Abstract
Background
Aerobic fitness is a predictor of cardiovascular health which correlates with health-related quality of life in the general population. The aim is to evaluate the aerobic capacity by cardiopulmonary exercise test (CPET) in children with sickle cell disease in comparison with healthy matched controls.
Methods
Controlled cross-sectional study.
Results
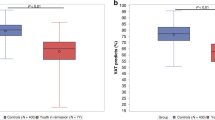
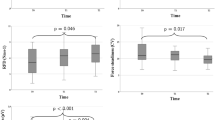
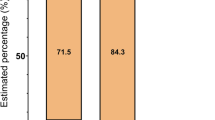
A total of 72 children (24 with sickle cell disease and 48 healthy controls), aged 6–17 years old were enrolled. Children with sickle cell disease had a poor aerobic capacity, with median VO2max Z-score values significantly lower than matched controls (−3.55[−4.68; −2.02] vs. 0.25[−0.22; 0.66], P < 0.01, respectively), and a high proportion of 92% children affected by an impaired aerobic capacity (VO2max Z-score < −1.64). The VO2max decrease was associated with the level of anemia, the existence of a homozygote HbS/S mutation, restrictive lung disease and health-related quality of life.
Conclusion
Aerobic capacity is poor in children with sickle cell disease. VO2max decrease is associated with the level of anemia, the existence of a homozygote HbS/S mutation, lung function, and health-related quality of life. These results represent a signal in favor of early initiation of cardiac rehabilitation in patients with sickle cell disease.
Clinical trials
NCT05995743.
Impact
-
Aerobic fitness is a predictor of cardiovascular health which correlates with health-related quality of life in the general population.
-
Aerobic capacity (VO2max) is poor in children with sickle cell disease, despite the absence of any pattern of heart failure.
-
VO2max decrease was associated with the level of anemia, the existence of a homozygote HbS/S mutation, restrictive lung disease, and health-related quality of life.
-
These results are in favor of early initiation of cardiac rehabilitation in children with sickle cell disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Piccin, A. et al. Insight into the complex pathophysiology of sickle cell anaemia and possible treatment. Eur. J. Haematol. 102, 319–330 (2019).
Piel, F. B., Steinberg, M. H. & Rees, D. C. Sickle cell disease. N. Engl. J. Med. 376, 1561–1573 (2017).
Piel, F. B., Hay, S. I., Gupta, S., Weatherall, D. J. & Williams, T. N. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. 10, e1001484 (2013).
Ferraresi, M. et al. Therapeutic perspective for children and young adults living with thalassemia and sickle cell disease. Eur. J. Pediatr. 182, 2509–2519 (2023).
Rees, D. C., Williams, T. N. & Gladwin, M. T. Sickle-cell disease. Lancet 376, 2018–2031 (2010).
Gardner, K. et al. Survival in adults with sickle cell disease in a high-income setting. Blood 128, 1436–1438 (2016).
Lê, P. Q. et al. Survival among children and adults with sickle cell disease in Belgium: benefit from hydroxyurea treatment. Pediatr. Blood Cancer 62, 1956–1961 (2015).
Connes, P., Machado, R., Hue, O. & Reid, H. Exercise limitation, exercise testing and exercise recommendations in sickle cell anemia. Clin. Hemorheol. Microcirc. 49, 151–163 (2011).
Panepinto, J. A., O’Mahar, K. M., DeBaun, M. R., Loberiza, F. R. & Scott, J. P. Health-related quality of life in children with sickle cell disease: child and parent perception. Br. J. Haematol. 130, 437–444 (2005).
Liem, R. I. et al. Reduced fitness and abnormal cardiopulmonary responses to maximal exercise testing in children and young adults with sickle cell anemia. Physiol. Rep. 3, e12338 (2015).
Callahan, L. A. et al. Cardiopulmonary responses to exercise in women with sickle cell anemia. Am. J. Respir. Crit. Care Med. 165, 1309–1316 (2002).
Woodson, R. D., Wills, R. E. & Lenfant, C. Effect of acute and established anaemia on O2 transport at rest, submaximal and maximal work. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 44, 36–43 (1978).
Woodson, R. D. Hemoglobin concentration and exercise capacity. Am. Rev. Respir. Dis. 129, S72–S75 (1984).
Pianosi, P., D’Souza, S. J., Esseltine, D. W., Charge, T. D. & Coates, A. L. Ventilation and gas exchange during exercise in sickle cell anemia. Am. Rev. Respir. Dis. 143, 226–230 (1991).
Klings, E. S., Wyszynski, D. F., Nolan, V. G. & Steinberg, M. H. Abnormal pulmonary function in adults with sickle cell anemia. Am. J. Respir. Crit. Care Med. 173, 1264–1269 (2006).
Willen, S. M. et al. Age is a predictor of a small decrease in lung function in children with sickle cell anemia. Am. J. Hematol. 93, 408–415 (2018).
Dhar, A. et al. Longitudinal analysis of cardiac abnormalities in pediatric patients with sickle cell anemia and effect of hydroxyurea therapy. Blood Adv. 5, 4406–4412 (2021).
Olorunyomi, O. O., Liem, R. I. & Hsu, L. L. Motivators and barriers to physical activity among youth with sickle cell disease: brief review. Children 9, 572 (2022).
Parent, F. et al. A hemodynamic study of pulmonary hypertension in sickle cell disease. N. Engl. J. Med. 365, 44–53 (2011).
Bode-Thomas, F., Hyacinth, H. I., Ogunkunle, O. & Omotoso, A. Myocardial ischaemia in sickle cell anaemia: evaluation using a new scoring system. Ann. Trop. Paediatr. 31, 67–74 (2011).
Montalembert et al. Myocardial ischaemia in children with sickle cell disease. Arch. Dis. Child. 89, 359–362 (2004).
Amedro, P. et al. Cardiopulmonary fitness in children with congenital heart diseases versus healthy children. Heart 104, 1026–1036 (2018).
Moreau, J. et al. Cardiopulmonary fitness in children with asthma versus healthy children. Arch. Dis. Child 108, 204–210 (2023).
Gavotto, A. et al. Impaired aerobic capacity in adolescents and young adults after treatment for cancer or non-malignant haematological disease. Pediatr. Res. 94, 626–31 (2023).
American Thoracic Society, American College of Chest Physicians. ATS/ACCP statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med. 167, 211–277 (2003).
Abassi, H. et al. Impaired pulmonary function and its association with clinical outcomes, exercise capacity and quality of life in children with congenital heart disease. Int. J. Cardiol. 285, 86–92 (2019).
Amedro, P. et al. Correlation between cardio-pulmonary exercise test variables and health-related quality of life among children with congenital heart diseases. Int. J. Cardiol. 203, 1052–1060 (2016).
Abassi, H. et al. Health-related quality of life in children with congenital heart disease aged 5 to 7 years: a multicentre controlled cross-sectional study. Health Qual. Life Outcomes 18, 366 (2020).
Amedro, P. et al. Health-related quality of life of patients with pulmonary arterial hypertension associated with CHD: the multicentre cross-sectional ACHILLE study. Cardiol. Young. 26, 1250–1259 (2016).
Das, B. B., Sobczyk, W., Bertolone, S. & Raj, A. Cardiopulmonary stress testing in children with sickle cell disease who are on long-term erythrocytapheresis. J. Pediatr. Hematol. Oncol. 30, 373–377 (2008).
Gavotto, A. et al. Reference values of aerobic fitness in the contemporary paediatric population. Eur. J. Prev. Cardiol. 30, 820–829 (2023).
Odièvre, M., Schaison, G., Baruchel, A. & Leblanc, T. Hématologie de l’enfant. Arch. Pédiatr. 2, 1233 (1995).
Kampmann, C. et al. Normal values of M mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart 83, 667–672 (2000).
Bowerman C. et al. A race-neutral approach to the interpretation of lung function measurements. Am. J. Respir. Crit. Care Med. 207, 768–74 (2022).
Hall G. L. et al. Official ERS technical standard: Global Lung Function Initiative reference values for static lung volumes in individuals of European ancestry. Eur. Resp. J. 57, https://erj.ersjournals.com/content/57/3/2000289 (2021). Accessed 15 February 2023.
Takken, T. et al. Cardiopulmonary exercise testing in congenital heart disease: equipment and test protocols. Neth. Heart J. 17, 339–344 (2009).
Barker, A. R., Williams, C. A., Jones, A. M. & Armstrong, N. Establishing maximal oxygen uptake in young people during a ramp cycle test to exhaustion. Br. J. Sports Med. 45, 498–503 (2011).
Amedro, P. et al. Early hybrid cardiac rehabilitation in congenital heart disease: the QUALIREHAB trial. Eur. Heart J. ehae085 https://doi.org/10.1093/eurheartj/ehae085 (2024).
Varni, J. W., Burwinkle, T. M., Seid, M. & Skarr, D. The PedsQLTM* 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul. Pediatr. 3, 329–341 (2003).
Tessier, S., Vuillemin, A., Lemelle, J.-L. & Briançon, S. Propriétés psychométriques du questionnaire générique français «Pediatric Quality of Life Inventory Version 4.0» (PedsQLTM 4.0). Eur. Rev. Appl. Psychol. 59, 291–300 (2009).
Amedro, P. et al. Psychometric validation of the French self and proxy versions of the PedsQLTM 4.0 generic health-related quality of life questionnaire for 8–12 year-old children. Health Qual. Life Outcomes 19, 75 (2021).
Vuillemin, A., Denis, G., Guillemin, F. & Jeandel, C. A review of evaluation questionnaires for physical activity. Rev. Epidemiol. Sante Publ. 46, 49–55 (1998).
Abid, R., Ammar, A., Maaloul, R., Souissi, N. & Hammouda, O. Effect of COVID-19-related home confinement on sleep quality, screen time and physical activity in Tunisian boys and girls: a survey. Int. J. Environ. Res. Public Health 18, 3065 (2021).
Kodama, S. et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301, 2024–2035 (2009).
Pianosi, P. et al. Cardiac output and oxygen delivery during exercise in sickle cell anemia. Am. Rev. Respir. Dis. 143, 231–235 (1991).
Ogunsile, F. J., Stewart, K. J., Kanter, J. & Lanzkron, S. M. An evaluation of cardiopulmonary endurance and muscular strength in adults living with sickle cell disease. Br. J. Haematol. 199, 597–602 (2022).
da Guarda, C. C. et al. Sickle cell disease: a distinction of two most frequent genotypes (HbSS and HbSC). PLoS One 15, e0228399 (2020).
Charache, S., Bleecker, E. R. & Bross, D. S. Effects of blood transfusion on exercise capacity in patients with sickle-cell anemia. Am. J. Med. 74, 757–764 (1983).
Miller, G. J., Serjeant, G. R., Sivapragasam, S. & Petch, M. C. Cardio-pulmonary responses and gas exchange during exercise in adults with homozygous sickle-cell disease (sickle-cell anaemia). Clin. Sci. 44, 113–128 (1973).
Liem, R. I. Balancing exercise risk and benefits: lessons learned from sickle cell trait and sickle cell anemia. Hematol. Am. Soc. Hematol. Educ. Program 2018, 418–425 (2018).
Author information
Authors and Affiliations
Contributions
Laurent-Lacroix and Vincenti contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Laurent-Lacroix, Vincenti, Matecki, Moulis, Amedro, and Gavotto. The first draft of the manuscript was written by Laurent-Lacroix, Vincenti, Amedro, and Gavotto and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was conducted in compliance with the Good Clinical Practices protocol and Declaration of Helsinki principles. It was approved by our institutional review board (IRB-MTP_2022_04_202201102) and registered on Clinicaltrials.gov (NCT05995743). Informed consent was obtained from all parents or legal guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Laurent-Lacroix, C., Vincenti, M., Matecki, S. et al. Aerobic physical capacity and health-related quality of life in children with sickle cell disease. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03143-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03143-1