Abstract
Study Design
Retrospective chart review.
Objectives
The objective of this study is to evaluate the efficacy of nonsteroidal anti-inflammatory drug (NSAID) prophylaxis for heterotopic ossification (HO) in the acute phase after spinal cord injury (SCI).
Setting
Acute rehabilitation hospital in California, USA.
Methods
This retrospective chart review (October 2013–March 2017) included individuals with motor complete SCI followed by the SCI service within 60 days of injury. Group demographics and HO diagnosis were compared in those who received and those who did not receive NSAID prophylaxis. A backward stepwise multiple regression was employed to assess the predictive association between injury characteristics and HO prophylaxis on HO diagnosis.
Results
A total of 108 AIS A and B cases were included, and 27 received ≥ 15 days of therapy (overall range 6–44 days). Logistic regression analysis revealed those who received ≥ 15 days of NSAID prophylaxis had an odds ratio of 0.1 of being diagnosed with HO compared with those who did not (95% CI, 0.02 to 0.52). Significant predictors of HO diagnosis were tracheostomy (OR 2.8, 95% CI, 1.05 to 7.5), urinary tract infection (OR 4.3, 95% CI, 1.5 to 12.2), and pressure injury (OR 3.3, 95% CI, 1.1 to 9.5). Adverse effects of NSAID use were minimal.
Conclusions
NSAID prophylaxis appears to help prevent HO development during the acute phase after SCI. Prospective study with prolonged follow up is necessary to confirm the long-term efficacy of HO prevention and to further evaluate safety following spinal fusion.
Sponsorship
None.
Similar content being viewed by others
Introduction
Clinically significant heterotopic ossification (HO) occurs in 20–30% of people following spinal cord injury (SCI) [1]. Manifestations of HO can range from mild to functionally debilitating. The time-consuming diagnostic work-up and effects of HO (loss of range of motion (ROM), fevers, pain, spasticity, and edema) may challenge SCI rehabilitation [2]. Medical management with a bisphosphonate is recognized as a mainstay of HO treatment to arrest the extra-articular bone formation, but these medications have a variety of known side effects and carry a teratogenic potential [3]. In advanced cases of HO with severe loss of joint motion, surgical excision of the heterotopic bone may be the only option to restore function. Although outcomes are generally good, surgery carries a high risk of infection, blood loss, and/or fracture, and post-operative recurrence is possible [4, 5]. Given this, prevention of HO should be a clinical priority among SCI providers.
Non-steroidal anti-inflammatory drugs (NSAIDs) have been recognized as effective prophylaxis for HO after total hip arthroplasty (THA) for over 30 years [6]. A recent meta-analysis revealed that both selective and non-selective NSAIDs effectively decrease HO after THA [7]. In two prior randomized controlled studies, Banovac et al. [8, 9] demonstrated the effectiveness of indomethacin and rofecoxib as primary HO prophylaxis in individuals with SCI. Despite these studies, our survey of SCI physicians at 13 American SCI centers revealed NSAID prophylaxis is not routinely being implemented. In addition, there have been no further published reports confirming the effectiveness of NSAIDs for primary HO prevention in the SCI population and there has specifically been no published work on the use of COX-2-selective inhibitors, as rofecoxib was taken off the market in late 2004. Overall, it appears there is no consensus regarding the use of NSAIDs for primary HO prevention after SCI.
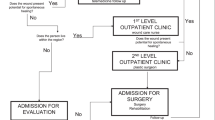
After a review of the available evidence and discussion with our local trauma and spine surgery colleagues, the SCI providers at our acute rehabilitation center instituted a formal HO prophylaxis protocol in August 2015. Even before this time, certain providers were routinely prescribing NSAID HO prophylaxis to people with traumatic motor complete SCI during acute rehabilitation. Given the limited published evidence regarding the effectiveness of primary HO prophylaxis in the SCI population and the mixed practice pattern among national and local SCI providers, we felt that a renewed evaluation of this question was warranted. In the current work, we sought to evaluate the effectiveness of NSAIDs for primary HO prevention at our center and investigate the predictive relationship between clinical comorbidities and HO diagnosis. We also explored adverse events associated with NSAID use.
Methods
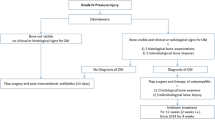
After obtaining approval from our institutional review board, we performed a retrospective chart review of all patients consecutively admitted to the SCI acute rehabilitation program at Santa Clara Valley Medical Center between October 2013 and March 2017. Chart review included admission history and physical notes, progress notes, laboratory data, imaging results, medication administration record, and discharge notes. We reviewed the charts of patients with motor complete SCI (AIS A or B) given prior literature showing an increased prevalence of HO in motor complete SCI [1]. We defined a case of HO as any patient who was diagnosed and started on treatment specifically for HO, including bisphosphonate therapy, unless contraindicated.
Although our institutional HO prophylaxis guideline recommends 4 weeks of prophylaxis (indomethacin 75 mg sustained release once daily or 25 mg immediate release three times daily, or celecoxib 200 mg once daily), we encountered a range of actual treatment durations in our chart review. For our statistical analyses, we designated a patient as having received an adequate course of NSAID prophylaxis if they were explicitly given an NSAID for the purposes of preventing HO for at least 15 days. The minimum duration of NSAID prophylactic therapy required for optimal prophylactic effect after SCI has never been defined; thus, we chose a duration of ≥ 15 days based on evidence from a combination of SCI and hip replacement literature. Banovac’s NSAID prophylaxis protocols required 3 weeks of indomethacin or 4 weeks of rofecoxib [8, 9], whereas post-hip replacement NSAID prophylaxis protocols range from 7 to 15 days of therapy [10,11,12,13].
Our institutional guidelines recommend the initiation of NSAID prophylaxis at 3–4 weeks after SCI. Banovac initiated his NSAID prophylaxis protocol at 20 ± 14 days (indomethacin) and 25 ± 7 days (rofecoxib) after injury [8, 9]. For this study we noted the time to NSAID initiation but did not specify a required time period for NSAID initiation. We only included individuals who received care from an SCI physician within 60 days of injury to avoid confounders of prolonged non-specialized care and given natural time course of HO development.
We also collected information on possible confounding variables including age, gender, etiology of injury, level of injury, presence of long bone fractures, tracheostomy and ventilation status, the presence of intramuscular bleeding, the presence of spasticity, and diagnosis of pneumonia, urinary tract infection (UTI), or pressure injury. We noted the use of medications that may have an effect on HO formation including warfarin, statins and bisphosphonates used for purposes other than HO treatment. Lastly, we collected possible associated outcome data including inpatient rehabilitation length of stay and adverse event data including rates of bony non-union and gastrointestinal (GI) bleeding.
Statistical analysis
Group demographics were analyzed using χ2-test and Fisher’s exact test (categorical variables), as well as t-test (continuous variables) were used as appropriate (Tables 1–3). Backward stepwise multiple regression was employed to investigate the role of injury characteristics and HO prophylaxis (independent variables) on HO diagnosis (dependent variable; Table 4). The backward stepwise logistic regression was run on SPSS and used the default setting of 20 iterations, probability cutoff of 0.5, and variable entry p = 0.05 and exclusion p = 0.1.
Results
Group demographics
One hundred and twenty people with motor complete (AIS A or B) SCI were admitted to our Acute Rehabilitation Center Unit (ARU) between October 2013 and March 2017, of whom 108 were included in our analysis. Two patient charts were excluded given uncertainty about HO diagnosis despite review by multiple physician authors (EZ, JC, SY), and 10 charts were excluded as the patients were not followed by the SCI service until > 60 days after their date of injury. Included patients were first seen by the SCI service an average of 21 days from injury (range 0–58 days). They were followed for an average of 63 days since the date of injury (19–143 days).
Thirty-six individuals were explicitly started on prophylaxis for HO (overall range 6–44 days); 10 received ≥ 28 days of therapy, an additional 17 individuals (total 27) received ≥ 15 days of therapy, and 9 individuals received < 15 days of therapy. Of the 27 individuals to receive ≥ 15 days of therapy, all courses of NSAID prophylaxis were initiated during acute rehabilitation (mean 34 days after injury; range 11–75 days). When comparing the baseline characteristics of those who did and did not receive NSAIDs (Table 1), we noted NSAIDs were more often prescribed to those with an AIS A injury (p = 0.03) or sport-related injury (p = 0.01). Providers also seemed to favor prophylaxis in younger patients, but this was not statistically significant (p = 0.09).
Among the nine patients who received < 15 days of HO prophylaxis, prophylaxis was stopped in three cases when HO treatment was initiated following diagnosis of HO. In two cases, NSAIDs were stopped due to hematoma and hematuria, which were attributed to different causes but believed to be at risk of worsening with NSAID use. Two NSAID courses were stopped early at the time of transfer to a higher level of care for clinical deterioration unrelated to bleeding or renal issues, and the remaining two prophylactic treatment courses were stopped early for unknown reasons. Indomethacin was used as prophylaxis in 23 cases, celecoxib was used in 3 cases, and 1 individual was on an initial course of ibuprofen converted to celecoxib.
HO diagnosis
Thirty-one individuals were diagnosed with HO in a total of 46 joints an average of 48 days from injury (14–94 days). HO was diagnosed in the hip in 30 individuals (6 right, 10 left, 14 bilateral) and there was one case of bilateral knee HO. Presenting symptoms of HO included loss of ROM (n = 15), pain (n = 2), edema (n = 7), warmth (n = 1), fever (n = 5), autonomic dysreflexia (n = 2), and increased spasticity (n = 1). In four cases, there were no symptoms documented; instead, imaging was pursued based on abnormal laboratory findings. HO was confirmed by imaging in 27 of 31 cases (23 by triple-phase bone scan, 1 by computed tomography, 3 by X-ray). Of the four HO cases diagnosed without imaging confirmation, two had indeterminant triple phase bone scans, one had a negative X-ray, and there was no imaging in one case. We included these cases despite the lack of definite imaging confirmation as there was a strong clinical suspicion for HO documented in the chart. Furthermore, we note that imaging is imperfect in the diagnosis of HO. There was one case, e.g., where HO was strongly suspected but triple-phase bone scan was negative twice before a third scan was ultimately positive for HO approximately 1 month later.
None of the ten individuals to receive ≥ 4 weeks of NSAID prophylaxis were diagnosed with HO. Two individuals receiving ≥ 15 days of NSAID prophylaxis (24 days each) were diagnosed with HO (7.4%) compared with the 29 cases of HO diagnosed in the 81 people who did not receive prophylaxis (35.8%; Fisher’s exact test p = 0.006) (Table 2). Univariate analysis (χ2-tests) revealed individuals with HO diagnosis had higher proportions of male gender (χ2(1) = 4.7, p = 0.03), UTI (χ2(1) = 5.5, p = 0.02), pressure injury (χ2(1) = 6.8, p = 0.009), and tracheostomy (χ2(1) = 4.5, p = 0.03); Age, tetraplegia, motor complete injury, spasticity, or etiology of injury were not significantly different from individuals not diagnosed with HO (Table 3). ARU length of stay was notably longer in those who were diagnosed with HO (mean = 36.6, SD = 14.2) compared with individuals not diagnosed with HO (mean = 30.0, SD = 10.1; t(106) = 2.7, p = 0.008).
One of five individuals to receive warfarin during their ARU stay was diagnosed with HO. One of seven individuals to receive statin therapy during their ARU stay was diagnosed with HO. Two individuals received bisphosphonate therapy for hypercalcemia during their stay; however, these two individuals also received NSAID prophylaxis for HO and neither was diagnosed with HO.
Backward stepwise logistic regression
A backward stepwise logistic regression was employed to investigate the role of injury characteristics and HO prophylaxis (independent variables) on HO diagnosis (dependent variable) (Table 4). The injury characteristics entered in the initial model included tetraplegia, AIS A, long bone fracture at injury, any intramuscular bleeding, pressure injury during hospitalization, UTI during hospitalization, presences of spasticity requiring medication at discharge, tracheostomy, NSAID prophylaxis ≥ 15 days. Of note, presence of a tracheostomy was not independent from mechanical ventilation and diagnosis of pneumonia; thus, we did not individually analyze the association between pneumonia or mechanical ventilation with HO. The final model was achieved after 6 steps (Omnibus test: χ2 (4) = 27, p < .001; Cox and Snell R2 = 0.222; Nagelkerke R2 = 0.317). The final model included tracheostomy (odds ratio (OR) 2.8, 95% confidence interval (CI) 1.1 to 7.5, p = 0.039), pressure injury during hospitalization (OR 3.3, 95% CI 1.1 to 9.5, p = 0.030), UTI during hospitalization (OR 4.3, 95% CI 1.5 to 12, p = 0.006), and NSAID prophylaxis greater than 15 days (OR 0.1, 95% CI 0.02 to .52, p = 0.006); in addition, the intercept was significant (p < 0.001).
Adverse effects of NSAIDs
No adverse events related to NSAID use were documented as such by the treating clinicians; however, NSAIDs were stopped in the context of concurrent hemoptysis (n = 1 ventilated patient with pneumonia), acute kidney injury (n = 3), hematuria (n = 2), GI upset (n = 4), and bloody stool (n = 1). There were no known cases of spine bony nonunion in our patient sample, but most people were discharged before neurosurgical follow-up and clearance of spinal orthoses. There was notably one case of long bone fracture nonunion in a patient who did not receive NSAIDs. There were no cases of hemodynamically significant lower GI bleed and only one case of upper GI bleed in our sample, which occurred in someone who was not treated with any NSAIDs.
Discussion
Secondary medical complications after SCI are numerous and only exacerbate the already tumultuous transition to life with severe neurologic injury. Prevention and management of these secondary complications is a continual challenge for individuals with SCI, their caregivers, and their clinical providers. Although symptomatic HO does not occur in all cases of SCI, the effects can be devastating for those who are affected. The effectiveness of NSAIDs to prevent HO after THA is well-established in the literature and, as such, NSAIDs are routinely used as prophylaxis in high risk cases. In two randomized controlled trials in 2001 and 2004, Banovac et al. [8, 9] reported a decrease in the incidence of HO diagnosis of approximately 20% and 40% with the use of NSAIDs for HO prophylaxis, respectively. In this retrospective review, we also note a protective effect of NSAID prophylaxis with a similar decrease in the incidence of HO of 28%.
Similar to prior reports, individuals in our sample with tracheostomy, UTI, and pressure injury were more likely to be diagnosed with HO [14,15,16], and individuals with peri-conal injuries were less likely to develop HO [1]. The average time to HO diagnosis, age of onset, and location of HO (predominantly hip) also corroborate the existing literature [1,2,3, 16]. Unlike in prior literature [14,15,16,17,18], spasticity was not a statistically significant predictor of HO in our study. This finding may reflect the definition of spasticity used in our study, which required prescription of an antispasticity medication at the time of rehabilitation discharge. Regarding safety, we did not find definite evidence that NSAID prophylaxis resulted in an increase in adverse outcomes; however, follow-up was too limited in this study to definitively comment on the potential for spinal nonunion. Finally, length of stay was longer in those with an HO diagnosis. This may relate to other covariates such as pressure injury and UTI. Nonetheless, prevention of HO may facilitate a more time-efficient rehabilitation course.
Limitations
The primary limitation of this study is the non-random, non-blinded decision to give HO prophylaxis to some individuals and not to others. We did attempt to extract the rationale for holding therapy among the 72 individuals who did not receive any NSAID prophylaxis, but explicit reasoning was only documented in six charts. These reasons included: restrictions by neurosurgery (n = 2), concern about renal function (n = 2), a history of significant GI bleeding (n = 1), NSAID intolerance (n = 1), and the presence of HO symptoms at the time of admission necessitating treatment rather than prophylaxis (n = 1). Overall, there are two presumed primary explanations for the variable use of NSAID prophylaxis in our study sample: date of admission and practice variations among different SCI providers. Our ARU instituted evidence-based practice guidelines in August of 2015, which recommend the use of NSAID prophylaxis for HO prevention after SCI. However, this practice has not yet been incorporated into admission order sets or other opt-out decision pathways. Prior to this recommendation, certain providers more routinely used HO prophylaxis than others based on individual training and practice style. Even after the introductions of the guidelines, many individuals still did not receive NSAID prophylaxis. In general, we assume that HO prophylaxis was more likely to be considered and used in those whom the SCI provider felt to be at highest risk of developing HO. Indeed, had NSAIDs use been random, we may have actually found a stronger prophylactic effect.
Another important limitation of our study is our limited follow-up duration. Patients were followed until a mean of 63 days after the date of injury (19–143 days); however, we know that HO may be diagnosed later than this. Indeed, even in our sample, six patients were diagnosed with HO later than 63 days after injury. We were unable to account for the possibility of HO formation after ARU discharge in all patients and therefore focused our analysis on HO diagnosis that was made during the ARU stay. Of the 77 individuals who were not diagnosed with HO before ARU discharge, 33 were followed at least once in our center’s outpatient SCI clinic (the remainder having presumably been followed elsewhere). Of these, one individual was later diagnosed with symptomatic HO, one individual had an incidental finding of HO on X-ray imaging, and one individual had symptoms suggestive of HO but never underwent the recommended confirmatory imaging. The first two of these patients were notably treated with ≥ 15 days of HO NSAID prophylaxis during their inpatient ARU stay. This could suggest HO formation is delayed but not prevented in people who receive NSAID prophylaxis.
Finally, as a retrospective analysis, our study could not control for all differences in patient care. For example, there are multiple reasons why someone might be treated with an NSAID during acute rehabilitation besides HO prophylaxis or treatment. Indeed, there were 30 patients in our sample that had non-HO related NSAID prescriptions during their ARU stay (scheduled or PRN). Although these prescriptions may confound our results, it should be noted that there were only 10 people to receive scheduled NSAIDs who did not otherwise receive NSAID HO prophylaxis (mean 11 days, range 5–25 days). Only one of these individuals was diagnosed with HO after receiving only 6 days of scheduled Ibuprofen. Importantly, none of the three individuals who received 15 or more days of non-HO-related NSAIDs were diagnosed with HO, which further supports our overall conclusion that NSAIDs are likely protective against HO formation.
Conclusions
Our retrospective study shows a drop in the rate of HO by 28.4% with NSAID prophylaxis for ≥ 15 days in the acute rehabilitation period after SCI. As a retrospective analysis, we cannot draw definite conclusions about causation. Nonetheless, we think that the findings of this study, in the context of prior work, support the need for a large, prospective study on NSAID prophylaxis for HO. Future prospective studies must include sufficient follow-up to tackle the remaining questions surrounding possible delayed HO formation and the effects of NSAID therapy on spinal fusion. Further studies may also help delineate the best NSAID class or medication choice, dose, and the optimal timing and duration of therapy to optimize prophylactic potential, while minimizing adverse effects.
References
Van Kuijk AA, Geurts ACH, van Kuppevelt HJM. Neurogenic heterotopic ossification in spinal cord injury. Spinal Cord. 2002;40:313–26.
Brady RD, Shultz SR, McDonald SJ, O’Brien TJ. Neurological heterotopic ossification: Current understanding and future directions. Bone . 2018;109:35–42.
Teasell RW, Mehta S, Aubut JL, Ashe MC, Sequeira K, Macaluso S, et al. A systematic review of the therapeutic interventions for heterotopic ossification after spinal cord injury. Spinal Cord. 2010;48:512–21.
Gatin L, Genet F, Dihn A, Denormandie P. Postoperative infections after excision of neurogenic heterotopic ossification at the hip: risk factors and causative organisms. Ortho Trauma Surg Res. 2017;103:357–61.
Denormandie P, de l’Escalopier N, Gatin L, Grelier A, Genet F. Resection of neurogenic heterotopic ossification (NHO) of the hip. Orthop Traumatol Surg Res. 2018;104(1S):S121–S127.
Eyb R, Knahr K. The effect of prophylaxis for thrombosis on heterotopic ossification following total hip joint replacement. Arch Orthop Trauma Surg. 1983;102:114–7.
Joice M, Vasileiadis GI, Amanatullah DF. Non-steroidal anti-inflammatory drugs for heterotopic ossification prophylaxis after total hip arthroplasty. Bone Joint J. 2018;100-B:915–22.
Banovac K, Williams JM, Patrick LD, Haniff YM. Prevention of heterotopic ossification after spinal cord injury with indomethacin. Spinal Cord. 2001;39:370–4.
Banovac K, Williams JM, Patrick LD, Levi A. Prevention of heterotopic ossification after spinal cord injury with COX-2 selective inhibitor (rofecoxib). Spinal Cord. 2004;42:707–10.
Pakos EE, Tsekeris PG, Paschos NK, Pitouli EJ, Motsis EK, Xenakis TA. The role of radiation dose in a combined therapeutic protocol for the prevention of heterotopic ossification after total hip replacement. J BUON. 2010;15:74–8.
Pakos EE, Stafilas KS, Politis AN, Tsekeris PG, Mitsionis G, Xenakis TA. Heterotopic ossification after total hip arthroplasty (THA) in congenital hip disease: comparison of two different prophylactic protocols. Clin Transl Oncol. 2009;11:103–8.
van der Heide HJ, Rijnberg WJ, van Sorge A, van Kampen A, Schreurs BW. Similar effects of rofecoxib and indomethacin on the incidence of heterotopic ossification after hip arthroplasty. Acta Orthop. 2007;78:90–4.
van der Heide HJ, Koorevaar RT, Schreurs BW, van Kampen A, Lemmens A. Indomethacin for 3 days is not effective as prophylaxis for heterotopic ossification after primary total hip arthroplasty. J Arthroplast. 1999;14:796–9.
Citak M, Suero EM, Backhaus M, Aach M, Godry H, Meindl R, et al. Risk factors for heterotopic ossification in patients with spinal cord injury: a case-control study of 264 patients. Spine. 2012;37:1953–7.
Kedlaya D, Nazir C. Heterotopic ossification with normal serum alkaline phosphatase levels: a case series. Arch Phys Med Rehabil. 2005;86:E44.
Wittenberg RH, Peschke U, Botel U. Heterotopic ossification after spinal cord injury. Epidemiology and risk factors. J Bone Jt Surg Br. 1992;74:215–8.
Lal S, Hamilton BB, Heinemann A, Betts HB. Risk factors for heterotopic ossification in spinal cord injury. Arch Phys Med Rehabil. 1989;70:387–90.
Coelho CV, Beraldo PS. Risk factors of heterotopic ossification in traumatic spinal cord injury. Arq Neuropsiquiatr. 2009;67(2B):382–7.
Acknowledgements
None
Author contributions
EZ was responsible for designing the study, writing the protocol, conducting the chart review/data extraction, analyzing data, interpreting results, primary writing of the report, and creating reference lists. SY assisted with chart review/data extraction and contributed to writing and editing the report and reference list. BD conducted the statistical analyses and contributed to writing and editing the report. BTP provided feedback on the protocol and report. JC assisted with chart review/data extraction and contributed to writing and editing the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zakrasek, E.C., Yurkiewicz, S., Dirlikov, B. et al. Use of nonsteroidal anti-inflammatory drugs to prevent heterotopic ossification after spinal cord injury: a retrospective chart review. Spinal Cord 57, 214–220 (2019). https://doi.org/10.1038/s41393-018-0199-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0199-3
This article is cited by
-
When the Nervous System Turns Skeletal Muscles into Bones: How to Solve the Conundrum of Neurogenic Heterotopic Ossification
Current Osteoporosis Reports (2020)
-
Heterotopic Ossification After Spinal Cord Injury: Current Clinical Approaches
Current Physical Medicine and Rehabilitation Reports (2020)