Abstract
Background
Nearly one-third of patients with prostate cancer (PCa) experience biochemical recurrence (BCR) after primary definitive treatment. BCR increases the risk of distant metastasis and mortality in patients with prognostically unfavorable features. These patients are best managed with a tailored treatment strategy incorporating risk stratification using clinicopathological factors, next-generation imaging, and genomic testing.
Objective
This narrative review examines the utility of risk stratification for the management of patients with BCR in the context of clinical trial data, referencing the latest recommendations by European and US medical societies.
Methods
PubMed was searched for relevant studies published through May 21 2023 on treatment of patients with BCR after radical prostatectomy (RP) or external beam radiotherapy (EBRT).
Results
European and US guidelines support the risk-stratified management of BCR. Post-RP, salvage EBRT (with or without androgen deprivation therapy [ADT]) is an accepted treatment option for patients with BCR. Post-EBRT, local salvage therapies (RP, cryotherapy, high-intensity focused ultrasound, stereotactic body radiotherapy, and low-dose-rate and high-dose-rate brachytherapy) have demonstrated comparable relapse-free survival rates but differing adverse event profiles, short and long term. Local salvage therapies should be used for local-only relapses while ADT should be considered for regional or distant relapses. In practice, patients often receive ADT, with varying guidance for intermittent ADT vs. continuous ADT, due to consideration of quality-of-life effects.
Conclusions
Despite a lack of consensus for BCR treatment among guideline associations and medical societies, risk stratification of patients is essential for personalized treatment approaches, as it allows for an informed selection of therapeutic strategies and estimation of adverse events. In lower-risk disease, observation is recommended while in higher-risk disease, after failed repeat local therapy, ADT and/or clinical trial enrollment may be appropriate. Results from ongoing clinical studies of patients with BCR should provide consensus for management.
Similar content being viewed by others
Introduction
In 2020, prostate cancer (PCa) was the second most common malignancy diagnosed in men with an incidence of 1414259 cases worldwide, representing 7.3% of all new cancers globally [1]. Older age, African American race, and a family history of PCa are established risk factors [2]. For patients with more aggressive localized disease, and when intervention is recommended, several options exist, including but not limited to radical prostatectomy (RP) and external beam radiation therapy (EBRT). Despite early intervention, 20–50% of men with PCa will develop biochemical recurrence (BCR) within 10 years after initial definitive therapy, characterized by a rising serum prostatic-specific antigen (PSA) [3, 4]. Of note, BCR can represent local recurrence and increases the risk of metastasis and PCa-specific mortality (PCSM) in patients with prognostically unfavorable pre- and post-treatment clinicopathological factors, including a high Gleason score (GS) and a short PSA doubling time (PSADT) [5,6,7]. Thus, patients with BCR would be best managed with a tailored treatment strategy that incorporates risk stratification using pathological grade group, PSADT, conventional imaging, molecular targeted imaging (MTI), also referred to as next-generation imaging, and possibly genomic testing [8,9,10]. The application of MTI in the diagnostic evaluation and management of patients with BCR will be discussed in a companion review.
Over the last decade, there has been important progress in the personalized management of BCR [11,12,13]. However, there is a current lack of consensus among guideline associations and medical societies regarding the most effective treatments for BCR. In the absence of this guidance, it is important for the uro-oncology community to be aware of the latest clinical evidence.
This narrative review comprehensively evaluates clinical trial data to summarize treatment approaches for BCR, including lifestyle interventions. Of note, we focused on BCR after whole gland treatment. We also discuss the extent to which clinicians apply guideline recommendations and impact of risk stratification on patient management, with reference to the latest recommendations by the American Urology Association/American Society for Radiation Oncology/Society of Urologic Oncology (AUA/ASTRO/SUO), American Society of Clinical Oncology (ASCO), European Association of Urology/European Association of Nuclear Medicine/European Society for Radiotherapy & Oncology/European Society of Urogenital Radiology/International Society of Urological Pathology/International Society of Geriatric Oncology (EAU/EANM/ESTRO/ESUR/ISUP/SIOG) and National Comprehensive Cancer Network® (NCCN®) [8, 9, 14,15,16].
Methods
A comprehensive search was conducted through PubMed to identify relevant publications on treatment strategies in patients with BCR and negative conventional imaging, with a particular focus on prospective clinical trials. Searches were conducted through May 21, 2023, with no date restriction. All searches were supplemented by examining reference lists in all relevant publications to identify additional articles for inclusion. The literature search was limited to English-language publications in peer-reviewed journals using the following Medical Subject Headings (MeSH) terms and keywords: ‘prostate neoplasms’; ‘biochemical recurrence’; ‘treatment’. To be eligible for inclusion in this review, the identified records must be reporting or providing recommendations on the risk stratification approaches, salvage treatment options, or lifestyle interventions in adult men with BCR. Database searches yielded 432 articles, of which 95 were included in this review after title/abstract screening and full-text selection.
Results
Biochemical recurrence following whole-gland treatment
Traditionally, BCR is defined by a rising serum PSA after primary definitive therapy without conventional imaging (computed tomography and bone scan) evidence of metastasis [17]. However, PSA is not cancer-specific and recurrent benign prostate growth after EBRT or other minimally invasive therapies and, rarely, residual benign prostate tissue remaining in situ post-RP can generate false positives [18, 19]. Therefore, confirmation of BCR prior to treatment is crucial to prevent unnecessary treatment. Despite the existing evidence on the ability of ultrasensitive PSA testing in determining BCR and informing salvage treatment at concentrations ≤0.1 ng/ml post-RP [20,21,22], the clinical utility of low-detectable PSA values is a matter of debate and the consensus is lacking for the optimal PSA threshold for initiating therapy post-RP; medical societies have proposed several criteria for establishing BCR and monitoring of serum PSA levels after initial definitive therapy (Table 1) [9, 14, 23, 24]. In general, BCR is classified as PSA increases above 0.1 ng/ml post-RP [9, 14]. Post-RP, the failure of PSA to decline to undetectable levels is defined as PSA persistence [9], biologically representing potentially larger residual cancer burden compared with PSA recurrence [25]. Post-EBRT, consensus exists among medical societies that BCR is defined as nadir +2.0 ng/ml [9, 14].
Risk stratification in patients with BCR
The inherent heterogeneity of BCR presents challenges for optimal disease management, particularly in the context of monitoring treatment response in patients with negative conventional imaging [17]. Given the prognostic value of clinicopathological and genomic parameters in BCR, risk stratification is essential for a personalized approach to the treatment of patients who experience BCR [6, 26, 27]. One of the strongest predictors of metastasis and death is PSADT, a mathematical determination of the time in months required for PSA to increase two-fold in an individual patient [28]. In patients with BCR post-RP, the risk of metastasis and PCSM decrease significantly from the lowest (<3 months) to the highest (≥15 months) PSADT levels [3, 6, 29]. Higher GSs are also strong positive predictors of distant metastatic recurrence, PCSM, and overall mortality in men who develop BCR [5]. In this context, European guidelines suggest that patients with BCR should be stratified by risk of disease progression prior to commencing additional treatment; classifying patients with BCR post-RP as high-risk of disease progression if they have either a PSADT ≤ 1 yr or GS 8–10 and low-risk with a PSADT > 1 yr and GS < 8 [15]. Post-EBRT, patients are defined as high-risk for disease progression if they have either biochemical failure (IBF) ≤ 18 mo or GS 8–10 and defined as low-risk if the interval from primary therapy to IBF > 18 mo and GS < 8 [30]. ASCO and NCCN recommend patients with BCR post-RP and post-EBRT should be stratified by risk of disease progression prior to commencing additional treatment [8, 9]. Based on the findings from a meta-analysis of studies with 44630 patients who underwent either RP or RT [5], the ASCO 2021 guideline update classifies patients with BCR post-RP as high-risk for disease progression if they have either a PSADT ≤ 1 year or a pathologic GS 8–10 (identified on prostatectomy histology report), and low risk if they have both a PSADT > 1 year and a GS < 8 [5, 8]. Post-RT, high-risk BCR is defined as an interval to BCR ≤ 18 months or a clinical GS 8–10 (identified on prostate biopsies), whereas low-risk BCR is defined as an interval to BCR > 18 months and a GS < 8 [5, 8]. Additionally, the NCCN and AUA/ASTRO/SUO guidelines recommend that genomic testing can contribute to development of a patient’s overall risk profile for recurrence [9, 23]. Post-RP, genomic tests that contribute to patient management by assessing expression levels of RNA include Decipher® (Decipher Biosciences Inc., San Diego, CA, USA; 22 genes) [31]. Multivariable analysis of 23 studies (n = 12600) demonstrated that the Decipher genomic classifier (GC) score was independently prognostic for biochemical failure, distant metastasis, and PCSM, and improved discrimination of these endpoints over standard of care [32]. In addition, in the G-MINOR multicenter, randomized trial of post-RP patients with PSA < 0.1 ng/ml, a high GC score in the GC arm (n = 175) significantly increased the probability of adjuvant treatment (OR 8.8, 95% CI 1.9–39.7, p = 0.005) [33].
Treatment recommendations for patients with BCR after primary definitive therapy
Salvage EBRT after RP
Salvage EBRT (sEBRT) is potentially curative and may delay the need for chronic, non-curative treatments, such as long-term androgen deprivation therapy (ADT) [12]. Notably, adjuvant EBRT (aEBRT) and early sEBRT have shown comparable efficacy in prospective trials; however, aEBRT has been associated with a higher rate of adverse events (AEs), particularly acute and late grade ≥2 genitourinary toxicity and grade ≥2 erectile dysfunction [34,35,36]. Furthermore, retrospective studies have demonstrated that early sEBRT can decrease the risk of all-cause mortality (ACM) and PCSM in patients with BCR [30, 37, 38]. Prognostic factors associated with oncologic outcomes following sEBRT are PSA levels at the time of sEBRT and PSADT [30, 39]. In a retrospective analysis of 5509 men, 1497 of whom experienced BCR (rising PSA ≥ 0.2 ng/ml from two consecutive measurements), early sEBRT (PSA < 0.5 ng/ml) was more effective in reducing the risk of metastatic progression (hazard ratio [HR] 0.32, 95% CI 0.20–0.53; p ≤ 0.001) compared with late sEBRT (PSA ≥ 0.5 ng/ml) (HR 0.56, 95% CI 0.35–0.88; p = 0.01) [30]. Similarly, the risk of PCSM was significantly lower following early sEBRT (HR 0.31, 95% CI 0.15–0.62; p ≤ 0.001) compared with late sEBRT (HR 0.58, 95% CI 0.32–1.04; p = 0.07) [30]. Additionally, a prospective institutional real-world study of patients with post-RP BCR from two treatment sites in Germany and the US (1990‒2020) found significant associations between pre-sEBRT PSA cutoffs (>0.10 to ≤0.50 ng/ml) and ACM, reporting a higher 10-year ACM risk estimate with sEBRT at PSA levels >0.25 ng/ml versus ≤0.25 ng/ml (HR 1.49, 95% CI 1.11–2.00; p = 0.008) [38].
The European guideline recommends sEBRT for patients classified as high-risk BCR and PSA levels ≤0.5 ng/ml [16]. The AUA/ASTRO/SUO guidelines recommend that patients should be informed that sEBRT for BCR is most effective at PSA levels <1.0 ng/ml [40]. Independent of clinical and pathological risk factors, Decipher risk classification has been shown to factor into the decision-making regarding the timing of treatment intensification for patients with BCR, such as sEBRT [41, 42]. Thus, the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) recommend patients with high GC scores (>0.6) should be strongly considered for EBRT and addition of ADT when the opportunity for early EBRT has been missed [9].
Combination ADT with sEBRT
sEBRT is often combined with ADT for the treatment of men with BCR. Preclinical studies demonstrated that androgen deprivation downregulates vascular endothelial growth factor, leading to apoptosis of endothelial cells and decreased vascularization, and also reduces the dose of EBRT required to control 50% of the tumor, providing a biological basis for combination treatment [43]. First-generation non-steroidal anti-androgens (NSAAs) combined with sEBRT have demonstrated a benefit in men with BCR. In the randomized RTOG 9601 trial of 760 men with BCR post-RP, 24-month treatment with high-dose bicalutamide (150 mg daily) in combination with sEBRT resulted in significantly increased overall survival (OS) rates (p = 0.04) [13]. However, improvements in OS were not identified until >10 years of follow-up. Subsequent analyses from this trial showed that the benefit to adding bicalutamide was only observed in patients with a pre-EBRT PSA > 0.6 ng/ml [44]. Indeed, in patients with lower PSA values, bicalutamide had no benefit and actually increased other-cause mortality (p = 0.01) [44], further highlighting the importance of risk stratification as well as potential risks of unwarranted treatment intensification. Nonetheless, given the delay until benefits are observed, life expectancy (LE) is an important factor for patients considering hormone therapy [17]. LE can be estimated as the average number of years of life remaining for persons at a certain age using the life table functions developed by the National Vital Statistics System [45]. The life table functions use national data on death and population counts to calculate LE based on the number of survivors and the number of person-years lived at and above a given age [45]. For patients with shorter LE even with severe disease, observation can be the best option. In the GETUG-AFU 16 prospective, phase 3 trial, 6 months of treatment with goserelin plus sEBRT significantly improved 9-year progression-free survival (p < 0.001) and metastasis-free survival (MFS; p = 0.034) compared with sEBRT alone [46]. Of note, the progression-free survival benefit of combined sEBRT and ADT was observed both in the high-risk (GS 8–10, T3 disease, and/or positive margins) and the low-risk subgroups (p < 0.001 and p = 0.004, respectively). In contrast, 9-year MFS was comparable between sEBRT+ADT and sEBRT alone for both high-risk and low-risk groups. In addition to consideration of tumor-related factors to determine which patients would benefit from sEBRT in combination with ADT, other patient-related factors that should be considered include comorbidities (frailty, heart disease, osteoporosis, and mental health) and LE [47].
Decipher was used to evaluate tumor samples from 486 patients with recurrent disease collected from RTOG 9601, the randomized trial of sEBRT vs. sEBRT with bicalutamide described above [48]. Adjusted for age, race/ethnicity, GS, T stage, margin status, baseline PSA, and treatment cohort, multivariable analysis demonstrated the GC score (continuous variable, per 0.1 unit) was independently associated with risk of distant metastasis (HR 1.17, 95% CI 1.05–1.32, p = 0.006), PCSM (HR 1.39, 95% CI 1.20–1.63, p < 0.001), and OS (HR 1.17, 95% CI 1.06–1.29, p = 0.002). Furthermore, the 12-year benefit provided by ADT improved OS three-fold in patients with intermediate- and high-risk GC scores compared with low-risk GC scores (8.9% vs. 2.4%). In addition, the patients who received early sEBRT (PSA < 0.7 ng/ml) in combination with ADT with high vs. low GC scores experienced benefits in 12-year risk of developing distant metastasis (11% vs. 0.4%), PCSM (8.4% vs. 1.0%), and OS (4.6% vs. –7.8%). Importantly, patients with low-risk GC scores who would not benefit clinically from treatment intensification could also be identified. Overall, these results demonstrated that genomic profiling may identify patients with BCR, independent of PSA level, who would or would not benefit from sEBRT+ADT combination relative to sEBRT alone.
Surgical and non-surgical salvage treatments after definitive EBRT
A number of surgical and non-surgical salvage treatments have been proposed for histologically confirmed localized BCR post-EBRT that include salvage RP (sRP), cryotherapy, high-intensity focused ultrasound (HIFU), stereotactic body radiotherapy (SBRT), and low-dose-rate (LDR) and high-dose-rate (HDR) brachytherapy. Meta-analyses of these treatments demonstrated comparable relapse-free survival rates at 5 years, ranging from <50% with HIFU to approximately 60% with SBRT, cryotherapy, and HDR brachytherapy, while 2-year relapse-free survival rate was significantly lower with HIFU compared with sRP (52% vs. 72%; p < 0.001) [49]. The best candidates for re-irradiation with brachytherapy or SBRT have good urinary function and performance status.
In RTOG 0526, LDR brachytherapy re-irradiation was associated with a 14% risk (95% CI 6–21) of late treatment-related grade ≥3 gastrointestinal/genitourinary toxicity [50]. Comparable rates of grade ≥2 genitourinary toxicity resulting from HDR brachytherapy and SBRT have been reported [26, 51,52,53]. Historically, open sRP has been associated with poor functional outcomes and high complication rates; however, robot-assisted sRP demonstrated reduced adverse outcomes (anastomotic and/or urethral strictures, 16.6% vs. 7.7%, p = 0.007) and significant improvements in blood loss and duration of hospital stay (both, p < 0.001) compared with open sRP [54]. In patients from both groups who were continent at baseline, urinary continence remained unchanged or improved in 57% of patients, and 24.6% of patients experienced severe incontinence defined as ≥3 pads per day [54]. Thus, European guidelines recommend sRP should only be considered for patients with few comorbidities and LE of ≥10 yrs, pre-sRP PSA < 10 ng/ml with no lymph node involvement or evidence of metastatic disease, and at initial diagnosis, GS ≤ 8 and clinical stage T1 or T2 [16]. NCCN Guidelines® recommend sRP (with pelvic lymph node dissection [LND]) as an option for highly selected patients with local recurrence after EBRT, brachytherapy, or cryotherapy in the absence of metastases [9]. Notably, sRP should be performed in experienced centers or as part of a clinical trial. According to NCCN guidelines, pelvic salvage LND (sLND) can be considered for patients with BCR and pelvic recurrence post-EBRT [9]. Single-center retrospective studies have reported encouraging survival outcomes for sLND in the post-RP node-recurrent setting [55, 56]; however, a retrospective analysis of multi-institutional data did not support the long-term clinical benefits of sLND in patients with MTI-detected post-RP nodal recurrence, with 36% and 34% probability of ACM and PCSM at 10 years, respectively [57]. Cryotherapy and HIFU are other local treatments recommended by European and NCCN guidelines for BCR post-EBRT in the absence of metastasis [9]. LE > 5 years, low or intermediate D’Amico risk category, and low pre-EBRT PSA level are factors associated with improved OS after HIFU [58].
Systemic treatment options
Strategies for BCR disease management include first- and second-generation ADT (with or without EBRT) as well as lifestyle interventions. NSAAs competitively inhibit the action of androgens by binding to cytosolic androgen receptors in the target tissue [59]. ADT blocks the release of hormones, such as luteinizing hormone-releasing hormone, and reduces both the rate of testicular androgen synthesis and levels of circulating androgens [60]. Androgen-sensitive PCa responds to treatment that counteracts the effect of androgen and/or removes its source. There is no consensus on the benefit of salvage ADT alone following BCR, therefore, the risk of AEs must be carefully assessed and discussed. A systematic review evaluating the effectiveness of ADT alone for BCR determined that ADT may be appropriate for men with a high risk of disease progression (PSADT < 6–12 months; GS > 7) and long LE [61]. The European and NCCN Guidelines are consistent with the outcomes of this review [9, 16]. The AUA/ASTRO/SUO guidelines suggest that men with high-risk BCR should only be recommended intermittent ADT with no evidence of metastasis [14]. These guidelines also recommend that these men be offered clinical trial enrollment or observation [14]. Despite its potential clinical benefits, ADT is associated with significant AEs, and its long-term use may contribute to an impaired quality of life (QoL), including depression, fatigue, hot flashes, and sexual dysfunction [62]. Long-term ADT also is associated with an increased risk of cardiovascular disease, diabetes mellitus, and osteoporosis [63,64,65,66]. Furthermore, ADT can confound PCa tumor imaging and detection [67].
Peripheral androgen blockade
NSAAs in combination with 5α-reductase inhibitors, such as finasteride, have been evaluated for delaying ADT initiation in BCR [68,69,70]. In a study of 37 patients with BCR treated with bicalutamide and finasteride, the median time to progression to ADT was 37.6 months (interquartile range [IQR] 20–75), and from the start of treatment the median time to castration resistance was 49.8 months (IQR 41–not reached). NSAAs plus 5α-reductase inhibitor combinations are not currently recommended in the guidelines, but may be considered for patients who are older and unfit, or carefully selected patients who want to avoid the toxicities of castration therapy [71].
Timing of ADT
The TOAD trial investigated the impact of delayed vs. immediate ADT treatment on OS in 293 men, of whom 261 experienced PSA relapse after curative therapy [72]. The 5-year OS was modestly increased in the immediate therapy arm vs. the delayed therapy arm (91% vs. 86%, p = 0.047). The study also found that immediate therapy was associated with a lower incidence of local progression (13% vs. 20%) and a significantly longer time to local progression (adjusted HR 0.51; 95% CI 0.34–0.76; p = 0.001), compared with delayed therapy. Nonetheless, time to distant progression was not significantly different between the immediate and delayed therapy 1-year or 6-year follow-ups. Immediate therapy also was associated with minimal diminishment in QoL; however, an increased percentage of patients experienced serious AEs vs. delayed therapy (41% vs. 32%). Moreover, despite the stratification by PSADT, the study did not report the subgroup analysis on BCR-experiencing patients with shorter (<10 months) vs. longer (≥10 months) PSADT, limiting the application of these findings to the management of high-risk BCR. As the evidence published thus far only demonstrates a modest clinical benefit in OS for early ADT and that side effects associated with chronic ADT therapy are an important consideration, only high-risk patients should consider early ADT according to both NCCN and European guidelines (defined by shorter PSADT and long LE) [9, 16].
Intermittent ADT
Intermittent ADT (iADT) has been proposed as an option that may delay disease progression while providing relief from the AEs and complications associated with continuous dosing [11, 73]. The Canadian PR.7 study demonstrated the non-inferiority of iADT compared with continuous ADT (cADT) with respect to OS in patients (n = 1386) with BCR post-EBRT (≥3 ng/ml increase over nadir PSA) together with improved QoL improvements in the iADT cohort [11]. Due to a high number of deaths (59%) unrelated to PCa, a post hoc analysis of PCa-specific survival was also conducted showing non-comparable deaths from PCa or related causes in the iADT (n = 120) vs. the cADT (n = 94) group (p = 0.13) [11]. A meta-analysis of 15 clinical trials, representing 6856 men with PCa who underwent iADT or cADT, concluded that certain physical and sexual functions improved with iADT, but there were no major between-group differences in OS, time to castration resistance, QoL, or AEs despite a lower trend in point estimates for iADT [74]. For patients with nonmetastatic BCR, the NCCN Guidelines recommend iADT, with no specific recommendations for patient selection [9]. Alternatively, a consensus statement reached by an expert panel of US-based uro-oncologists recommended IADT should be only considered for high-risk patients (defined as PSADT ≤ 9 months and GS ≥ 8) with early BCR (<3 years); low- and intermediate-risk patients with BCR should undergo observation [73]. Consistent with this, the ASCO guidelines recommend that iADT may be offered to patients with high-risk BCR after RP (PSADT ≤ 1 year or a pathologic GS 8–10) or RT (interval to BCR ≤ 18 months or a clinical GS 8–10); active surveillance may be considered in those with low-risk BCR after RP (PSADT > 1 year and GS < 8) or RT (interval to BCR > 18 months and GS < 8) [8].
Second-generation androgen-targeted therapies
Second-generation antiandrogen therapies have been developed with increased androgen receptor specificity and affinity, compared with their NSAA predecessors [75]. Enzalutamide, the first characterized second-generation NSAA, improved OS in both nonmetastatic castration-resistant and metastatic castration-sensitive PCa [76, 77]. Notably, in the STAMPEDE trial (NCT00268476), patients with high-risk nonmetastatic castration-sensitive PCa (nmCSPC) who received abiraterone acetate plus prednisolone with or without enzalutamide plus ADT for 2 years demonstrated significantly improved MFS and OS (both p < 0.001), compared with ADT alone [78]. The further addition of enzalutamide did not impact efficacy outcomes, but increased grade ≥3 AEs (57% vs. 37%). In contrast, the global phase 3 EMBARK trial (NCT02319837) demonstrated significant and clinically meaningful improvements in MFS for patients with high-risk BCR (PSADT ≤ 9 months) and negative conventional imaging who received enzalutamide plus leuprolide (HR 0.42, 95% CI 0.30–0.61; p < 0.0001) or enzalutamide monotherapy (HR 0.63, 95% CI 0.46–0.87; p = 0.005) vs. placebo combined with leuprolide after a median follow-up of 60.7 months [79]. A summary of other ongoing clinical trials in patients with BCR is presented in Table 2.
Other treatment options
Lifestyle
Dietary polyphenols, such as curcumin, have demonstrated inhibition of PCa growth in preclinical models and may complement a treatment or prevention strategy in men with PCa [80]. In a randomized controlled trial, patients with BCR after localized treatment or metastases at diagnosis were given iADT [80]. At ADT discontinuation, men were randomized (1:1) and received either curcuminoid powder capsules (1440 mg/day for 6 months) or placebo. While there was no significant difference in ADT “off-treatment” time, curcumin treatment significantly lowered PSA progression rate compared with control (10% vs. 30%; p = 0.026) [80]. A phase 2, single-arm study found that polyphenol-rich pomegranate juice prolonged PSADT, compared with baseline [81]; however, subsequent randomized trials found no differences in on-study PSADT between low- and high-dose pomegranate extract and between pomegranate extract and placebo [82, 83]. As such, these data do not support the use of pomegranate juice/extract for patients with BCR. Whole food supplements containing polyphenols have also demonstrated significant improvements in PSA levels for patients with BCR [84]. Patients with BCR (n = 199) randomized to a polyphenol-rich whole food supplement containing pomegranate, green tea, broccoli, and turmeric or placebo for 6 months demonstrated significant differences in the percentage increase in PSA (15% vs. 79%; p < 0.001) and percentage of patients with stable or lower PSA at the end of the study (46% vs. 14%; p < 0.001) [84].
Lifestyle interventions, such as weight loss and low-carbohydrate (LCD) and low-fat diets, have been studied in patients with BCR without affecting PSA or PSADT [85, 86]. A study of 57 patients with BCR randomized to LCD (n = 30) or control (n = 27) demonstrated that an LCD over 6 months did not significantly impact PSADT (p = 0.31) [86]. However, a post hoc analysis adjusting for key baseline covariates, including baseline PSA, pre-study PSADT, and prior treatment, in addition to hemoconcentration during the study, found that PSADT was significantly lowered in the LCD group (p = 0.007) [86]. Larger prospective studies are warranted to evaluate the impact of LCD on PCa disease progression. An evaluation of all the various dietary and lifestyle changes employed to manage PCa is beyond the scope of this paper; however, this topic has been reviewed elsewhere [87, 88].
Discussion
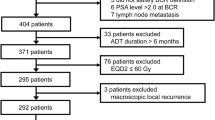
The treatment landscape of PCa has dramatically changed due to rapid therapeutic advancements, including MTI, genomic testing, and novel agents. While these developments are helpful, level-one evidence to guide clinicians prescribing treatment for BCR is lacking; thus clinical factors, such as PSADT, GS, and genomic testing can be applied to estimate the risk for PCa progression [73, 89]. A short PSADT (<9 months) is associated with increased risk of clinical progression, metastasis, and PCSM [3]. However, patients with BCR may require salvage treatment, and the decision-making must balance risk–benefit assessment (Fig. 1). Besides post-RP sEBRT, there are limited standard treatment options for men with BCR, and identifying optimal therapy remains an unmet need [9, 14]. Post-EBRT, salvage local therapies recommended for select patients include surgical and non-surgical options that have demonstrated similar relapse-free survival rates but differing AE profiles. For patients who have exhausted local treatment options, the AUA/ASTRO/SUO guidelines promote observation and clinical trial enrollment [14]. They do not recommend ADT and advise that, if used, it should be employed intermittently due to modest QoL improvements in patients with BCR. Second-generation anti-androgens have increased androgen specificity and affinity compared with their predecessors, with emerging phase 3 trial data demonstrating improved MFS following enzalutamide treatment in patients with high-risk BCR [76, 79, 90].
MTI will change the management of BCR and, in the future, may be as much of a stratification factor as PSADT, grade score, or genomic and molecular profiling. The results from three studies indicate that application of MTI to identify patients with BCR that would benefit from treatment may have a significant impact on patient outcomes, for example, the consideration of metastasis-directed therapy, thus specifically delaying the commencement of ADT [91,92,93]. The ultimate goal of treating BCR is to improve clinical outcomes with delayed disease progression and prolonged OS while minimizing AEs and preserving QoL. Thus, definition of BCR needs to evolve to match the increased sensitivity of PSA assays and MTI in detecting recurrence/metastasis at PSA levels below the traditional cutoffs.
In conclusion, despite a current lack of consensus for BCR treatment among guideline associations and medical societies, stratification of patients by risk is essential, assessing the potential AEs and clinical benefits of therapeutic strategies. According to the ASCO guidelines, active surveillance can be considered in low-risk BCR, whereas in higher-risk disease, iADT may be appropriate. European guidelines, AUA/ASTRO/SUO and NCCN recommend observation for select patients with BCR and no evidence of distant metastasis after RP or EBRT. Cryotherapy, HIFU, and, in selected patients, brachytherapy and sRP are local treatment options recommended for these patients by the European guidelines and NCCN. The AUA/ASTRO/SUO guidelines recommend early sEBRT for BCR post-RP, with the addition of ADT when early treatment is missed. The European guidelines and NCCN only recommend sEBRT for patients with BCR post-RP who have high-risk features. Additionally, early salvage ADT can be considered for higher risk patients with BCR and a long LE. Nevertheless, clinical data on the optimal treatment of patients with high-risk BCR after primary PCa treatment are limited. Results from ongoing clinical trials will address this unmet medical need and may provide additional treatment guidance.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Pernar CH, Ebot EM, Wilson KM, Mucci LA. The epidemiology of prostate cancer. Cold Spring Harb Perspect Med. 2018;8:a030361. https://doi.org/10.1101/cshperspect.a030361.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005;294:433–9.
Kupelian PA, Buchsbaum JC, Elshaikh M, Reddy CA, Zippe C, Klein EA. Factors affecting recurrence rates after prostatectomy or radiotherapy in localized prostate carcinoma patients with biopsy Gleason score 8 or above. Cancer. 2002;95:2302–7.
van den Broeck T, van den Bergh RCN, Arfi N, Gross T, Moris L, Briers E, et al. Prognostic value of biochemical recurrence following treatment with curative intent for prostate cancer: a systematic review. Eur Urol. 2019;75:967–87.
Antonarakis ES, Feng Z, Trock BJ, Humphreys EB, Carducci MA, Partin AW, et al. The natural history of metastatic progression in men with prostate-specific antigen recurrence after radical prostatectomy: long-term follow-up. BJU Int. 2012;109:32–39.
Zumsteg ZS, Spratt DE, Romesser PB, Pei X, Zhang Z, Polkinghorn W, et al. The natural history and predictors of outcome following biochemical relapse in the dose escalation era for prostate cancer patients undergoing definitive external beam radiotherapy. Eur Urol. 2015;67:1009–16.
Virgo KS, Rumble RB, de Wit R, Mendelson DS, Smith TJ, Taplin ME, et al. Initial management of noncastrate advanced, recurrent, or metastatic prostate cancer: ASCO Guideline Update. J Clin Oncol. 2021;10:1274–305.
National Comprehensive Cancer Network. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Prostate Cancer V.1.2023. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Available at www.NCCN.org. 2022.
Crawford ED, Harris RG, Slovin SF, Concepcion RS, Albala DM, Gomella LG, et al. Synthesizing and Applying Molecular Targeted Imaging Results in Patients With Prostate Cancer (RADAR VII). JU Open Plus. 2023;1.
Crook JM, O’Callaghan CJ, Duncan G, Dearnaley DP, Higano CS, Horwitz EM, et al. Intermittent androgen suppression for rising PSA level after radiotherapy. N Engl J Med. 2012;367:895–903.
Carrie C, Hasbini A, de Laroche G, Richaud P, Guerif S, Latorzeff I, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): a randomised, multicentre, open-label phase 3 trial. Lancet Oncol. 2016;17:747–56.
Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without antiandrogen therapy in recurrent prostate cancer. N Engl J Med. 2017;376:417–28.
Lowrance WT, Breau RH, Chou R, Chapin BF, Crispino T, Dreicer R, et al. Advanced prostate cancer: AUA/ASTRO/SUO guideline PART I. J Urol. 2021;205:14–21.
van den Broeck T, van den Bergh RCN, Briers E, Cornford P, Cumberbatch M, Tilki D, et al. Biochemical recurrence in prostate cancer: the European Association of Urology Prostate Cancer Guidelines Panel recommendations. Eur Urol Focus. 2020;6:231–4.
Mottet N, Cornford P, van den Berg RCN, Briers E, Eberli D, De Meerleer G, et al. EAU - EANM - ESTRO - ESUR - ISUP - SIOG Guidelines on Prostate Cancer. 2023. https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-EANM-ESTRO-ESUR-ISUP-SIOG-Guidelines-on-Prostate-Cancer-2023_2023-03-27-131655_pdvy.pdf.
Spratt DE, McHugh DJ, Morris MJ, Morgans AK. Management of biochemically recurrent prostate cancer: ensuring the right treatment of the right patient at the right time. Am Soc Clin Oncol Educ Book. 2018;38:355–62.
Godoy G, Tareen BU, Lepor H. Does benign prostatic tissue contribute to measurable PSA levels after radical prostatectomy? Urology. 2009;74:167–70.
Makarewicz R, Lebioda A, Terlikiewicz J, Biedka M, Wiśniewski T. PSA bouncing after brachytherapy HDR and external beam radiation therapy: a study of 121 patients with minimum 5-years follow-up. J Contemp Brachytherapy. 2009;1:92–96.
Szymaniak JA, Washington SL, Cowan JE, Cooperberg MR, Lonergan PE, Nguyen HG, et al. The natural history of a delayed detectable PSA after radical prostatectomy. Prostate Cancer Prostatic Dis. 2023. https://doi.org/10.1038/s41391-022-00638-y.
Freedland SJ, Sutter ME, Dorey F, Aronson WJ. Defining the ideal cutpoint for determining PSA recurrence after radical prostatectomy. Prostate-specific antigen. Urology. 2003;61:365–9.
Chung JH, Jeong JY, Lee JY, Song W, Kang M, Sung HH, et al. Biochemical recurrence after radical prostatectomy according to nadir prostate specific antigen value. PLoS One. 2021;16:e0249709.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part i: risk stratification, shared decision making, and care options. J Urol. 2018;199:683–90.
Trabulsi EJ, Rumble RB, Jadvar H, Hope T, Pomper M, Turkbey B, et al. Optimum imaging strategies for advanced prostate cancer: ASCO guideline. J Clin Oncol. 2020;38:1963–96.
Wu S, Lin SX, Cornejo KM, Crotty RK, Blute ML, Dahl DM, et al. Clinicopathological and oncological significance of persistent prostate-specific antigen after radical prostatectomy: a systematic review and meta-analysis. Asian J Urol. 2022;10:317–28.
Wu X, LV D, Eftekhar M, Khan A, Cai C, Zhao Z, et al. A new risk stratification system of prostate cancer to identify high-risk biochemical recurrence patients. Transl Androl Urol. 2020;9:2572–86.
Pierorazio PM, Ross AE, Lin BM, Epstein JI, Han M, Walsh PC, et al. Preoperative characteristics of high-Gleason disease predictive of favourable pathological and clinical outcomes at radical prostatectomy. BJU Int. 2012;110:1122–8.
Patel A, Dorey F, Franklin J, deKernion JB. Recurrence patterns after radical retropubic prostatectomy: clinical usefulness of prostate specific antigen doubling times and log slope prostate specific antigen. J Urol. 1997;158:1441–5.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Death in patients with recurrent prostate cancer after radical prostatectomy: prostate-specific antigen doubling time subgroups and their associated contributions to all-cause mortality. J Clin Oncol. 2007;25:1765–71.
Tilki D, Preisser F, Graefen M, Huland H, Pompe RS. External validation of the European Association of Urology biochemical recurrence risk groups to predict metastasis and mortality after radical prostatectomy in a European cohort. Eur Urol. 2019;75:896–900.
Erho N, Crisan A, Vergara IA, Mitra AP, Ghadessi M, Buerki C, et al. Discovery and validation of a prostate cancer genomic classifier that predicts early metastasis following radical prostatectomy. PLoS One. 2013;8:e66855.
Jairath NK, Dal Pra A, Vince R Jr., Dess RT, Jackson WC, Tosoian JJ, et al. A systematic review of the evidence for the decipher genomic classifier in prostate cancer. Eur Urol. 2021;79:374–83.
Morgan TM, Okoth LA, Spratt DE, Dunn R, Feng FY, Johnson AM, et al. Prospective randomized trial of gene expression classifier utility following radical prostatectomy (G-MINOR). J Clin Oncol. 2021;39:15–15.
Kneebone A, Fraser-Browne C, Duchesne GM, Fisher R, Frydenberg M, Herschtal A, et al. Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy (TROG 08.03/ANZUP RAVES): a randomised, controlled, phase 3, non-inferiority trial. Lancet Oncol. 2020;21:1331–40.
Sargos P, Chabaud S, Latorzeff I, Magné N, Benyoucef A, Supiot S, et al. Adjuvant radiotherapy versus early salvage radiotherapy plus short-term androgen deprivation therapy in men with localised prostate cancer after radical prostatectomy (GETUG-AFU 17): a randomised, phase 3 trial. Lancet Oncol. 2020;21:1341–52.
Parker CC, Clarke NW, Cook AD, Kynaston HG, Petersen PM, Catton C, et al. Timing of radiotherapy after radical prostatectomy (RADICALS-RT): a randomised, controlled phase 3 trial. Lancet. 2020;396:1413–21.
Trock BJ, Han M, Freedland SJ, Humphreys EB, DeWeese TL, Partin AW, et al. Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA. 2008;299:2760–9.
Tilki D, Chen M-H, Wu J, Huland H, Graefen M, Mohamad O, et al. Prostate-specific antigen level at the time of salvage therapy after radical prostatectomy for prostate cancer and the risk of death. J Clin Oncol. 2023;41:2428–35.
Tseng CS, Wang YJ, Chen CH, Wang SM, Huang KH, Chow PM, et al. Outcomes and prediction models for exclusive prostate bed salvage radiotherapy among patients with biochemical recurrence after radical prostatectomy. Cancers. 2021;13:2672.
Pisansky TM, Thompson IM, Valicenti RK, D’Amico AV, Selvarajah S. Adjuvant and salvage radiotherapy after prostatectomy: ASTRO/AUA guideline amendment 2018-29. J Urol. 2019;202:533.
Gore JL, du Plessis M, Zhang J, Dai D, Thompson DJS, Karsh L, et al. Clinical utility of a genomic classifier in men undergoing radical prostatectomy: the PRO-IMPACT trial. Pract Radiat Oncol. 2020;10:e82–e90.
Dal Pra A, Ghadjar P, Hayoz S, Liu VYT, Spratt DE, Thompson DJS, et al. Validation of the Decipher genomic classifier in patients receiving salvage radiotherapy without hormone therapy after radical prostatectomy - an ancillary study of the SAKK 09/10 randomized clinical trial. Ann Oncol. 2022;33:950–8.
Dal Pra A, Cury FL, Souhami L. Combining radiation therapy and androgen deprivation for localized prostate cancer-a critical review. Curr Oncol. 2010;17:28–38.
Dess RT, Sun Y, Jackson WC, Jairath NK, Kishan AU, Wallington DG, et al. Association of presalvage radiotherapy PSA levels after prostatectomy with outcomes of long-term antiandrogen therapy in men with prostate cancer. JAMA Oncol. 2020;6:735–43.
Arias E. United States life tables, 2008. Natl Vital Stat Rep. 2012;61:1–63.
Carrie C, Magné N, Burban-Provost P, Sargos P, Latorzeff I, Lagrange JL, et al. Short-term androgen deprivation therapy combined with radiotherapy as salvage treatment after radical prostatectomy for prostate cancer (GETUG-AFU 16): a 112-month follow-up of a phase 3, randomised trial. Lancet Oncol. 2019;20:1740–9.
Spratt DE, Dess RT, Zumsteg ZS, Lin DW, Tran PT, Morgan TM, et al. A systematic review and framework for the use of hormone therapy with salvage radiation therapy for recurrent prostate cancer. Eur Urol. 2018;73:156–65.
Feng FY, Huang H-C, Spratt DE, Zhao S, Sandler HM, Simko JP, et al. Validation of a 22-gene genomic classifier in patients with recurrent prostate cancer: an ancillary study of the NRG/RTOG 9601 randomized clinical trial. JAMA Oncol. 2021;7:544–52.
Valle LF, Lehrer EJ, Markovic D, Elashoff D, Levin-Epstein R, Karnes RJ, et al. A systematic review and meta-analysis of local salvage therapies after radiotherapy for prostate cancer (MASTER). Eur Urol. 2021;80:280–92.
Crook JM, Zhang P, Pisansky TM, Trabulsi EJ, Amin MB, Bice W, et al. A prospective phase 2 trial of transperineal ultrasound-guided brachytherapy for locally recurrent prostate cancer after external beam radiation therapy (NRG Oncology/RTOG-0526). Int J Radiat Oncol Biol Phys. 2019;103:335–43.
Pasquier D, Martinage G, Janoray G, Rojas DP, Zerini D, Goupy F, et al. Salvage stereotactic body radiation therapy for local prostate cancer recurrence after radiation therapy: a retrospective multicenter study of the GETUG. Int J Radiat Oncol Biol Phys. 2019;105:727–34.
Fuller D, Wurzer J, Shirazi R, Bridge S, Law J, Crabtree T, et al. Retreatment for local recurrence of prostatic carcinoma after prior therapeutic irradiation: efficacy and toxicity of HDR-like SBRT. Int J Radiat Oncol Biol Phys. 2020;106:291–9.
Wu SY, Wong AC, Shinohara K, Roach M, Cunha JAM, Valdes G, et al. Salvage high-dose-rate brachytherapy for recurrent prostate cancer after definitive radiation. Pract Radiat Oncol. 2021;11:515–26.
Gontero P, Marra G, Alessio P, Filippini C, Oderda M, Munoz F, et al. Salvage radical prostatectomy for recurrent prostate cancer: Morbidity and functional outcomes from a large multicenter series of open versus robotic approaches. J Urol. 2019;202:725–31.
Osmonov DK, Aksenov AV, Trick D, Naumann CM, Hamann MF, Faddan AA, et al. Cancer-specific and overall survival in patients with recurrent prostate cancer who underwent salvage extended pelvic lymph node dissection. BMC Urol. 2016;16:56.
Porres D, Pfister D, Thissen A, Kuru TH, Zugor V, Buettner R, et al. The role of salvage extended lymph node dissection in patients with rising PSA and PET/CT scan detected nodal recurrence of prostate cancer. Prostate Cancer Prostatic Dis. 2017;20:85–92.
Bravi CA, Fossati N, Gandaglia G, Suardi N, Mazzone E, Robesti D, et al. Long-term outcomes of salvage lymph node dissection for nodal recurrence of prostate cancer after radical prostatectomy: not as good as previously thought. Eur Urol. 2020;78:661–9.
Maestroni U, Tafuri A, Dinale F, Campobasso D, Antonelli A, Ziglioli F. Oncologic outcome of salvage high-intensity focused ultrasound (HIFU) in radiorecurrent prostate cancer. A systematic review. Acta Biomed. 2021;92:e2021191.
Siddiqui ZA, Krauss DJ. Adjuvant androgen deprivation therapy for prostate cancer treated with radiation therapy. Transl Androl Urol. 2018;7:378–89.
Harris WP, Mostaghel EA, Nelson PS, Montgomery B. Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol. 2009;6:76–85.
van den Bergh RC, van Casteren NJ, van den Broeck T, Fordyce ER, Gietzmann WK, Stewart F, et al. Role of hormonal treatment in prostate cancer patients with nonmetastatic disease recurrence after local curative treatment: a systematic review. Eur Urol. 2016;69:802–20.
Storey DJ, McLaren DB, Atkinson MA, Butcher I, Frew LC, Smyth JF, et al. Clinically relevant fatigue in men with hormone-sensitive prostate cancer on long-term androgen deprivation therapy. Ann Oncol. 2012;23:1542–9.
Lapi F, Azoulay L, Niazi MT, Yin H, Benayoun S, Suissa S. Androgen deprivation therapy and risk of acute kidney injury in patients with prostate cancer. JAMA. 2013;310:289–96.
Brawer MK. Hormonal therapy for prostate cancer. Rev Urol. 2006;8:S35–47.
Keating NL, O’Malley AJ, Freedland SJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy: observational study of veterans with prostate cancer. J Natl Cancer Inst. 2010;102:39–46.
Holzbeierlein JM, Castle E, Thrasher JB. Complications of androgen deprivation therapy: prevention and treatment. Oncology. 2004;18:303–9. discussion 310, 315, 319-21
Afshar-Oromieh A, Debus N, Uhrig M, Hope TA, Evans MJ, Holland-Letz T, et al. Impact of long-term androgen deprivation therapy on PSMA ligand PET/CT in patients with castration-sensitive prostate cancer. Eur J Nucl Med Mol Imaging. 2018;45:2045–54.
Reyes DK, Pienta KJ. Peripheral androgen blockade in men with castrate-sensitive biochemical recurrent prostate cancer. Med Oncol. 2021;38:80.
Bañez LL, Blake GW, McLeod DG, Crawford ED, Moul JW. Combined low-dose flutamide plus finasteride vs low-dose flutamide monotherapy for recurrent prostate cancer: a comparative analysis of two phase II trials with a long-term follow-up. BJU Int. 2009;104:310–4.
Monk JP, Halabi S, Picus J, Hussain A, Philips G, Kaplan E, et al. Efficacy of peripheral androgen blockade in prostate cancer patients with biochemical failure after definitive local therapy: results of cancer and leukemia group B (CALGB) 9782. Cancer. 2012;118:4139–47.
Sedhom R, Gupta A. Conceptual review of key themes in treating prostate cancer in older adults. J Geriatr Oncol. 2020;11:893–8.
Duchesne GM, Woo HH, Bassett JK, Bowe SJ, D’Este C, Frydenberg M, et al. Timing of androgen-deprivation therapy in patients with prostate cancer with a rising PSA (TROG 03.06 and VCOG PR 01-03 [TOAD]): a randomised, multicentre, non-blinded, phase 3 trial. Lancet Oncol. 2016;17:727–37.
Shore ND, Antonarakis ES, Cookson MS, Crawford ED, Morgans AK, Albala DM, et al. Optimizing the role of androgen deprivation therapy in advanced prostate cancer: challenges beyond the guidelines. Prostate. 2020;80:527–44.
Magnan S, Zarychanski R, Pilote L, Bernier L, Shemilt M, Vigneault E, et al. Intermittent vs continuous androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. JAMA Oncol. 2015;1:1261–9.
Rice MA, Malhotra SV, Stoyanova T. Second-generation antiandrogens: from discovery to standard of care in castration resistant prostate cancer. Front Oncol. 2019;9:801.
Sternberg CN, Fizazi K, Saad F, Shore ND, De Giorgi U, Penson DF, et al. Enzalutamide and survival in nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2020;382:2197–206.
Armstrong AJ, Azad AA, Iguchi T, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, et al. Improved survival with enzalutamide in patients with metastatic hormone-sensitive prostate cancer. J Clin Oncol. 2022;40:1616–22.
Attard G, Brown LC, Clarke N, Murphy L, Cross W, Jones R, et al. LBA4 Abiraterone acetate plus prednisolone (AAP) with or without enzalutamide (ENZ) added to androgen deprivation therapy (ADT) compared to ADT alone for men with high-risk non-metastatic (M0) prostate cancer (PCa): Combined analysis from two comparisons in the STAMPEDE platform protocol. Ann Oncol. 2021;32:S1298.
Shore ND, de Almeida Luz M, De Giorgi U, Gleave M, Gotto GT, Haas GP, et al. LBA02-09 EMBARK: a phase 3 randomized study of enzalutamide or placebo plus leuprolide acetate and enzalutamide monotherapy in high-risk biochemically recurrent prostate cancer. J Urol. 2023;209:e1190.
Choi YH, Han DH, Kim SW, Kim MJ, Sung HH, Jeon HG, et al. A randomized, double-blind, placebo-controlled trial to evaluate the role of curcumin in prostate cancer patients with intermittent androgen deprivation. Prostate. 2019;79:614–21.
Pantuck AJ, Leppert JT, Zomorodian N, Aronson W, Hong J, Barnard RJ, et al. Phase II study of pomegranate juice for men with rising prostate-specific antigen following surgery or radiation for prostate cancer. Clin Cancer Res. 2006;12:4018–26.
Pantuck AJ, Pettaway CA, Dreicer R, Corman J, Katz A, Ho A, et al. A randomized, double-blind, placebo-controlled study of the effects of pomegranate extract on rising PSA levels in men following primary therapy for prostate cancer. Prostate Cancer Prostatic Dis. 2015;18:242–8.
Paller CJ, Ye X, Wozniak PJ, Gillespie BK, Sieber PR, Greengold RH, et al. A randomized phase II study of pomegranate extract for men with rising PSA following initial therapy for localized prostate cancer. Prostate Cancer Prostatic Dis. 2013;16:50–55.
Thomas R, Williams M, Sharma H, Chaudry A, Bellamy P. A double-blind, placebo-controlled randomised trial evaluating the effect of a polyphenol-rich whole food supplement on PSA progression in men with prostate cancer–the U.K. NCRN Pomi-T study. Prostate Cancer Prostatic Dis. 2014;17:180–6.
Li Z, Aronson WJ, Arteaga JR, Hong K, Thames G, Henning SM, et al. Feasibility of a low-fat/high-fiber diet intervention with soy supplementation in prostate cancer patients after prostatectomy. Eur J Clin Nutr. 2008;62:526–36.
Freedland SJ, Allen J, Jarman A, Oyekunle T, Armstrong AJ, Moul JW, et al. A randomized controlled trial of a 6-month low-carbohydrate intervention on disease progression in men with recurrent prostate cancer: carbohydrate and prostate study 2 (CAPS2). Clin Cancer Res. 2020;26:3035–43.
Zuniga KB, Chan JM, Ryan CJ, Kenfield SA. Diet and lifestyle considerations for patients with prostate cancer. Urol Oncol. 2020;38:105–17.
Grammatikopoulou MG, Gkiouras K, Papageorgiou SΤ, Myrogiannis I, Mykoniatis I, Papamitsou T, et al. Dietary factors and supplements influencing prostate specific-antigen (PSA) concentrations in men with prostate cancer and increased cancer risk: an evidence analysis review based on randomized controlled trials. Nutrients. 2020;12:2985.
Spratt DE, Yousefi K, Deheshi S, Ross AE, Den RB, Schaeffer EM, et al. Individual patient-level meta-analysis of the performance of the decipher genomic classifier in high-risk men after prostatectomy to predict development of metastatic disease. J Clin Oncol. 2017;35:1991–8.
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2018;378:2465–74.
Jani AB, Schreibmann E, Goyal S, Halkar R, Hershatter B, Rossi PJ, et al. 18F-fluciclovine-PET/CT imaging versus conventional imaging alone to guide postprostatectomy salvage radiotherapy for prostate cancer (EMPIRE-1): a single centre, open-label, phase 2/3 randomised controlled trial. Lancet. 2021;397:1895–904.
Phillips R, Shi WY, Deek M, Radwan N, Lim SJ, Antonarakis ES, et al. Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: the ORIOLE phase 2 randomized clinical trial. JAMA Oncol. 2020;6:650–9.
Kroeze SGC, Henkenberens C, Schmidt-Hegemann NS, Vogel MME, Kirste S, Becker J, et al. Prostate-specific membrane antigen positron emission tomography-detected oligorecurrent prostate cancer treated with metastases-directed radiotherapy: role of addition and duration of androgen deprivation. Eur Urol Focus. 2021;7:309–16.
Sachdev S, Carroll P, Sandler H, Nguyen PL, Wafford E, Auffenberg G, et al. Assessment of postprostatectomy radiotherapy as adjuvant or salvage therapy in patients with prostate cancer: a systematic review. JAMA Oncol. 2020;6:1793–1800.
Sanda MG, Chen RC, Crispino T, Freedland SJ, Greene K, Klotz L, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline, 2017. 2017. https://www.auanet.org/documents/education/clinical-guidance/clinically-localized-prostate-cancer.pdf.
Acknowledgements
Medical writing and editorial support was provided by Roham Sadeghimakki, MD, PhD, Julie B. Stimmel, PhD, and Rosie Henderson, all of Onyx, (a Prime Global agency, London, UK) and funded by Pfizer, Inc. and Astellas Pharma, Inc., the co-developers of enzalutamide and sponsors of the EMBARK trial. The authors were involved in the collection and interpretation of information provided in the manuscript, and ultimate responsibility for opinions and conclusions lies with the authors.
Funding
Funded by Pfizer Inc. and Astellas Pharma Inc. Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Contributions
SJF had full access to the literature discussed in this review and takes responsibility for the interpretation and conclusions presented. Study concept and design: NDS, JWM, SJF. Acquisition of data: NDS, JWM, SJF. Analysis and interpretation of data: NDS, JWM, SJF. Drafting of manuscript: NDS, SJF. Reading and interpretation of literature: NDS, JWM, MTK, SJF. Critical revision of manuscript for important intellectual content: NDS, JWM, KJP, JC, MTK, SJF.
Corresponding author
Ethics declarations
Competing interests
NDS certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g. employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are as follows: NDS – grant support and consulting fees from AbbVie, Amgen, Astellas Pharma, AstraZeneca, Bayer, Clovis Oncology, Dendreon, Ferring, GenesisCare, Janssen Oncology, Merck, Myovant, Pfizer, Sanofi–Genzyme, and Tolmar Pharmaceuticals. JWM – stock or other ownership with Pfizer, Johnson & Johnson, Bavarian Nordic, Eli Lilly, Procter & Gamble, Walgreens, AstraZeneca, Novartis, and Theralogix; honoraria from AbbVie, Bayer, Ferring, Dendreon, Janssen, Astellas Pharma, Sanofi, Genomic Health, GenomeDx, and Pfizer; consulting or advisory role with AbbVie, Bayer, Theralogix, Tolmar, and Blue Earth Diagnostics; speakers’ bureau for Bayer, Ferring, Dendreon, Janssen, Sanofi, Genomic Health, and GenomeDx; research funding from Astellas Pharma (Inst) and Pfizer (Inst). KJP – founder, equity holder of Keystone Biopharma, Inc.; consultant with Cue Biopharma, Inc.; research funding from Progenics, Inc. JC – founder, equity holder of Sofie Biosciences and Trethera Therapeutics; advisory board member of Actinium, Actis, RayzeBio, and Jubillant. MTK – grant support and consulting fees from AstraZeneca, Bayer, and Palette Life Sciences. SJF – consultant to Astellas, AstraZeneca, Bayer, Dendreon Pharmaceuticals, Janssen, Merck, Myovant Sciences, Pfizer, and Sanofi.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shore, N.D., Moul, J.W., Pienta, K.J. et al. Biochemical recurrence in patients with prostate cancer after primary definitive therapy: treatment based on risk stratification. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00712-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00712-z
This article is cited by
-
Evaluation of the safety and efficacy of high-dose rate brachytherapy for radiorecurrent prostate cancer: a systematic review and meta-analysis
Strahlentherapie und Onkologie (2024)