Abstract
Purpose
Childhood cancer survivors are at increased risk for cardiovascular disease. Maximal oxygen uptake (VO2max) is a major determinant of cardiovascular morbidity. The aim of this study was to compare aerobic capacity, measured by cardiopulmonary exercise test (CPET), of adolescents and young adults in remission with that of healthy controls and to identify the predictors of aerobic capacity in this population.
Method
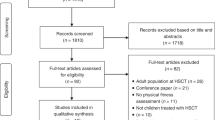
This is a controlled cross-sectional study.
Results
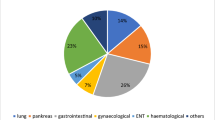
A total of 477 subjects (77 in remission and 400 controls), aged from 6 to 25 years, were included, with a mean delay between end of treatment and CPET of 2.9 ± 2.3 years in the remission group. In this group, the mean VO2max was significantly lower than in controls (37.3 ± 7.6 vs. 43.3 ± 13.1 mL/kg/min, P < 0.01, respectively), without any clinical or echocardiographic evidence of heart failure. The VAT was significantly lower in the remission group (26.9 ± 6.0 mL/kg/min vs. 31.0 ± 9.9 mL/kg/min, P < 0.01, respectively). A lower VO2max was associated with female sex, older age, higher BMI, radiotherapy, and hematopoietic stem cell transplantation.
Conclusion
Impaired aerobic capacity had a higher prevalence in adolescents and young adults in cancer remission. This impairment was primarily related to physical deconditioning and not to heart failure.
Trial registry
NCT04815447.
Impact
-
In childhood cancer survivors, aerobic capacity is five times more impaired than in healthy subjects.
-
This impairment mostly reflects early onset of physical deconditioning.
-
No evidence of heart failure was observed in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Chow, E. J. et al. Current and coming challenges in the management of the survivorship population. Semin. Oncol. 47, 23–39 (2020).
Siviero-Miachon, A. A., Spinola-Castro, A. M. & Guerra-Junior, G. Adiposity in childhood cancer survivors: insights into obesity physiopathology. Arq. Bras. Endocrinol. Metab. 53, 190–200 (2009).
Meacham, L. R. et al. Diabetes mellitus in long-term survivors of childhood cancer. Increased risk associated with radiation therapy: a report for the childhood cancer survivor study. Arch. Intern. Med. 169, 1381–1388 (2009).
Mulrooney, D. A. et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 339, b4606 (2009).
Tukenova, M. et al. Role of cancer treatment in long-term overall and cardiovascular mortality after childhood cancer. J. Clin. Oncol. 28, 1308–1315 (2010).
Meacham, L. R. et al. Cardiovascular risk factors in adult survivors of pediatric cancer-a report from the childhood cancer survivor study. Cancer Epidemiol. Biomarkers Prev. 19, 170–181 (2010).
Kucharska, W., Negrusz-Kawecka, M. & Gromkowska, M. Cardiotoxicity of oncological treatment in children. Adv. Clin. Exp. Med. 21, 281–288 (2012).
Brouwer, C. A. J. et al. Endothelial damage in long-term survivors of childhood cancer. J. Clin. Oncol. 31, 3906–3913 (2013).
Pein, F. et al. Cardiac abnormalities 15 years and more after adriamycin therapy in 229 childhood survivors of a solid tumour at the Institut Gustave Roussy. Br. J. Cancer 91, 37–44 (2004).
de Ferranti, S. D. et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association. Circulation 139, e603–e634 (2019).
Mertens, A. C. et al. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J. Natl Cancer Inst. 100, 1368–1379 (2008).
Lemay, V. et al. Prevention of long-term adverse health outcomes with cardiorespiratory fitness and physical activity in childhood acute lymphoblastic leukemia survivors. J. Pediatr. Hematol. Oncol. 41, e450–e458 (2019).
Schmid, D. & Leitzmann, M. F. Cardiorespiratory fitness as predictor of cancer mortality: a systematic review and meta-analysis. Ann. Oncol. 26, 272–278 (2015).
Kodama, S. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301, 2024 (2009).
Amedro, P. et al. Correlation between cardio-pulmonary exercise test variables and health-related quality of life among children with congenital heart diseases. Int J. Cardiol. 203, 1052–1060 (2016).
Amedro, P. et al. Cardiopulmonary fitness in children with congenital heart diseases versus healthy children. Heart 104, 1026–1036 (2018).
Klijn, P. H. C., van der Net, J., Kimpen, J. L., Helders, P. J. M. & van der Ent, C. K. Longitudinal determinants of peak aerobic performance in children with cystic fibrosis. Chest 124, 2215–2219 (2003).
Goldstein, S. L. Physical fitness in children with end-stage renal disease. Adv. Chronic Kidney Dis. 16, 430–436 (2009).
Kim, S., Song, I.-C. & Jee, S. Cardiopulmonary exercise test in leukemia patients after chemotherapy: a feasibility study. Ann. Rehabil. Med. 41, 456–464 (2017).
Kelsey, C. R. et al. Cardiopulmonary exercise testing prior to myeloablative allo-SCT: a feasibility study. Bone Marrow Transplant. 49, 1330–1336 (2014).
van Brussel, M., Takken, T., Lucia, A., van der Net, J. & Helders, P. J. M. Is physical fitness decreased in survivors of childhood leukemia? A systematic review. Leukemia 19, 13–17 (2005).
Yildiz Kabak, V., Calders, P., Duger, T., Mohammed, J. & van Breda, E. Short and long-term impairments of cardiopulmonary fitness level in previous childhood cancer cases: a systematic review. Support Care Cancer 27, 69–86 (2019).
Gavotto, A. et al. Oxygen uptake efficiency slope: a reliable surrogate parameter for exercise capacity in healthy and cardiac children? Arch. Dis. Child 105, 1167–1174 (2020).
Gavotto, A. et al. The V̇e/V̇co2 slope: a useful tool to evaluate the physiological status of children with congenital heart disease. J. Appl. Physiol. 129, 1102–1110 (2020).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343 (2012).
Cooper, D. M., Weiler-Ravell, D., Whipp, B. J. & Wasserman, K. Aerobic parameters of exercise as a function of body size during growth in children. J. Appl. Physiol. 56, 628–634 (1984).
Rowland, T. W. & Cunningham, L. N. Oxygen uptake plateau during maximal treadmill exercise in children. Chest 101, 485–489 (1992).
Barker, A. R., Williams, C. A., Jones, A. M. & Armstrong, N. Establishing maximal oxygen uptake in young people during a ramp cycle test to exhaustion. Br. J. Sports Med. 45, 498–503 (2011).
Blais, S., Berbari, J., Counil, F.-P. & Dallaire, F. A systematic review of reference values in pediatric cardiopulmonary exercise testing. Pediatr. Cardiol. 36, 1553–1564 (2015).
Beaver, W. L., Wasserman, K. & Whipp, B. J. A new method for detecting anaerobic threshold by gas exchange. J. Appl Physiol. 60, 2020–2027 (1986).
Stephens, P. & Paridon, S. M. Exercise testing in pediatrics. Pediatr. Clin. North Am. 51, 1569–1587 (2004).
Paolillo, S. et al. Heart failure prognosis over time: how the prognostic role of oxygen consumption and ventilatory efficiency during exercise has changed in the last 20 years. Eur. J. Heart Fail. 21, 208–217 (2019).
Atkinson, M. et al. A randomized controlled trial of a structured exercise intervention after the completion of acute cancer treatment in adolescents and young adults. Pediatr. Blood Cancer 68, e28751 (2021).
Braam, K. I. et al. Cardiorespiratory fitness and physical activity in children with cancer. Support Care Cancer 24, 2259–2268 (2016).
Morales, J. S. et al. Exercise interventions and cardiovascular health in childhood cancer: a meta-analysis. Int J. Sports Med. 41, 141–153 (2020).
Söntgerath, R. et al. Physical and functional performance assessment in pediatric oncology: a systematic review. Pediatr. Res. 91, 743–756 (2022).
Moreau, J. et al. Cardiopulmonary fitness in children with asthma versus healthy children. Arch. Dis. Child. 2022;archdischild-2021-323733. https://doi.org/10.1136/archdischild-2021-323733.
Sato, T. et al. Cardiorespiratory exercise capacity and its relation to a new Doppler index in children previously treated with anthracycline. J. Am. Soc. Echocardiogr. 14, 256–263 (2001).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 4, 23–35 (2020).
Fuemmeler, B. F. et al. Diet, physical activity, and body composition changes during the first year of treatment for childhood acute leukemia and lymphoma. J. Pediatr. Hematol. Oncol. 35, 437–443 (2013).
Hoffman, M. C. et al. Deficits in physical function among young childhood cancer survivors. J. Clin. Oncol. 31, 2799–2805 (2013).
Schneider, J., Schlüter, K., Sprave, T., Wiskemann, J. & Rosenberger, F. Exercise intensity prescription in cancer survivors: ventilatory and lactate thresholds are useful submaximal alternatives to VO2peak. Support Care Cancer 28, 5521–5528 (2020).
Amedro, P. et al. Impact of a centre and home-based cardiac rehabilitation program on the quality of life of teenagers and young adults with congenital heart disease: the QUALI-REHAB study rationale, design and methods. Int. J. Cardiol. 283, 112–118 (2019).
Schindera, C. et al. Physical fitness and modifiable cardiovascular disease risk factors in survivors of childhood cancer: a report from the SURfit study. Cancer 127, 1690–1698 (2021).
Amedro, P. et al. Use of speckle tracking echocardiography to detect late anthracycline-induced cardiotoxicity in childhood cancer: a prospective controlled cross-sectional study. Int J. Cardiol. 354, 75–83 (2022).
Chakouri, N. et al. Screening for in-vivo regional contractile defaults to predict the delayed doxorubicin cardiotoxicity in juvenile rat. Theranostics 10, 8130–8142 (2020).
Author information
Authors and Affiliations
Contributions
Study conception and design: A.G. and P.A. Acquisition of data: A.G. and V.D. Analysis and interpretation of data: A.G., V.D., H.H., M.-C.P., S.G., S.H., N.S., A.S., S.M. and P.A. Drafting the article: A.G., V.D., M.A. and P.A. Critical revising of the article for important intellectual content: all authors. Final approval of the version to be published: all authors. Study supervision: P.A.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gavotto, A., Dubard, V., Avesani, M. et al. Impaired aerobic capacity in adolescents and young adults after treatment for cancer or non-malignant haematological disease. Pediatr Res 94, 626–631 (2023). https://doi.org/10.1038/s41390-023-02477-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02477-6
This article is cited by
-
Aerobic physical capacity and health-related quality of life in children with sickle cell disease
Pediatric Research (2024)
-
Reference Values of Cardiopulmonary Exercise Test Parameters in the Contemporary Paediatric Population
Sports Medicine - Open (2023)
-
The importance of cardiopulmonary exercise test to improve supportive care in adolescent and young adult survivors of childhood cancer
Pediatric Research (2023)