Abstract
Background
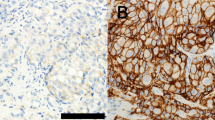
Identification of emerging molecular biomarkers on circulating tumor cells (CTCs) represents an attractive feature of liquid biopsy that facilitates precision and tailored medicine in the management of metastatic castration-resistant prostate cancer (mCRPC). Prostein is an androgen-regulated transmembrane protein with high prostate specificity. Prostein-positive circulating tumor cell (CTC) was recently suggested to have diagnostic potential; however, no study has been conducted to evaluate its prognostic value in mCRPC.
Methods
CTCs from mCRPC patients were enumerated using the CellSearch System. Prostein-positive CTCs were identified by immunostaining results. The relationships between prostein expression on CTCs and PSA response rate, PSA progression-free survival (PSA-PFS), radiographic progression-free survival (PFS), and overall survival (OS) were tested by Fisher’s exact test or evaluated using Kaplan–Meier and multivariate Cox analyses.
Results
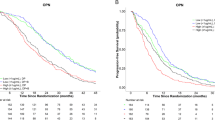
Prostein-positive CTCs were identified in 31 of 87 baseline samples from mCRPC patients and 16 of 51 samples collected at the first follow-up visit. PSA response rates were significantly lower in baseline prostein-positive patients (0%, 0/31) than in prostein-negative patients (19.6%, 11/56) (p = 0.007). The 31 prostein-positive patients had significantly shorter PSA-PFS (p < 0.001), radiographic PFS (p < 0.001), and OS (p = 0.018), compared to the 56 prostein-negative patients at baseline. The association with PSA-PFS maintained its significance (p = 0.028) in multivariate analyses. Analyzing prostein expression at the first follow-up as well as the conversion of prostein expression from baseline to follow-up samples not only confirmed the association with PSA-PFS, but also demonstrated prognostic significance with OS.
Conclusion
Our study provides the first evidence to support the potential of prostein expression on CTCs to serve as a novel prognostic marker in mCRPC patients. Future large-scale prospective studies are needed to validate our findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48.
Lowrance WT, Murad MH, Oh WK, Jarrard DF, Resnick MJ, Cookson MS. Castration-resistant prostate cancer: AUA Guideline Amendment 2018. J Urol. 2018;200:1264–72.
Schaeffer E, Srinivas S, Antonarakis ES, Armstrong AJ, Bekelman JE, Cheng H, et al. NCCN guidelines insights: prostate cancer, Version 1.2021. J Natl Compr Cancer Netw. 2021;19:134–43.
Crocetto F, Russo G, Di Zazzo E, Pisapia P, Mirto BF, Palmieri A, et al. Liquid biopsy in prostate cancer management-current challenges and future perspectives. Cancers. 2022;14:3272.
Trujillo B, Wu A, Wetterskog D, Attard G. Blood-based liquid biopsies for prostate cancer: clinical opportunities and challenges. Br J Cancer. 2022;127:1394–402.
Tulpule V, Morrison GJ, Falcone M, Quinn DI, Goldkorn A. Integration of liquid biopsies in clinical management of metastatic prostate cancer. Curr Oncol Rep. 2022;24:1287–98.
de Bono JS, Scher HI, Montgomery RB, Parker C, Miller MC, Tissing H, et al. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res. 2008;14:6302–9.
Scher HI, Jia X, de Bono JS, Fleisher M, Pienta KJ, Raghavan D, et al. Circulating tumour cells as prognostic markers in progressive, castration-resistant prostate cancer: a reanalysis of IMMC38 trial data. Lancet Oncol. 2009;10:233–9.
Goldkorn A, Ely B, Quinn DI, Tangen CM, Fink LM, Xu T, et al. Circulating tumor cell counts are prognostic of overall survival in SWOG S0421: a phase III trial of docetaxel with or without atrasentan for metastatic castration-resistant prostate cancer. J Clin Oncol. 2014;32:1136–42.
Heller G, McCormack R, Kheoh T, Molina A, Smith MR, Dreicer R, et al. Circulating tumor cell number as a response measure of prolonged survival for metastatic castration-resistant prostate cancer: a comparison with prostate-specific antigen across five randomized Phase III clinical trials. J Clin Oncol. 2018;36:572–80.
Wang C, Zhang Z, Chong W, Luo R, Myers RE, Gu J, et al. Improved prognostic stratification using circulating tumor cell clusters in patients with metastatic castration-resistant prostate cancer. Cancers. 2021;13:268.
van der Toom EE, Axelrod HD, de la Rosette JJ, de Reijke TM, Pienta KJ, Valkenburg KC. Prostate-specific markers to identify rare prostate cancer cells in liquid biopsies. Nat Rev Urol. 2019;16:7–22.
Antonarakis ES, Lu C, Wang H, Luber B, Nakazawa M, Roeser JC, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl J Med. 2014;371:1028–38.
Antonarakis ES, Lu C, Luber B, Wang H, Chen Y, Zhu Y, et al. Clinical significance of androgen receptor splice variant-7 mRNA detection in circulating tumor cells of men with metastatic castration-resistant prostate cancer treated with First- and Second-Line Abiraterone and Enzalutamide. J Clin Oncol. 2017;35:2149–56.
Nagaya N, Nagata M, Lu Y, Kanayama M, Hou Q, Hotta ZU, et al. Prostate-specific membrane antigen in circulating tumor cells is a new poor prognostic marker for castration-resistant prostate cancer. PLoS One. 2020;15:e0226219.
Francolini G, Loi M, Ciccone LP, Detti B, Di Cataldo V, Pinzani P, et al. Prospective assessment of AR splice variant and multi-biomarker expression on circulating tumor cells of mCRPC patients undergoing androgen receptor targeted agents: interim analysis of PRIMERA trial (NCT04188275). Med Oncol. 2022;39:119.
Nuhn P, De Bono JS, Fizazi K, Freedland SJ, Grilli M, Kantoff PW, et al. Update on systemic prostate cancer therapies: management of metastatic castration-resistant prostate cancer in the era of precision oncology. Eur Urol. 2019;75:88–99.
Xu J, Kalos M, Stolk JA, Zasloff EJ, Zhang X, Houghton RL, et al. Identification and characterization of prostein, a novel prostate-specific protein. Cancer Res. 2001;61:1563–8.
Sheridan T, Herawi M, Epstein JI, Illei PB. The role of P501S and PSA in the diagnosis of metastatic adenocarcinoma of the prostate. Am J Surg Pathol. 2007;31:1351–5.
Ried K, Tamanna T, Matthews S, Eng P, Sali A. New screening test improves detection of prostate cancer using circulating tumor cells and prostate-specific markers. Front Oncol. 2020;10:582.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials working Group 3. J Clin Oncol. 2016;34:1402–18.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Casanova-Salas I, Athie A, Boutros PC, Del Re M, Miyamoto DT, Pienta KJ, et al. Quantitative and qualitative analysis of blood-based liquid biopsies to inform clinical decision-making in prostate cancer. Eur Urol. 2021;79:762–71.
Scher HI, Graf RP, Schreiber NA, Jayaram A, Winquist E, McLaughlin B, et al. Assessment of the validity of nuclear-localized androgen receptor splice variant 7 in circulating tumor cells as a predictive biomarker for castration-resistant prostate cancer. JAMA Oncol. 2018;4:1179–86.
De Laere B, Oeyen S, Mayrhofer M, Whitington T, van Dam PJ, Van Oyen P, et al. TP53 outperforms other androgen receptor biomarkers to predict Abiraterone or Enzalutamide outcome in metastatic castration-resistant prostate cancer. Clin Cancer Res. 2019;25:1766–73.
Tommasi S, Pilato B, Carella C, Lasorella A, Danza K, Vallini I, et al. Standardization of CTC AR-V7 PCR assay and evaluation of its role in castration resistant prostate cancer progression. Prostate. 2019;79:54–61.
Uhlen M, Fagerberg L, Hallstrom BM, Lindskog C, Oksvold P, Mardinoglu A, et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347:1260419.
Yin M, Dhir R, Parwani AV. Diagnostic utility of p501s (prostein) in comparison to prostate specific antigen (PSA) for the detection of metastatic prostatic adenocarcinoma. Diagn Pathol. 2007;2:41.
Chuang AY, DeMarzo AM, Veltri RW, Sharma RB, Bieberich CJ, Epstein JI. Immunohistochemical differentiation of high-grade prostate carcinoma from urothelial carcinoma. Am J Surg Pathol. 2007;31:1246–55.
Srinivasan M, Parwani AV. Diagnostic utility of p63/P501S double sequential immunohistochemical staining in differentiating urothelial carcinoma from prostate carcinoma. Diagn Pathol. 2011;6:67.
Epstein JI, Egevad L, Humphrey PA, Montironi R, Members of the IIiDUPG. Best practices recommendations in the application of immunohistochemistry in the prostate: report from the International society of urologic pathology consensus conference. Am J Surg Pathol. 2014;38:e6–e19.
Mochizuki K, Kawai M, Odate T, Tahara I, Inoue T, Kasai K, et al. Diagnostic utility of prostein, Uroplakin II and SATB2 for diagnosing carcinoma of unknown primary origin: a systematic immunohistochemical profiling. Anticancer Res. 2018;38:4759–66.
Musiyenko A, Bitko V, Barik S. Ectopic expression of miR-126*, an intronic product of the vascular endothelial EGF-like 7 gene, regulates prostein translation and invasiveness of prostate cancer LNCaP cells. J Mol Med. 2008;86:313–22.
Kiessling A, Wehner R, Fussel S, Bachmann M, Wirth MP, Schmitz M. Tumor-associated antigens for specific immunotherapy of prostate cancer. Cancers. 2012;4:193–217.
Pin E, Henjes F, Hong MG, Wiklund F, Magnusson P, Bjartell A, et al. Identification of a Novel autoimmune peptide epitope of prostein in prostate cancer. J Proteome Res. 2017;16:204–16.
Kiessling A, Stevanovic S, Fussel S, Weigle B, Rieger MA, Temme A, et al. Identification of an HLA-A*0201-restricted T-cell epitope derived from the prostate cancer-associated protein prostein. Br J Cancer. 2004;90:1034–40.
Perner S, Rupp NJ, Braun M, Rubin MA, Moch H, Dietel M, et al. Loss of SLC45A3 protein (prostein) expression in prostate cancer is associated with SLC45A3-ERG gene rearrangement and an unfavorable clinical course. Int J Cancer. 2013;132:807–12.
Hernandez-Llodra S, Juanpere N, de Muga S, Lorenzo M, Gil J, Font-Tello A, et al. ERG overexpression plus SLC45A3 (prostein) and PTEN expression loss: strong association of the triple hit phenotype with an aggressive pathway of prostate cancer progression. Oncotarget. 2017;8:74106–18.
Payne H, Cornford P. Prostate-specific antigen: an evolving role in diagnosis, monitoring, and treatment evaluation in prostate cancer. Urol Oncol. 2011;29:593–601.
Cornford P, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II-2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol. 2021;79:263–82.
Kristiansen I, Stephan C, Jung K, Dietel M, Rieger A, Tolkach Y, et al. Sensitivity of HOXB13 as a diagnostic immunohistochemical marker of prostatic origin in prostate cancer metastases: comparison to PSA, prostein, androgen receptor, ERG, NKX3.1, PSAP, and PSMA. Int J Mol Sci. 2017;18:1151.
Rice MA, Malhotra SV, Stoyanova T. Second-generation antiandrogens: from discovery to standard of care in castration resistant prostate cancer. Front Oncol. 2019;9:801.
Funding
This study was supported by National Cancer Institute grants R01CA255792, R01CA244749 and P20CA233255, the American Cancer Society Institutional Research Grant IRG-21-138-13-IRG, the Philadelphia Prostate Cancer Biome Projects, and funding from the Sidney Kimmel Cancer Center of Thomas Jefferson University. Research reported in this publication utilized the Circulating Tumor Cell Core Facility at the Sidney Kimmel Cancer Center at Jefferson Health and was supported by the National Cancer Institute of the National Institutes of Health under Award Number P30CA056036. The funding agencies were not involved in the design, conduct, analysis or interpretation of the study.
Author information
Authors and Affiliations
Contributions
Study concept and design: HY, CW, ZZ; Acquisition of data: ZZ, JC, SD; Analysis and interpretation of data: HY, CW, WKK, NRH, WJT; Drafting of the manuscript: ZZ, CW, JC, KI; Critical revision of the manuscript for important intellectual content: WJT, FJK, MLT; Statistical analysis: RL, JC, CW; Obtaining funding: HY, WKK, GL-Y, CW; Administrative, technical, or material support: WKK, RM, JL, JG, BL; Supervision: HY.
Corresponding authors
Ethics declarations
Competing interests
HY is on the SAB of Oriomics Inc., a shareholder of Illumina, Pfizer, and Oriomics, and serves as a NIH study section reviewer. WKK is the consultant/SAB of Janssen, Bayer, and Merck-Sharpe Dome. The above reported activities were not related to the research reported in this article. All other authors did not report any competing interests related to the research reported in this article.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Luo, R., Kelly, W.K. et al. Prostein expression on circulating tumor cells as a prognostic marker in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00762-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00762-3