Abstract
Study design
Experimental before–after design.
Objectives
The objectives of this study were to explore the effects of local cooling rates on perfusion of sacral skin under externally applied pressure in people with spinal cord injury (SCI).
Setting
Research laboratory.
Methods
Seventeen participants, including seven wheelchair users with SCI and ten able-bodied (AB) controls. Each participant underwent seven protocols, including pressure (60 mmHg) with local cooling (∆t = −10 °C) for 20 min at three cooling rates (−0.5, −4, −10 °C/min), pressure with local cooling for 40 min, pressure with local heating (∆t = +10 °C), local cooling without pressure, and pressure without temperature changes. Each protocol included a 10-min baseline, a 20-min (or 40-min) loading period and a 20-min recovery. A compound sensor head consisting of laser Doppler and heating and cooling probes was used to measure sacral skin blood flow and temperature in the prone position. Blood flow responses were characterized by peak blood flow, recovery time, and total blood flow in the recovery period.
Results
The results demonstrated that the cooling rate at −10 °C/min resulted in smaller skin blood flow response compared with −0.5 °C/min (p < 0.05) but were not significantly different to the cooling rate at −4 °C/min. There was a significant difference in the recovery time between the 20-min cooling compared with the 40-min cooling for the SCI group (p < 0.05).
Conclusions
Our findings provide initial evidence that local cooling rates affect skin blood flow responses under externally applied pressure in people with SCI.
Similar content being viewed by others
Introduction
Pressure injury is one of most serious complications in wheelchair users with spinal cord injury (SCI) [1, 2]. Due to loss of sensory, motor, and autonomic functions along with repetitive exposures to mechanical stresses and deformations, wheelchair users with SCI are at high risk for pressure injury [3,4,5]. It is estimated that the incidence of pressure injury in community-dwelling adults with SCI is more than 30% per year and the cumulative incidence during their life time is up to 80% [6].
Numerous factors, including pressure, shear, temperature, and moisture, have been demonstrated to contribute to pressure injury formation in people with SCI [2]. Among these factors, temperature is a causative factor that has not been well studied and incorporated in support surface technology for the prevention of pressure injury [7,8,9]. Theoretically, soft tissues have a lower metabolic rate at a lower temperature. Accordingly, local cooling of weight-bearing tissues reduces metabolic demands and thus may reduce tissue ischemia and risk of pressure injury [10]. Research studies have provided initial evidence of using local skin cooling to reduce severity of tissue damage in animal models [9, 11,12,13] and human subjects [8, 14, 15].
Iaizzo, Kokate et al. have demonstrated a close relationship between the severity of tissue damage and skin temperature in a porcine model [11, 13], suggesting that local cooling may reduce tissue damage in weight-bearing tissues. Jan et al. examined skin blood flow (SBF) response to 700 mmHg (93.3 kPa) loading pressure at three temperatures, including local cooling (Δt = −10 °C), local heating (Δt = +10 °C), and no temperature changes in rats [12]. Their results showed that local cooling may reduce tissue ischemia by causing a smaller reactive hyperemic response. Later, they used the same experimental settings in another study and demonstrated that the reduced blood flow response under cooling is related to the release of TNF-alpha (a proinflammatory cytokine) in rats [9].
Tzen et al. compared reactive hyperemia in response to 60 mmHg (8 kPa) between local cooling to 25 °C and no cooling on the sacrum and demonstrated that local cooling induces a smaller hyperemia in able-bodied (AB) subjects [15]. However, people with SCI lose sympathetic innervation over peripheral microcirculation that may attenuate SBF response to local cooling. It is unclear whether local cooling is effective on reducing ischemia of weight-bearing tissues in people with SCI. Jan et al. studied SBF response to 60 mmHg loading pressure at three temperature (Δt = −10 °C, Δt = +10 °C, and Δt = 0) in people with SCI [8]. Their results showed that local cooling could induce a smaller reactive hyperemia in people with SCI. Using wavelet-based spectral analysis of blood flow oscillations [16], they further demonstrated that a smaller reactive hyperemia is attributed to a smaller contribution from both the metabolic and neurogenic activities.
The study of local cooling on SBF regulations of nonweight-bearing skin has been extensively studied [17]. Yamazaki et al. demonstrated that the rate of cooling (i.e., −0.5 and −4 °C/min) affects blood flow responses to local cooling [18]. Local cooling rate at −4 °C/min induces a biphasic response of SBF, including an initial vasoconstriction due to the Rho–Rho kinase system and then a transient vasodilation and a prolonged vasoconstriction involved with both activation of adrenoceptors and inhibition of nitric oxide synthase (NOS) [17]. Local cooling rate at −0.5 °C/min only induces a prolonged vasoconstriction. Following SCI, thermoregulation becomes an issue in people with high-level complete transaction [19]. People with SCI lose all or part of autonomic nervous system over thermoregulatory functions; however, local regulation such as vascular response to local cooling may still function following SCI. Also, studies discussing SBF response to local cooling did not intend to understand SBF response to local cooling under externally applied pressure, a needed process for pressure injury development. It is unclear whether under externally applied pressure, SBF response to local cooling would demonstrate similar responses, that is, not under externally applied pressure.
For the development of guideline and product of applying local cooling to weight-bearing tissues to reduce risk of pressure injury, it is imperative to explore how local cooling rates and durations affect SBF responses [8]. Furthermore, the effects of various parameters of local cooling (e.g., cooling rates and cooling duration) have not been studied in weight-bearing tissues that may limit the development of cooling technology for preventing pressure injury. This is particularly important because people with SCI may exhibit very different responses compared with people without SCI. Thus, the objectives of this study were to investigate the effects of rates and durations of local cooling on SBF under loading in people with SCI.
Methods
Participants
The inclusion criteria included traumatic SCI, injury level between C4 and T5, and American Spinal Injury Association Impairment Scale (AIS) between A and C. Each participant with SCI needed to be in a stable clinical condition (the traumatic event occurred more than 6 months before the time of the study). The recruitment of AB controls was to document normal responses of SBF during various experimental protocols. This study was approved by the local institutional review board for human subject research (OU #14307). All participants gave consent prior participating in this study.
Data acquisition
A before–after research design was used in this study. The experiments were performed in a research laboratory. Room temperature was maintained at 24 ± 2 °C. After at least 30 min stay in the lab to become acclimated to the room temperature for achieving a steady blood flow level [8, 20], the participant was positioned in a prone posture on a mat table. A compound probe (Perimed, Ardmore, PA, USA) consisting of temperature control and laser Doppler probe was placed over the sacral skin [8]. SBF and temperature were sampling at 32 Hz. A custom designed indenter was used to apply a pressure of 60 mmHg to the sacral skin [8].
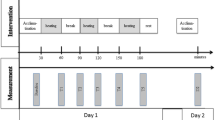
All participants underwent seven experimental protocols (Table 1) in two visits for a total of about 8–10 h, including:
Visit #1 (190 min)
P1: 10-min baseline, pressure (60 mmHg) without temperature changes for 20 min, 20-min recovery, and 20-min washout period.
P2: 10-min baseline, pressure (60 mmHg) with cooling (Δt = −10 °C) at a rate of −10 °C/min for 20 min, 20-min recovery, 20-min washout period.
P3: 10-min baseline, pressure (60 mmHg) with local heating (Δt = +10 °C) at a rate of +10 °C/min for 20 min, and 20-min recovery.
Visit #2 (280 min)
P4: 10-min baseline, pressure (60 mmHg) with cooling (Δt = −10 °C) at a rate of −10 °C/min for 40 min, 20-min recovery, and 20-min washout.
P5: 10-min baseline, cooling (Δt = −10 °C) to at a rate of −10 °C/min for 20 min, 20-min recovery, and 20-min washout.
P6: 10-min baseline, pressure (60 mmHg) with cooling (Δt = −10 °C) at a rate of −0.5 °C/min for 20 min, 20-min recovery, and 20-min washout.
P7: 10-min baseline, pressure (60 mmHg) with cooling (Δt = −10 °C) at a rate of −4.0 °C/min for 20 min, and 20-min recovery.
The data collected in the protocols 1, 2, and 3 were reported in our previous paper [8]. These data were used for the comparison purpose in this study. The main protocols (4, 5, 6, 7) were not reported in any other paper. All participants completed the second visit between 7 and 9 days of the first visit to ensure that the sacral skin was not under the influence of the experiment conducted in the first visit. The long hours required for completing these seven protocols significantly impacted the recruitment of participants with SCI. The original intent was to recruit ten people with SCI and ten AB controls. Examples of SBF and temperature response to seven protocols are provided in Figs. 1 and 2, respectively.
Typical examples of skin blood flow (SBF) response to seven protocols. a Pressure without temperature changes (P1). b Pressure with local cooling at a rate of −10 °C/min for 20 min (P2). c Pressure with local heating for 20 min (P3). d Pressure with cooling at a rate of −10 °C/min for 40 min (P4). e Cooling at a rate of −10 °C/min for 20 min (P5). f Pressure with cooling at a rate of −0.5 °C/min for 20 min (P6). g Pressure with cooling at a rate of −4.0 °C/min for 20 min (P7)
Typical examples of skin temperature in seven protocols. a Pressure without temperature control (P1). b Pressure with cooling at a rate of −10 °C/min for 20 min (P2). c Pressure with local heating (P3). d Pressure with cooling at a rate of −10 °C/min for 40 min (P4). e Cooling at a rate of −10 °C/min for 20 min (P5). f Pressure with cooling at a rate of −0.5 °C/min for 20 min (P6). g Pressure with cooling at a rate of −4.0 °C/min for 20 min (P7)
Data analysis
SBF response was characterized by the peak flow and total flow after removal of loading pressure and temperature control and the time needed for blood flow to return to the baseline (i.e., recovery time) [8]. Because the calculated peak blood flow and total blood flow may be influenced by the baseline blood flow level, the two measures were normalized by the baseline [20]. By comparisons of blood flow responses during P2 (cooling rate at −10 °C/min), P6 (cooling rate at −0.5 °C/min), and P7 (cooling rate at −4 °C/min), the effect of cooling rates on modulating SBF responses could be studied. By comparisons of P2 (cooling duration at 20 min) and P4 (cooling duration at 40 min), the effect of cooling durations on reducing skin ischemia could be studied. Because of the small sample size, the Wilcoxon signed rank test was used to examine the statistical differences among seven protocols. The level of significance was set at 0.05 for this exploratory study consisting of seven repeated measures. All calculations and statistical analyses were performed using Matlab R2017b (Natick, MA, USA).
Results
Seventeen participants were recruited into this study, including seven wheelchair users with SCI and ten AB controls. All participants with SCI had a traumatic spinal injury between C4 and T5 and met the American Spinal Injury AIS levels between A and C. None of the participants showed symptoms of cardiopulmonary diseases, diabetes, or used any medications that might affect cardiovascular function. Their demographic data are listed in Table 2.
Pressure with cooling
In the SCI group, peak blood flow (p < 0.05) and total blood flow (p < 0.05) were significantly lower in all protocols of pressure with cooling (P2, P4, P6, P7) compared with pressure with heating (P3), but did not show significant differences between pressure with cooling (P2, P4, P6, P7) and pressure without temperature changes (P1). In the AB group, peak hyperemia (p < 0.05) and total hyperemia (p < 0.05) in all protocols of pressure with cooling were significantly lower than those under pressure with heating. (Fig. 3 and Table 3)
Pressure with three cooling rates
For cooling rate effects, SBF responses of protocols P2 (pressure with cooling rate at −10 °C/min), P6 (pressure with cooling rate at −0.5 °C/min), and P7 (pressure with cooling rate at −4 °C/min) were compared in the SCI group. The results showed that cooling rate at −10 °C/min results in significantly smaller total blood flow compared with −0.5 °C/min (p < 0.05). However, there were no significant differences between −10 °C/min and −4 °C/min and between −4 °C/min and −0.5 °C/min. (Fig. 3 and Table 3)
Pressure with two cooling durations
For cooling duration effects, recovery time of protocols of P2 (20 min duration) and P4 (40 min duration) showed a significant difference (p < 0.05) in the SCI group. The AB group showed a significant difference in the peak hyperemic response between two protocols (p < 0.05) (Fig. 3 and Table 3).
Cooling without pressure
For cooling without pressure (P5), SBF shows an initial decrease (vasoconstriction), a small transient increase (vasodilation) and then a prolonged decrease (vasoconstriction) compared with baseline (Fig. 1e).
Skin temperature
Values of skin temperature during the baseline, stimulus (loading) period, and the first 5 min of the recovery period (reactive hyperemia) are listed in Table 4.
Discussion
The results of this study demonstrated that: (1) pressure with cooling resulted in a smaller blood flow response as compared with both pressure with heating and pressure without temperature changes after 20-min pressure at 60 mmHg in people with SCI, (2) a fast cooling rate was more effective on decreasing blood flow responses in the weight-bearing skin in people with SCI, and (3) the duration of cooling also affected blood flow responses of weight-bearing skin in people with SCI. Our findings may provide initial evidence for determining parameters of cooling technology (e.g., cooling rates and cooling durations) for preventing pressure injury in people with SCI. The findings of this study and previous animal studies [9, 11,12,13] suggest that a support surface (e.g., wheelchair cushion) with cooling might effectively reduce ischemia of compressed soft tissues around the ischial tuberosity for preventing pressure injury in wheelchair users with SCI. Although the microclimate factor (temperature and relative humidity) has been gaining recognitions among clinicians [7], the development and implementation of wheelchair cushions with cooling is worth more investigation.
Our study showed that total SBF was smaller in pressure (60 mmHg) with cooling rate of −10 °C/min (P2) compared with pressure with cooling rate of −0.5 °C/min (P6) in people with SCI. This suggests that a fast cooling rate may be more effective on reducing ischemia of weight-bearing tissues in people with SCI. This result is consistent with previous studies on investigating cooling rates in nonweight-bearing skin [18]. Yamazaki et al. reported that local cooling could induce a biphasic response, including an initial vasoconstriction and then a transient vasodilation and a prolonged vasoconstriction; and such response is dependent on the cooling rate [18]. In the present study, the results suggest that under the same loading pressure and the same duration, fast cooling simultaneously applied with pressure may cause a smaller stress (or stimulus) to the weight-bearing skin compared with slower cooling. This means that in the same person, a smaller ischemia caused by externally applied pressure would elicit a smaller reactive hyperemia response [21, 22]. It should be noted that in the protocol P2, mean skin temperature during the recovery period (23.9 ± 0.2 °C) was lower than that in the protocol P6 (25.1 ± 1.0 °C). The lower temperature was correlated to a smaller reactive hyperemia (or SBF response).
Intensities of reactive hyperemic response have led to the concept of flow- or oxygen-debt “repayment” [23]. Although the SBF response in this study is not strictly a reactive hyperemic response due to mixed loading and temperature stimuli, the blood flow responses under various cooling rates may follow the principle of oxygen-debt repayment. The flow debt repayment is represented by the area under the hyperemia curve [8, 23], which is proportional to total hyperemia. Our results showed that reactive hyperemic response was largest in pressure with heating (P3), modest in pressure without temperature changes (P1) and pressure with cooling for 40 min (P4), and smallest in pressure with cooling for 20 min (P2). Comparing reactive hyperemia between pressure with cooling for 20 min (P2) and for 40 min (P4), it can be deduced that a longer occlusion duration resulted in a larger reactive hyperemic response in weight-bearing tissues in people with SCI. This observation is consistent with the previous studies [22, 23]. By comparing reactive hyperemia between pressure with cooling and pressure without temperature changes for the same duration (P2 and P1), it could be deducted that local cooling reduces reactive hyperemic response in weight-bearing tissues. On the other hand, recovery time and total hyperemia in pressure with cooling for 40 min (P4) was comparable with those in pressure without temperature changes for 20 min (P1), suggesting that the effect of decreasing temperature by 10 °C on reducing reactive hyperemia was comparable with that of shortening the occlusion duration by 20 min.
Based on our results, people with SCI demonstrated a microvascular regulatory function in response to various interface loading pressure and temperature stimuli. These observed responses may be contributed by these local mechanisms, such as NOS. In the previous study [18], NOS enzymes include neuronal, inducible, and endothelial NOS that may be involved in skin blood regulation in response to local cooling. Among these NOS enzymes, endothelial NOS (released by vascular endothelial cells) may be particularly important in people with complete SCI (no sensory and motor functions below the injury level) in reducing ischemia of the weight-bearing skin. Also, a transient increase in SBF under fast cooling may be a promising function that can be used to increase skin and underlying soft tissue viability in people with SCI. This cooling-induced vasodilatory response was reported by Pergola et al. [24]. Cooling appears to be a promising intervention to reduce ischemia and risk of pressure injury in people with SCI given the fact of these local mechanisms (endothelial and vascular smooth muscle cells) remain functioning following SCI.
Our results indicated that SBF response in people with SCI showed less distinct differences among the protocols compared with AB controls. This means that the effect of local cooling on reducing tissue ischemia was attenuated. Such an attenuation might be associated with diminished function of sensory nerves in people with SCI, because sensory nerves have been found to be involved in reactive hyperemic response [25, 26] and cold-induced vasoconstriction [24, 27]. Nevertheless, our results may be worth further investigation for its potential therapeutic effects on helping to prevent pressure injury. Our results suggested that a decrease in skin temperature by 10 °C seems to be effective for reducing skin ischemia of weight-bearing tissues and that a higher cooling rate may be more beneficial for this purpose. However, our results were obtained using the protocols in which a surface pressure of 60 mmHg was applied to the sacral skin. In real life environments, wheelchair cushion interface pressure may vary considerably among individuals, especially in people with SCI [28]. More studies are needed to understand the interactions between various loading conditions and thermal stress (heating and cooling) and their effects on ischemia of weight-bearing tissues in people with SCI.
Study limitations
This study had several limitations. First, we were only able to recruit seven people with SCI for the experiments. Due to organizational aspects and lack of participants being willing to participate, the author had to finish earlier. The current protocols required participants to lie still in a prone position for better control of loading pressure patterns, which might cause discomfort in participants. Future study may need to develop a more comfortable position for participants. Our findings may be influenced by the small sample sizes. However, the purpose of this exploratory study was to test the feasibility of using local cooling for reducing skin ischemia in people with SCI and the efficacy of different cooling rates. Our results showed that local cooling can reduce reactive hyperemic response and that a higher cooling rate may be more effective. Second, people with SCI were older than AB controls. Hence, impaired microvascular function in this population was due to a combination of SCI and the aging process. However, as mentioned above, the purpose of this study was to compare the influence of various cooling rates on SBF responses under externally applied pressure. The author used the repeated measures design (cooling at different cooling rates for different durations, heating, and no temperature control) and therefore a participant served as his/her own controls. The age effect on the SBF response to three protocols should be kept minimal in our design. Last, there are many statistical comparisons in this study. Some of these findings may be spurious because of the high number of statistical tests used in this exploratory study.
Conclusion
Our results suggest that fast local cooling may be more effective on affecting SBF responses under loading pressure. By assessing SBF response to various cooling rates and durations, clinicians may develop local cooling parameters to prevent pressure injury in people with SCI.
Data availability
The skin blood flow data collected during the current study are available from the corresponding author on reasonable request
References
Krause JS, Saunders LL. Health, secondary conditions, and life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2011;92:1770–5.
Jan YK, Brienza DM. Technology for pressure ulcer prevention. Top Spinal Cord Inj Rehabil. 2006;11:30–41.
Jan YK, Anderson M, Soltani J, Burns S, Foreman RD. Comparison of changes in heart rate variability and sacral skin perfusion in response to postural changes in people with spinal cord injury. J Rehabil Res Dev. 2013;50:203–14.
Jan YK, Crane BA, Liao F, Woods JA, Ennis WJ. Comparison of muscle and skin perfusion over the ischial tuberosities in response to wheelchair tilt-in-space and recline in people with spinal cord injury. Arch Phys Med Rehabil. 2013;94:1990–6.
Jan YK, Liao F, Jones MA, Rice LA, Tisdell T. Effect of durations of wheelchair tilt-in-space and recline on skin perfusion over the ischial tuberosity in people with spinal cord injury. Arch Phys Med Rehabil. 2013;94:667–72.
Vaishampayan A, Clark F, Carlson M, Blanche EI. Preventing pressure ulcers in people with spinal cord injury: targeting risky life circumstances through community-based interventions. Adv Skin Wound Care. 2011;24:275–84. quiz 285-6.
Kottner J, Black J, Call E, Gefen A, Santamaria N. Microclimate: a critical review in the context of pressure ulcer prevention. Clin Biomech. 2018;59:62–70.
Jan YK, Liao F, Rice LA, Woods JA. Using reactive hyperemia to assess the efficacy of local cooling on reducing skin ischemia under surface pressure in people with spinal cord injury: a preliminary report. Arch Phys Med Rehabil. 2013;94:1982–9.
Lee B, Benyajati S, Woods JA, Jan YK. Effect of local cooling on pro-inflammatory cytokines and blood flow of the skin under surface pressure in rats: feasibility study. J Tissue Viability. 2014;23:69–77.
Lachenbruch C. Skin cooling surfaces: estimating the importance of limiting skin temperature. Ostomy Wound Manag. 2005;51:70–9.
Kokate JY, Leland KJ, Held AM, Hansen GL, Kveen GL, Johnson BA, et al. Temperature-modulated pressure ulcers: a porcine model. Arch Phys Med Rehabil. 1995;76:666–73.
Jan YK, Lee B, Liao F, Foreman RD. Local cooling reduces skin ischemia under surface pressure in rats: an assessment by wavelet analysis of laser Doppler blood flow oscillations. Physiol Meas. 2012;33:1733–45.
Iaizzo PA, Kveen GL, Kokate JY, Leland KJ, Hansen GL, Sparrow EM. Prevention of pressure ulcers by focal cooling: histological assessment in a porcine model. Wounds. 1995;7:161–9.
Liao FY, Yang TD, Wu FL, Cao CM, Mohamed A, Jan YK. Using Multiscale Entropy to Assess the Efficacy of Local Cooling on Reactive Hyperemia in People with a Spinal Cord Injury. Entropy-Switz. 2019;21:90.
Tzen YT, Brienza DM, Karg P, Loughlin P. Effects of local cooling on sacral skin perfusion response to pressure: implications for pressure ulcer prevention. J Tissue Viability. 2010;19:86–97.
Jan YK, Brienza DM, Geyer MJ, Karg P. Wavelet-based spectrum analysis of sacral skin blood flow response to alternating pressure. Arch Phys Med Rehabil. 2008;89:137–45.
Johnson JM, Kellogg DL. Local thermal control of the human cutaneous circulation. J Appl Physiol. 2010;109:1229–38.
Yamazaki F, Sone R, Zhao K, Alvarez GE, Kosiba WA, Johnson JM. Rate dependency and role of nitric oxide in the vascular response to direct cooling in human skin. J Appl Physiol. 2006;100:42–50.
Price MJ, Trbovich M. Thermoregulation following spinal cord injury. Hand Clin. 2018;157:799–820.
Jan YK, Brienza DM, Boninger ML, Brenes G. Comparison of skin perfusion response with alternating and constant pressures in people with spinal cord injury. Spinal Cord. 2011;49:136–41.
Brienza DM, Geyer MJ, Jan YK. A comparison of changes in rhythms of sacral skin blood flow in response to heating and indentation. Arch Phys Med Rehabil. 2005;86:1245–51.
Johnson PC, Burton KS, Henrich H, Henrich U. Effect of occlusion duration on reactive hyperemia in sartorius muscle capillaries. Am J Physiol. 1976;230:715–9.
Davis MJ, Hill MA, Kuo L, Tuma RF, Duran WN, Ley K. Local regulation of microvascular perfusion. Handbook of Physiology: Microcirculation. San Diego: Academic Press; 2008. 161–284.
Pergola PE, Kellogg DL Jr., Johnson JM, Kosiba WA, Solomon DE. Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin. Am J Physiol. 1993;265:H785–92.
Larkin SW, Williams TJ. Evidence for sensory nerve involvement in cutaneous reactive hyperemia in humans. Circ Res. 1993;73:147–54.
Lorenzo S, Minson CT. Human cutaneous reactive hyperaemia: role of BKCa channels and sensory nerves. J Physiol. 2007;585:295–303.
Alba BK, Castellani JW, Charkoudian N. Cold-induced cutaneous vasoconstriction in humans: function, dysfunction and the distinctly counterproductive. Exp Physiol. 2019;104:1202–14.
Gefen A. The biomechanics of sitting-acquired pressure ulcers in patients with spinal cord injury or lesions. Int Wound J. 2007;4:222–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Ethical approval
The author certifies that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jan, YK. The effects of local cooling rates on perfusion of sacral skin under externally applied pressure in people with spinal cord injury: an exploratory study. Spinal Cord 58, 476–483 (2020). https://doi.org/10.1038/s41393-019-0378-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0378-x