Abstract
Background
The aim of the study was to examine preceding risks and mortality outcomes of oliguric and non-oliguric acute kidney injury (AKI) in very preterm infants.
Methods
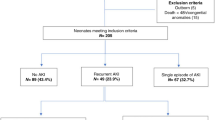
Infants born ≤30 weeks’ gestation were included. AKI was diagnosed based on neonatal Kidney Disease: Improving Global Outcomes criteria and was classified as oliguric and non-oliguric according to the urine-output criteria. We used modified Poisson and Cox proportional-hazards models for statistical comparisons.
Results
Of 865 enrolled infants (gestational age 27.2 ± 2.2 weeks and birth weight 983 ± 288 gm), 204 (23.6%) developed AKI. Before AKI, the oliguric AKI group had significantly higher prevalence of small-for-gestational age (p = 0.008), lower 5-min Apgar score (p = 0.009) and acidosis (p = 0.009) on admission, and hypotension (p = 0.008) and sepsis (p = 0.001) during admission than the non-oliguric AKI group. Oliguric (adjusted risk ratio 3.58, 95% CI 2.33–5.51; adjusted hazard ratio 4.93, 95% CI 3.14–7.72) instead of non-oliguric AKI had significantly higher mortality risks than no AKI. Oliguric AKI showed significantly higher mortality risks than non-oliguric AKI, irrespective of serum creatinine and severity of AKI.
Conclusions
Categorizing AKI as oliguric and non-oliguric was crucial because of the distinct preceding risks and mortality outcomes of these two types of AKI in very preterm neonates.
Impact
-
The differences of the underlying risks and prognosis between oliguric and non-oliguric AKI in very preterm infants remain unclear.
-
We found that oliguric AKI, but not non-oliguric AKI, carries higher mortality risks than infants without AKI. Oliguric AKI possessed higher mortality risks than non-oliguric AKI, irrespective of concomitant serum creatinine elevation and severe AKI.
-
Oliguric AKI is more associated with prenatal small-for-the-gestational age and perinatal and postnatal adverse events, while non-oliguric AKI is associated with nephrotoxins exposures.
-
Our finding highlighted the importance of oliguric AKI and is helpful in developing future protocol in neonatal critical care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The corresponding author had full access to the dataset used and analyzed during the current study. The datasets used during the current study are available from the corresponding author on reasonable request.
References
Carmody, J. B., Swanson, J. R., Rhone, E. T. & Charlton, J. R. Recognition and reporting of AKI in very low birth weight infants. Clin. J. Am. Soc. Nephrol. 9, 2036–2043 (2014).
Rodríguez, M. M. et al. Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr. Dev. Pathol. 7, 17–25 (2004).
Luyckx, V. A. Preterm birth and its impact on renal health. Semin. Nephrol. 37, 311–319 (2017).
Menendez-Castro, C. et al. Neonatal nephron loss during active nephrogenesis - detrimental impact with long-term renal consequences. Sci. Rep. 8, 4542 (2018).
Sutherland, M. R. et al. Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J. Am. Soc. Nephrol. 22, 1365–1374 (2011).
Kent, A. L. et al. Indomethacin, ibuprofen and gentamicin administered during late stages of glomerulogenesis do not reduce glomerular number at 14 days of age in the neonatal rat. Pediatr. Nephrol. 24, 1143–1149 (2009).
Charlton, J. R. et al. Incidence and risk factors of early onset neonatal AKI. Clin. J. Am. Soc. Nephrol. 14, 184–195 (2019).
Chen, C. C., Lin, Y. C., Wang, S. T. & Huang, C. C. Temporal trends of acute kidney injury and associated risk exposures in extremely preterm infants. Clin. J. Am. Soc. Nephrol. 16, 1169–1177 (2021).
Zappitelli, M. et al. Developing a neonatal acute kidney injury research definition: a report from the NIDDK Neonatal AKI Workshop. Pediatr. Res. 82, 569–573 (2017).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (Awaken): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–194 (2017).
Charlton, J. R. et al. Late onset neonatal acute kidney injury: results from the Awaken Study. Pediatr. Res. 85, 339–348 (2019).
Bezerra, C. T., Vaz Cunha, L. C. & Libório, A. B. Defining reduced urine output in neonatal icu: importance for mortality and acute kidney injury classification. Nephrol. Dial. Transplant. 28, 901–909 (2013).
Elmas, A. T., Tabel, Y. & Özdemir, R. Risk factors and mortality rate in premature babies with acute kidney injury. J. Clin. Lab. Anal. 32, e22441 (2018).
Gupta, B. D., Sharma, P., Bagla, J., Parakh, M. & Soni, J. P. Renal failure in asphyxiated neonates. Indian Pediatr. 42, 928–934 (2005).
Viswanathan, S., Manyam, B., Azhibekov, T. & Mhanna, M. J. Risk factors associated with acute kidney injury in extremely low birth weight (ELBW) infants. Pediatr. Nephrol. 27, 303–311 (2012).
Wu, M. H. et al. Prevalence of congenital heart disease at live birth in Taiwan. J. Pediatr. 156, 782–785 (2010).
Selewski, D. T. et al. Neonatal acute kidney injury. Pediatrics 136, e463–e473 (2015).
Kaddourah, A., Basu, R. K., Bagshaw, S. M. & Goldstein, S. L. Epidemiology of acute kidney injury in critically ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Jadhav, P., Parimi, P. S. & Kalhan, S. C. Parenteral amino acid and metabolic acidosis in premature infants. JPEN J. Parenter. Enter. Nutr. 31, 278–283 (2007).
Stoops, C. et al. Baby Ninja (nephrotoxic injury negated by just-in-time action): reduction of nephrotoxic medication-associated acute kidney injury in the neonatal intensive care unit. J. Pediatr. 215, 223.e6–228.e6 (2019).
Azur, M. J., Stuart, E. A., Frangakis, C. & Leaf, P. J. Multiple imputation by chained equations: what is it and how does it work? Int. J. Methods Psychiatr. Res. 20, 40–49 (2011).
Blazek, K., van Zwieten, A., Saglimbene, V. & Teixeira-Pinto, A. A practical guide to multiple imputation of missing data in nephrology. Kidney Int. 99, 68–74 (2021).
Chen, W., Qian, L., Shi, J. & Franklin, M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med. Res. Methodol. 18, 63 (2018).
Gubhaju, L. et al. Assessment of renal functional maturation and injury in preterm neonates during the first month of life. Am. J. Physiol. Ren. Physiol. 307, F149–F158 (2014).
Liangos, O. Nonoliguric Versus Oliguric Acute Kidney Injury Post TW edn (UpToDate Inc., 2022).
Honda, N. & Hishida, A. Pathophysiology of experimental nonoliguric acute renal failure. Kidney Int. 43, 513–521 (1993).
Carmody, J. B. & Charlton, J. R. Short-term gestation, long-term risk: prematurity and chronic kidney disease. Pediatrics 131, 1168–1179 (2013).
Behrendt, N. & Galan, H. L. Fetal growth in multiple gestations: evaluation and management. Obstet. Gynecol. Clin. North Am. 48, 401–417 (2021).
Perico, N., Askenazi, D., Cortinovis, M. & Remuzzi, G. Maternal and environmental risk factors for neonatal AKI and its long-term consequences. Nat. Rev. Nephrol. 14, 688–703 (2018).
Gallo, D., de Bijl-Marcus, K. A., Alderliesten, T., Lilien, M. & Groenendaal, F. Early acute kidney injury in preterm and term neonates: incidence, outcome, and associated clinical features. Neonatology 118, 174–179 (2021).
Starr, M. C. et al. Advances in neonatal acute kidney injury. Pediatrics 148, e2021051220 (2021).
Schetz, M. & Hoste, E. Understanding oliguria in the critically ill. Intensive Care Med. 43, 914–916 (2017).
Mathis, M. R. et al. Preoperative risk and the association between hypotension and postoperative acute kidney injury. Anesthesiology 132, 461–475 (2020).
Izawa, J. et al. Early-phase cumulative hypotension duration and severe-stage progression in oliguric acute kidney injury with and without sepsis: an observational study. Crit. Care 20, 405 (2016).
Hentschel, R., Lödige, B. & Bulla, M. Renal insufficiency in the neonatal period. Clin. Nephrol. 46, 54–58 (1996).
Honore, P. M. et al. Prevention and treatment of sepsis-induced acute kidney injury: an update. Ann. Intensive Care 5, 51 (2015).
Rhone, E. T., Carmody, J. B., Swanson, J. R. & Charlton, J. R. Nephrotoxic medication exposure in very low birth weight infants. J. Matern. Fetal Neonatal Med. 27, 1485–1490 (2014).
Wu, I. M., Marin, E. P., Kashgarian, M. & Brewster, U. C. A case of an acute kidney injury secondary to an implanted aminoglycoside. Kidney Int. 75, 1109–1112 (2009).
Dixit, M., Doan, T., Kirschner, R. & Dixit, N. Significant acute kidney injury due to non-steroidal anti-inflammatory drugs: inpatient setting. Pharmaceuticals 3, 1279–1285 (2010).
Kwiatkowska, E. et al. The mechanism of drug nephrotoxicity and the methods for preventing kidney damage. Int. J. Mol. Sci. 22, 6109 (2021).
Stoops, C. et al. The association of intraventricular hemorrhage and acute kidney injury in premature infants from the Assessment of the Worldwide Acute Kidney Injury Epidemiology in Neonates (Awaken) study. Neonatology 116, 321–330 (2019).
Aziz, K. B., Schles, E. M., Makker, K. & Wynn, J. L. Frequency of acute kidney injury and association with mortality among extremely preterm infants. JAMA Netw. Open 5, e2246327 (2022).
Kaddourah, A., Basu, R. K., Goldstein, S. L. & Sutherland, S. M. Oliguria and acute kidney injury in critically ill children: implications for diagnosis and outcomes. Pediatr. Crit. Care Med. 20, 332–339 (2019).
Alten, J. A. et al. Epidemiology of acute kidney injury after neonatal cardiac surgery: a report from the Multicenter Neonatal and Pediatric Heart and Renal Outcomes Network. Crit. Care Med. 49, e941–e951 (2021).
Doi, K. et al. The Japanese Clinical Practice Guideline for Acute Kidney Injury 2016. J. Intensive Care 6, 48 (2018).
Allegaert, K., Smits, A., Mekahli, D. & van den Anker, J. N. Creatinine at birth correlates with gestational age and birth weight: another factor of the imbroglio in early neonatal life. Neonatology 117, 637–640 (2020).
Gidi, N. W. et al. Incidence and associated factors of extrauterine growth restriction (EUGR) in preterm infants, a cross-sectional study in selected nicus in Ethiopia. BMJ Paediatr. Open 4, e000765 (2020).
Vaara, S. T. et al. Association of oliguria with the development of acute kidney injury in the critically ill. Kidney Int. 89, 200–208 (2015).
Mohsenin, V. Practical approach to detection and management of acute kidney injury in critically ill patient. J. Intensive Care 5, 57 (2017).
Acknowledgements
The authors thank the Taiwan Premature Baby Foundation and all team members in charge of data collection. None of these individuals were compensated for their contributions.
Funding
This study was supported by the grants from Taiwan Ministry of Science and Technology (MOST 110-2314-B-006-057, MOST-110-2314-B-006-113, MOST-109-2314-B-006-008) and from National Cheng Kung University Hospital (NCKUH-11001002, NCKUH-11101001).
Author information
Authors and Affiliations
Contributions
C.-C.C. and C.-C.H. contributed to research idea and study design; Y.-C.L. contributed to data acquisition; C.-C.C., C.-H.C., Y.-C.L., S.-T.W., and C.-C.H. contributed to data analysis/interpretation; C.-C.C., C.-H.C., and S.-T.W. provided statistical analysis; S.T.W. and C.C.H. provided supervision or mentorship. All authors contributed important intellectual content during manuscript drafting or revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the ethics review board of National Cheng-Kung University Hospital (A-BR-108-013, and ER-98-135). The informed consent of participants born after August 13, 2009 was obtained and that of infants born previously were waived.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, CC., Chu, CH., Lin, YC. et al. Preceding risks and mortality outcomes of different neonatal acute kidney injury in preterm infants. Pediatr Res 94, 1530–1537 (2023). https://doi.org/10.1038/s41390-023-02650-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02650-x