Abstract
Background
In 2004 docetaxel was the first life-prolonging drug (LPD) registered for metastatic castration-resistant prostate cancer (mCRPC) patients. Between 2011 and 2014 new LPDs for mCRPC (cabazitaxel, abiraterone, enzalutamide, and radium-223) were introduced in the Netherlands. The objective of this study is to assess the impact of the introduction of new LPDs on treatment patterns and overall survival (OS) over time.
Patients and methods
CRPC patients diagnosed in the years 2010–2016 in the observational, retrospective CAPRI registry (20 hospitals) were included and followed up to 2018. Two subgroups were analyzed: treatment-naïve patients (subgroup 1, n = 3600) and post-docetaxel patients (subgroup 2, n = 1355).
Results
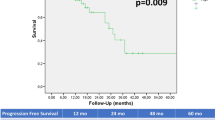
In both subgroups, the use of any LPD increased: from 57% (2010–2011) to 69% (2014–2015) in subgroup 1 and from 65% (2011–2012) to 79% (2015–2016) in subgroup 2. Chemotherapy as first mCRPC-treatment (i.e., docetaxel) and first post-docetaxel treatment (i.e., cabazitaxel or docetaxel rechallenge) decreased (46–29% and 20–9% in subgroup 1 and 2, respectively), while the use of androgen-receptor targeting treatments (ART) increased from 11% to 39% and 46% to 64% in subgroup 1 and 2, respectively. In subgroup 1, median OS (mOS) from diagnosis CRPC increased from 28.5 months to 31.0 months (p = 0.196). In subgroup 2, mOS from progression on docetaxel increased from 7.9 months to 12.5 months (p < 0.001). After multiple imputations of missing values, in multivariable cox-regression analysis with known prognostic parameters, the treatment period was independent significant for OS in subgroup 1 (2014–2015 vs. 2010–2011 with HR 0.749, p < 0.001) and subgroup 2 (2015–2016 vs. 2011–2012 with HR 0.811, p = 0.037).
Conclusion
Since 2010, a larger proportion of mCRPC patients was treated with LPDs, which was related to an increased mOS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siesling S, Visser O, Aarts MJ, Verhoeven RHA, Aben KKH, Dinmohamed AG, et al. Kankerbestrijding in Nederland [Fight against cancer in the Netherlands: current state of affairs]. Ned Tijdschr Geneeskd. 2019;163(Jun):D4150. Dutch.
Trama A, Foschi R, Larranaga N, Sant M, Fuentes-Raspall R, Serraino D, et al. Survival of male genital cancers (prostate, testis and penis) in Europe 1999–2007: results from the EUROCARE-5 study. Eur J Cancer. 2015;51:2206–16.
De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, et al. Cancer survival in Europe 1999–2007 by country and age: results of EUROCARE–5-a population-based study. Lancet Oncol. 2014;15:23–34.
Netherlands cancer registry (NCR)—NKR cijfers/IKNL. www.cijfersoverkanker.nl. Accessed 23 Jan 2020.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12.
de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54.
Fizazi K, Scher HI, Molina A, Logothetis CJ, Chi KN, Jones RJ, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13:983–92.
Ryan CJ, Smith MR, Fizazi K, Saad F, Mulders PF, Sternberg CN, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;16:152–60.
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33.
Parker C, Nilsson S, Heinrich D, Helle SI, O'Sullivan JM, Fossa SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23.
Westgeest HM, Uyl-de Groot CA, van Moorselaar RJA, de Wit R, van den Bergh ACM, Coenen JLLM, et al. Differences in trial and real-world populations in the dutch castration-resistant prostate cancer registry. Eur Urol Focus. 2018;4:694–701.
Westgeest HM, Kuppen MCP, van den Eertwegh AJM, de Wit R, Coenen JLLM, van den Berg HPP, et al. Second-line cabazitaxel treatment in castration-resistant prostate cancer clinical trials compared to standard of care in CAPRI: observational study in the Netherlands. Clin Genitourin Cancer. 2019;17:e946–e956.
Flaig TW, Potluri RC, Ng Y, Todd MB, Mehra M. Treatment evolution for metastatic castration-resistant prostate cancer with recent introduction of novel agents: retrospective analysis of real-world data. Cancer Med. 2016;5:182–91.
Kwan EM, Semira MC, Bergin ART, Muttiah C, Beck S, Anton A, et al. Impact of access to novel therapies on the initial management of castrate-resistant prostate cancer: an Australian multicentre study. Intern Med J. 2019;49:1378–85.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014;65:467–79.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377–99.
Francini E, Gray KP, Shaw GK, Evan CP, Hamid AA, Perry CE, et al. Impact of new systemic therapies on overall survival of patients with metastatic castration-resistant prostate cancer in a hospital-based registry. Prostate Cancer Prostatic Dis. 2019;22:420–7.
Halabi S, Small EJ, Kantoff PW, Kattan MW, Kaplan EB, Dawson NA, et al. Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol. 2003;21:1232–7.
Halabi S, Lin CY, Small EJ, Armstrong AJ, Kaplan EB, Petrylak D, et al. Prognostic model predicting metastatic castration-resistant prostate cancer survival in men treated with second-line chemotherapy. J Natl Cancer Inst. 2013;105:1729–37.
Soerdjbalie-Maikoe V, Pelger RC. Lycklama a Nijeholt GA, Arndt JW, Zwinderman AH, Bril H, et al. Bone scintigraphy predicts the risk of spinal cord compression in hormone-refractory prostate cancer. Eur J Nucl Med Mol Imaging. 2004;31:958–63.
Hwang SS, Chang VT, Alejandro Y, Mulaparthi S, Cogswell J, Srinivas S, et al. Study of hormone refractory prostate cancer: hospital care and palliative care resource use at a VA medical center. Cancer Inves. 2004;22:849–57.
Berruti A, Tucci M, Mosca A, Tarabuzzi R, Gorzegno G, Terrone C, et al. Predictive factors for skeletal complications in hormone-refractory prostate cancer patients with metastatic bone disease. Br J Cancer. 2005;93:633–8.
Chin SN, Wang L, Moore M, Sridhar SS. A review of the patterns of docetaxel use for hormone-resistant prostate cancer at the princess margaret hospital. Curr Oncol. 2010;17:24–9.
Chaumard-Billotey N, Chabaud S, Boyle HJ, Helle SI, O’Sullivan JM, Fosså SD, et al. Impact of news drugs in the median overall survival of patients with metastatic castration resistant prostate cancer (mCRPC). J Clin Oncol. 2013;31(Suppl 15):e16096–e16096. (abstract16096).
Funding
This research was funded by Sanofi-Aventis Netherlands B.V., Janssen-Cilag B.V., Astellas Pharma B.V., and Bayer B.V. The funding organizations had no role in the design and conduct of the study, collection, management, analysis, interpretation of the data, and preparation, review, or approval of the abstract.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HMW reports travel expenses paid by Ipsen and honoraria from Roche and Astellas. MCPK reports travel expenses from Ipsen. AJMvdE reports study grants from Sanofi and Roche, travel expenses from MSD Oncology, Roche, Pfizer, and Sanofi, honoraria from Bristol-Myers Squibb, and consulting/advisory role for Bristol-Myers Squibb, MSD Oncology, Amgen, Roche, Novartis, Sanofi, Pfizer, Ipsen, and Merck. RdW reports consulting/advisory role for Sanofi, Merck Sharp&Dohme, Roche/Genentech, Janssen, Bayer, Clivis; honoraria from Sanofi, Merck Sharp&Dohme; and research funding from Sanofi and Bayer. AMB reports research funding from Sanofi, Astellas, and Bayer; consulting/advisory role for Sanofi, Astellas, and Bayer; travel expenses for Sanofi, Astellas, and Bayer and speakers bureau for Sanofi, Astellas, Bayer, and Janssen. RJAvM reports honoraria from Astellas, AstraZeneca, Bayer, Janssen and Sanofi-Genzyme. JLLMC reports consulting/advisory role for Sanofi. DMS reports research funding from Astellas and consulting/advisory role for Astellas and Janssen. NM reports research funding (institute) for Astellas, Janssen, Pfizer, Roche, and Sanofi Genzyme; advisory role (compensated and institutional) for Roche, MSD, BMS, Bayer, Astellas, and Janssen; and travel expenses from Astellas and MSD. IMvO reports consulting/advisory role for Astellas, Janssen, Bayer, Roche, Mdx health; and research funding from Astellas, Janssen, Bayer. WRG reports speakers fees from Bayer and MSD; consulting/advisory role for Bristol-Myers Squibb, Astellas, Bayer, Sanofi, Amgen; and research funding from Bayer, Astellas, Janssen-Cilag. CAUdG reports research funding from Boehringer Ingelheim, Astellas, Celgene, Sanofi, Janssen-Cilag, Bayer, Amgen, Genzyme, Merck, Glycostem Therapeutics, Astra Zeneca, Roche, and Merck. All remaining authors have declared no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Westgeest, H.M., Kuppen, M.C.P., van den Eertwegh, A.J.M. et al. The effects of new life-prolonging drugs for metastatic castration-resistant prostate cancer (mCRPC) patients in a real-world population. Prostate Cancer Prostatic Dis 24, 871–879 (2021). https://doi.org/10.1038/s41391-021-00344-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00344-1
This article is cited by
-
The impact of locoregional treatments for metastatic castration resistant prostate cancer on disease progression: real life experience from a multicenter cohort
Prostate Cancer and Prostatic Diseases (2024)
-
Activity and safety of KEES - an oral multi-drug chemo-hormonal metronomic combination regimen in metastatic castration-resistant prostate cancer
BMC Cancer (2023)
-
Impact of molecular tumour board discussion on targeted therapy allocation in advanced prostate cancer
British Journal of Cancer (2022)