceived restrictions, whereas the frequency of leisure activities tended to decrease. Across participation domains, participation systematically varied with age, SCI severity, number of SHCs, education, financial strain, and disability pension level. Among modifiable parameters, the number of SHCs and the level of disability pension emerged as the most important modifiable partitioning variables, while education was most predictive for participation in productive, leisure, and social activities.
Participation frequency, restrictions, and satisfaction seemed a rather stable phenomenon with only slight within-person changes over 5 years. Scores of the frequency main scale and its subscales are comparable with other SCI populations [16]. The limited within-person variation is in line with previous longitudinal studies on participation in major life domains, for which most decrease was reported for the frequency of leisure activities [9], while satisfaction with social integration remained stable over time [10, 11]. In our sample, frequency of leisure activities also had the most pronounced decrease across subgroups. An underlying age effect as previously reported may be responsible for the decrease in the frequency of leisure activities [9]. In the general population, leisure activities have been linked to psychological and physical well-being as well as to increased survival [24]. Thus, in rehabilitation management and counseling the focus should not only be on living and vocational rehabilitation, but also on recreative leisure activities and unpaid productive activities.
The number of SHCs had an effect in most domains of participation, mostly conditioned on other characteristics, such as education, disability pension status or injury severity, and most pronounced for perceived restrictions (maximally 17 points difference between those with more than 1 SHC vs. less or equal than 1 SHC). The number of SHCs after SCI has been reported to be high, with an impact on life satisfaction, well-being and life expectancy [25]. This is also confirmed by a recent analysis of the Swiss SCI population with chronic pain, bladder and bowel dysfunction, contractures, spasticity, and urinary tract infections as rated most often as significant or chronic [26]. Because participation in community and social life is closely linked to health and well-being; optimizing the management of SHCs in people with SCI is very likely beneficial for social participation and well-being. The question on how to tackle SHCs in different settings, including the community, remains challenging. SwiSCI evidence showed that a proportion of persons were not treated for their SHCs rated as significant or chronic [26], and the success of reducing SHCs is still being researched. A scoping review showed ambiguous effects of health promotion interventions on community participation that contained physical activity and reduction and prevention of SHCs in a disability population [27].
The identification of non-modifiable factors, such as age and injury severity, has potential for guiding intervention by pointing to specific target groups that may respond to an intervention that is specifically tailored to their needs. For instance, to alleviate participation restrictions target groups may consist of persons with tetraplegia with more than one SHC or persons with paraplegia and higher age and with concurrent SHCs. Besides the management of SHCs in these groups, elderly persons with paraplegia may particularly benefit from programs aiming at fostering social networks and self-managing skills and an active engagement in social activities [28], while in persons with tetraplegia, besides the management of SHC, focus should be on the built environment, targeting accessibility and transportation as demonstrated in a recent analysis [29].
Policy interventions may also seek to adjust socioeconomic characteristics, and our study suggests the level of disability pension, financial strain, and education as potential targets to improve participation. It is not surprising that the combination of age and level of disability pension was mainly associated with frequency of productive activities, among which paid work is a key outcome. In Switzerland, the eligibility for and the level of disability pension are based on a work capacity assessment following initial rehabilitation. At this time point, restrictions in the ability to perform paid work may be a determinant of disability pension level. Later, in the community setting, it is more likely that the disability pension levels determine the frequency of paid work [30]. Thus, adjusting disability pension levels may appear a promising policy strategy to enhance participation in paid work for persons with SCI. Moreover, financial strain is a key indicator of profligate living and may worsen the burden of everyday life by restricting access to relevant resources and generating feelings of deprivation [31]. The present study suggests that the interaction of adverse socioeconomic and health-related characteristics such as financial strain, low education, and concomitant SHCs reinforces the negative impact of these determinants on people’s participation. The current findings call for an interdisciplinary approach to best tailor intervention strategies for persons with a multitude of adverse socioeconomic and health-related circumstances.
Strengths and limitations
The novel tree algorithm approach allowed for the detection of both within- and between-subject variation while taking into account higher-order interactions of the determinants of participation. Therefore, it is optimally suited for the identification of different groups with similarly low participation scores. Our findings indicate the importance of promoting tailored rehabilitation and counseling interventions that aim to enhance participation by considering the needs and limitations of particular groups. More advantages and a comparison to traditional statistical procedures (e.g., regression analysis) can be found in Supplementary File 2. Some limitations of tree-based analysis need mentioning. Instability is a known phenomenon in tree-based models, caused by small changes in the data set and usually associated with the heterogeneity of the study sample [20]. Small differences in the initial data can result in selection of a different set of variables for the hierarchical nodes that may produce a rather different tree. This is relevant insofar as it adds uncertainty to inferences and conclusions that are meant to inform policy to improve participation in the SCI community. The LMM tree algorithm is a newly developed algorithm in the abundance of tree building algorithms. Research on further real data is needed to analyze its prediction accuracy and stability. Moreover, trees are usually employed for exploratory purposes rather than used in hypothesis-driven research, and due to the various interaction effects in the trees a single-factor effect may not be assessed, which is useful for meta-analysis [32].
Given that there is still no registry of the entire adult Swiss SCI population, it is difficult to derive conclusions about the representativeness of the study population in relation to the entire adult Swiss SCI population. It is estimated that ~6000 adult persons (of roughly 6.7 million inhabitants of Switzerland) lived with an SCI in 2012 [12]. No more recent prevalence estimates are available. Taking into account all eligible persons on the sampling frame for the Survey 2012 (n = 3144) and 2017 (n = 3959), ~50 and 65% coverage rates can be estimated for response to USER-Participation in Survey 2012 and 2017, representing at least 25% of the Swiss SCI population [13]. Thus, generalizability of our findings is limited.
Conclusion
This study profiled the within- and between-person variation in participation in major life domains of the Swiss SCI population. Over a 5-year period, change in participation was marginal. Different participation profiles were identified with respect to medical and social dimensions. Our study suggests that improvements in participation frequency, restrictions, and satisfaction may be achieved by either personalized or group interventions that target modifiable factors, such as SHCs, disability pension level, financial strain, and education.
Data availability
Owing to our commitment to SwiSCI study participants and their privacy, data sets generated during the current study are not made publicly available but can be provided by the SwiSCI Study Center based on reasonable request (contact@swisci.ch)
Notes
The Community Survey: https://swisci.ch/en/research-projects-home/study-design/community-survey.
References
Barclay L, McDonald R, Lentin P. Social and community participation following spinal cord injury: a critical review. Int J Rehabil Res. 2015;38:1–19.
Kennedy P, Lude P, Taylor N. Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord. 2006;44:95–105.
van Leeuwen CM, Post MW, Westers P, van der Woude LH, de Groot S, Sluis T, et al. Relationships between activities, participation, personal factors, mental health, and life satisfaction in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93:82–9.
Hornby-Turner YC, Peel NM, Hubbard RE. Health assets in older age: a systematic review. BMJ Open. 2017;7:e013226.
Weitzenkamp DA, Jones RH, Whiteneck GG, Young DA. Ageing with spinal cord injury: cross-sectional and longitudinal effects. Spinal Cord. 2001;39:301–9.
Savic G, Frankel HL, Jamous MA, Soni BM, Charlifue S. Participation restriction and assistance needs in people with spinal cord injuries of more than 40 year duration. Spinal Cord Ser Cases. 2018;4:28.
Krause JS, Bozard JL. Natural course of life changes after spinal cord injury: a 35-year longitudinal study. Spinal Cord. 2012;50:227–31.
Charlifue S, Gerhart K. Community integration in spinal cord injury of long duration. NeuroRehabilitation. 2004;19:91–101.
Bushnik T. Access to equipment, participation, and quality of life in aging individuals with high tetraplegia (C1-C4). Top Spinal Cord Inj Rehabil. 2002;7:17–27.
Johnston M, Nissim EN, Wood K, Hwang K, Tulsky D. Objective and subjective handicap following spinal cord injury: interrelationships and predictors. J Spinal Cord Med. 2002;25:11–22.
Pershouse KJ, Barker RN, Kendall MB, Buettner PG, Kuipers P, Schuurs SB, et al. Investigating changes in quality of life and function along the lifespan for people with spinal cord injury. Arch Phys Med Rehabil. 2012;93:413–9.
Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A, SwiSCI Study Group. Swiss national community survey on functioning after spinal cord injury: protocol, characteristics of participants and determinants of non-response. J Rehabil Med. 2016;48:120–30.
Gross-Hemmi MH, Gemperli A, Fekete C, Brach M, Schwegler U, Stucki G. Methodology and study population of the second Swiss national community survey of functioning after spinal cord injury. Spinal Cord. 2020; https://doi.org/10.1038/s41393-020-00584-3.
Post MW, van der Zee CH, Hennink J, Schafrat CG, Visser-Meily JM, van Berlekom SB. Validity of the utrecht scale for evaluation of rehabilitation-participation. Disabil Rehabil. 2012;34:478–85.
Mader L, Post MW, Ballert CS, Michel G, Stucki G, Brinkhof MW. Metric properties of the utrecht scale for evaluation of rehabilitation-participation (USER-Participation) in persons with spinal cord injury living in Switzerland. J Rehabil Med. 2016;48:165–74.
de Ruijter LS, de Groot S, Adriaansen JJ, Smit CA, Post MWM. Associations between time since onset of injury and participation in Dutch people with long-term spinal cord injury. Spinal Cord. 2018;56:1134–43.
van der Zee CH, Priesterbach AR, van der Dussen L, Kap A, Schepers VP, Visser-Meily JM, et al. Reproducibility of three self-report participation measures: the ICF measure of participation and activities screener, the participation scale, and the utrecht scale for evaluation of rehabilitation-participation. J Rehabil Med. 2010;42:752–7.
van der Zee CH, Post MW, Brinkhof MW, Wagenaar RC. Comparison of the utrecht scale for evaluation of rehabilitation-participation with the ICF measure of participation and activities screener and the WHO Disability Assessment Schedule II in persons with spinal cord injury. Arch Phys Med Rehabil. 2014;95:87–93.
Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL. Preliminary reliability and validity of a spinal cord injury secondary conditions scale. J Spinal Cord Med. 2007;30:131–9.
Fokkema M, Smits N, Zeileis A, Hothorn T, Kelderman H. Detecting treatment-subgroup interactions in clustered data with generalized linear mixed-effects model trees. Behav Res Methods. 2018;50:2016–34.
Kundu MG, Harezlak J. Regression trees for longitudinal data with baseline covariates. Biostat Epidemiol. 2019;3:1–22.
Zeileis A, Hothorn T, Hornik K. Model-based recursive partitioning. J Comput Graph Stat. 2008;17:492–514.
R Core Team. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2020. https://www.R-project.org/.
Konlaan BB, Bygren LO, Johansson SE. Visiting the cinema, concerts, museums or art exhibitions as determinant of survival: a Swedish fourteen-year cohort follow-up. Scand J Public Health. 2000;28:174–8.
Rivers CS, Fallah N, Noonan VK, Whitehurst DG, Schwartz CE, Finkelstein JA, et al. Health conditions: effect on function, health-related quality of life, and life satisfaction after traumatic spinal cord injury. A prospective observational registry cohort study. Arch Phys Med Rehabil. 2018;99:443–51.
Buzzell A, Camargos KC, Chamberlain JD, Eriks-Hoogland I, Hug K, Jordan X et al. Receiving or not receiving treatment for secondary health conditions within the spinal cord injured community: results from a descriptive analysis using survey data. Spinal Cord (submitted).
White GW, Gonda C, Peterson JJ, Drum CE. Secondary analysis of a scoping review of health promotion interventions for persons with disabilities: do health promotion interventions for people with mobility impairments address secondary condition reduction and increased community participation? Disabil Health J. 2011;4:129–39.
van Hees SGM, van den Borne BHP, Menting J, Sattoe JNT. Patterns of social participation among older adults with disabilities and the relationship with well-being: a latent class analysis. Arch Gerontol Geriatr. 2020;86:103933.
Reinhardt JD, Fellinghauer CS, Post MWM. Change in environmental barriers experienced by people living with spinal cord injury in Switzerland over a five-year period: a prospective cohort study. Spinal Cord. 2020; https://doi.org/10.1038/s41393-020-00580-7.
Schwegler U, Fekete C, Finger M, Karcz K, Staubli S, Brinkhof MWG. Labor market participation of individuals with spinal cord injury living in Switzerland: determinants of between-person differences and counterfactual evaluation of their instrumental value for policy intervention outcomes. Spinal Cord (submitted).
Fekete C, Siegrist J, Reinhardt JD, Brinkhof MW. Is financial hardship associated with reduced health in disability? The case of spinal cord injury in Switzerland. PloS ONE . 2014;9:e90130.
Venkatasubramaniam A, Wolfson J, Mitchell N, Barnes T, JaKa M, French S. Decision trees in epidemiological research. Emerg Themes Epidemiol. 2017;14:11.
Acknowledgements
We thank the SwiSCI Steering Committee with its members Xavier Jordan and Fabienne Reynard (Clinique Romande de Réadaptation, Sion); Michael Baumberger and Hans Peter Gmünder (Swiss Paraplegic Center, Nottwil); Armin Curt and Martin Schubert (University Clinic Balgrist, Zürich); Margret Hund-Georgiadis and Kerstin Hug (REHAB Basel, Basel); Laurent Prince (Swiss Paraplegic Association, Nottwil); Heidi Hanselmann (Swiss Paraplegic Foundation, Nottwil); Daniel Joggi (Representative of persons with SCI); Nadja Münzel (Parahelp, Nottwil); Mirjam Brach and Gerold Stucki (Swiss Paraplegic Research, Nottwil); Armin Gemperli (SwiSCI Coordination Group at Swiss Paraplegic Research, Nottwil).
Funding
SwiSCI is hosted and funded by Swiss Paraplegic Research.
Author information
Authors and Affiliations
Contributions
MHGH, MWGB, and CF were responsible for designing and planning of the present study. MHGH was responsible for data analysis, interpretation, and development of the present paper. ASS, US, and MWMP contributed to the study proposal, to interpretation and discussion of results, and approved the final paper. All authors participated in a critical revision of this paper for important intellectual content and ultimately approved of the final version based on this submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval for Survey 2012 was approved by the principal ethics committee on research involving humans of the Canton of Lucerne (KEK Luzern, internal application 11042, approved June 28, 2011) and subsequently endorsed by the additional involved cantonal ethics committees of Cantons Basel-Stadt (EK Basel, internal application 306/11, approved September 6, 2011) and Valais (CCVEM Sion, internal application CCVEM042/11, approved December 6, 2011). Ethical approval for Survey 2017 was granted by the leading ethical institution Ethikkommision Nordwest-und Zentralschweiz (EKNZ, Project-ID: 11042 PB_2016-02608, approved December 2016). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gross-Hemmi, M.H., Fekete, C., Post, M.W.M. et al. Detecting subgroups in social participation among individuals living with spinal cord injury: a longitudinal analysis of community survey data. Spinal Cord 59, 419–428 (2021). https://doi.org/10.1038/s41393-020-00576-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00576-3
This article is cited by
-
Bladder and bowel function effects on emotional functioning in youth with spinal cord injury: a serial multiple mediator analysis
Spinal Cord (2023)
-
Self-care in spinal cord injuries inventory (SC-SCII) and self-care self-efficacy scale in spinal cord injuries (SCSES-SCI): development and psychometric properties
Spinal Cord (2021)