Abstract
Study design
Retrospective study
Objectives
To describe the epidemiological and clinical profile in a retrospective chart review of individuals with spinal cord injury (SCI) and osteoporosis-related fractures.
Setting
A Brazilian rehabilitation hospital.
Methods
This is a retrospective chart review that included 325 individuals with SCI and osteoporosis-related fractures who were admitted to a Brazilian rehabilitation hospital between January 1997 and December 2017.
Results
Overall, 52% were males with a mean (SD) age of 44.8 (±16.7) years at the time of first fracture. Overall, 82% had paraplegia and 56% had a thoracic neurological level. The mean (SD) time between SCI and fracture was 9.7 (±9.3) years. In 59% of cases the immediate cause of the fracture was a fall. The locations of the fractures were distal femur (27%), proximal femur (27%), and tibia and/or distal fibula (28%). The fractures occurred mostly at home (63%). Complications occurred in 19% of individuals and 25% reported worse performance in activities of daily living and 29% a deterioration in ambulation after they had recovered from the fracture. A second fracture was described in 15% of individuals, and five individuals had a third fracture. The mean (SD) level of 25 hydroxyvitamin D [25 (OH) D] was 25.6 (±15.2) ng/ml, and only 11 individuals (3%) underwent dual energy X-ray absorptiometry (DEXA), and 26 individuals (8%) were treated with antiresorptive drugs after fracture.
Conclusion
Little is done to prevent fractures in individuals with SCI and understanding the clinical and epidemiological profiles will help identify risk factors and establish prevention programs and appropriate treatment.
Similar content being viewed by others
Introduction
Osteoporosis affects the health of individuals with SCI because it increases the risk of fractures with consequences, such as skills, ulcers, immobility, depression, and mortality [1,2,3,4,5,6,7].
Bone demineralization after SCI occurs in 4% of bone loss per month in the first year [8,9,10], primarily in the knees. Demineralization begins in the early days, peaks around the 10th–16th week and stabilizes around the 16th–24th month [8, 9]. Recent studies suggest that the bone loss extends 3–8 years after SCI [10]. Previous studies demonstrated bone demineralization >20% in the hip, 37–52% in the distal femur and 36–70% in proximal tibia after 1–3 years after SCI [10,11,12,13].
Bone loss associated with spinal cord injury is related to immobility and metabolic changes [14, 15]. Individuals with SCI exhibit hypercalcemia, hypercalciuria, hyperparathyroidism, and decreased levels of osteocalcin. The loss of bone mineral density is 2–4 times greater than the loss that occurs in an immobilized individual without SCI [15]. Other related factors may contribute to this bone loss, such as vitamin D deficiency and the use of methylprednisolone, anticonvulsant drugs, and psychotropic substances [4].
The consequence of osteoporosis in individuals with SCI is fracture due to bone fragility. Fractures may occur in 25–46% of these individuals over their lifetimes [4,5,6,7, 16, 17]. Fractures are primarily related to torsional forces during transfer, passive mobilization, compressive forces and falls [4,5,6,7,8, 17]. Individuals with tetraplegia have more osteoporosis than those with paraplegia, however individuals with paraplegia have a higher frequency of fractures due to exposure to falls [4,5,6,7, 16, 17].
The following risk factors have been described in previous studies as associated with increased fracture: ASIA Impairment Scale (AIS) or B; age 40+ years old; SCI longer than three years; age at SCI of 16 years or less; three servings of coffee per day; smoking; woman; family history of osteoporotic fractures; low bone mineral density; low weight bone mass index < 19 kg/cm2; alcohol intake >30 g/day; paraplegia, and the use of corticosteroids [4,5,6,7]. Craven et al. [4] developed protocols conducive to treatment based on these risk factors.
Bone densitometry scan (DEXA) in individuals with SCI is a confirmatory test to predict the future risk of fracture. The use of T-scores proposed by the World Health Organization (WHO) or the Fracture Risk Assessment Tool (FRAX) for individuals with SCI is debatable [9]. Some studies suggested that a low score of FRAX and DEXA of the hip predicted fracture in individuals with SCI [18], and some authors suggest DEXA measurement of the distal femur and proximal tibia, with specific protocols for the evaluation of these sites [19].
The aims of this study are:
- To describe the epidemiological and clinical profiles from a retrospective chart review of individuals with SCI and osteoporosis-related fractures in our population.
- To compare the type of locomotion (wheelchair or ambulation) with the fracture site and to compare the age of the first fracture with gender.
Methods
The present study is a retrospective chart review of individuals with SCI from the Rehabilitation Program at the Belo Horizonte Unit of the Sarah Network of Rehabilitation Hospitals from Association of Social Pioneers.
Individuals were admitted from January 1997 to December 2017 and every individual had at least one osteoporosis-related fracture during the period of investigation.
Data were obtained from electronic records containing information about all consultations and examinations with the participants. Fractures were defined using International Statistical Classification of Diseases, ninth revision codes (ICD-9).
The time (in years) between SCI and the osteoporosis-related fracture was extracted. In addition, data as per the International Spinal Cord Injury Fracture History Extended Data Set [20] were extracted. This included: fracture location in one of the five groups (proximal femur, distal femur, distal tibia and/or fibula, foot, and others); and fracture etiology (unknown, turning over in bed/transfer, fall from wheelchair or standing height, self-passive mobilization, dropped object on body, stretching/physical therapy activities, findings on x-ray, caught foot on object while wheeling, weight-bearing or assisted ambulation activities, and others). We considered transfer as the cause of fractured if the fracture occurred during the transfer per se and classified the cause of fracture as a fall if the fracture occurred after the transfer.
Some fractures were excluded: fall from greater than standing height, sports injuries, and motor vehicle/motorcycle accidents. We considered only surgery (yes or no) for fracture treatment. We excluded patients with diagnosis of congenital spinal disease as bifid spine and genetic diseases as progressive paraparesis.
The following fracture complications were also extracted: none, skin ulcer, infection, amputation, fracture nonunion/delayed union, deep venous thrombosis, loss of range of motion. We entered 40 for the WHO FRAX age if the participant was younger than 40 years old, and “yes” for secondary osteoporosis was entered for all individuals with SCI. Results are expressed as percentages in the 10-year probability of major osteoporotic fracture.
We used the American Spinal Injury AIS from the American Spinal Injury Association (ASIA) [21] for level classification.
The following factors were used as independent variables: (1) socioepidemiological characteristics including sex, age, and schooling (in years) (2) lifestyle, including drugs, alcohol intake of three or more units/day and tobacco consumption; (3) clinical data, such as weight, height, family history of fracture, and comorbidities (diabetes mellitus, hypertension, hypothyroidism, rheumatoid arthritis); (4) physical signs as Ashworth Scale [22] for the wrist extensors, triceps, knee extensors and ankle extensors was used to evaluate spasticity of lower and upper limbs, the use of some type of support for locomotion, the level of the neurological lesion (cervical, thoracic or lumbosacral), range of motion measurement after fracture was performed using a goniometer; (5) medications; and (6) laboratory findings including vitamin D, calcium, phosphorus, magnesium, parathyroid hormone, and alkaline phosphatase levels and (7) DEXA result for total femur/femoral neck bone measurement density (g/cm2).
Socioepidemiological, lifestyle, and clinical data refer to the time of SCI. Physical signs, medication, laboratory data and DEXA refer to the time of the fracture.
Individuals age was considered at the age of SCI and the occurrence of fracture. We divided the participants as ambulatory (at least daily training or walking with an orthosis and walker or sticks) or wheelchair-bound (no walking training at all).
Statistical analysis
Data from the electronic health records were entered into a Microsoft Excel 2010 spreadsheet and analyzed using the IBM SPSS Statistics for Windows, Version 21.0. An exploratory analysis of the data was performed to ascertain the characteristics of the study population and the prevalence of the variables described. The presence of associations was considered at the 0.05 significance level. Pearson’s correlation coefficient, Student’s t test and Yate´s Chi-square test (χ2) were used to test for associations between groups in univariate analyses.
Results
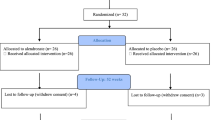
We conducted a retrospective study comprising individuals selected from a cohort of patients with traumatic and nontraumatic SCI with fractures related to SCI (n = 1535). A total of 325 participants with SCI and 378 osteoporosis-related fractures were selected for analyses after the application of inclusion and exclusion criteria (excluded n = 1210). Characteristics of the participants are described in Table 1.
Ambulatory individuals (49%) and wheelchair-bound (51%) individuals exhibited similar frequencies. The time to the first fracture was varying from a few months (minima 3 months) to many years (maxima 66 years) after SCI.
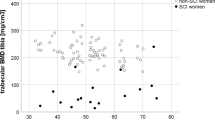
The most frequent cause of fracture was falls (Table 2) with 78 individuals (24%) reporting falls from their wheelchairs, and 114 individuals (35%) experiencing falls from their own height while standing or walking. The three most common locations of the fractures were the tibia and/or distal fibula (27%), distal femur (27%), and proximal femur (26%). Only 20 fractures were in the proximal tibia and/or fibula (6%). The most common location of fractures among ambulatory individuals was the distal tibia/fibula (36%) and among wheelchair-bound individuals was the femur (68%). Wheelchair-bound participants fractured mainly the femur compared to ambulatory participants who fractured mainly the distal lower limb (tibia/fibula/ foot) (p < 0.0001). Mean (SD) age of first fracture for women were 50.1 (±17.0) and for men 40.0 (±14.9) (p < 0.001). Forty-eight (15%) individuals experienced a second fracture, and five (2%) individuals experienced a third fracture (Table 2).
The mean (SD) major osteoporotic risk factor found on FRAX was 3.9% (±1.9) and there was a weak negative linear relationship with time to fracture (r = −0.19; p = 0.016; n = 165). Only 11 participants (3%) underwent DEXA and the median values were 0.60 g/cm2 for total femur and 0.72 g/cm2 for neck femur. Only 26 (8%) participants underwent bisphosphonate treatment after fracture. Just 41% of electronic records described the environment and fractures occurred mostly at home (Table 2). The following variables were not analyzed due to missing data: history of family fractures (27%), vitamin D (71%), calcium (68%), phosphorus (69%), magnesium (86%), parathyroid hormone (84%), and alkaline phosphatase levels (41%).
Discussion
The present study has been described osteoporosis-related fractures in individuals with SCI. The prevalence of fractures attributable to osteoporosis in Brazilian individuals has been described only in person without neurological impairment [23].
Our study found similar clinical and epidemiological profiles to other publications [3, 13, 14], including the prevalence of individuals with paraplegia, AIS A, spasticity, age of fracture (40+ years old) and time to fracture. Men and women had a similar frequency of fractures in the present study.
Most fractures occurred in the tibia and/or distal fibula, distal femur, or hip/proximal femur, and only a few cases occurred in the proximal tibia. Some previous findings demonstrated most fractures in the tibia/fibula [17, 24] and in the hip [25]. These results contrast some previous studies that demonstrated distal femur and proximal tibia as the most common fracture locations and bone loss. Some authors suggest DEXA measurement of the distal femur and proximal tibia [10, 12, 19, 26]. Our study found that fractures in hip/proximal femur and distal tibia/fibula were as common as the distal femur. However, the present study included individuals who were ambulatory and wheelchair dependent at a similar frequency. Ambulatory individuals fractured more often the distal tibia/fibula, and wheelchair-bound patients fractured the distal and proximal femur
The most frequent cause of the fractures was fall from a wheelchair or their own height while walking or standing. This result is not surprising because falls are a common health problem in individuals with SCI, and prevention of falls should be a priority. Another study found transfer as the main cause of fracture [17, 27]. However, we only considered transfer as the cause of fractured if the fracture occurred during the transfer per se, and classified the cause of fracture as a fall if the fracture occurred after the transfer or if the individuals fell on the floor during the transfer. This classification may explain the difference in results.
Notably, one-third of the participants had 25 hydroxyvitamin D [25(OH)D] levels <20 ng/ml. Previous studies found that 14–32% of individuals with SCI were deficient in vitamin D and 32% were deficient in vitamin D insufficient [27, 28]. In this study, we detected similar findings which emphasizes that even in a tropical country like Brazil, vitamin D deficiency is a common health problem as has already been published [28]. Nevertheless, 25(OH)D levels <20 ng/ml were not related to a short time development of fractures in our study.
Most participants were hospitalized after the fracture, and some had complications. Almost one-third of the participants reported worse performance in activities of daily living and ambulation after the fracture had healed. This result reflects the impact of fractures on the lives of individuals with SCI.
Brazil is still a country with a young population with SCI, and falls and fractures will be a major health problem in these individuals as they age. Special attention should be paid to the prevention of fractures, and appropriate treatments should be instigated to prevent excessive bone loss.
The design of this study precludes any causal conclusion. We noted that much of the data that could be associated with fracture occurrence were missing, such as history of family fractures, environmental conditions where the fractures occurred, and vitamin D, calcium, phosphorus, magnesium, parathyroid hormone alkaline phosphatase levels, which indicates that these investigations are not performed even in a rehabilitation hospital. Most of the physicians are not educated to measure these risk factors. DEXA was performed only in a few cases, and even after an osteoporotic fracture only 8% of patients received bisphosphonate prescriptions, which indicates that most physicians neglect osteoporosis after SCI.
Individuals with osteoporosis-related fractures after SCI had several complications. Most individuals were hospitalized, and half of them underwent surgery. These issues mean increased disability and cost for the health system. Understanding the clinical and epidemiological profile of this population will can help identify risk factors and establish prevention programs and appropriate treatment. Campaigns to prevent falls and stimulate the appropriate identification and treatment of osteoporosis in individuals with SCI should be promoted.
Data availability
Anonymized data will be shared by request from any qualified investigator.
References
Zleik N, Weaver F, Harmon RL, Le B, Radhakrishnan R, Jirau-Rosaly WD et al. Prevention and management of osteoporosis and osteoporotic fractures in persons with a spinal cord injury or disorder: a systematic scoping review. J Spinal Cord Med. 2019;42:735–59.
Jiang SD, Dai LY, Jiang LS. Osteoporosis after spinal cord injury. Osteoporos Int. 2006;17:180–92.
Frontera JE, Mollett P. Aging with spinal cord injury: an update. Phys Med Rehabil Clin N Am. 2017;28:821–28.
Craven BC, Robertson LA, McGillivray CF, Adachi JD. Detection and treatment of sublesional osteoporosis among patients with chronic spinal cord injury. Top Spinal Cord Inj Rehabil 2009;14:1–22.
Morse LR, Battaglino RA, Stolzmann KL, Hallett LD, Waddimba A, Gagnon D, et al. Osteoporotic fractures and hospitalization risk in chronic spinal cord injury. Osteoporos Int. 2009;20:385–92.
Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. Morbidity following lower extremity fractures in men with spinal cord injury. Osteoporos Int. 2013;24:2261–67.
Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. Mortality after lower extremity fractures in men with spinal cord injury. J Bone Min Res. 2014;29:432–39.
Battaglino RA, Lazzari AA, Garshick E, Morse LR. Spinal cord injury-induced osteoporosis: pathogenesis and emerging therapies. Curr Osteoporos Rep. 2012;10:278–85.
Bauman WA, Cardozo CP. Osteoporosis in individuals with spinal cord injury. PM R. 2015;7:188–201. quiz 201
Haider IT, Lobos SM, Simonian N, Schnitzer TJ, Edwards WB. Bone fragility after spinal cord injury: reductions in stiffness and bone mineral at the distal femur and proximal tibia as a function of time. Osteoporos Int. 2018;29:2703–15.
Riggs BL, Wahner HW, Dunn WL, Mazess RB, Offord KP, Melton LJ 3rd. Differential changes in bone mineral density of the appendicular and axial skeleton with aging: relationship to spinal osteoporosis. J Clin Investig. 1981;67:328–35.
Garland D, Adkins R, Stewart C. Fracture threshold and risk for osteoporosis and pathologic fractures in individuals with spinal cord injury. Top Spinal Cord Inj Rehabil. 2005;11:61–9.
Troy KL, Morse LR. Measurement of bone: diagnosis of SCI-induced osteoporosis and fracture risk prediction. Top Spinal Cord Inj Rehabil. 2015;21:267–74.
Uebelhart D, Demiaux-Domenech B, Roth M, Chantraine A. Bone metabolism in spinal cord injured individuals and in others who have prolonged immobilisation. A review. Paraplegia. 1995;33:669–73.
Bauman WA, Spungen AM. Metabolic changes in persons after spinal cord injury. Phys Med Rehabil Clin N Am. 2000;11:109–40.
Bethel M, Bailey L, Weaver F, Harmon RL, Priebe MM, Le B, et al. A historical study of appendicular fractures in veterans with traumatic chronic spinal cord injury: 2002–2007. J Spinal Cord Med. 2016;39:686–92.
Akhigbe T, Chin AS, Svircev JN, Hoenig H, Burns SP, Weaver FM, et al. A retrospective review of lower extremity fracture care in patients with spinal cord injury. J Spinal Cord Med. 2015;38:2–9.
Abderhalden L, Weaver FM, Bethel M, Demirtas H, Burns S, Svircev J, et al. Dual-energy X-ray absorptiometry and fracture prediction in patients with spinal cord injuries and disorders. Osteoporos Int. 2017;28:925–34.
Cirnigliaro CM, Myslinski MJ, La Fountaine MF, Kirshblum SC, Forrest GF, Bauman WA. Bone loss at the distal femur and proximal tibia in persons with spinal cord injury: imaging approaches, risk of fracture, and potential treatment options. Osteoporos Int. 2017;28:747–65.
Morse LR, Bauman WA, Craven C, Frotzler A, Leslie W, Schnitzer TJ et al. International spinal cord injury fracture history extended data set (version 1.0). https://www.iscos.org.uk/uploads/sitefiles/Data20Sets/Fracture%20History/ISCIEDS_Fracture. Accessed Feb 2017.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–07.
Marinho BC, Guerra LP, Drummond JB, Silva BC, Soares MM. The burden of osteoporosis in Brazil. Arq Bras Endocrinol Metabol. 2014;58:434–43.
Frotzler A, Cheikh-Sarraf B, Pourtehrani M, Krebs J, Lippuner K. Long-bone fractures in persons with spinal cord injury. Spinal Cord. 2015;53:701–4.
Cochran TP, Bayley JC, Smith M. Lower extremity fractures in paraplegics: pattern, treatment, and functional results. J Spinal Disord. 1988;1:219–23.
Nottage WM. A review of long-bone fractures in patients with spinal cord injuries. Clin Orthop Relat Res. 1981;155:65–70.
Koutrakis NE, Goldstein RL, Walia P, Polak MM, Lazzari AA, Tun CG, et al. Vitamin D, diet, and lifestyle in a chronic SCI population. Spinal Cord. 2019;57:117–27.
Maeda SS, Borba VZ, Camargo MB, Silva DM, Borges JL, Bandeira F, et al. Recommendations of the Brazilian Society of Endocrinology and Metabology (SBEM) for the diagnosis and treatment of hypovitaminosis D. Arq Bras Endocrinol Metabol. 2014;58:411–33.
Acknowledgements
The authors would like to thank Luiz Sérgio Vaz for statistical analysis.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
The Research Ethics Committees of the Sarah Network of Rehabilitation Hospitals approved this study number: 66396817.7.0000.0022
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Champs, A.P.S., Maia, G.A.G., Oliveira, F.G. et al. Osteoporosis-related fractures after spinal cord injury: a retrospective study from Brazil. Spinal Cord 58, 484–489 (2020). https://doi.org/10.1038/s41393-019-0387-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0387-9