Abstract
Study design
Prospective cohort study of the Thai Spinal Cord Injury Registry.
Objective
To determine whether being admitted to a spinal cord injury (SCI) specialized rehabilitation facility (SSRF) is associated with better functional outcomes.
Setting
Four rehabilitation facilities in Thailand; one a SSRF and the others non-SSRFs.
Methods
Data from the one SSRF and three non-SSRFs were extracted from the Thai Spinal Cord Injury Registry. Multivariate regression analysis was used to exclude the effect of confounding factors and prove the independent association of SSRF admission with respect to Spinal Cord Independence Measurement (SCIM) at discharge.
Results
Among the 234 new SCI inpatients enrolled, 167 persons (71%) had been admitted to the SSRF. The SSRF had a greater proportion of persons with AIS A, B, C tetraplegia and people with AIS D, whereas the non-SSRFs had a higher proportion of patients with AIS A, B or C paraplegia. Patients discharged from the SSRF demonstrated a greater SCIM score improvement than those from the non-SSRFs (24.1 vs 17.0; p = 0.003). By using multivariate regression analysis controlling for age, time from injury to rehabilitation, severity of injury and SCIM score on admission, SSRF admission was found to be an independent predictive factor of SCIM score improvement at discharge (p = 0.008).
Conclusion
Admission to an SSRF is associated with better rehabilitation outcomes. This finding supports the importance of SSRF access to improve the functional outcome of patients with SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) potentially leads to impairment of bodily functions, resulting in limitation of activities and participation. The incidence of SCI varies worldwide, ranging from ten per million in the Netherlands to 83 per million in North America [1]. In Thailand, Kovindha et al. (1993) reported that the approximate incidence of SCI was 23 cases per million individuals [2]. The direct costs for the care of persons with SCI are staggering at a lifetime US$ 1.1–4.6 million per person [1]. Although there have been major advances in understanding the pathophysiologic mechanisms of SCI, to date, a treatment resulting in significant neurologic recovery has not been found [3]. Therefore, a comprehensive medical rehabilitation program aimed to maximize functional recovery, remains the conventional management of SCI.
To evaluate the efficiency of SCI rehabilitation, a number of rehabilitation outcome measures have been introduced [4, 5]. Among these, the Spinal Cord Independence Measure (SCIM) is one of the most commonly used functional outcome measures in SCI [6]. SCIM is a well-developed, valid and reliable tool, specifically for people with SCI [7,8,9]. It was introduced in 1997, revised in 2002 [10, 11], with the latest version SCIM III published in 2007 [12]. The SCIM score ranges from 0 points, indicating complete dependence, to 100 points, indicating complete independence. The SCIM is used as a measure of rehabilitation outcomes, with a greater improvement of SCIM scores reflecting greater rehabilitation effectiveness. To evaluate the time-dependent efficiency of the rehabilitation process, dividing SCIM improvement by length of stay (LOS) is proposed to represent rehabilitation efficiency [13].
Thailand, similar to most low-middle income countries [14,15,16], has no rehabilitation center solely dedicated to SCI rehabilitation [17]. Rehabilitation at Maharaj Nakorn Chiang Mai Hospital, a university hospital, is the only rehabilitation facility closest to a SCI specialized rehabilitation center, as determined by its 30-year history of continuous services and research dedicated to patients with SCI [17]. As SCI rehabilitation generally demands specialized knowledge and skills, with staff and leadership with SCI-expertise, it is reasonable to expect that admission to the SCI specialized rehabilitation facility (SSRF) should lead to better functional outcomes than admission to a non-SSRF. Previous evidence from Cheng et al. (2017) has demonstrated a significantly higher rate of return to home in rehabilitation than non-rehabilitation-participating SCI patients in Canada [18]. New et al. (2011) compared Functional Independence Measurement (FIM) at discharge between people with SCI admitted to a SSRF and non-SSRF in Australia [19], and found that those from an SSRF had significantly better FIM improvement than those from non-SSRF. However, this effect was only found in persons with non-traumatic SCI [19]. To the best of our knowledge, there has yet to be research published directly comparing rehabilitation effectiveness and efficiency of SSRFs and non SSRFs in a low-middle income country.
According to the literature, there are numerous factors that could affect functional independence [20, 21]. For example, Mamound et al. (2017) reported that tetraplegia and longer time from injury to rehabilitation admission had small but significant negative association with discharge FIM motor score [20]. Another study also demonstrated the negative association between time from injury to rehabilitation admission in traumatic SCI [22]. Age has been suggested to be a factor affecting functional independence after SCI. Although the effect of age on SCI rehabilitation outcome is inconsistent [23, 24], the tendency is an inverse effect [25]. Studies have also demonstrated that non-traumatic etiology had a negative effect on function improvement after rehabilitation [26, 27], although this effect was not demonstrated in another study [28]. Therefore, level of injury, severity of injury (determined by the American Spinal Injury Association Impairment Scale (AIS)), SCIM score on admission, time from injury to rehabilitation, age, and etiology of SCI (traumatic vs non-traumatic) can have a confounding effect on functional outcomes and need to be controlled.
The aim of this study was (1) to compare rehabilitation effectiveness of patients admitted for rehabilitation to SSRFs and non SSRFs and (2) to determine if there is an association between SSRF admission and improvement of functional outcomes. Our hypothesis was that (1) patients admitted to an SSRF have better rehabilitation outcomes than those from non SSRFs and (2) there is an independent association between admission to a SSRF and SCIM score improvement at discharge.
Methods
SCI and non-SCI specialized rehabilitation facilities
Data were obtained from the medical records of patients with SCI admitted into each of four tertiary rehabilitation facilities in Thailand: (1) Maharaj Nakorn Chiang Mai Hospital, Faculty of Medicine, Chiang Mai University, Chiang Mai Province; (2) Sirindhorn National Medical Rehabilitation Institute, Ministry of Health, Nonthaburi Province; (3) Ratchaburi Hospital, Ministry of Public Health, Ratchaburi Province; and (4) Siriraj Hospital, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok. The percentage of SCI rehabilitation per total rehabilitation admission/the total number of rehabilitation beds/the number of SCI admission per year in the study period were 80/20/160 for Maharaj Nakorn Chiang Mai Hospital, 37/48/137 for Sirindhorn National Medical Rehabilitation Institute, 2.5/28/15 for Ratchaburi Hospital and 2.5/25/23 for Siriraj Hospital, respectively (these numbers include readmissions). Focusing on both the number of annual cases and concentration in SCI rehabilitation, we defined the criteria for SCI-specialized rehabilitation facilities (SSRFs) as (1) having more than 100 SCI rehabilitation admissions annually and (2) having SCI rehabilitation admissions greater than 60% of total rehabilitation admissions. Using these criteria, only Maharaj Nakorn Chiang Mai met the SSRF criteria, while the other three rehabilitation facilities were defined as non SSRFs.
Participants
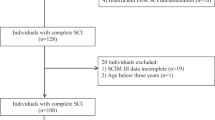
Both patients with traumatic and non-traumatic SCI were enrolled in this study. The inclusion criteria were (1) over 18 years of age; (2) first rehabilitation admission for SCI. The exclusion criteria were (1) admitted for the treatment of complications; (2) admitted for less than 5 days. The later criterion was used to exclude admissions that ended with incomplete rehabilitation programs.
Study protocol
This study comprised a secondary analysis of the SCI registry study in Thailand. The study protocol was approved by the Institutional Ethics Committee of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand and was in accordance with the current version of the Helsinki Declaration. The research ID is 2880 and the study code is REH-2558–02880. The study was also approved by the local Ethics Committee of each rehabilitation facility. Persons with SCI were admitted to a rehabilitation facility according to the catchment area of the universal coverage public health system of Thailand, as well as the willingness of the patient. On admission, informed consent was obtained from each eligible patient. Age, sex, level of injury (paraplegia/tetraplegia), AIS and LOS for rehabilitation were collected using the International Spinal Cord Injury core data set [29]. Time from injury to rehabilitation admission, the number of the days between injury date and rehabilitation admission date, were also calculated. Patients were classed into four groups according to the advisory guidelines of the International Spinal Cord Society (ISCoS): [30] (1) tetraplegia C1-C4 AIS A, B, C; (2) tetraplegia C5-C8 AIS A, B, C; (3) paraplegia AIS A, B, C; and (4) tetraplegia and paraplegia AIS D. Rehabilitation outcomes were collected using SCIM III [12]. The SCIM scores were obtained at least two times, on admission and at discharge. Rehabilitation effectiveness was calculated using the SCIM score improvement. Rehabilitation efficiency, which determines the change of rehabilitation outcome per one day of admission, was calculated using SCIM score improvement divided by LOS. Inpatient complications were also extracted.
Statistical analysis
Categorical variables were described using percentages of frequency. Normally distributed numerical variables were described using arithmetic means and standard deviations. Non-normally distributed numerical variables were described using median and interquartile range. Differences of parameters between SSRFs and non SSRFs were compared using an independent t-test or Mann–Whitney U test, depending on the type of distribution. Multiple linear regression analysis, backward method, was applied to determine the independent effect of the studied parameters on SCIM score at discharge: age, etiology of SCI, time from injury to rehabilitation admission, severity of injury, SCIM score on admission, time between SCIM measurements, LOS and having been admitted to the SSRF were included as the predicting factors. Statistical analyses were performed using SPSS version 22.0 for Windows (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
Demographic data
Demographic data are presented in Table 1. Patients from the SSRF were significantly older than those from the non-SSRFs (50.6 vs 43.1 years old, p = 0.004; independent t-test). SSRF patients had significantly shorter time from injury to rehabilitation than non SSRF patients (30 vs 168 days, p < 0.001; Mann–Whitney U test). Significant differences in the level and severity of injury were observed between the two types of rehabilitation facilities (p < 0.001; chi-square test). The SSRF had significantly greater proportion of people with AIS D tetraplegia and paraplegia, while non SSRFs had significantly greater proportion of people with AIS A, B, C paraplegia (42 vs 17% and 27 vs 58%, respectively). Patients from the SSRF had significantly longer LOS than those from non SSRFs (53.2 days vs 37.6 days, p < 0.001; Mann–Whitney U test). No difference in ratio of traumatic and non-traumatic SCI between participants in SSRF and non-SSRF was observed (p = 0.632, chi-square test) (Table 1).
Rehabilitation outcomes
No significant differences in SCIM scores at admission or at discharge were observed between the two types of rehabilitation facilities. Patients from the SSRF demonstrated greater improvement in SCIM scores than those from the non-SSRFs (24.1 vs 17.0, p = 0.01; Mann–Whitney U test). The rehabilitation efficiency, demonstrated by the improvement of the SCIM scores per day of admission, was also significantly greater in the SSRF compared with the non-SSRFs (Table 1).
In-patient complication rates
No significant differences in terms of inpatient overall and individual complication rates, including the incidences of urinary tract infections, pressure ulcers, venous thromboembolism, postural hypotension, musculoskeletal, and respiratory and psychiatric complications, were observed (Table 1).
Determining independent effect of the selected parameters on SCIM score at discharge using multivariate regression model
To avoid the non-linear effect of the continuous parameters, namely age, time from injury to rehabilitation admission, and LOS, we modified these parameters to ordinal dummy variables as per ISCOS recommendations [30]. Details of the modifications are presented in Table 2. Multiple linear regression analysis (backward method), demonstrated that age, severity of injury, admission SCIM, and SSRF admission were independent predictive factors of SCIM score at discharge. Factors of SCI etiology, time from injury to rehabilitation and LOS were not found to be independent predictive factors. Specifically, age had an unstandardized coefficient of −2.125 (Table 3). This result suggests that when all other independent variables are held constant, for each increasing age group, the SCIM score at discharge decreases by 2.1 points. Severity of injury on admission, defined as 0 when the patient was diagnosed with C1-C4 AIS A, B, C tetraplegia, 1 for C5-C8 AIS A, B, C tetraplegia, 2 for AIS A, B, C paraplegia, and 3 when the patient was diagnosed with AIS D tetraplegia or paraplegia, had an unstandardized coefficient of 8.884 (Table 3). This result suggests that when all other independent variables are held constant, people with C5-C8 AIS A, B, C tetraplegia have 8.9 higher SCIM scores at discharge when compared to those with C1-C4 A, B, C tetraplegia; persons with A, B, C paraplegia have 8.9 higher SCIM scores at discharge compared to those with C5-C8 AIS A, B, C tetraplegia, and persons with AIS D have 8.9 higher SCIM scores at discharge when compared to AIS A, B, C paraplegia. SCIM scores on admission had an unstandardized coefficient of 0.699. (Table 3), suggesting that when all other independent variables are held constant, for each increase in SCIM score at admission, the SCIM score at discharge decreases by 0.7 points. Importantly, being admitted into an SSRF had an unstandardized coefficient of 6.836. (Table 3), which suggests that when all other independent variables are held constant, those admitted to an SSRF will have a 6.9 greater SCIM score improvement after rehabilitation that those admitted to a non-SSRF.
Discussion
The major findings of this study are that the patients with SCI rehabilitated at the SSRF demonstrated significantly higher SCIM score improvement than those rehabilitated at non-SSRFs. This finding corresponds with other studies, and demonstrates that admission to an SSRF was an independent positive factor of SCIM score improvement after rehabilitation, with a relatively high unstandardized coefficient (6.836). Since a clinically significant SCIM change is considered to be at least 4 points [31], the difference of SCIM score between SSRF and non-SSRF in this study has clinical importance. We also confirm the results from previous studies that age [25] and severity of injury [20, 21] have an independent effect on SCIM score improvement after the rehabilitation process. These results confirmed our hypotheses; however, the interpretation and application of this result must be carefully considered due to several interesting aspects.
First, the difference in the SCI characteristics may be responsible for the variation in rehabilitation outcomes. The SSRF had significantly greater proportion of people with AIS D tetraplegia and paraplegia than the non-SSRF, whereas non-SSRFs had greater ratio of people with AIS A, B, C paraplegia. People with AIS D tetraplegia, whose lower extremity motor scores should be better, have more capacity in mobility, whereas people with AIS A, B, C paraplegia, whose upper extremity motor scores should be better, have increased ability to perform self-care activities. The SCIM comprises 40 points in the mobility subscores but only 20 points in the self-care measures [12]. Therefore, patients from the SSRF, which contained a greater ratio of people with AIS D tetraplegia, had increased ability for improvement of their SCIM scores than those from non-SSRFs, which contained a greater ratio of people with AIS A, B, C paraplegia.
Next, our results are inconsistent with the previous results from the study of New et al. (2011), who demonstrated significantly better functional improvements between SSRF and non- SSRF only in people with non-traumatic SCI [19]. Our findings may be due to the difference in the outcome measure used. In our study, we used SCIM score improvement, while the previous study used FIM score improvement as an indicator of rehabilitation effectiveness. Although both SCIM and FIM are functional measures, there are a number of differences in the details. Firstly, the SCIM has ten points possible for respiratory function, which can be improved in people with tetraplegia, but the FIM does not have this item. Secondly, although both SCIM and FIM have an item related to bladder function, the SCIM has more scoring options on management methods, such as indwelling catheterization, intermittent catherization, or voluntary voiding. Next, SCIM has more items on mobility function, such as mobility indoor, mobility for moderate distances and mobility outdoor, whereas FIM has only one item dedicated to locomotion [10, 32]. Since the SCIM is specifically made for evaluating the functional independence of people with SCI, we propose that using the SCIM to evaluate rehabilitation effectiveness in persons with SCI is more reasonable than using FIM.
In Thailand, there is no SCI rehabilitation center, and only one SSRF. This SSRF as described in this study is a tertiary level hospital. Among the three non-SSRFs, one is a tertiary public hospital, one is a general rehabilitation center and the other a university hospital. Notice that in this study, the number of the new patients recruited from the SSRF is 2.5 times more than those from the non-SSRFs. This difference may account for the better rehabilitation effectiveness in the SSRF, which has more SCI patients, resulting in more experience in caring for and rehabilitating patients with SCI. On the other hand, the complication rates in the SSRF were not different from those with shorter-admitted patients at the non-SSRFs, despite a longer LOS. This result may be due to both SSRF and non SSRFs being based in tertiary level hospitals, which have extensive experience in treating and preventing inpatient medical complications.
It is also worth noting that the rehabilitation efficiency was still greater in the SSRF than the non-SSRFs although the results of this study demonstrated a significant longer LOS of patients in the SSRF compared with patients in the non-SSRFs. As previously mentioned, rehabilitation efficiency is defined by functional improvement per day. This finding addresses the significant effect of SCIM score improvement that could dominate the difference in LOS. However, compared with previous studies from other countries [13, 33], the LOS for SCI rehabilitation (including the SSRF) in Thailand is relatively short due to limitations associated with the reimbursement process of the health care system in Thailand [34]. The LOS for neurological patients rehabilitated in Thailand is limited to 23 days [17]. This approach leads to admitting patients for longer than 23 days, which increases the cost without expanding the reimbursement. We suggest that the LOS in patients admitted to non SSRFs is too short to allow patients to achieve their expected SCIM scores and the system for reimbursement of medical rehabilitation in Thailand needs to be reconsidered.
Although this study is based on the largest SCI cohort in Thailand, it still has limitations. A major limitation in this study was that it potentially had a high risk from two types of biases, namely unmeasured confounding factors and unknown selection bias. Unmeasured confounding factors potentially included patients’ socio-economic factors (environmental factors), as well as premorbid general physical and mental health status (personal factors). Both are called “contextual factors” according to the International Classification of Functioning, Disability and Health (ICF) framework. We suggest that a direct acyclic graph (DAG) identifying all associated factors by using the ICF Core Sets for individuals with SCI in the early post-acute context [35] might be used for conducting further cohort studies. An example of a DAG for this study is presented in Fig. 1. A DAG is a causal diagram presented by a graphic model that depicts a set of hypotheses about the causal process that generates a set of variables of interest. DAG is used to demonstrate the putative effect of a set of variables, called exposures, on another set of variables called outcomes. It can be used to identify confounding factors, which could affect both exposures and outcomes, called biases. One can study DAG in www.dagitty.net [36]. The selection bias was described by survivor bias due to differential mortality prior to admission. This might be due to the long time between SCI diagnosis and admission to first rehabilitation in combination with a potentially high mortality of SCI in low-middle income countries.
The theoretical paradigm for the further study using a direct acyclic graph model. The outcome was a rehabilitation outcome, which was SCIM score at discharge. The focusing exposure was having been admitted to a SCI specialized rehabilitation facility. The adjusted confounding factors were age, time from injury to rehabilitation admission, etiology of SCI, SCIM score on admission, severity of injury and length of stay. However, only age, time from injury to rehabilitation admission, etiology of SCI and severity of injury can influence both exposure and outcome, indicating potential biases. SCIM Spinal cord independence measure, SCI spinal cord injury
Another limitation in our study is that no psychological factors were determined. Thietje et al. (2010) reported that success in the parameters of emotion, energy or social status, is independent influencing factor of success in the parameter of functional status [37]. Finally, although often used and easily collected, LOS may be the only surrogate outcome of the treatment time of rehabilitation program. It might be more representative to collect the exact treatment time across the disciplines of a rehabilitation program (e.g., the total duration of therapy throughout the entire admission time) rather than the LOS. However, such an approach may be more difficult to perform in this multicenter study.
In conclusion, the results of this Thailand-based, multicenter study demonstrated that admission to an SSRF may be associated with better rehabilitation outcomes. This result addresses the importance of having SSRF in low-middle income countries, including Thailand, to improve the rehabilitation outcomes of those with SCI. Studies to identify long-term rehabilitation outcomes, such as long-term readmission rate and family burden, are required to further demonstrate the importance of SSRF.
Data archiving
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31.
Kovindha A. A retrospective study of spinal cord injuries at Maharaj Nakorn Chiang Mai Hospital during 1985–91. Chiang Mai Med Bull. 1993;32:85–92.
Myers J, Lee M, Kiratli J. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil. 2007;86:142–52.
Alexander MS, Anderson KD, Biering-Sorensen F, Blight AR, Brannon R, Bryce TN, et al. Outcome measures in spinal cord injury: recent assessments and recommendations for future directions. Spinal Cord. 2009;47:582–91.
Furlan JC, Noonan V, Singh A, Fehlings MG. Assessment of disability in patients with acute traumatic spinal cord injury: a systematic review of the literature. J Neurotrauma. 2011;28:1413–30.
Liu N, Xing H, Zhou M, Biering-Sorensen F. Lack of knowledge and training are the major obstacles in application of the Spinal Cord Independence Measure (SCIM) in China. J Spinal Cord Med. 2018;29:1–16.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K, et al. United States (US) multi-center study to assess the validity and reliability of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2011;49:880–5.
Bluvshtein V, Front L, Itzkovich M, Aidinoff E, Gelernter I, Hart J, et al. SCIM III is reliable and valid in a separate analysis for traumatic spinal cord lesions. Spinal Cord. 2011;49:292–6.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehab. 2007;29:1926–33.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM--spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6.
Itzkovich M, Tripolski M, Zeilig G, Ring H, Rosentul N, Ronen J, et al. Rasch analysis of the Catz-Itzkovich spinal cord independence measure. Spinal Cord. 2002;40:396–407.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Fromovich-Amit Y, Biering-Sorensen F, Baskov V, Juocevicius A, Hansen HV, Gelernter I, et al. Properties and outcomes of spinal rehabilitation units in four countries. Spinal Cord. 2009;47:597–603.
Tulaar AB, Karyana M, Karunia Wahyuni L, Paulus AF, Tinduh D, Anestherita F, et al. People with spinal cord injury in Indonesia. Am J Phys Med Rehabil. 2017;96(2Suppl 1):S74–77.
Engkasan JP, Hasnan N, Mohd Yusuf Y, Abdul Latif L. People with spinal cord injury in Malaysia. Am J Phys Med Rehabil. 2017;96(2Suppl 1):S90–92.
Rapidi CA, Kyriakides A. People with spinal cord injury in Greece. Am J Phys Med Rehabil. 2017;96(2Suppl 1):S71–73.
Kovindha A. People with spinal cord injury in Thailand. Am J Phys Med Rehabil. 2017;96(2Suppl 1):S120–123.
Cheng CL, Plashkes T, Shen T, Fallah N, Humphreys S, O’Connell C, et al. Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home? J Neurotrauma. 2017;34:2867–76.
New PW, Simmonds F, Stevermuer T. Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord. 2011;49:909–16.
Mahmoud H, Qannam H, Zbogar D, Mortenson B. Spinal cord injury rehabilitation in Riyadh, Saudi Arabia: time to rehabilitation admission, length of stay and functional independence. Spinal Cord. 2017;55:509–14.
Wilson JR, Grossman RG, Frankowski RF, Kiss A, Davis AM, Kulkarni AV, et al. A clinical prediction model for long-term functional outcome after traumatic spinal cord injury based on acute clinical and imaging factors. J Neurotrauma. 2012;29:2263–71.
Herzer KR, Chen Y, Heinemann AW, Gonzalez-Fernandez M. Association between time to rehabilitation and outcomes after traumatic spinal cord injury. Arch Phys Med Rehabil. 2016;97:1620–e4.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M. Effects on age on spinal cord lesion patients’ rehabilitation. Spinal Cord. 2003;41:457–64.
Furlan JC, Fehlings MG. The impact of age on mortality, impairment, and disability among adults with acute traumatic spinal cord injury. J Neurotrauma. 2009;26:1707–17.
Cifu DX, Seel RT, Kreutzer JS, McKinley WO. A multicenter investigation of age-related differences in lengths of stay, hospitalization charges, and outcomes for a matched tetraplegia sample. Arch Phys Med Rehabil. 1999;80:733–40.
Ones K, Yilmaz E, Beydogan A, Gultekin O, Caglar N. Comparison of functional results in non-traumatic and traumatic spinal cord injury. Disabil Rehab. 2007;29:1185–91.
Scivoletto G, Farchi S, Laurenza L, Molinari M. Traumatic and non-traumatic spinal cord lesions: an Italian comparison of neurological and functional outcomes. Spinal Cord. 2011;49:391–6.
Gupta A, Taly AB, Srivastava A, Vishal S, Murali T. Traumatic vs non-traumatic spinal cord lesions: comparison of neurological and functional outcome after in-patient rehabilitation. Spinal Cord. 2008;46:482–7.
DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International spinal cord injury core data set. Spinal Cord. 2006;44:535–40.
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International spinal cord injury core data set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
Scivoletto G, Tamburella F, Laurenza L, Molinari M. The spinal cord independence measure: how much change is clinically significant for spinal cord injury subjects. Disabil Rehab. 2013;35:1808–13.
Karamehmetoglu SS, Karacan I, Elbasi N, Demirel G, Koyuncu H, Dosoglu M. The functional independence measure in spinal cord injured patients: comparison of questioning with observational rating. Spinal Cord. 1997;35:22–5.
Eastwood EA, Hagglund KJ, Ragnarsson KT, Gordon WA, Marino RJ. Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury—1990–1997. Arch Phys Med Rehabil. 1999;80:1457–63.
Srisuppaphon D. Spinal cord injury rehabilitation service system: notes from the 16th ASCoN conference and the proposal for Thai system development. J Thai Rehabil Med. 2018;28:2–3.
Nam HS, Kim KD, Shin HI. ICF-based comprehensive evaluation for post-acute spinal cord injury. Ann Rehabil Med. 2012;36:804–14.
Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745.
Thietje R, Giese R, Kaphengst C, Runde P, Schulz AP. Parameters for positive outcome of the in-hospital rehabilitation of spinal cord lesion patients: the Boberg Quality Score. Spinal Cord. 2010;48:537–41.
Acknowledgements
We would like to thank Faculty of Medicine Chiang Mai University, Sirindhorn National Medical Rehabilitation Institute, Ratchaburi Hospital and Faculty of Medicine Siriraj Hospital Mahidol University for supporting data collections of this study.
Author information
Authors and Affiliations
Contributions
SP was responsible for designing the research question, collecting and analyzing the data, drafting the manuscript and writing the final version of the manuscript. NK, RM, CC, and PK were responsible for designing the research question, collecting the data and commenting on the final version of the manuscript. AK was responsible for designing the research question, collecting and analyzing the data and commenting on the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study protocol was approved by the Institutional Ethics Committee of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand and was in accordance with the current version of the Helsinki Declaration. The research ID is 2880 and the study code is REH-2558–02880. The study was also approved by the local Ethics Committee of Sirindhorn National Medical Rehabilitation Institute, Ratchaburi Hospital and Faculty of Medicine Siriraj Hospital Mahidol University. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during all course of this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pattanakuhar, S., Kammuang-lue, P., Kovindha, A. et al. Is admission to an SCI specialized rehabilitation facility associated with better functional outcomes? Analysis of data from the Thai Spinal Cord Injury Registry. Spinal Cord 57, 684–691 (2019). https://doi.org/10.1038/s41393-019-0267-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0267-3
This article is cited by
-
Minimal clinically important difference (MCID) and minimal detectable change (MDC) of Spinal Cord Ability Ruler (SCAR)
Spinal Cord (2023)
-
Performance of the Dutch clinical prediction rule for the ambulation outcome after spinal cord injury in a middle-income country clinical setting: an external validation study in the Thai retrospective cohort
Spinal Cord (2023)
-
Standard set of network outcomes for traumatic spinal cord injury: a consensus-based approach using the Delphi method
Spinal Cord (2022)
-
Health care and rehabilitation services utilization, benefits and satisfaction: a community survey of individuals with spinal cord injury in Thailand
Spinal Cord (2022)