Abstract
This phase I/II trial characterized the tolerability, safety, and antitumor activities of unecritinib, a novel derivative of crizotinib and a multi-tyrosine kinase inhibitor targeting ROS1, ALK, and c-MET, in advanced tumors and ROS1 inhibitor-naive advanced or metastatic non-small cell lung cancer (NSCLC) harboring ROS1 rearrangements. Eligible patients received unecritinib 100, 200, and 300 mg QD, and 200, 250, 300, and 350 mg BID in a 3 + 3 design during dose escalation and 300 and 350 mg BID during expansion. Phase II trial patients received unecritinib 300 mg BID in continuous 28-day cycles until disease progression or unacceptable toxicity. The primary endpoint was the objective response rate (ORR) per independent review committee (IRC). Key secondary endpoints included intracranial ORR and safety. The ORR of 36 efficacy evaluable patients in the phase I trial was 63.9% (95% CI 46.2%, 79.2%). In the phase II trial, 111 eligible patients in the main study cohort received unecritinib. The ORR per IRC was 80.2% (95% CI 71.5%, 87.1%) and the median progression-free survival (PFS) per IRC was 16.5 months (95% CI 10.2, 27.0). Additionally, 46.9% of the patients who received recommended phase II dose of 300 mg BID experienced grade 3 or higher treatment-related adverse events. Treatment-related ocular disorders and neurotoxicity occurred in 28.1% and 34.4% of patients, respectively, but none was grade 3 or higher. Unecritinib is efficacious and safe for ROS1 inhibitor-naive patients with ROS1-positive advanced NSCLC, particularly patients with brain metastases at baseline, strongly supporting that unecritinib should become one of the standards of care for ROS1-positive NSCLC.
ClinicalTrials.gov identifier: NCT03019276 and NCT03972189.
Similar content being viewed by others
Introduciton
Lung cancer remains the leading cause of cancer death globally, accounting for approximately one in five (18.0%) of the total cancer deaths,1 and is expected to be the principal cause of death in both sexes in China and the USA in 2022.2 Recent remarkable advances in molecular targeted therapies have significantly extended the survival of patients with lung cancer harboring actionable mutations including EGFR exon 19 deletion and L858R mutations, and ALK and ROS1 rearrangements.3,4,5,6,7 The ROS1 oncogene, which is located on chromosome 6 (6q22), encodes protooncogene receptor tyrosine kinase ROS1. The kinase is composed of an intracellular C-terminus containing the kinase domain, a single transmembrane domain, and an extracellular N-terminal domain8 and is constitutively activated by fusion partner proteins as a result of chromosomal rearrangements that occur in approximately 1% to 2% of patients with non-small cell lung cancer (NSCLC).8,9,10 Among diverse ROS1 fusions, CD74 is the most frequent ROS1 fusion partner, and CD74–ROS1 fusion is present in ~44% of NSCLC cases with ROS1 rearrangements.9 Intriguingly, we have previously noted that NSCLC patients carrying CD74–ROS1 fusion are more likely to develop brain metastases.11 Targeted therapies are well established for NSCLC with ALK and ROS1 rearrangements that lead to constitutive kinase activity of ALK or ROS1.6 Crizotinib, an ALK and ROS1 tyrosine kinase inhibitor (TKI), has become not only one of the standards of care for ALK-positive but also the preferred drug for ROS1-rearranged NSCLC patients.12
Several pivotal trials, including the METROS trial,13 the PROFILE 1001 study14 and the OO 12-01 study,15 have demonstrated that crizotinib elicits a durable response and extends the progression-free survival (PFS) of patients with ROS1-rearranged advanced NSCLC, establishing ROS1 as a valid therapeutic target in ROS1-rearranged lung cancers. However, despite significant improvement in the objective response rate (ORR) and survival outcome of ROS1-rearranged NSCLC patients, there are concerning treatment-related adverse events (TRAEs) such as prominent gastrointestinal disturbances and ocular toxicities with crizotinib12,16 and neurotoxicity with entrectinib.17
Unecritinib (TQ-B3101), a multi-TKI targeting ROS1, ALK, and c-MET, is a derivative of crizotinib via structural modification of the pyridine ring. Our in vitro study showed that similar to crizotinib, unecritinib inhibited AKT phosphorylation and its downstream signaling molecules ERK1/2 (extracellular signal-regulated protein kinases 1 and 2) (Supplementary Fig. S1). Furthermore, unecritinib had an IC50 of 142.7 nM and an IC90 of 821.3 nM while unecritinib M had an IC50 of 0.8 nM and an IC90 of 6.2 nM for wildtype ROS1. Unecritinib also displayed notable growth inhibitory effects on several cancer cell lines carrying ALK rearrangements or mutations or overexpressing c-MET, with an IC50 of 180 to 378.9 nm for lung cancer cells and an IC50 of 23.5 nm for gastric cancer cells overexpressing c-MET. The IC50 of growth inhibition by unecritinib is comparable to that by crizotinib (Supplementary Table S1).
Meanwhile, our preclinical studies showed a greater bioavailability of unecritinib than crizotinib in beagles (data not published). In mouse xenografts bearing human lung adenocarcinoma NCI-H3122 cells, unecritinib showed greater tumor growth inhibition than crizotinib, which may be explained by higher tumor tissue exposure to unecritinib vs. crizotinib (data not published). Notably, unecritinib M, the metabolite of unecritinib, had a considerably lower AUCocular tissue/AUCplasma than crizotinib in rats (data not published). The remarkably smaller distribution of unecritinib M in the ocular tissues suggests a lower risk of ocular toxicities. Indeed, no apparent ocular toxicities were observed in rats and beagles receiving unecritinib for 4 weeks (rats 135 mg/kg; beagles 81 mg/kg) (data not published).
In this phase I/II study, we aimed to characterize the tolerability, safety, and antitumor activities of unecritinib in ROS1 inhibitor-naive patients with ROS1-rearranged advanced NSCLC and other selected advanced solid tumors who had failed standard chemotherapy. As CD74 is the most frequent ROS1 fusion partner and CD74-ROS1 fusion is present in ~44% of NSCLC cases with ROS1 rearrangements,18,19 we also carried out a prespecified analysis of the efficacy of unecritinib for NSCLC cases with CD74-ROS1 fusion.
Results
Patient characteristics
The phase I/II trial was conducted between July 12, 2017, and March 2, 2021, and the cutoff date for this analysis was December 20, 2021. Patient demographic, baseline, and prior treatment characteristics are described in Table 1 and the study flowcharts are shown in Supplementary Fig. S2. Twenty patients were enrolled in the dose escalation portion and 19 patients in the dose expanse portion of the phase I trial. Two of them (5.1%) had stage III tumors and 37 (94.9%) had stage IV tumors, and 61.5% received prior chemotherapy.
One hundred sixty patients were screened for eligibility for the phase II trial and 113 patients were eligible and received unecritinib, including 2 patients in the exploratory study cohort and 111 patients in the main study cohort. In the main study cohort, 103 patients (92.8%) had stage IV NSCLC. Thirty-three patients (29.7%) had brain metastasis and 15 (13.5%) had liver metastasis. Forty-eight patients (43.2%) received prior chemotherapy. Forty patients with ROS1 rearrangement detected by AmoyDx assay at the central laboratory subsequently underwent central testing by NGS. The concordance rate was 100% between the Amoydx assay and central NGS testing (excluding samples that failed quality control). Twenty-seven patients (67.5%) had CD74-ROS1 fusion. Five patients (12.5%) had SDC4-ROS1 fusion, and 3 (7.5%) had SLC34A2-ROS1 fusion. In addition, EZR-ROS1 and TPM3-ROS1 fusion was each present in 1 patient (2.5%). Furthermore, one patient carried both EZR-ROS1 and TGFBR1-ROS1 fusions and another carried both EZR-ROS1 and SLC34A2-ROS1 fusions. ROS1 fusion partners were indeterminate in 71 patients who did not undergo NGS.
Safety
The safety population was composed of 128 patients, including three patients who received unecritinib 300 mg BID during dose escalation, 12 patients who received unecritinib 300 mg BID during dose expansion, and 113 patients from the phase 2 trial. Data on gene mutations were available from six patients from the phase 1 trial, including 3 cases who had ALK fusion, 2 cases who had unspecified ALK mutations, 1 case with unspecified ROS1 mutation. All 113 patients from the phase 2 trial had ROS1 fusions.
No dose-limiting toxicities (DLTs) were observed in the dose-escalation portion of the phase I trial. Patients receiving unecritinib 300 mg BID reported lower rates of grade 3 or higher adverse events (AEs) and treatment-emergent AEs leading to dose reductions or interruptions than those receiving unecritinib 350 mg BID (Supplementary Table S2). Taking into consideration the results of subsequent efficacy analysis, we chose oral unecritinib 350 mg BID as the maximum-tolerated dose (MTD) and unecritinib 300 mg BID as the recommended phase II dose (RP2D) to provide a safe dosing regimen without jeopardizing the efficacy of unecritinib.
Grade 3 or higher TRAEs occurred in 41.0% of the patients in the phase I trial and 46.9% of the patients who received unecritinib 300 mg BID in both trials (Supplementary Tables S2 and S3). TRAEs led to dose reductions in 17.2% and dosing interruptions in 37.5% of the patients in all patients who received unecritinib 300 mg BID. Three patients (2.3%) discontinued unecritinib due to TRAEs. Among 128 patients who received RP2D 300 mg BID in both trials, the most frequently reported grade 3 or 4 TRAEs were reduced neutrophil count (25.8%), elevated alanine aminotransferase (7.8%), and reduced leukocyte count (6.3%) (Table 2). Reduced neutrophil count led to treatment interruptions in 26 cases (20.3%), but no treatment discontinuation. Treatment-related ocular disorders (cluster term) were reported in 28.1% of the patients, but none were grade 3 or higher (Supplementary Table 4). Furthermore, 34.4% of the patients had neurotoxicity (cluster term), and none were grade 3 or higher. TRAEs were manageable through dose reductions or interruptions and supportive therapy. No treatment-related death occurred in either trial. In addition, 4 patients in the phase II trial received prior PD-1/PD-L1 inhibitor therapy. They experienced a total of 88 any grade TRAEs, all of which were grade 1 or 2 except grade 3 elevated alanine aminotransferase in 1 patient.
Pharmacokinetics
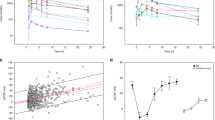
Unecritinib was rapidly absorbed regardless of doses or dosing schedule and reached peak plasma concentration in 30–60 min. Meanwhile, plasma unecritinib M concentrations peaked between 2 and 4 h after dosing (Fig. 1 and Supplementary Fig. S3). The levels of systemic exposure to unecritinib and unecritinib M (Cmax and AUC0–t) increased as the dose level increased from 100 to 200 mg (single oral administration) and from 100 to 300 mg QD (multiple once-daily oral administrations). The dose proportionality was inconclusive for multiple twice daily oral administrations. Unecritinib had a seemingly dose-independent and rather brief T1/2 after single or multiple administrations. The short T1/2 caused no significant plasma accumulation of unecritinib over time, with a geometric mean Rac between 0.8 and 1 at the steady state after multiple twice-daily oral administrations at 200–350 mg. Though the geometric mean Rac ranged between 0.8 and 1.5 at the steady state after multiple once-daily oral administrations at 100, 200, and 300 mg, it was dose independent. Notably, the metabolite of unecritinib had a considerably longer T1/2 (between 4.6 and 69.9 h) after single or multiple administrations, which contributed to plasma accumulation of unecritinib M, with a geometric mean Rac between 3.6 and 6.0 at the steady state after multiple twice daily oral administrations at 200–350 mg. Overall, CL/F of unecritinib M declined over time after multiple twice-daily oral administrations at 200–350 mg.
Pharmacokinetics characteristics. Mean plasma concentration-time curves of unecritinib M (a) after a single oral administration at 100 and 200 mg (linear scale). Mean plasma concentration-time curves of unecritinib M (b) after once daily multiple oral administrations at 100, 200, and 300 mg (linear scale). Mean plasma concentration-time curves of unecritinib M (c) after twice-daily multiple oral administrations at 200, 250, 300, and 350 mg (linear scale). The dotted lines indicate IC50 (0.8 nm [0.4 ng/mL], green) and IC90 (6.2 nm [2.8 ng/mL], black) of unecritinib M for wildtype ROS1
Efficacy
Overall efficacy
The ORR of the 36 efficacy evaluable patients in the phase I trial was 63.9% (95% CI 46.2–79.2) and the DCR was 94.4% (95% CI 81.3–99.3) (Fig. 2a, c; Supplementary Table S5).
Treatment responses. Waterfall plots of the best percentage changes for the sum of target lesion diameters after unecritinib treatment are shown for individual patients with the best objective response assessed by the independent review committee (IRC) per RECIST v1.1 as indicated by the color codes. The dotted line indicates a 30% reduction in the target lesion size. Each bar represents one patient in the efficacy-evaluable population in phase I trial (a) and phase II trial (b). Treatment responses in (b) are also color-coded for gene fusion partners CD74-ROS1, non-CD74-ROS1 fusions, and indeterminate. Swimmer plot of duration of treatment duration (months) of individual patients in phase I trial (c). Each bar represents one efficacy evaluable patient who had attained partial response. Deaths are marked in solid cycles. Patients receiving ongoing treatment are marked with an arrow. d The Kaplan–Meier curve for estimated progression-free survival (PFS) in the intention-to-treat population of phase II trial patients treated with unecritinib. Vertical lines on the survival curve indicate censoring of data. NE not evaluable
At the data cutoff, 53 patients were still receiving unecritinib. Of the 113 patients who received unecritinib, 2 patients in the exploratory study cohort were excluded from the efficacy analysis. One of the 111 efficacy evaluable patients attained CR and 88 of them achieved PR, with an ORR of 80.2% (95% CI 71.5%, 87.1%). Furthermore, 9 patients had SD, and the DCR was 88.3% (95% CI 80.8%, 93.6%). Eleven patients had PD. One hundred and nine patients experienced a reduction from baseline in target lesion size (Fig. 2b). The median DOR was 20.3 months (95% CI 11.0, 26.1) (Table 3). Forty-eight PFS events had occurred and the median PFS was 16.5 months (95% CI 10.2, 27.0) (Fig. 2d). The 6-month PFS rate reached 83.2% (95% CI 74.6%, 89.0%) and the 12-month PFS rate 53.8% (95% CI 42.7%, 63.6%).
Subgroup analysis
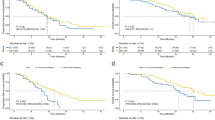
Twenty-seven patients who had CD74-ROS1 rearrangements exhibited a notable response to unecritinib therapy, with CR in 1 patient and PR in 23 patients, and an ORR of 88.9% (95% CI 70.8%, 97.7%). Furthermore, the median PFS was 21.2 months (95% CI 10.2, not reached) in patients with CD74-ROS1 rearrangements (Fig. 3a) and 10.1 months (95% CI 6.4, not reached) in patients with non-CD74-ROS1 rearrangements (Fig. 3b).
An exploratory subgroup analysis showed that both patients without brain metastasis (ORR 83.3%, 95% CI 73.2%, 90.8%) and those with brain metastasis (ORR 72.7%, 95% CI 54.5%, 86.7%) showed remarkable response to unecritinib therapy. Patients receiving no prior radiotherapy (ORR 82.4%, 95% CI 73.6%, 89.2%), prior or ever smoked (ORR 93.5%, 95% CI 78.6%, 99.2%), or no prior line of chemotherapy (ORR 81.5%, 95% CI 70.0%, 90.1%) exhibited significant response to unecritinib therapy. Patients receiving one prior line of chemotherapy also displayed notable responses to unecritinib therapy (ORR 82.9%, 95% CI 66.4%, 93.4%) (Fig. 4a). Twenty-three PFS events occurred among 33 patients with baseline brain metastases and the median PFS was 10.1 months (95% CI 5.5, 12.0) (Fig. 4b), with a 6-month PFS rate of 66.3% (95% CI 47.4%, 79.7%) and a 12-month PFS rate of 24.3% (95% CI 9.7%, 42.5%). Meanwhile, the median PFS was not reached among 78 patients without baseline brain metastases (Fig. 4c).
a Forest plot analysis of objective response rates (ORR) per patient subgroups in the main study cohort (n = 111). RTHYN, prior receipt of radiotherapy; SMKYN, prior or current smokers. The Kaplan–Meier curve for estimated PFS in the intention-to-treat population of phase II trial with (b) and without (c) baseline brain metastases who were treated with unecritinib. d The Kaplan Meier curve for estimated intracranial PFS. Vertical lines on the survival curve indicate the censoring of data
In addition, 4 patients (3 in the phase 1 trial and 1 in the exploratory study cohort of the phase 2 trial) had previously received crizotinib. Two of them attained PR as their best overall response (Supplementary Table S6).
Intracranial efficacy
There were 11 patients with intracranial target lesions among 33 patients who had brain metastases at baseline. Three patients had previously received radiotherapy for brain metastases. The intracranial ORR by IRC per RANO-BM was achieved in 8/11 patients (72.7%; 95% CI, 39.0%, 94.0%), including 1 patient who attained CR and 7 patients who achieved PR (Table 4). Two patients had SD, and 10/11 patients achieved disease control, with a DCR of 90.9% (95% CI, 58.7%, 99.8%). No patients developed PD. Eight (8/11, 72.7%) intracranial PFS events occurred and the median intracranial PFS was 10.1 months (95% CI 1.4, 27.0) (Fig. 4d). The 6-month PFS rate was 71.6% (95% CI 35.0%, 89.9%) and the 12-month PFS rate was 30.7% (95% CI 7.3%, 58.6%).
Discussion
Recent remarkable advances in molecular targeted therapies for advanced NSCLC harboring mutations such as ALK and ROS1 rearrangement have extended the survival of these patients.3,4,5,6,20 However, safety concerns such as ocular toxicities with crizotinib.12,16 and neurotoxicity with entrectinib.17 have emerged, highlighting the need for the development of effective and safer molecular targeted therapeutic agents. We developed a novel TKI, unecritinib, with favorable pharmacokinetics characteristics and promising antitumor activities, which, at the same time, avoided or lessened the special toxicities of crizotinib and entrectinib. Our preclinical evidence indicates that this novel multi-kinase inhibitor of ROS1, ALK and c-MET has a greater bioavailability than crizotinib, and unecritinib M has a 200-fold lower distribution in ocular tissues than crizotinib. As far as we know, this is the largest trial of ROS-1 positive tumors harboring ROS1 rearrangements showing that unecritinib had an acceptable toxicity profile, with lower rates of and no grade 3 or higher ocular toxicities and neurotoxicities, and elicited a durable response, with more than half (53.8%) of the patients being progression-free at 12 months. These findings demonstrate that unecritinib is safe and has promising activities against advanced NSCLC harboring ROS1 rearrangement.
In this trial, unecritinib demonstrated promising antitumor activities in advanced NSCLC patients with ROS1 rearrangement. Notably, unecritinib achieved an ORR by IRC of 80.2% while the ORR by IRC was 71.7% for crizotinib in the OO 12-01 study of East Asians with ROS1-positive advanced NSCLC15 and 67.1% for entrectinib in the integrated analysis of data from the STARTRK-1 and −2 and ALKA-372-00121 trials. The DCR reached 88.3% with unecritinib and is comparable to that of crizotinib (88.2%)15 and higher than that (75.8%) of entrectinib.21 The median PFS was 16.5 months in the current trial and 15.9 months with crizotinib15 and 15.7 months with entrectinib in the integrated analysis of data from the STARTRK-1 and -2 and ALKA-372-00121 trials. The high efficacy of unecritinib could be at least partially attributed to its high levels in the tumor tissues, as shown in our preclinical studies (data not published).
Previous studies showed that NSCLC patients with ROS1 fusions are more predisposed to brain metastases22; 20–50% of NSCLC patients have brain metastases,22 and CNS is the site of initial progression in approximately half of ROS1 fusion-positive NSCLC patients treated with crizotinib,23 highlighting the importance of CNS activity for ROS1 TKIs. There are no preclinical data on the comparison of the intracranial efficacy of unecritinib versus other ROS1 inhibitors.24 In the current study, the ORR of the patients who had brain metastases at baseline was 72.7% while that of entrectinib was 62.5%. In addition, unecritinib achieved an intracranial ORR of 72.7% per IRC among patients with baseline intracranial target lesions, which is largely comparable to that attained with entrectinib (79.2%) in the integrated analysis of data from the STARTRK-1 and -2 and ALKA-372-00121 trials. Notably, 46.4% of these patients in the integrated analysis had received radiotherapy for brain metastases, including 20 patients who received radiotherapy within the preceding 6 months and 26 patients who received or did not receive radiotherapy before the preceding 6 months. The intracranial ORR was 60% for those who had received radiotherapy within the preceding 6 months versus 46.2% for those who had not. Meanwhile, the intracranial PFS was 16.1 months for those who had received radiotherapy within the preceding 6 months versus 8.8 months for those who had not. Only 9 (8.1%) of our patients had received radiotherapy and 9.1% of the patients with baseline brain lesions had received radiotherapy. Meanwhile, ceritinib had a low intracranial ORR (29%) in NSCLC with ROS1 rearrangements.25 Intracranial response to crizotinib was not assessed in the phase II OO 12-01 study of East Asians with ROS1-positive advanced NSCLC.15 and the intracranial ORR was 33% (2/6) with crizotinib in the phase II METROS trial.13 In addition, the median intracranial PFS reached 10.1 months in our patients with baseline intracranial target lesions versus 12.0 months with entrectinib in patients with measurable central nervous system lesions at baseline.21
Accurate delineation of targetable oncogenic alterations is critical to the targeted therapies for NSCLC21 and testing of all non-squamous NSCLC for therapy-predictive biomarkers is recommended in clinical practice guidelines.26 Our previous study showed that NSCLC patients with different ROS1 fusions responded differently to crizotinib therapy.22 Among diverse ROS1 fusions, CD74 is the most frequent ROS1 fusion partner and CD74–ROS1 fusion is present in ~44% of NSCLC cases with ROS1 rearrangements.18,19 In this trial, about two-thirds of the NSCLC patients (67.5%) who had undergone central NGS testing had CD74-ROS1 fusion. Currently, it remains inconclusive whether TKI is efficacious for NSCLC harboring CD74-ROS1 fusions. In the PROFILE 1001 trial, crizotinib efficacy was independent of ROS1 translocation type.14 A retrospective analysis showed that patients whose tumor harboring CD74-ROS1 had a significantly shorter median PFS with first-line crizotinib than those harboring non-CD74-ROS1 fusions27 (17.0 months vs. 21.0 months; P = 0.008). Reduced efficacy of crizotinib in CD74-ROS1-positive patients was also noted by other investigators.12,22 The ORR with entrectinib for those with CD74-ROS1 fusions was 72.9%, which is higher than that (67.1%) of the overall patient populations.21 In the current trial, unecritinib attained an ORR of 88.9% in patients with CD74-ROS1 rearrangements, and the median PFS of these patients doubled that of patients without CD74-ROS1 rearrangements (21.2 vs. 10.1 months). To our knowledge, this is the first time that ROS1-TKI has been found to have a greater ORR and longer PFS in a large sample of patients with CD74-ROS1 rearrangements in a prospective clinical study.
The safety profile of unecritinib is overall consistent with that of other ROS1 inhibitors. The rate of drug dose interruptions due to TRAEs was 37.5% in the patients who received unecritinib 300 mg BID, which is higher than that (22.8%) of crizotinib.15 However, the proportion of patients who discontinued treatment due to TRAEs is low in these patients (2.3%) and comparable to that of crizotinib.12 Reduced neutrophil count was the most frequent TRAE in this study, occurring in 25.8% of the patients, compared to 12% with crizotinib.12 Reduced neutrophil count contributed to treatment interruptions in this trial, but it was manageable through dose reductions or interruptions and supportive therapy, which may explain the similar rate of treatment discontinuations of unecritinib and crizotinib. Among 128 patients who received unecritinib 300 mg BID, the other most frequently reported grade 3 or 4 TRAEs included elevated alanine aminotransferase (7.8%), and reduced leukocyte count (6.3%), which are common AEs that are also reported with other ROS1 TKIs. The TRK family of kinases are implicated in CNS homeostasis and inhibition of these kinases may lead to CNS symptoms such as dizziness and dysgeusia.28 Dizziness occurred in 10.9% and dysgeusia in 13.3% of our patients receiving unecritinib 300 mg BID, but neither was grade 3 or higher. These CNS abnormalities were also reported in NSCLC patients treated with crizotinib (dizziness 16%; dysgeusia 18%)12 and entrectinib (dizziness 34.8%; dysgeusia 43.4%).21 Ophthalmological AEs are unique AEs that were reported in a high proportion of NSCLC patients treated with crizotinib (82%)12 and also occurred in patients treated with other ROS1 inhibitors including brigatinib,29 entrectinib,30 and lorlatinib.18 As expected, ophthalmological AEs including visual impairment and blurred vision occurred in 36 patients (28.1%) in the current trial. This low rate of ophthalmological AEs might be at least partially due to the notably smaller distribution of unecritinib metabolite in ocular tissues than that of crizotinib, as shown in our preclinical studies (data not published). In addition, though the rate of any grade elevated AST (73.4%) and elevated ALT (71.9%) is higher with unecritinib than that reported for crizotinib (22% and 14%, respectively),4 the rate of grade III or higher elevated AST (3.9%) and ALT (7.8%) is largely comparable to crizotinib (2% and 4%, respectively).
A previous pharmacokinetics analysis of quantifiable unecritinib and unecritinib M data from 40 subjects after oral administration of unecritinib showed that unecritinib pharmacokinetics could be explained by a 1-compartment model with first-order absorption and elimination for unecritinib coupled with a 2-compartment model with time-dependent clearance for the metabolite.31 Our pharmacokinetics analysis found that the AUC0-t of unecritinib increased in a dose-proportional manner following rapid intestinal absorption of unecritinib BID from 200 to 350 mg. However, there was no apparent accumulation of unecritinib with unecritinib BID. The metabolite unecritinib M had considerable plasma accumulation at the steady state after multiple twice-daily oral administrations at 200–350 mg. Unecritinib is not a next-generation ROS1 inhibitor that could overcome ROS1 resistance mutations. Novel next-generation TKIs such as repotrectinib which has highly potent activities against ROS1, TRKA-C, and ALK could target on-target kinase domain mutations, which are a major mechanism of acquired resistance.32 In the early-stage TRIDENT-1 trial, repotrectinib demonstrated potent activities in ROS1 rearranged NSCLC with solvent-front mutations.33 Taletrectinib, a novel ROS1 and pan-NTRK TKI, has demonstrated preclinical activities against ROS1G2032R solvent-front mutation and also shown meaningful clinical antitumor activities against advanced crizotinib-refractory ROS1 + NSCLC.34 The 4th generation TKI NVL-655 with activities against a variety of ALK mutations is under active development.35 These novel TKIs could offer potentially effective treatment for NSCLC with solvent-front mutations including ALKG1202R, ROS1G2032R or ROS1D2033N, TRKAG595R, and TRKCG623R. Two patients in our study received prior crizotinib and achieved PR. It is of intrigue and clinical relevance to learn whether unecritinib could also target ROS1 resistance mutations in advanced NSCLC, the answer to which, however, requires validation in future clinical trials with a larger target population.
Overall, this study demonstrated that unecritinib had an acceptable safety profile and established the clinical benefit of unecritinib for ROS1 inhibitor-naive patients with ROS1-positive advanced NSCLC and other selected advanced solid tumors who had failed prior chemotherapy. Notably, unecritinib was more effective in CD74-ROS1 rearrangements NSCLC patients. Given that the CNS is a common site of metastases and a frequent site of disease progression in advanced NSCLC, unecritinib led to durable intracranial tumor responses, reflecting its potent intracranial activities. The findings strongly support that unecritinib should become one of the standards of care for NSCLC harboring ROS1 rearrangements, particularly those patients with baseline brain metastases or CD74-ROS1 fusions, and further clinical development of unecritinib for NSCLC with ALK rearrangement is warranted.
Materials and methods
Ethics statement
The trial protocols were approved by the independent ethics committee at each site and complied with the International Ethical Guidelines for Biomedical Research Involving Human Subjects. The studies were conducted according to Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written informed consent prior to any trial activities.
Screening criteria
This phase I/II trial enrolled adult patients with histologically confirmed advanced tumors (phase I) or locally advanced or metastatic NSCLC with ROS1 rearrangements (phase II). ROS1 rearrangements were determined using a reverse transcription-polymerase chain reaction (RT-PCR) AmoyDx assay.15 (Amoy Diagnostics, Xiamen, China) in the main study cohort of the phase II trial. Furthermore, ROS1 fusions detected at the central laboratory underwent next-generation sequencing (NGS) for further comparison of efficacy for patients with CD74-ROS1 fusions and those with non-CD74-ROS1 fusions if there were enough tissue. NGS was performed on the NextSeq CN500 platform (Berry Genomics Co., Ltd) at a central laboratory using the HANDLE Classic NGS Panel (Amoy Diagnostics). Patients who were positive for ROS1 fusions other than those included in the AmoyDx assays as detected by fluorescent in situ hybridization (FISH) or NGS and those who progressed on crizotinib were categorized into the exploratory study cohort of the phase II trial. Other eligibility criteria were no more than two prior chemotherapy regimens, at least one radiologically confirmed measurable target lesion per Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, and an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0–1. Prior therapy with crizotinib or other ROS1 inhibitors was not permitted in the main study cohort. Additional eligibility criteria are provided in the study protocol.
Study design and treatment
In the phase I trial, the MTD and the RP2D were determined using a dose–escalation strategy with a 3 + 3 design using a modified Fibonacci scheme, with preferential enrollment of ALK and ROS1-rearranged NSCLC patients. In the phase II trial, all patients harboring ROS1 rearrangement received the RP2D of unecritinib 300 mg twice daily (BID) orally in continuous 28-day cycles until disease progression or development of unacceptable toxicity. The primary endpoints for phase I trial were to determine the safety, tolerability, DLTs, MTD, and pharmacokinetics of unecritinib. The primary endpoint of the phase II trial was ORR per the independent review committee (IRC). Secondary endpoints included the antitumor activities of unecritinib in ALK- and ROS1-rearranged advanced lung cancer patients for phase I and duration of response (DOR), disease control rate (DCR), PFS, intracranial ORR, intracranial DOR, intracranial time to progression (TTP), intracranial PFS, overall survival and safety for phase II.
Dose modification was allowed for grade 3 or higher adverse events (AEs) per the National Cancer Institute Common Terminology Criteria for AEs (NCI-CTC AE) version 5.0, with two levels of dose reduction, from 300 mg BID to 250 mg BID and from 250 mg BID to 200 mg BID. If more than two dose levels need to be reduced, the study treatment was terminated.
The trial protocols were approved by the independent ethics committee at each site and complied with the International Ethical Guidelines for Biomedical Research Involving Human Subjects. The studies were conducted according to Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written informed consent prior to any trial activities.
Assessments
Tumor responses were evaluated by investigators and IRC per RECIST v1.1 using computed tomography (CT) or magnetic resonance imaging (MRI) within 2 weeks of study entry, at 6 weeks post-treatment, and once every two cycles thereafter. Complete response (CR), partial response (PR), and stable disease (SD) had to be confirmed with a repeat scan after at least 6 weeks. The response of intracranial disease was evaluated radiologically per Response Assessment in Neuro-Oncology Brain Metastases (RANO-BM). AEs were evaluated using NCI-CTC AE version 5.0.
Pharmacokinetic assessments
Blood samples for pharmacokinetics analyses were collected predose on days 1, 7, 14, 21, and 28, and 30 min, 1, 2, 4, 6, 10, and 12 h postdose on days 1 and 28. The concentrations of unecritinib and unecritinib M were measured by tandem mass spectrometry hyphenated to liquid chromatography separation systems (HPLC–MS/MS). The pharmacokinetics parameters were calculated by non-compartmental analysis (NCA) model using WinNonLin® v 6.4 (Certara, Princeton, NJ, USA) and included Cmax and time to reach Cmax (Tmax), minimum and average steady-state concentration [CSS(min) and Css-av], the area under the steady-state plasma concentration–time curve (AUCss), terminal elimination half-life (T1/2) and degree of fluctuation.
Statistical analysis
Based on the phase II OO 12-01 study,15 an ORR of 50% as the lower limit of two-sided 95% CI was required to demonstrate the efficacy of unecritinib. The statistical power (1−β) to demonstrate efficacy based on this threshold was 85%. For a targeted ORR of 65%, with one-sided α of 0.025, 94 evaluable patients with ROS1-rearranged NSCLC were required for the main study cohort of the phase II trial. Assuming a drop-off rate of 15%, the maximum estimated target sample size was 111.
The Full Analysis Set (FAS) included all enrolled patients who had received at least one dose of unecritinib except for the patients enrolled into the exploratory study cohort, and the Per Protocol Set (PPS) included all enrolled patients who had received at least one cycle of treatment, with at least one radiological evaluation, good compliance, and no major study protocol violations. The pharmacokinetics concentration set included all enrolled patients who had received at least one dose of unecritinib and had one post-treatment measurement of plasma concentration of unecritinib. The pharmacokinetics parameter set includes all enrolled patients who had received at least one dose of unecritinib and had at least one valid pharmacokinetic parameter data. The safety set included all enrolled patients who had received at least one dose of unecritinib. No imputation was done for missing data. We estimated 95% CIs using the conventional Wald method for ORR and the Clopper-Pearson method for DCR and intracranial ORR. ORR and its 95% CI were presented graphically using forest plots. Kaplan–Meier methods were used to determine medians and 95% CIs for DOR, PFS, intracranial DOR, intracranial TTP and intracranial PFS. AEs were mainly analyzed using descriptive statistics.
Statistical analyses were undertaken using the SAS software package, version 9.4 M5 (SAS Institute Inc., Cary, NC). All tests were two-tailed with a level of significance set at P ≤ 0.05.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Cao, W. et al. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin. Med J. (Engl.). 134, 783–791 (2021).
Wang, M., Herbst, R. S. & Boshoff, C. Toward personalized treatment approaches for non-small-cell lung cancer. Nat. Med. 27, 1345–1356 (2021).
Ramalingam, S. S. et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N. Engl. J. Med. 382, 41–50 (2020).
Lin, J. J. et al. Five-year survival in EGFR-mutant metastatic lung adenocarcinoma treated with EGFR-TKIs. J. Thorac. Oncol. 11, 556–565 (2016).
Tan, A. C. & Tan, D. S. W. Targeted therapies for lung cancer patients with oncogenic driver molecular alterations. J. Clin. Oncol. 40, 611–625 (2022).
Mok, T. S. et al. IASLC Atlas of EGFR Testing in Lung Cancer. wclc2017.iaslc.org. [Internet]. IASLC (2017).
Gendarme, S., Bylicki, O., Chouaid, C. & Guisier, F. ROS-1 fusions in non-small-cell lung cancer: evidence to date. Curr. Oncol. 29, 641–658 (2022).
Bergethon, K. et al. ROS1 rearrangements define a unique molecular class of lung cancers. J. Clin. Oncol. 30, 863–870 (2012).
Soda, M. et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 448, 561–566 (2007).
Li, Z. et al. Efficacy of Crizotinib among different types of ROS1 fusion partners in patients with ROS1-rearranged non-small cell lung cancer. J. Thorac. Oncol. 13, 987–995 (2018).
Shaw, A. T. et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N. Engl. J. Med. 371, 1963–1971 (2014).
Landi, L. et al. Crizotinib in MET-deregulated or ROS1-rearranged pretreated non-small cell lung cancer (METROS): a Phase II, prospective, multicenter, two-arms trial. Clin. Cancer Res. 25, 7312–7319 (2019).
Shaw, A. T. et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): updated results, including overall survival, from PROFILE 1001. Ann. Oncol. 30, 1121–1126 (2019).
Wu, Y. L. et al. Phase II study of crizotinib in East Asian patients with ROS1-positive advanced non-small-cell lung cancer. J. Clin. Oncol. 36, 1405–1411 (2018).
Dikopf, A., Wood, K. & Salgia, R. A safety assessment of crizotinib in the treatment of ALK-positive NSCLC patients. Expert Opin. Drug Saf. 14, 485–493 (2015).
Christofyllakis, K. et al. Biomarker guided treatment in oncogene-driven advanced non-small cell lung cancer in older adults: a Young International Society of Geriatric Oncology Report. J. Geriatr. Oncol. 13, 1071–1083 (2015).
Drilon, A. et al. ROS1-dependent cancers—biology, diagnostics and therapeutics. Nat. Rev. Clin. Oncol. 18, 35–55 (2021).
Lee, J. J. et al. Tracing oncogene rearrangements in the mutational history of lung adenocarcinoma. Cell 177, 1842–1857.e1821 (2019).
Mok, T. & Carbone, D. IASLC Atlas of EGFR Testing in Lung Cancer (IASLC, Denver, CO, 2017).
Dziadziuszko, R. et al. Updated integrated analysis of the efficacy and safety of entrectinib in locally advanced or metastatic ROS1 fusion-positive non-small-cell lung cancer. J. Clin. Oncol. 39, 1253–1263 (2021).
Drilon, A. et al. Frequency of brain metastases and multikinase inhibitor outcomes in patients with RET-rearranged lung cancers. J. Thorac. Oncol. 13, 1595–1601 (2018).
Patil, T. et al. The incidence of brain metastases in Stage IV ROS1-rearranged non-small cell lung cancer and rate of central nervous system progression on crizotinib. J. Thorac. Oncol. 13, 1717–1726 (2018).
Zhou, W. J. et al. Crizotinib (PF-02341066) reverses multidrug resistance in cancer cells by inhibiting the function of P-glycoprotein. Br. J. Pharm. 166, 1669–1683 (2012).
Lim, S. M. et al. Open-label, multicenter, Phase II Study of ceritinib in patients with non-small-cell lung cancer harboring ROS1 rearrangement. J. Clin. Oncol. 35, 2613–2618 (2017).
Planchard, D. et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 29, iv192–iv237 (2018).
Zhang, Y. et al. Clinical and molecular factors that impact the efficacy of first-line crizotinib in ROS1-rearranged non-small-cell lung cancer: a large multicenter retrospective study. BMC Med 19, 206 (2021).
Drilon, A. TRK inhibitors in TRK fusion-positive cancers. Ann. Oncol. 30(Suppl. 8), viii23–viii30 (2019).
Camidge, D. R. et al. Brigatinib versus crizotinib in ALK-positive non-small-cell lung cancer. N. Engl. J. Med. 379, 2027–2039 (2018).
Demetri, G. D. et al. Updated integrated analysis of the efficacy and safety of entrectinib in patients with NTRK fusion-positive solid tumors. Clin. Cancer Res. 28, 1302–1312 (2022).
Yang, F. et al. Population pharmacokinetic modeling and simulation of TQ-B3101 to inform dosing in pediatric patients with solid tumors. Front. Pharm. 12, 782518 (2021).
Drilon, A. et al. Repotrectinib (TPX-0005) is a next-generation ROS1/TRK/ALK inhibitor that potently inhibits ROS1/TRK/ALK solvent-front mutations. Cancer Discov. 8, 1227–1236 (2018).
Yun, M. R. et al. Repotrectinib exhibits potent antitumor activity in treatment-naïve and solvent-front-mutant ROS1-rearranged non-small cell lung cancer. Clin. Cancer Res. 26, 3287–3295 (2020).
Ou, S. I. et al. Efficacy of taletrectinib (AB-106/DS-6051b) in ROS1+ NSCLC: an updated pooled analysis of U.S. and Japan Phase 1 studies. JTO Clin. Res. Rep. 2, 100108 (2021).
Henry, E. et al. Abstract 1468: NUV-655 (NVL-655) is a selective, brain-penetrant ALK inhibitor with antitumor activity against the lorlatinib-resistant G1202R/L1196M compound mutation. Cancer Res. 81, 1468 (2021).
Acknowledgements
This work was supported by funds provided to Dr. Shun Lu by the National Key R&D Program of China (2016YFC1303300), the National Natural Science Foundation of China (82030045), Shanghai Municipal Science & Technology Commission Research Project (17431906103; 19411950500), Shanghai Chest Hospital Project of Collaborative Innovation (YJXT20190105) and the Clinical Research Plan of SHDC (16CR3005A; 2020CR5001).
Author information
Authors and Affiliations
Contributions
S.L. and H.P. contributed to the study’s conception and design. All authors except for T.W. and J.Z. collected the data. T.W. and J.Z. performed the data analysis. All authors contributed to the interpretation of the data and the completion of figures and tables. All authors contributed to the drafting of the article, have read and given final approval of the submitted version.
Corresponding authors
Ethics declarations
Competing interests
S.L. has received research support from Astra Zeneca, Hutchison, BMS, Heng Rui, Beigene and Roche, Hansoh, Lilly Suzhou Pharmaceutical Co. Ltd; has received speaker fees from Astra Zeneca, Roche, Hansoh, Hengrui Therapeutics; and is an advisor and consultant of Astra Zeneca, Pfizer, Boehringer Ingelheim, Hutchison MediPharma, ZaiLab, GenomiCare, Yuhan Corporation, Menarini, InventisBio Co. Ltd., Shanghai Fosun Pharmaceutical (Group) Co., Ltd., Simcere Zaiming Pharmaceutical Co., Ltd. and Roche. T.W. and J.Z. are employees of Chia Tai Tianqing Pharmaceutical Group Co., Ltd. All the other authors declare no competing interests.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, S., Pan, H., Wu, L. et al. Efficacy, safety and pharmacokinetics of Unecritinib (TQ-B3101) for patients with ROS1 positive advanced non-small cell lung cancer: a Phase I/II Trial. Sig Transduct Target Ther 8, 249 (2023). https://doi.org/10.1038/s41392-023-01454-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41392-023-01454-z