Abstract
Background
Recent oncology guidelines recommend BRCA1/2 testing for a wide range of prostate cancer (PCa) patients. In addition, PARP inhibitors are available for mutation-positive metastatic castration-resistant PCa (mCRPC) patients following prior treatment with abiraterone, enzalutamide or docetaxel. However, the question of which of these standard treatments is the most effective for BRCA1/2 positive mCRPC patients remains to be answered. The aim of this meta-analysis was to assess the efficacy of abiraterone, enzalutamide and docetaxel in BRCA1/2 mutation-positive mCRPC patients in terms of PSA-response (PSA50), progression-free survival (PFS) and overall survival (OS).
Methods
As no interventional trials are available on this topic, we performed the data synthesis of BRCA1/2 positive mCRPC patients by using both proportional and individual patient data. For PSA50 evaluation, we pooled event rates with 95% confidence intervals (CI), while for time-to-event (PFS, OS) analyses we used individual patient data with random effect Cox regression calculations.
Results
Our meta-analysis included 16 eligible studies with 348 BRCA1/2 positive mCRPC patients. In the first treatment line, response rates for abiraterone, enzalutamide and docetaxel were 52% (CI: 25–79%), 64% (CI: 43–80%) and 55% (CI: 36–73%), respectively. Analyses of individual patient data revealed a PFS (HR: 0.47, CI: 0.26–0.83, p = 0.010) but no OS (HR: 1.41, CI: 0.82–2.42, p = 0.210) benefit for enzalutamide compared to abiraterone-treated patients.
Conclusions
Our PSA50 analyses revealed that all the three first-line treatments have therapeutic effect in BRCA1/2 positive mCRPC; although, based on the results of PSA50 and PFS analyses, BRCA positive mCRPC patients might better respond to enzalutamide treatment. However, molecular marker-driven interventional studies directly comparing these agents are crucial for providing higher-level evidence.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most common solid tumor in men, with an estimated incidence of 473,344 new cases per year in Europe [1]. While the 5-year relative survival of localized and locoregional disease is nearly 100%, despite the therapeutic advances of the past two decades, the distant metastatic cases still have a much worse prognosis (a 5-year relative survival of 32.3%) [2]. With the development of taxanes, androgen signaling inhibitors (ASIs), molecularly targeted therapies (PARP inhibitors) and theranostics, the life expectancy and life quality of patients with metastatic castration-resistant prostate cancer (mCRPC) have improved. However, this development of the treatment landscape raised an urgent need for predictive biomarkers to guide therapy optimization and sequencing.
Recently, a special attention was directed to Breast Cancer Gene 1/2 (BRCA1/2) mutation-positive PCa-s. These genes and their protein products play a crucial role in the homologous recombination repair (HRR) of double-strand DNA (dsDNA) breaks; therefore, their loss-of-function mutation results in elevated mutation burden and accelerated tumorigenesis. Several studies demonstrated that BRCA1/2 positive PCa occurs at a younger age and is associated with more unfavorable clinicopathological features and inferior prognosis [3,4,5]. The guidelines of the European Association of Urology and National Comprehensive Cancer Network recommend BRCA1/2 testing for PCa patients with positive family history, high-risk or very high-risk localized or metastatic disease [6, 7]. Considering the wide range of indications for testing, the number of PCa patients with known BRCA1/2 mutation is rising. In the last few years, PARP inhibitor treatments have become available for HRR mutation-positive mCRPC patients after ASI or docetaxel therapies, although according to the results of PROfound and PROREPAIR-B studies, they provide the highest clinical benefit for BRCA1/2 mutation carriers [6,7,8,9]. Despite the high prevalence of BRCA1/2 mutation among mCRPC patients, the question of which standard first-line treatment is the most effective in this molecular subgroup remained unanswered. However, it is crucial to understand how the presence of BRCA1/2 mutations impacts sensitivity to abiraterone, enzalutamide and docetaxel monotherapy for mCRPC. Therefore, our meta-analysis aimed to assess the efficacy of these treatments in BRCA1/2 mutation-positive mCRPC patients.
Methods
This systematic review and meta-analysis is reported according to the recommendations of the PRISMA 2020 guideline (see Supplementary Table 1), and the Cochrane Handbook [10, 11]. The study protocol was registered on PROSPERO (registration number CRD42021285267).
Eligibility criteria, outcome measures
Studies reporting PSA50, progression-free survival (PFS) or overall survival (OS) data from pathogenic BRCA1/2 mutation-positive mCRPC patients who underwent docetaxel, abiraterone or enzalutamide treatment were considered eligible. Case reports, case series and cross-sectional studies were excluded.
The primary endpoint of this study was the PSA response rate, defined as at least a 50% decrease in serum PSA level during treatment. Our secondary endpoints were PFS and OS. More detailed definitions of the reported outcomes and data collection from the included studies are listed in Supplementary Tables 2 and 3.
In order to synthesize PSA50 response rates, PFS and OS data, we used the CoCoPop framework by Munn et al., where the PSA50 response rates (Co-Condition) were evaluated in the context of (Co-Context) administered treatments (abiraterone, enzalutamide and docetaxel) in the mCRPC population (Pop-population) [12].
To assess time-to-event data, we used the PICO framework, where the population (P) was pathogenic BRCA1/2 positive mCRPC patients, the interventions and controls (I and C) were abiraterone, enzalutamide, docetaxel, and the outcomes were PFS (O1) and OS (O2) [13].
Search strategy, study selection, data collection
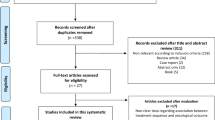
The Embase, MEDLINE (via PubMed) and CENTRAL (The Cochrane Central Register of Controlled Trials) databases were searched on the 17th of October 2021 (see search key in Supplementary File 1) to identify all available articles containing information about BRCA1/2 positive mCRPC patients. After duplicates were removed, two independent review authors (TF, ÁSZ) performed selection first by title and abstract, then by full-text. All disagreements were resolved via a third reviewer (TSZ). We calculated Cohen’s kappa coefficient to evaluate inter-rater reliability during the selection process [14].
From the eligible articles, the following data were extracted by two authors (TF and BV) independently: title, first author, the year of publication, study population, study period, countries, study design, main study findings, number of patients, patient demographics, data on mutations, interventions, outcomes. In addition, when available, we collected individual patient data. If it was not reported, we contacted the corresponding authors for supporting information. In the case of inconsistent or overlapping data, we performed adjustments in the samples from the articles (see Supplementary Table 4 for details). The disagreements were resolved via consensus with a third author (TSZ).
Risk of bias
The risk of bias was evaluated for each study according to the Joanna Briggs Critical Appraisal Checklist for Studies Reporting Prevalence Data, Cohort Studies, and Randomized Controlled Trials by two independent reviewers (TF, BV). Disagreements were resolved by a third author (TSZ) [15].
Statistical analyses
Quantitative synthesis of data was carried out with the packages ‘coxme‘, ‘IPDfromKM‘, ‘meta‘, ‘survival‘ and ‘survminer‘ of the R statistical software (version 4.1.2.). For our calculations, we followed the recommendation of Harrer et al. [16]. For all statistical analyses, a p value of ≤0.05 was considered significant. Depending on the type of the outcomes, different random-effect meta-analysis tools were applied.
For our CoCoPop question, we used the classical inverse variance method with logit transformation. We pooled the PSA50 response rates for each treatment line separately and compared the different treatments by applying subgroup analyses based on the type of intervention. We calculated pooled event rates with 95% confidence and prediction intervals. To estimate τ2, we used the Paule-Mandel method. Heterogeneity was assessed by calculating the I2 measure, its confidence interval (CI) and the Cochrane Q test. Pooling the median survival time for PFS and OS was not feasible due to the low number of articles on the specific interventions.
The method for performing time-to-event analyses for our PICO question is detailed below. We collected individual PFS and OS data from the studies according to the methodology described by Goodman-Meza et al. [17]. When the individual patient data was not accessible, we used the WebPlotDigitizer tool (Version 4.5 Copyright 2010–2021) to read digitized Kaplan-Meier curves, then we applied the methodology of Guyot et al. in order to estimate individual patient time-to-event data [18]. We performed a one-step random-effects meta-analysis on the data of the BRCA1/2 positive patients. We estimated hazard ratios (HR) between the treatments by applying the mixed effects Cox Proportional Hazards model. The Kaplan-Meier curves for each outcome are shown in a common figure.
Publication bias could not be assessed due to the low number of articles (<10) for one outcome [19].
Protocol amendment
As there were not enough articles directly comparing time-to-event outcomes (OS, PFS) between the assessed agents in the particular subgroup of BRCA1/2 positive patients, we deviated from the original plan and assessed OS and PFS based on individual patient data.
Results
Selection and baseline characteristics
Our search key identified 11,042 articles. After duplication removal 7979 studies were screened. Finally, 16 publications were eligible for qualitative and quantitative evidence synthesis (Fig. 1).
Table 1 includes the baseline characteristics of the included studies. Altogether we assessed 348 BRCA1/2 mutation-positive mCRPC patients from 16 studies. We identified four randomized trials, seven prospective and five retrospective cohort studies. We used individual patient data from 11 studies [8, 20,21,22,23,24,25,26,27,28,29]. Most publications included both germline and somatic mutations, moreover, nine reported details on the type and location of BRCA1/2 mutations as well. For further details regarding the studies and the individual patient data see Supplementary Tables 2 and 5.
PSA50 response rates for abiraterone, enzalutamide and docetaxel treatments
PSA50 response rates for the three treatments for the first and second-line settings were available for 211 patients from 13 articles [9, 21,22,23,24,25,26,27, 29,30,31,32,33]. Response rates for abiraterone, enzalutamide and docetaxel were 0.53 (CI: 0.35–0.71; I2 = 36%), 0.56 (CI: 0.39–0.72; I2 = 15%) and 0.47 (CI: 0.33–0.62; I2 = 0%), respectively (Supplementary Fig. 1). When separating results according to treatment lines for mCRPC, we found greater differences in PSA50 response rates between the agents. In the first-line setting, we synthesized the data of 97 patients from eight articles and found PSA50 response rates of 0.52 (CI: 0.25–0.79; I2 = 57%), 0.64 (CI: 0.43–0.80; I2 = 0%), 0.55 (CI: 0.36–0.73; I2 = 1%) for abiraterone, enzalutamide and docetaxel, respectively (Fig. 2) [9, 22, 24,25,26, 29,30,31]. Second-line data were available for 57 patients from five articles and response rates tended to be generally lower compared to the first-line setting but showed similar distributions between abiraterone, enzalutamide and docetaxel therapies; 0.36 (CI: 0.17–0.61; I2 = 3%), 0.46 (CI: 0.24–0.70; I2 = 0%) and 0.42 (CI: 0.22–0.65; I2 = 2%), respectively (Supplementary Fig. 2) [21, 24, 29,30,31].
PFS analysis based on individual patient data
By comparing the PFS rates of 78 BRCA1/2 positive patients from seven articles, we found a significantly lower chance (HR: 0.47, CI: 0.27–0.83, p = 0.010) for progression in enzalutamide-treated compared to abiraterone-treated patients in the pooled first- and second-line setting [21,22,23,24,25, 27, 29]. This tendency also appeared in the first-line setting; however, it did not reach significance (HR: 0.56, CI: 0.27–1.17, p = 0.120, n = 47) [22,23,24,25, 29]. HR-s for comparisons of docetaxel with abiraterone (HR: 0.38, CI: 0.56–1.47, p = 0.500, n = 86) and enzalutamide with docetaxel (HR: 0.59, CI: 0.67–1.82, p = 0.370, n = 68) showed no significant PFS differences when pooling the first and second treatment lines [21,22,23,24,25, 27,28,29].
OS analysis based on individual patient data
The HR for OS in the analysis of pooled first and second treatment lines for the enzalutamide vs. abiraterone comparison was 1.41 (CI: 0.82–2.42, p = 0.210, n = 101), for docetaxel vs. abiraterone 1.65 (CI: 0.67–4.03, p = 0.280, n = 82) and for enzalutamide vs. docetaxel 1.69 (CI: 0.79–3.58, p = 0.280, n = 69) [21, 22, 24, 26, 29, 30]. In the first-line setting, we compared enzalutamide with abiraterone (77 patients from four articles) [22, 24, 29, 30]. This analysis revealed a HR of 1.91 for enzalutamide (CI: 0.99–3.66, p = 0.051).
Risk of bias assessment, publication bias and heterogeneity
The Joanna Briggs Critical Appraisal Tool for Prevalence, Cohort and Randomized Interventional Studies identified a low overall risk of bias in the included studies for PSA50, PFS and OS outcomes as well. The risk of bias assessment results are presented in Supplementary Tables 6–8.
Discussion
In this review and meta-analysis, we aimed to compare the therapeutic effects of abiraterone, enzalutamide and docetaxel in BRCA1/2 mutation-positive mCRPC patients. We found therapeutic responses to all three agents with some potentially important differences.
BRCA1/2 positive cases represent a characteristically distinct molecular subtype of PCa-s with earlier-onset disease and a more aggressive clinical phenotype [3,4,5]. With higher sensitivity to PARP inhibitor treatments, BRCA1/2 positive PCa-s seem to have a different therapeutic sensitivity, suggesting that these patients may benefit from different treatment strategies. In this context, it is interesting that recent in vivo and in vitro data shed light on the crosstalk between androgen receptor (AR) signaling and dsDNA repair [34,35,36]. The AR has been shown to activate the non-homologous end-joining DNA damage repair, which is—besides the HRR pathway—responsible for the repair of dsDNA breaks [34,35,36]. The identification of this crosstalk between the AR and DNA repair pathways led to the hypothesis that ASI may cause “synthetic lethality” in HRR deficient PCa-s. In other words, ASI treatment may augment the effect of HRR deficiency, resulting in a greater therapeutic response to ASI in BRCA1/2 positive PCa patients [34,35,36].
There are only two studies directly comparing abiraterone, enzalutamide and docetaxel in BRCA1/2 positive mCRPC patients, and the results are conflicting. A retrospective cohort study by Sokolova et al. found comparable PSA50 responses with the three agents in germline BRCA2 carriers [31]. In contrast, a retrospective series of 149 HRR mutated (BRCA2 n = 60; BRCA1 n = 5) mCRPC patients by Kwon et al. showed higher PSA50 response rates and longer OS for first-line abiraterone treatment among BRCA1/2 carriers compared with enzalutamide [30].
The remaining few studies on this topic compared therapy responses between BRCA1/2 (or HRR) carriers and non-carriers in various treatment groups. In a prospective randomized study, abiraterone and enzalutamide were compared directly in the first-line setting, and the presence of BRCA1/2 mutation status proved to be an independent prognostic factor for shorter PFS [22, 37]. In the PROREPAIR-B trial Castro et al. found that germline BRCA1/2 mutation carriers treated with the taxane-ASI sequence had worse cancer-specific- and PFS rates compared to non-carriers. At the same time, this difference was not observed in the case of first-line ASI followed by taxane, but, of note, they did not report on the type of ASI (abiraterone or enzalutamide) [9].
However, a comparison of responses to a certain treatment between BRCA1/2 mutation carriers and non-carriers is only able to provide prognostic, but not therapy predictive, information, which cannot be used for decision-making on the selection of the most effective drug for BRCA1/2 positive patients [38]. To answer the question of which treatment is the most effective for BRCA1/2 positive mCRPC patients, a head-to-head comparison of agents in the BRCA positive population is needed. According to this approach, in this meta-analysis focusing only on BRCA1/2 positive cases, we collected data from 348 mCRPC patients. We then compared treatment efficacy between abiraterone, enzalutamide and docetaxel in terms of PSA response (pooled event rates), OS and PFS (pooled individual patient data). When focusing on the first-line setting, we found the highest PSA50 response rate for enzalutamide (64%), followed by docetaxel (55%) and abiraterone (52%). These results were supported by time-to-event PFS evaluation, showing significantly longer PFS in the enzalutamide treatment group. Seemingly in contrast, first-line enzalutamide treated patients tended to have a shorter OS compared to those who received abiraterone. This apparent discrepancy between the PFS and OS results might be explained by the findings of the first crossover study comparing the abiraterone-to-enzalutamide and enzalutamide-to-abiraterone treatment sequences. Based on their results, the authors recommended abiraterone-to-enzalutamide as the preferred treatment sequence [21, 22]. As our meta-analysis included patients from the above-mentioned study, a significant number of patients received crossover between abiraterone and enzalutamide, which may explain the OS benefit in the first-line abiraterone-treated patients. A similar evaluation for docetaxel was not possible, because of the low numbers of patients with first-line docetaxel treatment.
Based on our results, abiraterone, enzalutamide and docetaxel are effective first-line treatments for BRCA1/2 positive mCRPC patients. Our data suggest that enzalutamide might provide a more favorable therapeutic response and PFS for this molecular subgroup of mCRPC patients. However, taking into account the limitations of the available studies, the provided results should be considered hypothesis-generating, providing a basis for further prospective data collection, including the hormone-sensitive stage to provide higher-level evidence. BRCA1/2 mutation-selected prospective randomized clinical trials comparing abiraterone, enzalutamide, and docetaxel might give additional answers. In summary, BRCA1/2 status may be a predictive marker for treatment decisions in earlier treatment settings. Therefore, our results underline the importance of genetic testing before the start of any systemic treatment for advanced PCa, in order to plan ahead the best possible therapeutic sequence. This is in accordance with current EAU and NCCN guidelines recommending BRCA1/2 testing for PCa patients with high-risk and very high-risk localized or metastatic disease or for those with positive family history [6, 7]. While currently PARPi-s can be given after progression on an ASI treatment, there are several clinical trials assessing combinations of the two agents in the first-line setting. In the PROpel trial combination of olaparib and abiraterone was shown to provide a significant PFS benefit for molecularly unselected mCRPC patients, although analysis of molecular subgroups and final OS data have not been published yet [39]. Preliminary results of the MAGNITUDE study showed a PFS, but not OS benefit for the combination of niraparib and abiraterone vs. abiraterone only in the BRCA1/2 selected subgroup [40]. Finally, early results from the BRCAAway study which randomized BRCA1/2 and ATM positive patients to olaparib plus abiraterone combination vs. abiraterone-olaparib vs. olaparib-abiraterone sequences suggest a PFS benefit for the combination treatment, however PFS2 and OS data are not mature yet [41]. These studies suggest a synergistic effect of the two compounds, however data published up to date are immature to support the superior effect of the combination over sequencing of abiraterone and PARPi-s. In the context of our findings, enzalutamide might be a sufficient candidate as well for the combination treatment with PARPi-s. Currently the CASPAR (NCT04455750), TALAPRO-2 (NCT03395197) and TALAPRO-3 (NCT04821622) studies are investigating the combination of enzalutamide and PARPi-s, but no results are available yet. Treatment selection for BRCA1/2 patients after progressing on conventional agents and PARP inhibitors is of increasing clinical relevance. In this context it is important to note that there is emerging data supporting the enriched effect of platinum treatment in BRCA1/2 positive mCRPC patients even after progression on PARPi therapy [42]. However, the efficacy of platinum and its possible place in the treatment sequence needs to be assessed in more detail. Besides platinum, mCRPC patients harboring BRCA1/2 mutations thought to benefit more from PSMA-radioligand treatment, based on the higher sensitivity of HRR mutant cells to irradiation [43, 44]. Although clinical data currently available on this topic is limited to retrospective case series and cohorts with controversial results, but it seems that these patients respond to PSMA-ligand therapy also after failure to PARP inhibitors [43, 44].
This study has several limitations. (1) A major limitation of this work is the relatively low patient number and (2) the lack of prospective, interventional studies for inclusion. (3) A further limitation is that PFS was not uniformly defined in the included studies (see supplementary Tables 2 and 3), which may represent a potential bias. (4) The recommendations on BRCA1/2 testing have evolved in the past decade, which may introduce potential bias when including retrospective studies. (5) Heterogeneity in study design, patient selection, baseline characteristics, endpoint definitions, method of mutation testing (sequencing method and germline vs. somatic) and definition, genes tested (only BRCA1/2 vs. also other HRR genes) may influence our results.
The strengths of this study include (1) the fact that this is the first meta-analysis directly comparing the efficacy of abiraterone, enzalutamide and docetaxel treatments in BRCA1/2 mutation-positive mCRPC patients as well as (2) the fact that individual patient data were used for data synthesis.
Conclusions
BRCA1/2 positive mCRPC patients respond to standard first-line treatments, including abiraterone, enzalutamide and docetaxel. Moreover, our study suggests that these patients might benefit most from enzalutamide treatment in the first-line setting, although molecularly selected interventional trials are needed to validate this hypothesis.
Data availability
The data that supports the findings of this study are available in the supplementary material of this paper.
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. 2020. https://gco.iarc.fr/today.
National Cancer Institute. SEER Cancer Stat Facts: Prostate Cancer [cited 2022 May 3]. https://seer.cancer.gov/statfacts/html/prost.html.
Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M, et al. Germline BRCA Mutations Are Associated With Higher Risk of Nodal Involvement, Distant Metastasis, and Poor Survival Outcomes in Prostate Cancer. J Clin Oncol. 2013;31:1748–57.
Kote-Jarai Z, Leongamornlert D, Saunders E, Tymrakiewicz M, Castro E, Mahmud N, et al. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105:1230–4.
Oh M, Alkhushaym N, Fallatah S, Althagafi A, Aljadeed R, Alsowaida Y, et al. The association of BRCA1 and BRCA2 mutations with prostate cancer risk, frequency, and mortality: a meta-analysis. Prostate. 2019;79:880–95.
National Comprehensive Cancer Network Prostate Cancer Guideline Version 4.2022. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1459.
Mottet N, Cornford P, Bergh RCNVD, Briers E, Santis MD, Gillessen S, et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer. https://uroweb.org/guidelines/prostate-cancer.
de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med. 2020;382:2091–102.
Castro E, Romero-Laorden N, Del Pozo A, Lozano R, Medina A, Puente J, et al. PROREPAIR-B: A Prospective Cohort Study of the Impact of Germline DNA Repair Mutations on the Outcomes of Patients With Metastatic Castration-Resistant Prostate Cancer. J Clin Oncol. 2019;37:490–503.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Health. 2015;13:147–53.
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inf Decis Mak. 2007;7:16.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276–82.
Institute JB JBI Critical Appraisal Tools 2022. https://jbi.global/critical-appraisal-tools.
Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing Meta-Analysis With R: A Hands-On Guide. 1st ed. Boca Raton, FL and London: Chapman & Hall/CRC Press; 2021.
Goodman-Meza D, Weiss RE, Gamboa S, Gallegos A, Bui AAT, Goetz MB, et al. Long term surgical outcomes for infective endocarditis in people who inject drugs: a systematic review and meta-analysis. BMC Infect Dis. 2019;19:918.
Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9.
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002.
Annala M, Struss WJ, Warner EW, Beja K, Vandekerkhove G, Wong A, et al. Treatment Outcomes and Tumor Loss of Heterozygosity in Germline DNA Repair-deficient Prostate Cancer. Eur Urol. 2017;72:34–42.
Annala M, Taavitsainen S, Khalaf DJ, Vandekerkhove G, Beja K, Sipola J, et al. Evolution of Castration-Resistant Prostate Cancer in ctDNA during Sequential Androgen Receptor Pathway Inhibition. Clin Cancer Res. 2021;27:4610–23.
Annala M, Vandekerkhove G, Khalaf D, Taavitsainen S, Beja K, Warner EW, et al. Circulating Tumor DNA Genomics Correlate with Resistance to Abiraterone and Enzalutamide in Prostate Cancer. Cancer Disco. 2018;8:444–57.
Wyatt AW, Azad AA, Volik SV, Annala M, Beja K, McConeghy B, et al. Genomic Alterations in Cell-Free DNA and Enzalutamide Resistance in Castration-Resistant Prostate Cancer. JAMA Oncol. 2016;2:1598–606.
Dong B, Fan L, Yang B, Chen W, Li Y, Wu K, et al. Use of Circulating Tumor DNA for the Clinical Management of Metastatic Castration-Resistant Prostate Cancer: A Multicenter, Real-World Study. J Natl Compr Canc Netw. 2021;19:905–14.
Zhao J, Sun G, Zhu S, Dai J, Chen J, Zhang M, et al. Circulating tumour DNA reveals genetic traits of patients with intraductal carcinoma of the prostate. BJU Int. 2022;129:345–55.
Gallagher DJ, Cronin AM, Milowsky MI, Morris MJ, Bhatia J, Scardino PT, et al. Germline BRCA mutation does not prevent response to taxane-based therapy for the treatment of castration-resistant prostate cancer. BJU Int. 2012;109:713–9.
Hussain M, Daignault-Newton S, Twardowski PW, Albany C, Stein MN, Kunju LP, et al. Targeting Androgen Receptor and DNA Repair in Metastatic Castration-Resistant Prostate Cancer: Results From NCI 9012. J Clin Oncol. 2018;36:991–9.
Mateo J, Cheng HH, Beltran H, Dolling D, Xu W, Pritchard CC, et al. Clinical Outcome of Prostate Cancer Patients with Germline DNA Repair Mutations: Retrospective Analysis from an International Study. Eur Urol. 2018;73:687–93.
Torquato S, Pallavajjala A, Goldstein A, Toro PV, Silberstein JL, Lee J, et al. Genetic Alterations Detected in Cell-Free DNA Are Associated With Enzalutamide and Abiraterone Resistance in Castration-Resistant Prostate Cancer. JCO Precis Oncol. 2019;3.PO.18.00227.
Kwon DH, Chou J, Yip SM, Reimers MA, Zhang L, Wright F, et al. Differential treatment outcomes in BRCA1/2-, CDK12-, and ATM-mutated metastatic castration-resistant prostate cancer. Cancer 2021;127:1965–73.
Sokolova AO, Marshall CH, Lozano R, Gulati R, Ledet EM, De Sarkar N, et al. Efficacy of systemic therapies in men with metastatic castration resistant prostate cancer harboring germline ATM versus BRCA2 mutations. Prostate 2021;81:1382–9.
McKay RR, Kwak L, Crowdis JP, Sperger JM, Zhao SG, Xie W, et al. Phase II Multicenter Study of Enzalutamide in Metastatic Castration-Resistant Prostate Cancer to Identify Mechanisms Driving Resistance. Clin Cancer Res. 2021;27:3610–9.
Nientiedt C, Heller M, Endris V, Volckmar AL, Zschäbitz S, Tapia-Laliena MA, et al. Mutations in BRCA2 and taxane resistance in prostate cancer. Sci Rep. 2017;7:4574.
Polkinghorn WR, Parker JS, Lee MX, Kass EM, Spratt DE, Iaquinta PJ, et al. Androgen Receptor Signaling Regulates DNA Repair in Prostate Cancers. Cancer Discov. 2013;3:1245–53.
Goodwin JF, Schiewer MJ, Dean JL, Schrecengost RS, de Leeuw R, Han S, et al. A hormone-DNA repair circuit governs the response to genotoxic insult. Cancer Disco. 2013;3:1254–71.
Antonarakis ES, Lu C, Luber B, Liang C, Wang H, Chen Y, et al. Germline DNA-repair Gene Mutations and Outcomes in Men with Metastatic Castration-resistant Prostate Cancer Receiving First-line Abiraterone and Enzalutamide. Eur Urol. 2018;74:218–25.
Khalaf DJ, Annala M, Taavitsainen S, Finch DL, Oja C, Vergidis J, et al. Optimal sequencing of enzalutamide and abiraterone acetate plus prednisone in metastatic castration-resistant prostate cancer: a multicentre, randomised, open-label, phase 2, crossover trial. Lancet Oncol. 2019;20:1730–9.
Ballman KV. Biomarker: Predictive or Prognostic? J Clin Oncol. 2015;33:3968–71.
Clarke NW, Armstrong AJ, Thiery-Vuillemin A, Oya M, Shore N, Loredo E, et al. Abiraterone and Olaparib for Metastatic Castration-Resistant Prostate Cancer. NEJM Evidence.0(0):EVIDoa2200043.
Chi KN, Rathkopf DE, Smith MR, Efstathiou E, Attard G, Olmos D, et al. Phase 3 MAGNITUDE study: First results of niraparib (NIRA) with abiraterone acetate and prednisone (AAP) as first-line therapy in patients (pts) with metastatic castration-resistant prostate cancer (mCRPC) with and without homologous recombination repair (HRR) gene alterations. J Clin Oncol. 2022;40:12.
Hussain MHA, Kocherginsky M, Agarwal N, Zhang J, Adra N, Paller CJ, et al. BRCAAWAY: A randomized phase 2 trial of abiraterone, olaparib, or abiraterone + olaparib in patients with metastatic castration-resistant prostate cancer (mCRPC) with DNA repair defects. J Clin Oncol. 2022;40:5018.
Mota JM, Barnett E, Nauseef JT, Nguyen B, Stopsack KH, Wibmer A, et al. Platinum-Based Chemotherapy in Metastatic Prostate Cancer With DNA Repair Gene Alterations. JCO Precis Oncol. 2020;4:355–66.
Privé BM, Slootbeek PHJ, Laarhuis BI, Naga SP, van der Doelen MJ, van Kalmthout LWM, et al. Impact of DNA damage repair defects on response to PSMA radioligand therapy in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2022;25:71–8.
van der Doelen MJ, Mehra N, van Oort IM, Looijen-Salamon MG, Janssen MJR, Custers JAE, et al. Clinical outcomes and molecular profiling of advanced metastatic castration-resistant prostate cancer patients treated with 225Ac-PSMA-617 targeted alpha-radiation therapy. Urologic Oncol: Semin Original Investig. 2021;39:729.e7–e16.
Funding
TS was supported by a János Bolyai Research Scholarship of the Hungarian Academy of Sciences (BO/00451/20/5). This work was supported by the ÚNKP-21-5-SE-3, ÚNKP-21-3-II-SE-13, ÚNKP-22-3-1-SE-19 New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development and Innovation Fund. Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
All authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the paper. CRediT author contribution https://www.elsevier.com/authors/policies-and-guidelines/credit-author-statement. TF: conceptualization, project administration, methodology, visualization, formal analysis, investigation, data curation, writing—Original Draft. ÁS: investigation, writing—Review & Editing. BT: methodology, conceptualization, project administration, supervision, writing—Review & Editing. AC: project administration, supervision, resources, writing—Review & Editing. BV: investigation, writing—Review & Editing. AV: formal analysis, software, data curation, methodology, visualization. TK: formal analysis, validation, software, data curation, methodology, writing—Original Draft, visualization. ZL: formal analysis, validation, software, data curation, methodology, writing—Original Draft, visualization. NÁ: conceptualization, supervision, writing—Review & Editing. ZK: conceptualization, writing—Review & Editing. PH: validation, methodology, conceptualization, supervision, project administration, funding acquisition, writing—Review & Editing. BH: conceptualization, writing—Review & Editing. VG: conceptualization, writing—Review & Editing. PN: conceptualization, supervision, funding acquisition, writing—Review & Editing. TS: validation, conceptualization, visualization, supervision, project administration, funding acquisition, writing—Review & Editing. All authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the paper.
Corresponding author
Ethics declarations
Competing interests
BH has had advisory roles for ABX, AAA/Novartis, Astellas, AstraZeneca, Bayer, Bristol Myers Squibb, Janssen R&D, Lightpoint Medical, Inc., and Pfizer; has received research funding from Astellas, Bristol Myers Squibb, AAA/Novartis, German Research Foundation, Janssen R&D, and Pfizer; and has received compensation for travel from Astellas, AstraZeneca, Bayer and Janssen R&D.
Ethics approval
No ethical approval was required for this systematic review with meta-analysis, as all data were already published in peer-reviewed journals. No patients were involved in the design, conduct or interpretation of our study. The datasets used in this study can be found in the full-text paper included in the systematic review and meta-analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fazekas, T., Széles, Á.D., Teutsch, B. et al. Therapeutic sensitivity to standard treatments in BRCA positive metastatic castration-resistant prostate cancer patients—a systematic review and meta-analysis. Prostate Cancer Prostatic Dis 26, 665–672 (2023). https://doi.org/10.1038/s41391-022-00626-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00626-2
This article is cited by
-
Association between concomitant proton pump inhibitor use and survival of patients with metastatic prostate cancer receiving abiraterone acetate: a post-hoc analysis of pooled data from three randomized controlled trials
Prostate Cancer and Prostatic Diseases (2023)
-
Extensive review on breast cancer its etiology, progression, prognostic markers, and treatment
Medical Oncology (2023)