Abstract
The twenty-first century has been marked by a surge in viral epidemics and pandemics, highlighting the global health challenge posed by emerging and re-emerging pediatric viral diseases. This review article explores the complex dynamics contributing to this challenge, including climate change, globalization, socio-economic interconnectedness, geopolitical tensions, vaccine hesitancy, misinformation, and disparities in access to healthcare resources. Understanding the interactions between the environment, socioeconomics, and health is crucial for effectively addressing current and future outbreaks. This scoping review focuses on emerging and re-emerging viral infectious diseases, with an emphasis on pediatric vulnerability. It highlights the urgent need for prevention, preparedness, and response efforts, particularly in resource-limited communities disproportionately affected by climate change and spillover events. Adopting a One Health/Planetary Health approach, which integrates human, animal, and ecosystem health, can enhance equity and resilience in global communities.
Impact
-
We provide a scoping review of emerging and re-emerging viral threats to global pediatric populations
-
This review provides an update on current pediatric viral threats in the context of the COVID-19 pandemic
-
This review aims to sensitize clinicians, epidemiologists, public health practitioners, and policy stakeholders/decision-makers to the role these viral diseases have in persistent pediatric morbidity and mortality
Similar content being viewed by others
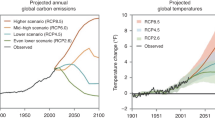
In the first 2 decades of the twenty-first century, the world has witnessed an unprecedented number of viral epidemics and pandemics.1,2,3,4,5,6,7,8,9,10,11,12,13,14 This phenomenon coincides with the growing interconnectedness and interdependence of global society, facilitated by advancements in international trade, travel, and other forms of exchange. These events have been caused by both novel, emerging viral diseases and the resurgence of previously known, now re-emerging infectious diseases, which appear to exploit the impacts of climate change, the socio-economic connectedness of global society, geopolitical tensions, and social dynamics such as vaccine hesitancy and misinformation, as well as an imbalanced lack of access to vaccines, therapeutics, and other health interventions.10,14,15,16,17,18,19,20,21,22,23 There is a pressing need for ongoing global partnership and cooperation in surveillance, research, and preparedness measures to address current and future outbreaks, which require a multidisciplinary approach to tackle the complex interactions between the environment, socioeconomics, and health.19,24 Further, managing these events will also depend on consideration of low-probability, high-risk scenarios.
To develop a framework for preparedness planning for unpredictable events, the World Health Organization (WHO) introduced the concept of “Disease X” in 2018, well before the COVID-19 pandemic.19,25 “Disease X” represents a hypothetical pathogen, a ‘knowable unknown’, that could potentially trigger a future epidemic or pandemic. Since its introduction, “Disease X” has been included in the WHO’s list of emerging infectious diseases for research prioritization. The inclusion of “Disease X” highlights the need for preparedness measures that go beyond known pathogens and anticipate the emergence of new or unknown diseases. The WHO’s research and preparedness efforts for “Disease X” aim to develop effective interventions and response strategies that can be quickly deployed in the event of an outbreak of a new or unknown disease.19,25
The global pandemic caused by SARS-CoV-2 swept the world starting in late 2019 and resulted in the disease COVID-19.11,12,26 While preparation for “Disease X” resulted in calls to action and expert recommendations, chronically underfunded national and international public health institutions were slow to react and bogged down in multinational bureaucracy.27,28 Ultimately, as of April 2023 there have been over 640 million cases and nearly 8 million reported global deaths due to SARS-CoV-2 (the Institute of Health Metrics and Evaluation estimates total SARS-CoV-2-related deaths at over 18 million as of April 2022).29 According to the US Centers for Disease Control and Prevention (CDC), as of April 2023 there have been nearly 17 million cases and 2158 deaths due to SARS-CoV-2 in children and young people under the age of 18 in the United States.30 While transmission to children and young people are similar to adult transmission rates, differences in adult and pediatric mortality, with substantially lower mortality in children and young people, are thought to be mediated by age-associated immunological factors and the prevalence of comorbid conditions with age (increasing risk for hospitalization and death with age).31,32
The United States White House ended its national emergency concerning COVID-19 on May 11, 2023, after just over 3 years (enacted on March 13, 2020).33As our global community reflects on the response and aftermath of the COVID-19 pandemic, there is an urgent need for more effective preparedness and response strategies for emerging and re-emerging viral diseases. Children remain vulnerable to these diseases and the impact on their health and well-being can be severe.26,34,35,36,37,38 Understanding the trends in the emergence and re-emergence of viral diseases, as well as the current state of global efforts to prevent and control them, is critical for addressing this ongoing public health challenge.23 Moreover, the COVID-19 pandemic has revealed the detrimental impact of misinformation and disinformation on public health messaging, highlighting the complex interplay of sociocultural, psychological, and economic factors that shape effective and sustainable approaches to public health communication in the twenty-first century.16,21,22,23,27,39,40 Special attention must be paid to respiratory pathogens of pandemic potential, arboviral diseases whose vector ecology may change in the setting of climate change, and viral hemorrhagic fevers.23
In this scoping review, we showcase key emerging and re-emerging viral infectious diseases of significance, with particular attention to the vulnerability of pediatric patients. This review can inform clinicians, researchers, public health policymakers, stakeholders, and the lay public of the breadth by which to consider and stimulate action on prevention, preparedness, and response efforts. Emphasis must be placed on resource-limited communities that are most disenfranchised and most at-risk of the acute effects of climate change and spillover events, especially in emerging/re-emerging pathogen preparedness and response efforts. Focus on prevention efforts, which must include a One Health/Planetary Health framework, can provide more equity to all in our global community.23
One Health/Planetary Health
One Health is defined as an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems41,42 and is related to Planetary Health, which seeks to address the interconnected challenges of climate change, biodiversity loss, and pollution, which all have negative impacts on human health—“Planetary Health is the health of human civilization and the state of the natural systems on which it depends.”43,44 Adapting a One Health/Planetary Health approach to combat emerging/re-emerging infectious diseases focuses attention on a key weakness of current prevention, preparedness, and response discourse: preventing spillover events, which bring zoonotic diseases in close proximity to humans and domesticated animals.23 All stakeholders must consider the effects of deforestation and land management, global animal husbandry and agricultural practices, and the global commercial wildlife trade.23
Global action to turn polio into a disease of waning significance
Paralytic poliomyelitis is caused by the single-stranded positive-sense RNA poliovirus, a human-restricted enterovirus.45 Since the World Health Assembly unanimously voted to end global polio in 1988, global paralytic polio cases dropped from greater than 350,000 cases per year to only 30 cases at the close of 2022.46,47,48 This great human achievement can serve as a model for addressing other diseases which are candidates for either elimination or eradication, highlighting the principles of success to date due to the development of effective vaccines,49,50 global coordination and political will, and persistence in funding.48 However, despite the great progress that has been made in the fight against polio, political support for elimination efforts has waned. This is a major challenge that must be addressed if we are to achieve the goal of a polio-free world. There is a tremendous need for polio vaccine incentives, especially in the setting of decreasing polio vaccination rates, which have been linked to anti-vaccine groups and vaccine misinformation/disinformation, revisiting the global vaccination strategy as cases of vaccine-derived polio arise, as well as addressing underestimation of polio vaccine global production needs.16,47,51,52
Emerging viral diseases
SARS-CoV-2
SARS-CoV-2, the causative agent of COVID-19, is an enveloped, positive-sense, single-stranded RNA virus in the subgenera Sarbecovirus, genus Betacoronavirus, family Coronaviridae.11 It is the cause of over 640 million cases and nearly 8 million reported global deaths since being first isolated in December 2019 in Wuhan, Hubei Province, China.12,29,53 Since the outset of the global COVID-19 pandemic, the impact of SARS-CoV-2 on pediatric populations has been variably described but appears to have low associated mortality when compared to adults, and yet high multi-factorial morbidity.26,34,35,36,37,54,55 Mechanisms and risk factors for the differential rates of infection and severe disease in children versus adults remain to be elucidated.26,34,36,56,57,58,59 One consequence of SARS-CoV-2 infection that appears to impact children at a higher rate is the subsequent development of multisystem inflammatory syndrome (MIS-C) as a severe complication, which manifests approximately 4–6 weeks after an initial asymptomatic or mild SARS-CoV-2 infection.60,61 The symptoms of MIS-C can vary, but can include persistent fever, chest pain, shortness of breath, rash, fatigue, abdominal pain, and diarrhea.62 Management of children diagnosed with MIS-C or children who develop hyperinflammation and respiratory difficulty associated with severe COVID-19 is centered around immunomodulatory treatments, antivirals such as remdesivir or in select cases Paxlovid (nirmatrelvir-ritonavir), and respiratory support.26,63,64 Children with chronic medical conditions appear to be at higher risk for severe COVID-19.34,65,66
Additional complications arising from acute SARS-CoV-2 infection include “post-COVID-19 condition” (PCC) or “long-COVID” or “post-acute sequelae of SARS-CoV-2 infection” (PASC) or “post-acute COVID-19 syndrome” (PACS), which refer to long-term symptoms and health effects that some individuals experience after recovery from acute SARS-CoV-2 infection,67 and can also occur in children.35,38 To date, there are no evidence-based treatments of PCC, and management is multidisciplinary including targeting specific symptom management. Specialty multidisciplinary pediatric PCC management clinics have been developed to support children with persistent symptoms. Of note, in one adult Veteran’s Affairs cohort study, treatment with the anti-viral Paxlovid (nirmatrelvir-ritonavir) resulted in reduced risk of PCC development, and in a phase 3 double-blind, randomized, placebo-controlled trial metformin was also associated with a reduced risk of PCC development.68,69
Non-pharmaceutical interventions, such as social distancing, hand hygiene and sanitizing practices, masking, and ventilation improvements have been shown to reduce COVID-19 transmission in children;70,71 and more broadly at the population level.72,73,74,75 However, any risk-mitigation intervention(s) must be taken in the context of minimizing impacts on pediatric mental health and well-being,37,76 as well as any social and economic impacts at local, national, and international levels that may require sustained individual effort to maintain their effectiveness. Improved indoor ventilation, air filtration, and air disinfection have been recognized as effective and sustainable alternatives to some of these measures.77
In the United States SARS-CoV-2 vaccines have been primarily the Pfizer/BioNTech Comirnaty BNT162b2 vaccine and the Moderna mRNA-1273 vaccine. These two vaccines have been shown to be safe and have varying degrees of effectiveness when given to children under the age of 18 for preventing infection, transmission, progression to hospitalization and severe COVID-19, death, MIS-C, and perhaps PCC.78,79,80,81,82,83,84,85,86,87 As of May 2023, the United States CDC recommends SARS-CoV-2 vaccination for all persons over the age of 6 months, while the WHO has deprioritized pediatric (6 months to 17 years) vaccination, communicating that globally the limited supply of vaccines should be prioritized for adults who are at higher risk of severe disease.88,89
SARS-CoV-2 remains a potent threat to human health and well-being, and more than serving as a model for future pandemics capable of disrupting the globe, it continues to kill over 5000 people per week—of which, the United States accounts for nearly 1/3 of cases (week of March 25, 2023).90 Further, between April 1, 2020—August 31, 2022, COVID-19 was a leading cause of death in children and young people aged 0–19 years.91
Zika virus
Zika virus (ZIKV) is an enveloped, positive-sense, single-stranded RNA virus in the genus Flavivirus, family Flaviviridae; it is a mosquito-borne virus (arbovirus).92 In 2022 there were a reported >40,000 cases of ZIKV in the Americas.93 It was first discovered in Uganda in the late 1940s,94,95 but has spread globally due to the vector ecology of its preferred Aedes aegypti and Aedes albopictus mosquito vectors.92,96 After multiple outbreaks in the Pacific between 2007–2015, in which ZIKV presented much like dengue virus,97,98,99,100,101 an exanthematic disease began to impact northeastern Brazil in 2015—this likely reflected the introduction of ZIKV into a fully susceptible population.8,102,103 In late 2015, increased microcephaly cases were noted in the most ZIKV-affected areas of Brazil and the WHO subsequently declared a global public health emergency on February 1, 2016.104,105 Further case data has closely linked ZIKV maternal infection during the first two trimesters and subsequent development of microcephaly.106,107,108 The majority of acute cases of ZIKV suffer no complications, but the symptoms most commonly associated with disease in children include fever, rash, conjunctivitis, and arthralgia.109,110,111 Management of acute cases is supportive and there are no evidenced-based, approved therapies for use.111 Recommendations have been made on further subspecialty follow up of infants suspected to have congenital ZIKV infection and subsequent development of congenital ZIKV syndrome associated with microcephaly and other birth defects.112 The causative mechanism of microcephaly, and other birth defects associated with congenital ZIKV syndrome, is still not fully understood and serves as caution to the unanticipated effects of emerging infectious diseases.113 There are no approved vaccines or therapeutics specifically targeting ZIKV, but several are in the pipeline.114
Nipah virus
Nipah virus (NiV) is an enveloped, negative sense, single-stranded RNA virus in the genus Henipavirus, family Paramyxoviridae.115 It was first isolated in 1999 after a Malaysian outbreak from 1998 to 1999 tied to pig farms, resulting in 283 cases and 109 deaths.116,117,118,119 Subsequent outbreaks of NiV in Bangladesh have been tied to the consumption of raw date palm sap that has been contaminated by Pteropus fruit bats (saliva, urine, feces).120,121,122 NiV can be transmitted person-to-person via droplet infection, but is particularly inefficient at using this mechanism of transmission as a driver of infection.123,124 Yet the possibility of developing more efficient person-to-person spread in a pathogen associated with mortality as high as >70%,125 has resulted in prioritizing NiV research due to its pandemic potential, particularly via the Coalition for Epidemic Preparedness Innovations (CEPI).126 Clinically, the disease course is rapid, severe, and associated with acute respiratory distress syndrome.125 In a review of 14 years of data on NiV transmission investigations in Bangladesh, individuals aged 14 years and younger were the most common primary case patients (37%), and within this age demographic, the estimated case fatality rate was nearly 80%.127 There are no approved vaccines or therapeutics specifically targeting NiV, but several are in the pipeline.128
Mpox virus
Mpox virus (mpox; formerly Monkey Pox) is an enveloped, double-stranded DNA virus in the genus Orthopoxvirus, family Poxviridae.129 Mpox is a zoonotic disease (unknown animal reservoir),129 first isolated in 1958 subsequent to outbreaks of smallpox-like disease in cynomolgus monkeys kept in research facilities in Copenhagen, Denmark.130 During the course of smallpox surveillance and eradication campaigns, the first human case of mpox was detected in 1970 in a 9-month-old boy in Basankusu, Democratic Republic of Congo.131 Prior to 2017, outbreaks have been largely limited to the African continent and have not portrayed substantial risk of efficient person-to-person spread.132,133,134,135,136,137 Historical mpox case burden has been disproportionately reported in children.136 A 2003 outbreak of mpox in the United States resulted in over 72 confirmed or suspected cases in children and adults and was due to imported animals from Ghana (Gambian pouched rats that infected prairie dogs).138
In 2017–2018 a large outbreak of mpox occurred in Nigeria, primarily in male adults, with higher rates of person-to-person spread, and was hypothesized to involve sexual transmission and increased severity amongst people living with HIV.139,140,141 Starting in May 2022, the largest outbreak of mpox in history occurred, resulting in over 86,000 confirmed cases globally, mostly in the United States (>30,000 cases).129,142 The WHO declared the outbreak a public health emergency of international concern on July 23, 2022.143 The majority of cases in the 2022 mpox outbreak have occurred in men who have sex with men (MSM), >90% of cases across cohorts, with evidence of mucosal transmission through sexual contact as a possible key driver of transmission.144,145,146 While pediatric cases of mpox during the 2022 outbreak were rare (~40 US cases ≤15 years of age),147 prior data suggest an increased risk for severe disease in children.133,134,135,148 During the 2022 outbreak, the smallpox vaccine ACAM2000 (Pasteur Biologics Company) and the smallpox/mpox vaccine JYNNEOS (Bavarian Nordic) have been utilized for pre- and post-exposure prophylaxis,149 with a preliminary vaccine effectiveness of a single dose of subcutaneous JYNNEOS vaccine (full schedule includes 2 doses) of 86% reduction in risk for mpox in vaccinated individuals.150 The anti-viral TPOXX (tecovirimat; SIGA Technologies), an FDA-approved treatment for smallpox,151 was used for treatment of severe mpox under the FDA-regulated Expanded Access Investigational New Drug program, with encouraging but limited efficacy and safety data.152,153,154 Other drugs investigated, given pre-clinical effectiveness against mpox, include brincidofovir and cidofovir, but use of either drug is limited secondary to their side-effect profiles.154,155 Of note, a disproportionate fraction of mpox cases were experienced by people living with HIV,144,145,146,156 emphasizing the importance of education, communication, and prevention efforts in high-risk communities. Further, the case series identified an increased risk of progression to severe mpox disease and death in people living with advanced HIV/AIDS not on antiretroviral therapy,157,158 suggesting special attention to immunocompromised hosts. The global response to mpox has been effective in reducing the number of cases worldwide as of March 2023.159 However, this success is overshowed by issues in health inequity, especially as experienced by the African countries with long histories of mpox outbreaks, primarily affecting children, and wherein the disease is endemic. Despite the epidemiologic historical burden, these countries have not received equal access to mpox vaccines or antivirals.149,160,161
Re-emerging infectious diseases
Ebola virus
Ebola virus (EBOV) is an enveloped, negative sense, single-stranded RNA virus in the genus Ebolavirus, family Filoviridae, and the causative agent of Ebola virus disease (EVD).162 In 1976 simultaneous, but separate, viral hemorrhagic fever outbreaks in the Democratic Republic of the Congo (previously Zaire) and Sudan resulted in the isolation of EBOV.163,164,165,166,167 In these original outbreaks, the case fatality rate was 88% in Zaire and 53% in Sudan.166,167 Until 2013, most EBOV outbreaks occurred in Central Africa.162 The largest historical EBOV outbreak, declared an epidemic, occurred between late 2013 and early 2016 throughout West Africa (officially the 2014–2016 West African Ebola epidemic), spreading from Guinea to Liberia and Sierra Leone, and declared a WHO Public Health Emergency of International Concern on August 8, 2014.168,169,170 This outbreak resulted in more than 28,600 cases and 11,325 deaths, with an estimated adjusted case fatality ratio of nearly 83%.171,172 While children and young people represent a smaller proportion of overall cases, children under 5 years of age experience a shorter EVD incubation period and higher risk of death compared to older children and young people,173,174 emphasizing the importance of rapid assessment of young children in the context of future EBOV outbreaks.
Of note, a related filovirus—Marburg virus (MARV)—has resulted in outbreaks in Guinea, Ghana, Equatorial Guinea, and Tanzania between 2021–2023.175 Although data are limited, the impact of Marburg virus disease (MVD) on children and young persons is likely similar to that of EVD, highlighting the need for heightened surveillance.
Measles virus
Measles virus (MV, also known as rubeola) is an enveloped, negative sense, single-stranded RNA virus in the genus Morbillivirus, family Paramyxoviridae.176 MV is transmitted via respiratory droplets and aerosols, is highly contagious, and lifelong immunity follows the survival of infection or vaccination.176 As there are no natural MV non-human reservoirs and there is a highly effective vaccine, MV elimination and eradication are possible and efforts to achieve these goals have been a global priority for decades. Prior to widespread measles vaccination, MV resulted in an estimated over 2.6 million global deaths per year, mostly among children under five years of age, dropping to over 760,000 global deaths in the year 2000 and down to just over 127,000 in 2021.177 Unfortunately, global MV cases and deaths have steadily increased since 2016, driven largely by a failure to vaccinate persons.177,178 Most of these deaths occur in children under the age of five.177,178 Children who are malnourished or have weakened immune systems, especially those living in low and middle-income countries (LMIC), are at the highest risk for severe illness and death.176 Additionally, complications of measles infection in children include blindness, deafness, and brain damage.176 The resurgence of measles in high-income country settings, and the failure to complete measles elimination in LMIC settings speak to the importance of persistent investment in global vaccination and surveillance, as well as the threat of vaccine hesitancy and vaccine misinformation/disinformation, which erode the public’s trust and imperil global vaccination efforts to prevent infection and disease.16,179
Dengue virus
Dengue virus (DENV) is an enveloped, positive-sense, single-stranded RNA virus in the genus Flavivirus, family Flaviviridae, and the causative agent of dengue fever.180,181 It is a mosquito-borne virus (arbovirus) spread primarily by the Aedes aegypti mosquito (also, less commonly, via Aedes albopictus).180,181 There are four dengue serotypes (DENV-1, DENV-2, DENV-3 and DENV-4), and initial infection with one serotype followed by subsequent infection with another may result in severe dengue, associated with dengue hemorrhagic fever and dengue shock syndrome via antibody-dependent enhancement.180,181,182 Dengue is considered the most rapidly spreading mosquito-borne infectious disease in the world, with a recorded approximately 500,000 cases in the year 2000 increasing to over 5 million cases in 2019,183 while modeled estimates suggest true case burden is likely as much as 400 million cases per year in 2021.183,184 As is true for many arboviral diseases, dengue incidence is most common among children and young persons.185 Further, dengue infection is disproportionately more severe in children (including hemorrhagic disease and neurologic manifestations of disease), with severe consequences of maternal-fetal infection.186,187,188 Treatment of dengue is supportive, and there are no evidence-based, approved therapies or antivirals.182 There is one internationally licensed dengue vaccine with WHO prequalification, Dengvaxia produced by Sanofi Pasteur, which is indicated for adults, young people and children (from 6 to 45 years of age) with prior dengue virus infection confirmed by test; it is not indicated for travelers and is only approved in the United States for children (age 6–16 years) with laboratory-confirmed previous dengue infection and who live in endemic areas.182,189,190 Serologic testing for prior dengue infection is required prior to vaccination with Dengvaxia because persons without prior history of dengue infection are at-risk for severe dengue if they are infected with DENV after vaccination, similar to the risk of secondary serotype infection that causes antibody-dependent enhancement.191 There are several other vaccine candidates in the pre-clinical and clinical evaluation pipeline, some of which may not require pre-vaccination serologic testing.192
Chikungunya virus
Chikungunya virus (CHIKV) is an enveloped, positive-sense, single-stranded RNA virus in the genus Alphaviridae, family Togaviridae, and the causative agent of chikungunya fever. It is a mosquito-borne virus (arbovirus) spread by Aedes mosquitoes (aegypti, albopictus, africanus, furcifer-taylori, dalzeili).193 First described during an outbreak of dengue-like illness between 1952-1953 in southern Tanzania, it has spread across the globe in a similar pattern as ZIKV subsequently did from Africa, to the Asia/Pacific region, and finally, to Europe and the Americas—all largely driven by the geographically and ecologically diverse habitats in which Aedes mosquitoes can thrive.193,194,195 Chikungunya fever is an acute febrile disease associated with severe arthralgia and arthritis, as well as headache and maculopapular rash—in comparison to DENV, CHIKV infection is more frequently associated with symptomatic disease.193,196,197 In children, cutaneous, neurologic, and hematologic manifestations are more broad and sometimes more common than in adults (although data are limited), including pigmentation, bullous rash, blistering, seizures, encephalopathy, thrombocytopenia, hemorrhage, and lymphopenia.194,195,198,199,200,201 There are no approved vaccines or therapeutics specifically targeting CHIKV, but several are in development.201,202
A One Health/Planetary Health approach is key to global child health
The COVID-19 pandemic has highlighted the global community’s lack of preparedness for the next viral pandemic, given the political and socio-economic impacts of the current crisis. Unfortunately, we may not have time to prepare for impending new pandemics, as the global spread of highly pathogenic avian influenza H5N1 viruses has resulted in the culling or death of tens of millions of poultry and wild birds since 2022.203,204 The increasing mammalian spillover of H5N1, although still inefficient at human transmission, raises concerns about the ability of the virus to evolve as a more transmissible pathogen to mammals, including humans. The threat of another pathogen outbreak is compounded by the spread of misinformation and disinformation in a globally interconnected society. Moreover, the effects of climate change disproportionately impact under-served communities with scarce resources, resulting in widened gaps in health equity. Experts fear that climate change could increase the geographic spread of Aedes aegypti, causing a shift from long-standing infectious diseases of certain locations, such as malaria spread by Anopheles mosquitoes, to more arboviral diseases with limited vaccines and therapeutics.205 Preparing for low-probability, high-risk events, such as “Disease X”, will be of increasing importance. Addressing these issues requires international governmental partnerships that adopt a One Health/Planetary Health framework and ensure equitable distribution of resources, thereby preventing the disproportionate burden of emerging and re-emerging viral infectious diseases on all populations and especially children.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Drosten, C. et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome.N. Engl. J. Med. 348, 1967–1976 (2003).
LeDuc, J. & Barry, M. A. SARS, the first pandemic of the 21st century. Emerg. Infect. Dis. J. 10, e26 (2004).
Jones, K. E. et al. Global trends in emerging infectious diseases. Nature 451, 990–993 (2008).
Dawood, F. S. et al. Emergence of a Novel Swine-Origin Influenza a (H1n1) virus in humans. N. Engl. J. Med. 360, 2605–2615 (2009).
Smith, G. J. et al. Origins and evolutionary genomics of the 2009 swine-origin H1n1 influenza a epidemic. Nature 459, 1122–1125 (2009).
Zaki, A. M., van Boheemen, S., Bestebroer, T. M., Osterhaus, A. D. & Fouchier, R. A. Isolation of a novel coronavirus from a man with Pneumonia in Saudi Arabia. N. Engl. J. Med. 367, 1814–1820 (2012).
Team, W. H. O. E. R. et al. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N. Engl. J. Med. 371, 1481–1495 (2014).
Zanluca, C. et al. First report of autochthonous transmission of Zika virus in Brazil. Mem. Inst. Oswaldo Cruz 110, 569–572 (2015).
Mlakar, J. et al. Zika virus associated with microcephaly. N. Engl. J. Med. 374, 951–958 (2016).
Bedford, J. et al. A new twenty-first century science for effective epidemic response. Nature 575, 130–136 (2019).
Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-Ncov and naming it Sars-Cov-2. Nat. Microbiol. 5, 536–544 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel Coronavirus in Wuhan, China. Lancet 395, 497–506 (2020).
Roychoudhury, S. et al. Viral pandemics of the last four decades: pathophysiology, health impacts and perspectives. Int. J. Environ. Res. Public Health 17, 9411 (2020).
Marani, M., Katul, G. G., Pan, W. K. & Parolari, A. J. Intensity and frequency of extreme novel epidemics. Proc. Natl Acad. Sci. USA 118, e2105482118 (2021).
Hughes, J. M. et al. The origin and prevention of pandemics. Clin. Infect. Dis. 50, 1636–1640 (2010).
Garett, R. & Young, S. D. Online misinformation and vaccine hesitancy. Transl. Behav. Med. 11, 2194–2199 (2021).
Zappa, A., Amendola, A., Romanò, L. & Zanetti, A. Emerging and re-emerging viruses in the era of globalisation. Blood Transfus. 7, 167–171 (2009).
Bloom, D. E. & Cadarette, D. Infectious disease threats in the twenty-first century: strengthening the global response. Front. Immunol. 10, 549 (2019).
Grubaugh, N. D. et al. Tracking virus outbreaks in the twenty-first century. Nat. Microbiol. 4, 10–19 (2019).
Wolfe, N. D., Dunavan, C. P. & Diamond, J. Origins of major human infectious diseases. Nature 447, 279–283 (2007).
Wilhelm, E. et al. Measuring the burden of infodemics: summary of the methods and results of the Fifth Who Infodemic Management Conference. JMIR Infodemiol. 3, e44207 (2023).
Cooks, E. J. et al. What did the pandemic teach us about effective health communication? Unpacking the Covid-19 infodemic. BMC Public Health 22, 2339 (2022).
Vora, N. M. et al. Interventions to reduce risk for pathogen spillover and early disease spread to prevent outbreaks, epidemics, and pandemics. Emerg. Infect. Dis. 29, 1–9 (2023).
Holmes, E. C., Rambaut, A. & Andersen, K. G. Pandemics: spend on surveillance, not prediction. Nature 558, 180–182 (2018).
World Health Organization. Prioritizing Diseases for Research and Development in Emergency Contexts, <https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts> (World Health Organization, 2023).
Zachariah, P. Covid-19 in children. Infect. Dis. Clin. North Am. 36, 1–14 (2022).
Assefa, Y. et al. Analysis of the Covid-19 pandemic: lessons towards a more effective response to public health emergencies. Glob. Health 18, 10 (2022).
Bollyky, T. J. et al. Assessing Covid-19 pandemic policies and behaviours and their economic and educational trade-offs across US States from Jan 1, 2020, to July 31, 2022: an observational analysis. Lancet 401, 1341–1360 (2023).
Institute for Health Metrics and Evaluation (IHME). Covid-19 Projections., <https://covid19.healthdata.org/> (IHME, 2023).
CDC. Covid Data Tracker: Pediatric Data, <https://covid.cdc.gov/covid-data-tracker/#pediatric-data> (CDC, 2023).
Smith, C. et al. Deaths in children and young people in England after Sars-Cov-2 infection during the first pandemic year. Nat. Med. 28, 185–192 (2022).
Wilde, H. et al. Hospital admissions linked to Sars-Cov-2 infection in children and adolescents: cohort study of 3.2 million first ascertained infections in England. BMJ 382, e073639 (2023).
The White House. Notice on the Continuation of the National Emergency Concerning the Coronavirus Disease 2019 (Covid-19) Pandemic, <https://www.whitehouse.gov/briefing-room/presidential-actions/2023/02/10/notice-on-the-continuation-of-the-national-emergency-concerning-the-coronavirus-disease-2019-covid-19-pandemic-3/> (The White House, 2023).
Woodruff, R. C. et al. Risk factors for severe Covid-19 in children. Pediatrics 149, e2021053418 (2022).
Lopez-Leon, S. et al. Long-Covid in children and adolescents: a systematic review and meta-analyses. Sci. Rep. 12, 9950 (2022).
Howard-Jones, A. R. et al. Covid-19 in children. II: Pathogenesis, Disease Spectrum and Management. J. Paediatr. Child Health 58, 46–53 (2022).
Dalabih, A., Bennett, E. & Javier, J. R. The Covid-19 pandemic and pediatric mental health: advocating for improved access and recognition. Pediatr. Res 91, 1018–1020 (2022).
Behnood, S. A. et al. Persistent symptoms following Sars-Cov-2 infection amongst children and young people: a meta-analysis of controlled and uncontrolled studies. J. Infect. 84, 158–170 (2022).
Eggli, Y. & Rousson, V. Lessons from a pandemic. PLoS Glob Public Health 2, e0000404 (2022).
Dzinamarira, T. et al. The case to scale up edutainment as an effective public health communication intervention to combat the Covid-19 pandemic in Zimbabwe. Health Promot. Perspect. 12, 34–36 (2022).
Mwangi, W., de Figueiredo, P. & Criscitiello, M. F. One health: addressing global challenges at the nexus of human, animal, and environmental health. PLoS Pathog. 12, e1005731 (2016).
World Health Organization. Tripartite and Unep Support Ohhlep’s Definition of “One Health”, <https://www.who.int/news/item/01-12-2021-tripartite-and-unep-support-ohhlep-s-definition-of-one-health> (World Health Organization, 2021).
Horton, R. et al. From public to Planetary Health: a manifesto. Lancet 383, 847 (2014).
Whitmee, S. et al. Safeguarding human health in the Anthropocene Epoch: report of the Rockefeller Foundation-Lancet Commission on Planetary Health. Lancet 386, 1973–2028 (2015).
Racaniello, V. R. One hundred years of poliovirus pathogenesis. Virology 344, 9–16 (2006).
World Health Organization. Poliomyelitis (Polio), <https://www.who.int/health-topics/poliomyelitis> (World Health Organization, 2022).
Maldonado, Y. A. Lessons from a House on Fire—from Smallpox to Polio. J. Infect. Dis. 227, 1025–1027 (2023).
Bigouette, J. P. et al. Progress toward polio eradication-worldwide, January 2019-June 2021. MMWR Morb. Mortal. Wkly Rep. 70, 1129–1135 (2021).
Salk, J. E. Studies in human subjects on active immunization against poliomyelitis. I. A preliminary report of experiments in progress. J. Am. Med Assoc. 151, 1081–1098 (1953).
Sabin, A. B. Properties and behavior of orally administered attenuated poliovirus vaccine. J. Am. Med Assoc. 164, 1216–1223 (1957).
Conis, E. The history of the personal belief exemption. Pediatrics 145, e20192551 (2020).
Batson, A. et al. The world needs to prepare now to prevent polio resurgence post eradication. BMJ Glob. Health 7, e011485 (2022).
Zhu, N. et al. A novel coronavirus from patients with Pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Lu, X. et al. Sars-Cov-2 infection in children. N. Engl. J. Med. 382, 1663–1665 (2020).
Castagnoli, R. et al. Severe acute respiratory syndrome coronavirus 2 (Sars-Cov-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 174, 882–889 (2020).
Steinman, J. B., Lum, F. M., Ho, P. P., Kaminski, N. & Steinman, L. Reduced development of Covid-19 in children reveals molecular checkpoints gating pathogenesis illuminating potential therapeutics. Proc. Natl Acad. Sci. USA 117, 24620–24626 (2020).
Bunyavanich, S., Do, A. & Vicencio, A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA 323, 2427–2429 (2020).
Poston, D. et al. Absence of severe acute respiratory syndrome coronavirus 2 neutralizing activity in prepandemic sera from individuals with recent seasonal coronavirus infection. Clin. Infect. Dis. 73, e1208–e1211 (2021).
Pierce, C. A. et al. Natural mucosal barriers and Covid-19 in children. JCI Insight 6, e148694 (2021).
Riphagen, S., Gomez, X., Gonzalez-Martinez, C., Wilkinson, N. & Theocharis, P. Hyperinflammatory shock in children during Covid-19 pandemic. Lancet 395, 1607–1608 (2020).
Feldstein, L. R. et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N. Engl. J. Med. 383, 334–346 (2020).
CDC. Information for Healthcare Providers About Multisystem Inflammatory Syndrome in Children (Mis-C), <https://www.cdc.gov/mis/mis-c/hcp_cstecdc/index.html#:~:text=Case%20Definition%20for%20MIS%2DC&text=Any%20illness%20in%20a%20person,The%20vital%20records%20criteria%20(Suspect)> (CDC, 2023).
Henderson, L. A. et al. American College of Rheumatology Clinical Guidance for Multisystem Inflammatory Syndrome in children associated with Sars-Cov-2 and hyperinflammation in pediatric Covid-19: version 3. Arthritis Rheumatol. 74, e1–e20 (2022).
Chiotos, K. et al. Multicenter interim guidance on use of antivirals for children with coronavirus disease 2019/severe acute respiratory syndrome coronavirus 2. J. Pediatr. Infect. Dis. Soc. 10, 34–48 (2021).
Saatci, D. et al. Association between race and Covid-19 outcomes among 2.6 million children in England. JAMA Pediatr. 175, 928–938 (2021).
Kim, L. et al. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed Covid-19-Covid-Net, 14 States, March 1-July 25, 2020. MMWR Morb. Mortal. Wkly Rep. 69, 1081–1088 (2020).
Nalbandian, A. et al. Post-acute Covid-19 syndrome. Nat. Med. 27, 601–615 (2021).
Xie, Y., Choi, T. & Al-Aly, Z. Association of treatment with Nirmatrelvir and the risk of post–covid-19 condition. JAMA Intern. Med. 183, 554–564 (2023).
Bramante, C. T. et al. Outpatient treatment of Covid-19 and incidence of post-Covid-19 condition over 10 months (Covid-out): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial. Lancet Infect. Dis. 23, 1119–1129 (2023).
Blaisdell, L. L., Cohn, W., Pavell, J. R., Rubin, D. S. & Vergales, J. E. Preventing and mitigating Sars-Cov-2 transmission-four overnight camps, Maine, June-August 2020. MMWR Morb. Mortal. Wkly Rep. 69, 1216–1220 (2020).
Garst, B. A., Dubin, A. & Gaslin, T. Application of non-pharmaceutical interventions in camps following the onset of Covid-19. Child Care Health Dev. 48, 956–962 (2022).
Fazio, R. H. et al. Social distancing decreases an individual’s likelihood of contracting Covid-19. Proc. Natl Acad. Sci. USA 118, e2023131118 (2021).
Sun, K. S. et al. Effectiveness of different types and levels of social distancing measures: a scoping review of global evidence from earlier stage of Covid-19 pandemic. BMJ Open 12, e053938 (2022).
Abaluck, J. et al. Impact of community masking on Covid-19: a cluster-randomized trial in Bangladesh. Science 375, eabi9069 (2022).
Andrejko, K. L. et al. Effectiveness of face mask or respirator use in indoor public settings for prevention of Sars-Cov-2 infection-California, February-December 2021. MMWR Morb. Mortal. Wkly Rep. 71, 212–216 (2022).
Meherali, S. et al. Mental health of children and adolescents amidst Covid-19 and past pandemics: a rapid systematic review. Int. J. Environ. Res. Public Health 18, 3432 (2021).
Bueno de Mesquita, P. J., Delp, W. W., Chan, W. R., Bahnfleth, W. P. & Singer, B. C. Control of airborne infectious disease in buildings: evidence and research priorities. Indoor Air 32, e12965 (2022).
Polack, F. P. et al. Safety and efficacy of the Bnt162b2 Mrna Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615 (2020).
Ali, K. et al. Evaluation of Mrna-1273 Sars-Cov-2 vaccine in adolescents. N. Engl. J. Med. 385, 2241–2251 (2021).
Frenck, R. W. Jr. et al. Safety, immunogenicity, and efficacy of the Bnt162b2 Covid-19 vaccine in adolescents. N. Engl. J. Med. 385, 239–250 (2021).
Anderson, E. J. et al. Evaluation of Mrna-1273 vaccine in children 6 months to 5 years of age. N. Engl. J. Med. 387, 1673–1687 (2022).
Creech, C. B. et al. Evaluation of Mrna-1273 Covid-19 vaccine in children 6 to 11 years of age. N. Engl. J. Med. 386, 2011–2023 (2022).
Hause, A. M. et al. Safety of Covid-19 vaccination in United States Children ages 5 to 11 Years. Pediatrics 150, e2022057313 (2022).
Walter, E. B. et al. Evaluation of the Bnt162b2 Covid-19 vaccine in children 5 to 11 years of age. N. Engl. J. Med. 386, 35–46 (2022).
Fleming-Dutra, K. E. et al. Preliminary estimates of effectiveness of monovalent Mrna vaccines in preventing symptomatic Sars-Cov-2 infection among children aged 3-5 Years-increasing community access to testing program, United States, July 2022-February 2023. MMWR Morb. Mortal. Wkly Rep. 72, 177–182 (2023).
Muñoz, F. M. et al. Evaluation of Bnt162b2 Covid-19 vaccine in children younger than 5 years of age. N. Engl. J. Med. 388, 621–634 (2023).
Watanabe, A. et al. Assessment of efficacy and safety of Mrna Covid-19 vaccines in children Aged 5 to 11 years: a systematic review and meta-analysis. JAMA Pediatr. 177, 384–394 (2023).
CDC. Stay up to Date with Covid-19 Vaccines, <https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html#children> (CDC, 2023).
World Health Organization. Sage Updates Covid-19 Vaccination Guidance, <https://www.who.int/news/item/28-03-2023-sage-updates-covid-19-vaccination-guidance> (World Health Organization, 2023).
World Health Organization. WHO Covid-19 Dashboard, <https://covid19.who.int/data> (World Health Organization, 2023).
Flaxman, S. et al. Assessment of Covid-19 as the underlying cause of death among children and young people aged 0 to 19 years in the US. JAMA Netw. Open 6, e2253590–e2253590 (2023).
Musso, D. & Gubler, D. J. Zika virus. Clin. Microbiol. Rev. 29, 487–524 (2016).
PAHO. Zika, <https://www3.paho.org/data/index.php/en/mnu-topics/zika.html> (PAHO, 2023).
Dick, G. W., Kitchen, S. F. & Haddow, A. J. Zika Virus. I. Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 46, 509–520 (1952).
Dick, G. W. Zika Virus. II. pathogenicity and physical properties. Trans. R. Soc. Trop. Med. Hyg. 46, 521–534 (1952).
Musso, D., Cao-Lormeau, V. M. & Gubler, D. J. Zika Virus: following the path of Dengue and Chikungunya? Lancet 386, 243–244 (2015).
Cao-Lormeau, V. M. et al. Zika virus, French Polynesia, South Pacific, 2013. Emerg. Infect. Dis. 20, 1085–1086 (2014).
Dupont-Rouzeyrol, M. et al. Co-infection with Zika and Dengue viruses in 2 patients, New Caledonia, 2014. Emerg. Infect. Dis. 21, 381–382 (2015).
Musso, D., Nilles, E. J. & Cao-Lormeau, V. M. Rapid spread of emerging Zika virus in the Pacific Area. Clin. Microbiol. Infect. 20, O595–O596 (2014).
Roth, A. et al. Concurrent outbreaks of Dengue, Chikungunya and Zika virus infections -an unprecedented epidemic wave of mosquito-borne viruses in the Pacific 2012-2014. Eur. Surveill. 19, 20929 (2014).
Duffy, M. R. et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N. Engl. J. Med. 360, 2536–2543 (2009).
Cardoso, C. W. et al. Outbreak of exanthematous illness associated with Zika, Chikungunya, and Dengue Viruses, Salvador, Brazil. Emerg. Infect. Dis. 21, 2274–2276 (2015).
Campos, G. S., Bandeira, A. C. & Sardi, S. I. Zika Virus Outbreak, Bahia, Brazil. Emerg. Infect. Dis. 21, 1885–1886 (2015).
Schuler-Faccini, L. et al. Possible association between Zika Virus Infection and Microcephaly—Brazil, 2015. MMWR Morb. Mortal. Wkly Rep. 65, 59–62 (2016).
Gulland, A. Zika virus is a global public health emergency, declares WHO. BMJ 352, i657 (2016).
van der Linden, V. et al. Description of 13 infants born during October 2015-January 2016 with Congenital Zika Virus infection without microcephaly at birth-Brazil. MMWR Morb. Mortal. Wkly Rep. 65, 1343–1348 (2016).
Moura da Silva, A. A. et al. Early growth and neurologic outcomes of infants with probable congenital Zika Virus syndrome. Emerg. Infect. Dis. 22, 1953–1956 (2016).
Brady, O. J. et al. The association between Zika Virus infection and microcephaly in Brazil 2015-2017: an observational analysis of over 4 million births. PLoS Med. 16, e1002755 (2019).
Li, J. et al. Characteristics of Zika virus disease in children: clinical, hematological, and virological findings from an outbreak in Singapore. Clin. Infect. Dis. 64, 1445–1448 (2017).
Goodman, A. B. et al. Characteristics of children aged <18 years with Zika virus disease acquired postnatally-U.S. States, January 2015-July 2016. MMWR Morb. Mortal. Wkly Rep. 65, 1082–1085 (2016).
Fleming-Dutra, K. E. et al. Update: interim guidelines for health care providers caring for infants and children with possible Zika virus infection-United States, February 2016. MMWR Morb. Mortal. Wkly Rep. 65, 182–187 (2016).
Adebanjo, T. et al. Update: interim guidance for the diagnosis, evaluation, and management of infants with possible congenital Zika virus infection-United States, October 2017. MMWR Morb. Mortal. Wkly Rep. 66, 1089–1099 (2017).
Rasmussen, S. A., Jamieson, D. J., Honein, M. A. & Petersen, L. R. Zika Virus and birth defects—reviewing the evidence for causality. N. Engl. J. Med 374, 1981–1987 (2016).
Wang, Y., Ling, L., Zhang, Z. & Marin-Lopez, A. Current advances in Zika vaccine development. Vaccines (Basel) 10, 1816 (2022).
Aditi & Shariff, M. Nipah virus infection: a review. Epidemiol. Infect. 147, e95 (2019).
Paton, N. I. et al. Outbreak of Nipah-Virus Infection among Abattoir Workers in Singapore. Lancet 354, 1253–1256 (1999).
Parashar, U. D. et al. Case-control study of risk factors for human infection with a new zoonotic paramyxovirus, Nipah Virus, during a 1998-1999 outbreak of severe encephalitis in Malaysia. J. Infect. Dis. 181, 1755–1759 (2000).
Chua, K. B. Nipah virus outbreak in Malaysia. J. Clin. Virol. 26, 265–275 (2003).
Chua, K. B. et al. Fatal encephalitis due to Nipah Virus amonG Pig-farmers in Malaysia. Lancet 354, 1257–1259 (1999).
Luby, S. P. et al. Foodborne transmission of Nipah Virus, Bangladesh. Emerg. Infect. Dis. 12, 1888–1894 (2006).
Khan, M. S. et al. Use of infrared camera to understand bats’ access to date Palm sap: implications for preventing Nipah Virus transmission. Ecohealth 7, 517–525 (2010).
Luby, S. P. & Gurley, E. S. Epidemiology of Henipavirus disease in humans. Curr. Top. Microbiol. Immunol. 359, 25–40 (2012).
Gurley, E. S. et al. Person-to-person transmission of Nipah virus in a bangladeshi community. Emerg. Infect. Dis. 13, 1031–1037 (2007).
Homaira, N. et al. Nipah virus outbreak with person-to-person transmission in a district of Bangladesh, 2007. Epidemiol. Infect. 138, 1630–1636 (2010).
Hossain, M. J. et al. Clinical presentation of Nipah virus infection in Bangladesh. Clin. Infect. Dis. 46, 977–984 (2008).
Gouglas, D., Christodoulou, M., Plotkin, S. A. & Hatchett, R. Cepi: driving progress toward epidemic preparedness and response. Epidemiol. Rev. 41, 28–33 (2019).
Nikolay, B. et al. Transmission of Nipah Virus-14 years of investigations in Bangladesh. N. Engl. J. Med. 380, 1804–1814 (2019).
Amaya, M. & Broder, C. C. Vaccines to emerging viruses: Nipah and Hendra. Annu. Rev. Virol. 7, 447–473 (2020).
Gessain, A., Nakoune, E. & Yazdanpanah, Y. Monkeypox. N. Engl. J. Med. 387, 1783–1793 (2022).
Magnus, P. V., Andersen, E. K., Petersen, K. B. & Birch-Andersen, A. A Pox-Like disease in Cynomolgus monkeys. Acta Pathol. Microbiol. Scand. 46, 156–176 (1959).
Ladnyj, I. D., Ziegler, P. & Kima, E. A human infection caused by Monkeypox Virus in Basankusu Territory, Democratic Republic of the Congo. Bull. World Health Organ. 46, 593–597 (1972).
Lourie, B. et al. Human infection with Monkeypox virus: laboratory investigation of Six Cases in West Africa. Bull. World Health Organ. 46, 633–639 (1972).
Breman, J. G. et al. Human Monkeypox, 1970-79. Bull. World Health Organ. 58, 165–182 (1980).
Hutin, Y. J. et al. Outbreak of Human Monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerg. Infect. Dis. 7, 434–438 (2001).
Meyer, H. et al. Outbreaks of disease suspected of being due to human Monkeypox virus infection in the democratic Republic of Congo in 2001. J. Clin. Microbiol. 40, 2919–2921 (2002).
Beer, E. M. & Rao, V. B. A systematic review of the epidemiology of human Monkeypox outbreaks and implications for outbreak strategy. PLoS Negl. Trop. Dis. 13, e0007791 (2019).
Bunge, E. M. et al. The changing epidemiology of human monkeypox-a potential threat? A systematic review. PLOS Negl. Trop. Dis. 16, e0010141 (2022).
CDC. Update: multistate outbreak of monkeypox-Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. MMWR Morb. Mortal. Wkly Rep. 52, 642–646 (2003).
Yinka-Ogunleye, A. et al. Reemergence of human Monkeypox in Nigeria, 2017. Emerg. Infect. Dis. 24, 1149–1151 (2018).
Yinka-Ogunleye, A. et al. Outbreak of human Monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. Lancet Infect. Dis. 19, 872–879 (2019).
Ogoina, D. et al. The 2017 human Monkeypox outbreak in Nigeria-report of outbreak experience and response in the Niger Delta University teaching hospital, Bayelsa State, Nigeria. PLoS ONE 14, e0214229 (2019).
CDC. 2022 Mpox Outbreak Global Map, <https://www.cdc.gov/poxvirus/mpox/response/2022/world-map.html> (CDC, 2023).
Wenham, C. & Eccleston-Turner, M. Monkeypox as a Pheic: implications for Global Health Governance. Lancet 400, 2169–2171 (2022).
Philpott, D. et al. Epidemiologic and clinical characteristics of Monkeypox cases-United States, May 17-July 22, 2022. MMWR Morb. Mortal. Wkly Rep. 71, 1018–1022 (2022).
Thornhill, J. P. et al. Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series. Lancet 400, 1953–1965 (2022).
Thornhill, J. P. et al. Monkeypox virus infection in humans across 16 countries-April–June 2022. N. Engl. J. Med. 387, 679–691 (2022).
CDC. Mpox Cases by Age and Gender and Race and Ethnicity, <https://www.cdc.gov/poxvirus/mpox/response/2022/demographics.html> (CDC, 2023).
Huhn, G. D. et al. Clinical characteristics of Human Monkeypox, and risk factors for severe disease. Clin. Infect. Dis. 41, 1742–1751 (2005).
Titanji, B. K. & Marconi, V. C. Vaxxing to elimination: smallpox vaccines as tools to fight Mpox. J. Clin. Invest. 133, e167632 (2023).
Wolff Sagy, Y. et al. Real-world effectiveness of a single dose of Mpox vaccine in males. Nat. Med. 29, 748–752 (2023).
Merchlinsky, M. et al. The development and approval of Tecoviromat (Tpoxx(®)), the first antiviral against smallpox. Antivir. Res. 168, 168–174 (2019).
Matias, W. R. et al. Tecovirimat for the treatment of human Monkeypox: an initial series from Massachusetts, United States. Open Forum Infect. Dis. 9, ofac377 (2022).
O’Laughlin, K. et al. Clinical use of Tecovirimat (Tpoxx) for treatment of Monkeypox under an investigational new drug protocol-United States, May-August 2022. MMWR Morb. Mortal. Wkly Rep. 71, 1190–1195 (2022).
Fox, T. et al. Therapeutics for treating Mpox in humans. Cochrane Database Syst. Rev. 3, Cd015769 (2023).
Siegrist, E. A. & Sassine, J. Antivirals with activity against Mpox: a clinically oriented review. Clin. Infect. Dis. 76, 155–164 (2022).
Curran, K. G. et al. Hiv and sexually transmitted infections among persons with monkeypox-Eight U.S. Jurisdictions, May 17-July 22, 2022. MMWR Morb. Mortal. Wkly Rep. 71, 1141–1147 (2022).
Mitjà, O. et al. Mpox in people with advanced HIV infection: a global case series. Lancet 401, 939–949 (2023).
Miller, M. J. et al. Severe Monkeypox in hospitalized patients-United States, August 10-October 10, 2022. MMWR Morb. Mortal. Wkly Rep. 71, 1412–1417 (2022).
World Health Organization. Multi-Country Outbreak of Mpox, External Situation Report #19–30 March 2023, <https://www.who.int/publications/m/item/multi-country-outbreak-of-mpox--external-situation-report--19---30-march-2023> (World Health Organization, 2023).
O’Sullivan, B. et al. Global vaccine equity? Reflections, lessons, and a way forward. N. Microbes N. Infect. 52, 101107 (2023).
Farlow, A. et al. The future of epidemic and pandemic vaccines to serve global public health needs. Vaccines (Basel) 11, 690 (2023).
Jacob, S. T. et al. Ebola virus disease. Nat. Rev. Dis. Prim. 6, 13 (2020).
Breman, J. G. et al. Discovery and description of Ebola Zaire Virus in 1976 and relevance to the West African Epidemic During 2013-2016. J. Infect. Dis. 214, S93–s101 (2016).
Report of a, W. H. O. I. S. T. Ebola haemorrhagic fever in Sudan, 1976. report of a WHO/International Study Team. Bull. World Health Organ. 56, 247–270 (1978).
Report of an International, C. Ebola haemorrhagic fever in Zaire, 1976. Bull. World Health Organ. 56, 271–293 (1978).
Pattyn, S., van der Groen, G., Jacob, W., Piot, P. & Courteille, G. Isolation of Marburg-like virus from a case of haemorrhagic fever in Zaire. Lancet 1, 573–574 (1977).
Johnson, K. M., Lange, J. V., Webb, P. A. & Murphy, F. A. Isolation and partial characterisation of a new virus causing acute haemorrhagic fever in Zaire. Lancet 1, 569–571 (1977).
Dixon, M. G. & Schafer, I. J. Ebola viral disease outbreak-West Africa, 2014. MMWR Morb. Mortal. Wkly Rep. 63, 548–551 (2014).
World Health Organization. Statement on the 1st Meeting of the Ihr Emergency Committee on the 2014 Ebola Outbreak in West Africa, <https://www.who.int/news/item/08-08-2014-statement-on-the-1st-meeting-of-the-ihr-emergency-committee-on-the-2014-ebola-outbreak-in-west-africa> (World Health Organization, 2014).
Bell, B. P. et al. Overview, control strategies, and lessons learned in the Cdc response to the 2014-2016 Ebola epidemic. MMWR Suppl. 65, 4–11 (2016).
World Health Organization. Ebola Outbreak 2014-2016—West Africa, <https://www.who.int/emergencies/situations/ebola-outbreak-2014-2016-West-Africa> (World Health Organization, 2016).
Forna, A., Nouvellet, P., Dorigatti, I. & Donnelly, C. A. Case fatality ratio estimates for the 2013–2016 West African Ebola epidemic: application of boosted regression trees for imputation. Clin. Infect. Dis. 70, 2476–2483 (2019).
Team, W. H. O. E. R. et al. Ebola virus disease among children in West Africa. N. Engl. J. Med. 372, 1274–1277 (2015).
Chérif, M. S. et al. Ebola virus disease in children during the 2014-2015 epidemic in Guinea: a Nationwide Cohort Study. Eur. J. Pediatr. 176, 791–796 (2017).
Nakkazi, E. Increasing Marburg Vhf outbreaks in Africa. Lancet Infect. Dis. 23, e284–e285 (2023).
Moss, W. J. Measles. Lancet 390, 2490–2502 (2017).
Minta, A. A. et al. Progress toward regional measles elimination-worldwide, 2000-2021. MMWR Morb. Mortal. Wkly Rep. 71, 1489–1495 (2022).
Patel, M. K. et al. Progress toward regional measles elimination-worldwide, 2000-2019. MMWR Morb. Mortal. Wkly Rep. 69, 1700–1705 (2020).
European Centre for Disease Prevention and Control. Systematic Scoping Review on Social Media Monitoring Methods and Interventions Relating to Vaccine Hesitancy. (ECDC, Stockholm, 2020).
Gubler, D. J. Dengue and dengue hemorrhagic fever. Clin. Microbiol. Rev. 11, 480–496 (1998).
Simmons, C. P., Farrar, J. J., Nguyen, V. V. & Wills, B. Dengue. N. Engl. J. Med. 366, 1423–1432 (2012).
Paz-Bailey, G. et al. Dengue vaccine: recommendations of the Advisory Committee on Immunization Practices, United States, 2021. MMWR Recomm. Rep. 70, 1–16 (2021).
World Health Organization. Dengue and Severe Dengue, <https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue> (World Health Organization, 2023).
CDC. About Dengue: What You Need to Know, <https://www.cdc.gov/dengue/about/index.html> (CDC, 2023).
Du, M., Jing, W., Liu, M. & Liu, J. The global trends and regional differences in incidence of dengue infection from 1990 to 2019: an analysis from the Global Burden of Disease Study 2019. Infect. Dis. Ther. 10, 1625–1643 (2021).
Verhagen, L. M. & de Groot, R. Dengue in children. J. Infect. 69, S77–S86 (2014).
Bentes, A. A. et al. Neurological manifestations due to dengue virus infection in children: clinical follow-up. Pathog. Glob. Health 115, 476–482 (2021).
Basurko, C., Carles, G., Youssef, M. & Guindi, W. E. Maternal and fetal consequences of dengue fever during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 147, 29–32 (2009).
World Health Organization. Dengvaxia: Product Overview, <https://extranet.who.int/pqweb/content/dengvaxia> (World Health Organization, 2022).
U.S. Food and Drug Administration. Dengvaxia, <https://www.fda.gov/vaccines-blood-biologics/dengvaxia#:~:text=For%20the%20prevention%20of%20dengue,and%20living%20in%20endemic%20areas.> (U.S. Food and Drug Administration, 2023).
Sridhar, S. et al. Effect of dengue serostatus on dengue vaccine safety and efficacy. N. Engl. J. Med. 379, 327–340 (2018).
Wilder-Smith, A. Dengue vaccine development by the year 2020: Challenges and Prospects. Curr. Opin. Virol. 43, 71–78 (2020).
Vu, D. M., Jungkind, D. & Angelle Desiree, L. Chikungunya virus. Clin. Lab. Med. 37, 371–382 (2017).
Silva, J. V. J. Jr. et al. A scoping review of chikungunya virus infection: epidemiology, clinical characteristics, viral co-circulation complications, and control. Acta Trop. 188, 213–224 (2018).
Puntasecca, C. J., King, C. H. & LaBeaud, A. D. Measuring the global burden of Chikungunya and Zika viruses: a systematic review. PLOS Negl. Trop. Dis. 15, e0009055 (2021).
Robinson, M. C. An epidemic of virus disease in Southern Province, Tanganyika Territory, in 1952-53. I. Clinical features. Trans. R. Soc. Trop. Med. Hyg. 49, 28–32 (1955).
Thiberville, S. D. et al. Chikungunya fever: epidemiology, clinical syndrome, pathogenesis and therapy. Antivir. Res. 99, 345–370 (2013).
Gérardin, P. et al. Multidisciplinary prospective study of mother-to-child chikungunya virus infections on the Island of La Réunion. PLoS Med. 5, e60 (2008).
van Keulen, V., Huibers, M., Manshande, M., van Hensbroek, M. B. & van Rooij, L. Chikungunya virus infections among infants-WHO classification not applicable. Pediatr. Infect. Dis. J. 37, e83–e86 (2018).
Nyamwaya, D. K., Thumbi, S. M., Bejon, P., Warimwe, G. M. & Mokaya, J. The global burden of chikungunya fever among children: a systematic literature review and meta-analysis. PLOS Glob. Public Health 2, e0000914 (2022).
Bartholomeeusen, K. et al. Chikungunya fever. Nat. Rev. Dis. Prim. 9, 17 (2023).
DeFilippis, V. R. Chikungunya virus vaccines: platforms, progress, and challenges. Curr. Top. Microbiol. Immunol. 435, 81–106 (2022).
CDC. Technical Report: Highly Pathogenic Avian Influenza a(H5n1) Viruses, <https://www.cdc.gov/flu/avianflu/spotlights/2022-2023/h5n1-technical-report.htm> (CDC, 2023).
CDC. H5n1 Bird Flu: Current Situation Summary, <https://www.cdc.gov/flu/avianflu/avian-flu-summary.htm> (CDC, 2023).
Mordecai, E. A., Ryan, S. J., Caldwell, J. M., Shah, M. M. & LaBeaud, A. D. Climate change could shift disease burden from Malaria to Arboviruses in Africa. Lancet Planet Health 4, e416–e423 (2020).
Funding
S.A.H. is supported in part by the National Institutes of Health under the National Institute of Allergy and Infectious Diseases grant T32AI007502, as well as by the Stanford Maternal and Child Health Research Institute.
Author information
Authors and Affiliations
Contributions
S.A.H. and Y.A.M. equally contributed to the conception and design, drafting and revising, and final approval of the version submitted.
Corresponding author
Ethics declarations
Competing interests
Y.A.M. reports no competing interests. Y.A.H. reports funding from Pfizer grants as PI for COVID-19 vaccine trials and for maternal RSV vaccine trials, hourly payment as a member of a Pfizer Data Safety Monitoring Board, and honorarium from NIH/NIAID/ACTIV as a member of a Data Safety Monitoring Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoffman, S.A., Maldonado, Y.A. Emerging and re-emerging pediatric viral diseases: a continuing global challenge. Pediatr Res 95, 480–487 (2024). https://doi.org/10.1038/s41390-023-02878-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02878-7
This article is cited by
-
Preparing for the next emerging perinatal infectious disease
Pediatric Research (2024)
-
Trends in prenatal and pediatric viral infections, and the impact of climate change
Pediatric Research (2024)