Abstract
Background
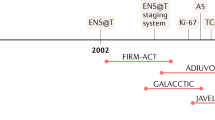
Prostate cancer (PCa) typically spreads to the bone, and this distribution is attributed to the central role of the microenvironment in progression. However, metastasis to the adrenal glands, while not as common, does occur. The biology that accounts for adrenal metastases may be attributed to the unique local steroid metabolome and co-clinical characterization may elucidate the role steroid biosynthesis plays in PCa progression.
Methods
Three patients with metastatic PCa who had archived tumor tissue from an adrenalectomy were retrospectively identified, and one adrenal metastasis was developed into a xenograft (MDA-PCa-250). The adrenal metastases were characterized by performing somatic DNA whole exome sequencing (WES), RNA-Seq, immunohistochemistry (IHC), and steroid metabolite quantitation. The influence of steroid metabolites on adrenal metastasis cells and tumor growth was tested in vitro and in vivo.
Results
Clinically, adrenalectomy was performed during castration-resistant oligometastatic disease, and two men experienced resensitization to leuprolide. Somatic DNA WES revealed heterogeneous alterations in tumor suppressor and DNA damage repair pathway genes. Adrenal metastases had active androgen receptor (AR) signaling by IHC, and RNA-Seq supported a potential role for adrenal androgen precursor metabolism in activating the AR. Steroid quantitation suggested the adrenal androgen precursors were converted into testosterone in these metastases, and stable isotope tracing of an organoid from MDA-PCa-250 confirmed the capability of adrenal metastases to biosynthesize testosterone from adrenal precursors. In vitro testing of a cell line derived from MDA-PCa-250 showed that testosterone and cortisol stimulated tumor cell growth. In vivo experiments demonstrated that MDA-PCa-250 grew in intact mice with circulating testosterone, but not in castrated mice.
Conclusions
PCa adrenal metastases depend upon AR signaling driven by androgen precursors, androstenedione and dehydroepiandrosterone, available in the microenvironment, despite the presence of heterogeneous somatic DNA alterations. Moreover, MDA-PCa-250 provides a preclinical model that can recapitulate the unique androgen-dependence of adrenal metastases.
Clinical trial registration
This study does not report the clinical results of a clinical trial, but it does use samples from a completed clinical trial that is registered with clinicaltrials.gov (NCT01254864).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data is available to any reader upon request. Please email the corresponding author to request the data.
References
Weiss L. Comments on hematogenous metastatic patterns in humans as revealed by autopsy. Clin Exp Metastasis. 1992;10:191–9.
Gandaglia G, Abdollah F, Schiffmann J, Trudeau V, Shariat SF, Kim SP, et al. Distribution of metastatic sites in patients with prostate cancer: A population-based analysis. Prostate 2014;74:210–6.
Ashrafi AN, Fay C, Yip W, de Freitas DM, Nabhani J, Aron M. Durable biochemical response following adrenal metastasectomy for oligometastatic castrate-resistant prostate cancer. Urol Case Rep. 2020;32:101229.
Rubin MA, Putzi M, Mucci N, Smith DC, Wojno K, Korenchuk S, et al. Rapid (“warm”) autopsy study for procurement of metastatic prostate cancer. Clin Cancer Res. 2000;6:1038–45.
Stanbrough M, Bubley GJ, Ross K, Golub TR, Rubin MA, Penning TM, et al. Increased expression of genes converting adrenal androgens to testosterone in androgen-independent prostate cancer. Cancer Res. 2006;66:2815–25.
Tamae D, Mostaghel E, Montgomery B, Nelson PS, Balk SP, Kantoff PW, et al. The DHEA-sulfate depot following P450c17 inhibition supports the case for AKR1C3 inhibition in high-risk localized and advanced castration-resistant prostate cancer. Chem-Biol Interact. 2015;234:332–8.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N. Engl J Med. 2011;364:1995–2005.
Schiffer L, Barnard L, Baranowski ES, Gilligan LC, Taylor AE, Arlt W, et al. Human steroid biosynthesis, metabolism and excretion are differentially reflected by serum and urine steroid metabolomes: A comprehensive review. J Steroid Biochem Mol Biol. 2019;194:105439.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N. Engl J Med. 2014;371:424–33.
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira de Santana Gomes AJ, Given R, et al. Apalutamide for metastatic, castration-sensitive prostate cancer. N. Engl J Med. 2019;381:13–24.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N. Engl J Med. 2013;368:138–48.
de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Olaparib for metastatic castration-resistant prostate cancer. N. Engl J Med. 2020;382:2091–102.
Aparicio AM, Harzstark AL, Corn PG, Wen S, Araujo JC, Tu SM, et al. Platinum-based chemotherapy for variant castrate-resistant prostate cancer. Clin Cancer Res. 2013;19:3621–30.
Beltran H, Prandi D, Mosquera JM, Benelli M, Puca L, Cyrta J, et al. Divergent clonal evolution of castration-resistant neuroendocrine prostate cancer. Nat Med. 2016;22:298–305.
Bluemn EG, Coleman IM, Lucas JM, Coleman RT, Hernandez-Lopez S, Tharakan R, et al. Androgen receptor pathway-independent prostate cancer is sustained through FGF signaling. Cancer Cell. 2017;32:474–89. e6.
Mu P, Zhang Z, Benelli M, Karthaus WR, Hoover E, Chen CC, et al. SOX2 promotes lineage plasticity and antiandrogen resistance in TP53- and RB1-deficient prostate cancer. Science. 2017;355:84–8.
Boukovala M, Spetsieris N, Weldon JA, Tsikkinis A, Hoang A, Aparicio A, et al. A candidate androgen signalling signature predictive of response to abiraterone acetate in men with metastatic castration-resistant prostate cancer. Eur J Cancer 2020;127:67–75.
Spetsieris N, Boukovala M, Weldon JA, Tsikkinis A, Hoang A, Aparicio A, et al. A Phase 2 trial of abiraterone followed by randomization to addition of Dasatinib or Sunitinib in men with metastatic castration-resistant prostate cancer. Clin Genitourin Cancer. 2021;19:22–31. e5.
Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinforma. 2009;25:1754–60.
DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet. 2011;43:491–8.
Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31:213–9.
Ye K, Schulz MH, Long Q, Apweiler R, Ning Z. Pindel: a pattern growth approach to detect break points of large deletions and medium sized insertions from paired-end short reads. Bioinforma. 2009;25:2865–71.
Mayakonda A, Lin DC, Assenov Y, Plass C, Koeffler HP. Maftools: efficient and comprehensive analysis of somatic variants in cancer. Genome Res. 2018;28:1747–56.
Zhang J, Fujimoto J, Zhang J, Wedge DC, Song X, Zhang J, et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science 2014;346:256–9.
Olshen AB, Venkatraman ES, Lucito R, Wigler M. Circular binary segmentation for the analysis of array-based DNA copy number data. Biostatistics. 2004;5:557–72.
Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, et al. STAR: ultrafast universal RNA-seq aligner. Bioinforma. 2013;29:15–21.
Anders S, Pyl PT, Huber W. HTSeq—a Python framework to work with high-throughput sequencing data. Bioinforma. 2015;31:166–9.
Efstathiou E, Titus M, Wen S, Hoang A, Karlou M, Ashe R, et al. Molecular characterization of enzalutamide-treated bone metastatic castration-resistant prostate cancer. Eur Urol. 2015;67:53–60.
Efstathiou E, Titus M, Tsavachidou D, Tzelepi V, Wen S, Hoang A, et al. Effects of abiraterone acetate on androgen signaling in castrate-resistant prostate cancer in bone. J Clin Oncol: Off J Am Soc Clin Oncol. 2012;30:637–43.
Titus MA, Schell MJ, Lih FB, Tomer KB, Mohler JL. Testosterone and dihydrotestosterone tissue levels in recurrent prostate cancer. Clin Cancer Res. 2005;11:4653–7.
Palanisamy N, Yang J, Shepherd PDA, Li-Ning-Tapia EM, Labanca E, Manyam GC, et al. The MD Anderson Prostate Cancer Patient-derived Xenograft Series (MDA PCa PDX) captures the molecular landscape of prostate cancer and facilitates Marker-driven therapy development. Clin Cancer Res. 2020;26:4933–46.
Varkaris A, Corn PG, Parikh NU, Efstathiou E, Song JH, Lee YC, et al. Integrating Murine and clinical trials with Cabozantinib to understand roles of MET and VEGFR2 as targets for growth inhibition of prostate cancer. Clin Cancer Res. 2016;22:107–21.
Arora VK, Schenkein E, Murali R, Subudhi SK, Wongvipat J, Balbas MD, et al. Glucocorticoid receptor confers resistance to antiandrogens by bypassing androgen receptor blockade. Cell 2013;155:1309–22.
Isikbay M, Otto K, Kregel S, Kach J, Cai Y, Vander Griend DJ, et al. Glucocorticoid receptor activity contributes to resistance to androgen-targeted therapy in prostate cancer. Hormones Cancer. 2014;5:72–89.
Missaghian E, Kempná P, Dick B, Hirsch A, Alikhani-Koupaei R, Jégou B, et al. Role of DNA methylation in the tissue-specific expression of the CYP17A1 gene for steroidogenesis in rodents. J Endocrinol. 2009;202:99–109.
Perkins LM, Payne AH. Quantification of P450scc, P450(17) alpha, and iron sulfur protein reductase in Leydig cells and adrenals of inbred strains of mice. Endocrinology 1988;123:2675–82.
Abida W, Cyrta J, Heller G, Prandi D, Armenia J, Coleman I, et al. Genomic correlates of clinical outcome in advanced prostate cancer. Proc Natl Acad Sci USA. 2019;116:11428–36.
Armstrong AJ, Halabi S, Luo J, Nanus DM, Giannakakou P, Szmulewitz RZ, et al. Prospective multicenter validation of androgen receptor Splice Variant 7 and hormone therapy resistance in high-risk castration-resistant prostate cancer: The PROPHECY Study. J Clin Oncol: Off J Am Soc Clin Oncol. 2019;37:1120–9.
Mostaghel EA, Zhang A, Hernandez S, Marck BT, Zhang X, Tamae D, et al. Contribution of adrenal glands to intratumor androgens and growth of castration-resistant prostate cancer. Clin Cancer Res. 2019;25:426–39.
Mostaghel EA, Marck BT, Kolokythas O, Chew F, Yu EY, Schweizer MT, et al. Circulating and intratumoral adrenal androgens correlate with response to abiraterone in men with castration-resistant prostate cancer. Clin Cancer Res. 2021;27:6001–11.
Aparicio AM, Shen L, Tapia EL, Lu JF, Chen HC, Zhang J, et al. Combined tumor suppressor defects characterize clinically defined aggressive variant prostate cancers. Clin Cancer Res. 2016;22:1520–30.
Montgomery RB, Mostaghel EA, Vessella R, Hess DL, Kalhorn TF, Higano CS, et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 2008;68:4447–54.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus Prednisone in metastatic, castration-sensitive prostate cancer. N. Engl J Med. 2017;377:352–60.
Evaul K, Li R, Papari-Zareei M, Auchus RJ, Sharifi N. 3beta-hydroxysteroid dehydrogenase is a possible pharmacological target in the treatment of castration-resistant prostate cancer. Endocrinology 2010;151:3514–20.
Efstathiou E, Davis JW, Pisters L, Li W, Wen S, McMullin RP, et al. Clinical and biological characterisation of localised high-risk prostate cancer: results of a randomised preoperative study of a luteinising hormone-releasing hormone agonist with or without Abiraterone Acetate plus Prednisone. Eur Urol. 2019;76:418–24.
Funding
The experiments reported in this study were funded by the David H. Koch Center for Applied Research of Genitourinary Cancers. AWH is supported by a Conquer Cancer Foundation Young Investigator Award, the Rob Heyvaert and Paul Heynen Prostate Cancer Foundation Young Investigator Award, and philanthropic donations from Michael and Patricia Berns.
Author information
Authors and Affiliations
Contributions
Concept and design: Christopher J. Logothetis and Mark A. Titus. Collection and assembly of data: Minas J Sakellakis, Andrew W. Hahn, Sumankalai Ramachandran, Anh Hoang, Jian H. Song, Peter Sheperd, Miao Zhang, Patricia Troncoso, and Mark A. Titus. Data analysis and interpretation: All authors. Manuscript writing: All authors. Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Competing interests
DEF has received research funding from GTx, Inc and has a familial relationship with Hummingbird Bioscience, Maia Biotechnology, Alms Therapeutics, Hinova Pharmaceuticals, and Barricade Therapeutics. CJL reports commercial research grants from Janssen, ORIC Pharmaceuticals, Novartis, Aragon Pharmaceuticals, and honoraria from Merck, Sharp, and Dohme, Bayer, and Amgen. The other authors report no potential conflicts of interest.
Consent for publication
Informed consent was obtained from each patient for the studies described above and subsequent publication.
Ethics approval
This study was approved by the University of Texas MD Anderson Cancer Center Institutional Review Board and the IACUC committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41391_2022_590_MOESM2_ESM.png
Supplemental Figure 1: Immunohistochemical staining of prostate cancer adrenal metastases for androgen receptor (AR), glucocorticoid receptor (GR), and NKX3.1.
41391_2022_590_MOESM3_ESM.png
Supplemental Figure 2: Organoids developed from MDA-PCa-250 can convert adrenal androgens and progesterone to testosterone
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakellakis, M.J., Hahn, A.W., Ramachandran, S. et al. Characterization of prostate cancer adrenal metastases: dependence upon androgen receptor signaling and steroid hormones. Prostate Cancer Prostatic Dis 26, 751–758 (2023). https://doi.org/10.1038/s41391-022-00590-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00590-x