Abstract
Study design
Multicentre cross-sectional study.
Objectives
To describe relationships between time since injury (TSI) and participation in individuals with tetraplegia and paraplegia.
Setting
Community sample from the Netherlands
Methods
Individuals (N = 265) aged 28–65 years, living with spinal cord injury (SCI) for ≥10 years, age at injury between 18–35 years and using a wheelchair for everyday mobility in three TSI strata: 10–19, 20–29, and ≥30 years post-injury. The Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-Participation) was used, which consists of three scales: Frequency (including subscales for Productive, Leisure, and Social activities), Restrictions, and Satisfaction. Linear regression analyses were used to study the effect of TSI on participation, and to adjust for personal and lesion characteristics, for individuals with tetraplegia and paraplegia separately.
Results
Mean age was 48.4 years, with a mean TSI of 24 years. About 73.6% were male, 40.4% had tetraplegia and 81.9% had a motor complete injury. In individuals with tetraplegia (N = 107), longer TSI was independently associated with lower scores on the Frequency scale (p = 0.025) and the subscale frequency of Leisure activities (p = 0.004). In individuals with paraplegia (N = 158), longer TSI was independently associated with lower scores on the subscale frequency of Productive activities (p = 0.006). TSI was not associated with participation Restrictions and Satisfaction with participation.
Conclusions
Longer TSI is associated with a reduced frequency of participation in individuals with long-term SCI. Interestingly, this negative association is not accompanied by a similar association in the person’s experience of participation.
Similar content being viewed by others
Introduction
Life expectancy in individuals with spinal cord injury (SCI) has increased because of specialized medical care [1]. Therefore, research into the quality of living with SCI has gained importance [2]. Participation is related to higher life satisfaction [3], and even stronger related to quality of life than impairment or disability [4]. Therefore, participation is an important outcome measure in rehabilitation medicine.
Participation can be measured in objective terms, for example, in how many hours a week a person performs paid work or how often he meets friends. In addition, subjective participation can be measured in terms of levels of satisfaction with participation or experienced restrictions when participating in society. Studies on participation after SCI showed less than optimal levels of participation [5,6,7]. A frequently used questionnaire to measure objective participation is the Craig Handicap Assessment and Reporting Technique (CHART), in which the maximum score of all domains is 100, which reflects the level of performance typical of the average non-disabled person [8]. When analyzing data from 350 individuals with SCI (mean TSI 21 years) from Germany, the UK, Austria, and Switzerland [9], similar CHART scores were found on Physical Independence, Mobility, Occupation, Social Integration, and Economic Self-sufficiency as in other studies evaluating participation in people with chronic SCI [10,11,12,13]. In a cross-sectional study, CHART scores in individuals 1–2 years post-injury were significantly lower than in individuals with longer duration of injury [14]. Subjective participation assessed with the Impact on Participation and Autonomy questionnaire (IPA) was described in 161 individuals with SCI with TSI ranging from 1–58 years. The majority of the respondents reported one or more severe problems with participation. Insufficient perceived participation was reported mostly in the domains of family life, autonomy outdoors, work, and education [6]. Even though participation was expected to decline with time [15], this association was found in only one out of five cross-sectional studies [14].
Available longitudinal studies showed diverging evidence on the course of participation over time [5]. Participation was evaluated with the CHART at three year intervals from 1990 to 1999 in a longitudinal study among individuals with SCI for more than 20 years at baseline [16]. Over a period of 10 years, a significant, but subtle, decline was found in terms of Physical Independence, Mobility, and Occupation, whereas Economic Self-sufficiency significantly increased over time. Another longitudinal study in which participation was measured by the Community Integration Measure (CIM), showed a significant increase with TSI in bi-variable analyses, but not in multivariable analyses with adjustment for level of injury, income level, and living situation [17].
Regarding factors influencing participation, several studies found associations between participation and demographic factors such as age and years of education [18]. Further, individuals with higher levels of injury were more likely to report lower participation [16, 19] or experienced severe problems with participation more often [6]. In a study among 3835 individuals with SCI, lesion level was a highly significant determinant of all CHART dimensions except Economic Self-sufficiency, with complete high tetraplegia (C1–C4) having the largest negative impact on CHART scores [14]. Because of the strong associations between level of injury and levels of participation, it could be useful to analyze associations between TSI and participation in individuals with tetraplegia or paraplegia separately. None of the before-mentioned cross-sectional studies on objective and subjective participation tested for interactions between level of injury and TSI.
In conclusion, at this moment diverging evidence exists on the effect of TSI on participation in individuals with long-term SCI (>10 years) specifically, urging for more research on participation in this group [5]. Furthermore, objective and subjective participation are rarely measured simultaneously, and, if so, using different instruments, which hampers a comparison between objective and subjective participation [20]. To improve rehabilitation care of people with long-term SCI, it is important to get more insight in the effect of TSI on participation of people with long-term SCI. Therefore, the objective of this study was to determine the effect of TSI in individuals with tetraplegia and paraplegia on objective and subjective participation measured by the same instrument. The hypothesis is that TSI is related to participation, and that TSI has more effect on participation in people with tetraplegia compared to those with paraplegia.
Methods
Participants
Data used in this study were collected as part of the multicentre ALLRISC study (Active LifestyLe Rehabilitation Interventions in aging Spinal Cord injury) [21]. Inclusion criteria were: SCI; age at injury between 18 and 35 years; TSI 10 years or longer; current age between 28 and 65 years; using a wheelchair at least for longer distances (>500 m; electric or hand-rim propelled). Exclusion criteria were: insufficient mastery of the Dutch language to respond to an oral interview or to understand test instructions.
Strata of TSI were 10 to 19, 20 to 29, and 30 years or more after SCI. It was aimed to include 100 participants per stratum.
Procedures
Individuals with long-term SCI were identified from all eight rehabilitation centers with a SCI unit in the Netherlands. TSI stratification took place per center. Data were collected between November 2011 and February 2014. A total of 566 persons were invited to participate in the study, 292 of whom were ultimately included. A large travel distance, unwillingness, too busy with daily life, and health issues were the main reasons for non-participation. After the inclusion procedure, 10 participants were excluded from the analyses because of not meeting all the inclusion criteria. Participants were invited for a one-day visit to the rehabilitation center. This visit included a neurological assessment in accordance with the International Standards for the Neurological Classification of Spinal Cord Injury (ISNCSCI) conducted by a physician. Participants were also asked to complete a self-report questionnaire in advance, which could be completed digitally, as well as on paper.
The study protocol was approved by the Medical Ethics Committee of the University Medical Center Utrecht. All participants completed written informed consent.
Instruments
Demographic variables were gender, age, education and relationship (married or steady relationship vs. single). Education was classified as: low (no education to vocational education) and high (completed high school to bachelor/master).
Injury characteristics were TSI, level of injury (categorized as tetraplegia (defined as a lesion at or above the T1 segment), or paraplegia (lesion lower than T1)), and completeness of injury (categorized as motor complete (Abbreviated Injury Scale (AIS) grade A or B) or motor incomplete (AIS grade C or D)).
Participation was measured using the Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-Participation) that was part of the self-report questionnaire. This instrument measures three aspects of participation: Frequency (11 items), experienced Restrictions (11 items), and Satisfaction with participation (10 items). The sum of scores of the Frequency, Restrictions, and Satisfaction scales are based on the items that are applicable to the person’s situation and each sum score is converted to a 0–100 scale, higher scores reflect more favorable participation (higher frequency, fewer restrictions, and higher satisfaction). There is no USER-Participation total score. Only participants with no missing data on one of the USER-Participation items were included in the analyses. The USER-Participation showed generally satisfactory psychometric properties in Dutch individuals with long-term SCI living in the community [22], in a Swiss population [23], and in a multi-diagnostic outpatient rehabilitation population [24, 25]. To further explore different domains of participation, three subscales were computed from the USER-Participation Frequency scale: Productive activities, Leisure activities, and Social activities. These subscales were constructed in the same way the main scales of the USER-Participation were constructed by converting each sum score to a 0–100 scale with higher scores reflecting more favorable participation [26].
Statistics
Descriptive statistics were used to describe participants’ demographic and injury-related characteristics and their scores on the USER-Participation scales. To explore differences in participation between the two lesion level groups and between the three TSI strata with categorical variables, the chi-square test was used. In case of continuous variables, the independent samples t-test and one-way ANOVA with post-hoc Bonferroni were used, respectively.
To study the effect of TSI on participation with adjustments for demographic (gender, relationship, or education level) and lesion (completeness) characteristics, linear regression analyses were performed for participants with tetraplegia and paraplegia separately. Curve-estimations were performed to determine the best relationship between the USER-P (sub)scales and TSI in tetraplegia and paraplegia separately and there was no non-linear association with a better fit than linear. Due to the ceiling effect visible in the USER-P Restrictions scale, we also dichotomized the sum score of the restriction score (based on the median value) and performed a logistic regression on this outcome measure.
The dependent variables were the USER-Participation scales and TSI in years was the continuous independent variable of interest. Personal and lesion characteristics were added to each model one by one. If the regression coefficient of the independent variable changed 10% or more [27] when adding the demographic or lesion characteristic, this characteristic was added to the final model, as was previously described by Maldonado & Greenland [28]. Collinearity by adding both TSI and age to the model was checked according to the criteria described by Field [29]: correlation between age and TSI ≥ 0.8, largest variance inflation factor (VIF) > 10 or average VIF > 1, and tolerance statistic < 0.1 of the multivariate regression models. The correlation coefficient for TSI and age was 0.86 with a VIF of 1.0. All analyses were performed using IBM SPSS Statistics v. 21.0 for Windows [30].
Results
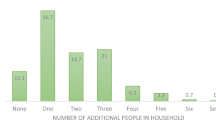
Of the 282 individuals who participated in the ALLRISC study, 265 (94%) individuals completed the online questionnaire and were included in this study. Demographics, SCI characteristics, and USER-Participation scale and subscale scores for the whole group, across TSI strata and lesion levels are displayed in Table 1. Except for age and TSI, there were no significant differences across TSI strata in demographics and lesion characteristics. Furthermore, significantly higher scores on the Frequency scale and Productive activities subscale were found in the TSI-stratum 10–19 years compared to the stratum more than 30 years since injury.
Comparison of USER-Participation scores showed lower (worse) scores for Restrictions, Satisfaction, and Productive activities, but higher scores for Social activities in individuals with tetraplegia compared to individuals with paraplegia.
Associations between time since injury and participation
Age was excluded from the regression models because of multicollinearity with TSI. The relationship between all USER-Participation scales and subscales and TSI are visualized in scatterplots (Figs. 1, 2). In individuals with tetraplegia (N = 107) longer TSI was associated with lower scores on the Frequency scale (p = 0.025) and with reduced Leisure activities (p = 0.004) (Table 2). In individuals with paraplegia (N = 158), longer TSI was associated with reduced Productive activities (p = 0.006) (Table 3). TSI was not associated with participation Restrictions (linear and logistic regression showed similar results) and Satisfaction with participation.
Discussion
TSI was significantly associated with the frequency of Leisure activities and the total Frequency scale in the group with tetraplegia. In the group of individuals with paraplegia, a significant association was found between TSI and Productive activities. TSI was not significantly associated with participation Restrictions and Satisfaction with participation.
Mean scores on the USER-Participation were similar to those found in a previous Dutch study (sharing some participants with the current study) [22] and a Swiss cross-sectional study among 1549 individuals with SCI [23], with Frequency scores of 33.3, 34.8, and 34.2, Restrictions scores of 76.5, 72.6, and 70, and Satisfaction scores of 69.6, 69.9, and 69.3, respectively. In contrast, the present study found a higher mean score (10 ± 15) on the subscale Productive Activities compared to a group of aging individuals with SCI [26]. With a higher mean age of 69 years in the latter study, this difference on Productive Activities could be attributable to retirement from paid employment.
Associations between time since injury and participation
Our results indicated a significant though subtle negative association between frequency of Leisure activities and the total Frequency scale and TSI in people with tetraplegia and between Productive activities and TSI in people with paraplegia. Except for one study [14], which in the longitudinal part but not in the cross-sectional part of the study adjusted for age, none of the other cross-sectional studies that studied this effect found an association between participation and TSI [10, 11] nor did they adjust for age.
With respect to objective participation, Charlifue et al. [16] found a similar significant subtle negative change in CHART domains Physical Independence, Mobility, and Occupation over time, adjusted for age, in a longitudinal study among 178 individuals with SCI with a mean TSI of 36 years. Only individuals younger than 65 years were included in the ALLRISC study. We might have found stronger relationships between age and participation if we would have included individuals older than 65 years of age, because decline in participation mainly takes place after the age of 65 [31]. In a longitudinal study, Whiteneck et al found higher CHART scores with longer TSI, as well as lower CHART scores with older age [14]. These contrary associations may explain the weaker than expected associations between TSI and participation in our study. Current literature on objective participation shows diverging results urging the need for further research.
In individuals with tetraplegia, longer TSI was significantly associated with reduced Leisure activities. In contrast, no significant association with TSI was found for Leisure activities in individuals with paraplegia. This difference might be explained by the finding of Gerhart et al [32], in the same study population as Charlifue [16], that individuals with cervical injuries needed additional functional assistance at a younger age than their counterparts with lower level injuries resulting in the reduced ability to perform leisure activities.
TSI was not associated with subjective participation (Restrictions and Satisfaction). Subjective participation is stronger than objective participation, influenced by psychosocial factors, such as emotional distress or depression [33, 34]. Furthermore, several studies indicated that life satisfaction does not decline or even increases with growing age in aging SCI populations [16, 35]. The underlying process is probably that people are able to adapt to varying circumstances, in this case decreasing frequency of participation and thereby maintain their levels of satisfaction with participation [36].
Implications
Apart from a subtle negative association between TSI and participation frequency, the lack of significant associations between TSI and experienced participation may be interpreted as good news. This study also confirms the usefulness of measuring both objective and subjective participation. When observing a decline in frequency of participation among individuals with long-term SCI, rehabilitation physicians could evaluate the levels of experienced restrictions and satisfaction with participation. When these are adequate, there may not be a real concern regarding the decline in objective participation over time.
Limitations
Our study design was cross-sectional, which makes it difficult to draw conclusions on associations with time. An important factor influencing participation apart from TSI is age. Because of the inclusion criteria of the ALLRISC research program with an age limitation of 65 years we were not able to completely separate the effect of age and TSI (correlation between age and TSI (r = 0.862)). However, because we expected a decline in participation to happen mainly over the age of 65, we believe that the associations we found are mainly due to TSI instead of age. Because of the inclusion criteria our study sample does not reflect the general SCI population. Unfortunately, the information on the sampling frame and non-responders per center was incomplete and, therefore, the degree of possible response bias is unknown.
Conclusion
Longer TSI is associated with a reduced frequency of participation in individuals with long-term SCI. Interestingly, this negative change is not accompanied by a similar change in the person’s experience of participation, which could be explained by other psychosocial factors such as emotional distress or depression.
References
Savic G, DeVivo MJ, Frankel HL, Jamous MA, Soni BM, Charlifue S, Long-term survival after traumatic spinal cord injury: a 70-year British study. Spinal Cord. 2017;55:651–8.
Post MWM, van Leeuwen CMC. Psychosocial issues in spinal cord injury: a review. Spinal Cord. 2012;50:382–9. https://doi.org/10.1038/sc.2011.182.
Van Leeuwen CM, Post MW, Westers P, Van Der Woude LH, De Groot S, Sluis T, et al. Relationships between activities, participation, personal factors, mental health, and life satisfaction in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93:82–9.
Dijkers M. Quality of life after spinal cord injury: a meta analysis of the effects of disablement components. Spinal Cord. 1997;35:829–40.
Barclay L, McDonald R, Lentin P. Social and community participation following spinal cord injury. Int J Rehabil Res. 2015;38:1–19.
Lund ML, Nordlund A, Nygård L, Lexell J, Bernspång B. Perceptions of participation and predictors of perceived problems with participation in persons with spinal cord injury. J Rehabil Med. 2005;37:3–8.
Schönherr MC, Groothoff JW, Mulder GA, Eisma WH. Participation and satisfaction after spinal cord injury: results of a vocational and leisure outcome study. Spinal Cord. 2005;43:241–8.
Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil. 1992;73:519–26.
Kennedy P, Lude P, Taylor N. Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord. 2006;44:95–105.
Mccoll Ma, Charlifue S, Glass C, Savic G, Meehan M. International differences in ageing and spinal cord injury. Spinal Cord. 2002;40:128–36.
Dijkers MPM, Yavuzer G, Ergin S, Weitzenkamp D, Whiteneck GG. A tale of two countries: environmental impacts on social participation after spinal cord injury. Spinal Cord. 2002;40:351–62.
Ballinger DA, Rintala DH, Hart KA. The relation of shoulder pain and range-of-motion problems to functional limitations, disability, and perceived health of men with spinal cord injury: A multifaceted longitudinal study. Arch Phys Med Rehabil. 2000;81:1575–81.
Johnston M, Nissim EN, Wood K, Hwang K, Tulsky D. Objective and subjective handicap following spinal cord injury: interrelationships and predictors. J Spinal Cord Med. 2002;25:11–25.
Whiteneck G, Tate D, Charlifue S. Predicting community reintegration after spinal cord injury from demographic and injury characteristics. Arch Phys Med Rehabil. 1999;80:1485–91.
Desrosiers J, Noreau L, Rochette A. Social participation of older adults in Quebec. Aging Clin Exp Res. 2004;16:406–12.
Charlifue S, Gerhart K. Community integration in spinal cord injury of long duration. NeuroRehabilitation. 2004;19:91–101.
Pershouse KJ, Barker RN, Kendall MB, Buettner PG, Kuipers P, Schuurs SB, et al. Investigating changes in quality of life and function along the lifespan for people with spinal cord injury. Arch Phys Med Rehabil. 2012;93:413–9. https://doi.org/10.1016/j.apmr.2011.10.014.
Craig A, Nicholson Perry K, Guest R, Tran Y, Middleton J. Adjustment following chronic spinal cord injury: determining factors that contribute to social participation. Br J Health Psychol. 2015;20:807–23.
Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB, et al. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1793–803.
Suttiwong J, Vongsirinavarat M, Chaiyawat P, Vachalathiti R. Predicting community participation after spinal cord injury in Thailand. J Rehabil Med. 2015;47:325–9.
van der Woude LHV, de Groot S, Postema K, Bussmann JBJ, Janssen TWJ, Post MWM. Active LifestyLe Rehabilitation Interventions in aging Spinal Cord injury (ALLRISC): a multicentre research program. Disabil Rehabil. 2013;35:1097–103.
Van Der Zee CH, Post MW, Brinkhof MW, Wagenaar RC. Comparison of the Utrecht scale for evaluation of rehabilitation-participation with the ICF measure of participation and activities screener and the WHO disability assessment schedule ii in persons with spinal cord injury. Arch Phys Med Rehabil. 2014;95:87–93.
Mader L, Post MWM, Ballert CS, Michel G, Stucki G, Brinkhof MWG. Metric properties of the utrecht scale for evaluation of rehabilitation-participation (user-participation) in persons with spinal cord injury living in Switzerland. J Rehabil Med. 2016;48:165–74.
Post MWM, Van Der Zee CH, Hennink J, Schafrat CG, Visser-Meily JM, Berlekom SB. Validity of the Utrecht Scale for evaluation of rehabilitation-participation. Disabil Rehabil. 2012;34:478–85.
Van Der Zee CH, Priesterbach AR, Van Dussen Der L, Kap A, Schepers VPM, Visser-Meily JMA, et al. Reproducibility of three self-report participation measures: The icf measure of participation and activities screener, the participation scale, and the utrecht scale for evaluation of rehabilitation-participation. J Rehabil Med. 2010;42:752–7.
Post MWM, Reinhardt JD. Participation and life satisfaction in aged people with spinal cord injury: does age at onset make a difference? Top Spinal Cord Inj Rehabil. 2015;21:233–40.
Twisk J. Introduction into Applied Biostatistics (in Dutch). Maarssen: Elsevier Gezondheidszorg; 2010.
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–36.
Field A. Discovering statistics using SPSS. Third.. London, UK: SAGE; 2009.
IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.
de Graaf JA, van Mierlo ML, Post MWM, Achterberg WP, Kappelle LJ, Visser-Meily JMA, Long-term restrictions in participation in stroke survivors under and over 70 years of age. Disabil Rehabil. 2017;8288:1–9.
Gerhart KA, Bergstrom E, Charlifue SW, Menter RR, Whiteneck GG, Long-term spinal cord injury: functional changes over time. Arch Phys Med Rehabil. 1993;74:1030–4.
Cardol M, de Jong BA, van den Bos GA, Beelen A, de Groot IJ, de Haan RJ. Beyond disability: perceived participation in people with a chronic disabling condition. Clin Rehabil. 2002;16:27–35.
Tate DG, Maynard F, Forchheimer MB. Predictors of psychologic distress one year after spinal cord injury. Am J Phys Med Rehabil. 1993;72:272–5.
Krause JS, Bozard JL. Natural course of life changes after spinal cord injury: a 35-year longitudinal study. Spinal Cord. 2012;50:227–31. https://doi.org/10.1038/sc.2011.106.
von Faber M, Bootsma-van der Wiel A, van Exel E, Gussekloo J, Lagaay AM, van Dongen E, et al. Successful aging in the oldest old: who can be characterized as succesfully aged? Arch Intern Med. 2001;161:2694–700.
Acknowledgements
Sponsorship: ALLRISC is sponsored by ‘Fonds NutsOHRA’ under the responsibility of the Netherlands Organization for Health Research and Development, Project number 89000006.
Author contributions
LSR was responsible for data analysis, interpreting results, and drafting the manuscript. SG was responsible for data analysis and critical revision of the manuscript. JJA was responsible for designing the study, collecting data, and provided feedback on the manuscript. CAS provided feedback on the manuscript. MWP was responsible for designing the study and critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Ruijter, L.S., de Groot, S., Adriaansen, J.J. et al. Associations between time since onset of injury and participation in Dutch people with long-term spinal cord injury. Spinal Cord 56, 1134–1143 (2018). https://doi.org/10.1038/s41393-018-0134-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0134-7
This article is cited by
-
Longitudinal effects of time since injury and age at injury on outcomes of people with spinal cord injury in Queensland, Australia
Spinal Cord (2022)
-
Detecting subgroups in social participation among individuals living with spinal cord injury: a longitudinal analysis of community survey data
Spinal Cord (2021)