Abstract
Background
Rapid next-generation sequencing (NGS) offers the potential to shorten the diagnostic process and improve the care of acutely ill children. The goal of this study was to report our findings, including benefits and limitations, of a targeted NGS panel and rapid genome sequencing (rGS) in neonatal and pediatric acute clinical care settings.
Methods
Retrospective analysis of patient characteristics, diagnostic yields, turnaround time, and changes in management for infants and children receiving either RapSeq, a targeted NGS panel for 4500+ genes, or rGS, at the University of Utah Hospital and Primary Children’s Hospital, from 2015 to 2020.
Results
Over a 5-year period, 142 probands underwent rapid NGS: 66 received RapSeq and 76 rGS. Overall diagnostic yield was 39%. In the majority of diagnostic cases, there were one or more changes in clinical care management. Of note, 7% of diagnoses identified by rGS would not have been identified by RapSeq.
Conclusions
Our results indicate that rapid NGS impacts acute pediatric care in real-life clinical settings. Although affected by patient selection criteria, diagnostic yields were similar to those from clinical trial settings. Future studies are needed to determine relative advantages, including cost, turnaround time, and benefits for patients, of each approach in specific clinical circumstances.
Impact
-
The use of comprehensive Mendelian gene panels and genome sequencing in the clinical setting allows for early diagnosis of patients in neonatal, pediatric, and cardiac intensive care units and impactful change in management.
-
Diagnoses led to significant changes in management for several patients in lower acuity inpatient units supporting further exploration of the utility of rapid sequencing in these settings.
-
This study reviews the limitations of comparing sequencing platforms in the clinical setting and the variables that should be considered in evaluating diagnostic rates across studies.
Similar content being viewed by others

Introduction
Genetic disorders are a leading contributor to the morbidity and mortality of acutely ill neonates and children cared for in neonatal, cardiac, and pediatric intensive care units (NICUs, CICUs, and PICUs, respectively).1,2,3 Initially, genome-wide sequencing technologies had limited applicability to the care of critically ill children due to turnaround times (TATs) of weeks to months.4,5 However, in the past several years the introduction of rapid testing using next-generation sequencing (NGS) technologies, including targeted gene panels, exome sequencing (ES), and rapid genome sequencing (rGS), has been demonstrated to expedite diagnostic processes and improve the care of critically ill children.2,3,6,7,8,9,10,11,12.
Currently, targeted gene panels, ES, and rGS, can provide information on the majority of known disease-causing genes, with results in 1–2 weeks or less. The major differences between tests are in depth and the ability to detect different variant types.13 GS provides the most comprehensive investigation of variant type detecting intronic, mitochondrial, and copy number variants (CNVs) not captured by targeted panels or ES.13 Although not offered on all commercial platforms, GS, can be validated to detect repeat expansions and structural variants. Targeted gene panels may not include all genes of interest such as those with newly discovered or evolving disease associations. Cost is currently correlated with genome coverage, with targeted panels being the least expensive, followed by ES and GS.
Due to high costs, interpretation complexity, and limited access to rGS, targeted gene panels have gained interest as lower-cost alternatives.12 Additionally, while rGS has been used in controlled trial settings, limited studies have evaluated how TATs and diagnostic yields would reflect broader clinical use.14 Our goal was to understand the performance, benefits, and limitations of targeted gene panel and rGS in a “real world” clinical setting. We reviewed two technologies: a rapid targeted gene panel with 4500+ disease‐causing genes (Rapid Mendelian Genes Sequencing Panel, RapSeq)11,15 and rGS. Testing was performed and results were evaluated for infants and children in the NICU, CICU, and PICU at the University of Utah and Primary Children’s Hospital from 2015 to 2020. The two platforms were used in standard clinical care without strict inclusion/exclusion criteria. Here we summarize our observations with these approaches, including diagnostic rates, TAT, and changes in management.
Methods
Subjects and study design
The analysis and publication of data related to this program were approved by the Institutional Review Boards at the University of Utah and Primary Children’s Hospital with a waiver of consent and authorization. Informed consent for the clinical testing was obtained for all patients from at least one parent.
A retrospective data collection and analysis was completed for the period of October 2015–October 2020. RapSeq was performed at the University of Utah Level III and Primary Children’s Hospital (PCH) Level IV NICU from October 2015 to March 2017 at which time testing expanded to include the PCH PICU, CICU, and several regional level III NICUs. rGS was initiated at PCH in August 2019.
Patients were referred for testing by their providers, typically a neonatologist, pediatric intensivist, geneticist, or pediatric subspecialist. Referrals for RapSeq were reviewed by the referring intensivist and the laboratory genetic counseling team. Referrals for rGS were reviewed by a team of neonatologists, geneticists, genetic counselors, and other sub-specialists as needed.
There were no specific inclusion and exclusion criteria for either test. General guidelines were first, suspicion for a genetic condition such as multiple congenital anomalies, a single congenital anomaly with additional dysmorphic features concerning genetic etiology, epileptic encephalopathy, unexplained severe hypotonia, arthrogryposis, and unexplained acute course. Phenotypes typically not considered appropriate for testing included isolated congenital anomalies, associations or sequences with low monogenic yield (e.g., VACTERL association, isolated Pierre Robin sequence), a high suspicion for aneuploidy or phenotypically distinct CNVs (e.g., del22q11.2), and patients with immediate impending demise. Clinical requirements at the onset of testing in 2015 were restricted to acutely ill NICU patients including those with any of the following: respiratory and/or cardiovascular failure, encephalopathy, profound hypotonia, complex brain malformations, severe metabolic disturbance, or multiple congenital anomalies (without a known syndrome), unusually severe or prolonged disease, or multi‐system organ failure. Testing was later expanded to the CICU and PICU in 2016. After initiation of rGS, testing was also offered in lower acuity units, including the infant, neurology, and cardiac medical units.
Descriptive statistics were used to summarize demographic information, diagnostic rates, TAT, and change in management for rGS and RapSeq. The impact on patient clinical management was evaluated through retrospective chart review for all diagnostic cases. Identified management changes were required to be documented in the medical record as contingent on the genetic diagnosis in order to be counted. Care plan changes were divided into nine “Change in Patient Management” categories, and two additional “Family Counseling” categories focused on whether the diagnosis impacted education on the developmental trajectory or recurrence risk.
Variant data is routinely submitted to ClinVar by both reporting laboratories and therefore was not independently uploaded as part of this study.
Clinical test methods and reporting for RapSeq and rGS
RapSeq
RapSeq was performed at ARUP Laboratories, Salt Lake City, UT using a human, nuclear, inherited disease panel with biotinylated DNA probes initially designed to target all known 4503 disease‐causing genes and expanded in 2018 to include over 4900 genes. Detailed methods for DNA extraction, sequencing, and variant annotation have been published.11 RapSeq interpretation focused on pathogenic variants or variants of uncertain significance in genes potentially causative for the patient’s clinical phenotype. Pathogenic variants were confirmed by Sanger sequencing. Initially, RapSeq used a two-staged result reporting system, with preliminary and final reports; diagnostic variants with high confidence calls were received in a preliminary report, with subsequent orthogonal testing confirmation received in the final report. In November of 2018, RapSeq discontinued the use of preliminary reporting due to clinician concern, only returning results after orthogonal testing confirmation. The need for orthogonal confirmation prior to reporting was re-evaluated at the time of rGS implementation and the use of a preliminary report was determined to be appropriate in the setting of acute care.
Rapid GS
The rGS was performed at Rady Children’s Institute for Genomic Medicine using previously described methods.3,14 PCR-free library preparation was performed, and sequencing was conducted on the NovaSeq6000 systems using S1 or S2 flow cells. Genome sequences were aligned to human genome assembly GRCh37 (hg19), and sequence variants were identified with the DRAGEN Platform (Illumina).
Sequence variants were filtered to retain those with allele frequencies of <0.5% in the gnomAD database and classified according to the American College of Medical Genetics and Genomics/Association of Molecular Pathology guidelines. CNVs were identified with Manta and CNVnator and filtered to retain those coding regions of 8000 known disease genes with allele frequencies <2% in the Rady Children’s Institute of Genomic Medicine database. Starting in June 2020, CNV calling was performed using the DRAGEN Platform, and filters were expanded to include all known consensus coding sequence genes. Nucleotide and CNVs were automatically annotated and ranked using Opal Clinical (Fabric Genomics). If a provisional diagnosis was made, it was immediately conveyed to the providers by phone. Reported variants were confirmed by Sanger sequencing or multiplex ligation-dependent probe amplification (MLPA).
Results
Over a 5-year period, there were a total of 142 probands who received rapid NGS with 66 receiving RapSeq and 76 receiving rGS (Table 1). All RapSeq cases were enrolled prior to August 2019 at which time rGS became available at PCH. The majority were completed as parent–child trios in both the RapSeq (65 of 66, 99%) and rGS groups (70 of 76, 92%). Admission data were available from PCH NICU; approximately 11% (50/469 patients) of neonates admitted to the NICU received rGS testing from 2019 to 2020 and approximately 2% (41/1736 patients) of admitted neonates received RapSeq from 2015 to 2019.
Patient characteristics and enrollment locations
Patient demographic and applicable clinical information is summarized in Table 1. Sex and ethnicity were similar, with the majority of patients being male and white of European ancestry. A higher proportion of patients receiving RapSeq were admitted as neonates and ascertained in the NICU as compared to rGS. For patients admitted as neonates, the average age when RapSeq or rGS was ordered was 19 days of age, whereas the average age for testing infants and children was more varied.
Diagnostic rates
In total, across both groups, the diagnostic rate was 39% (56 of 142 cases): 46% for RapSeq and 34% for rGS. Diagnoses were made by identification of pathogenic or likely pathogenic variants as classified by the reporting laboratory and/or identification of a highly suspicious variant of uncertain significance determined to be disease-causing by the clinician following correlation with patient’s presentation. All variants that had confirmatory Sanger sequencing or MLPA were concordant with NGS panel or GS interpretation. Of the diagnostic results, 59% were established as de novo variants through trio sequencing. There were two rGS cases that identified variants in genes that lacked a well-established gene-disease association but were felt to provide a possible explanation for the patient’s phenotype; these were classified as suspected diagnostic but were not counted in the diagnostic rate. “Minor partial diagnoses” were identified in 2 (2.6%) cases by rGS and 1 (1.5%) case by RapSeq (Supplementary Table 1). Cases were considered minor partial diagnoses if they explained part of the presentation, such as in one case the identification of variants that explained congenital hypothyroidism but did not explain the primary reason (congenital diaphragmatic hernia, echogenicity of renal cortex, moderate multifocal white matter injury) for referral to sequencing. Secondary findings are also reported in both groups (Table 2).
We evaluated the impact of patient and testing characteristics on diagnostic yield, including age at admittance and the hospital/unit location (Table 2). The impact of gestational age and birth weight on diagnosis was evaluated for the neonatal groups. Across both groups, 1 of 10 patients (10%) born before 32 weeks had a positive diagnosis compared to 19 of 29 (66%) born between 32 and 37 weeks, and 18 of 39 (46%) patients with a gestational age >37 weeks. Of those neonates born at the low birth weight (<2500 g), 15 of 41 (37%) had a positive diagnosis compared to 23 of 47 (49%) with a birth weight >2500 g. Five of the 76 patients (7%) had diagnostic or medically actionable secondary findings identified on rGS that would not be expected to be found by RapSeq (Supplementary Table 1). These included CNVs (n = 2), mtDNA variants (n = 2) that are considered medically actionable incidental findings, and a suspected diagnostic case that had a novel disease gene that was not included on the RapSeq panel (n = 1). We did not have access to exon-level coverage data to determine the likelihood that specific variants in either group would be missed due to unpredicted technical limitations.
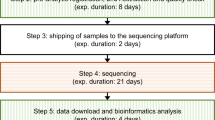
Laboratory TAT
The day to the initial report from the laboratory to the clinician ranged from 2-38 days, with an average laboratory TAT to the first report of 10 days for rGS and 15 days for RapSeq. In both groups, TAT in positive (diagnostic) cases was shorter (Table 2). Laboratory TAT was calculated based on laboratory reported sample receipt date and sample report date; this did not include shipping times or other factors such as delays in sample collection.
Impact on clinical care management and family counseling
The majority of diagnostic cases (75%) had one or more clinical management changes documented (Table 3), without a significant difference between the rWGS (77%) and RapSeq (73%) groups. Of those patients living at the time of the return of results, 81% had a documented change in management. The most common changes in management included new specialist referrals and initiation of imaging screening. A new medication therapy was recommended in 13% of RapSeq diagnostic cases and 27% of rGS diagnostic cases. Recommendations for the avoidance of medication, diet, or exposure were made in 10% of RapSeq diagnostic cases and 15% of rGS diagnostic cases. Recommendations for the avoidance of a procedure were made in 7% of RapSeq diagnostic cases and 12% of rGS diagnostic cases. Additionally, results significantly impacted genetic counseling; all families with diagnostic results received recurrence risk counseling and the majority of families (73% of RapSeq and 54% of rGS) received prognostic information regarding developmental trajectory.
Discussion
We have found that NGS technologies perform well in pediatric and neonatal intensive care unit settings, with diagnostic yields and changes in clinical management similar to clinical trials. Using a targeted gene panel (RapSeq) or rGS, the diagnostic yield was 39% overall (rGS 34% and RapSeq 46%), which is similar to previously published studies for NGS panels, ES, and GS in neonatal and pediatric intensive care populations.3,8,9,10,12,16,17,18 Of those patients with a diagnostic variant reported, 75% had at least one resulting change in clinical management documented. Although not formally tracked, we observed that these tests were well accepted by families with high participation rates.
In this report, as well as in previous clinical studies, inclusion criteria are likely a major contributor to differences in diagnostic rates. We found that more strict selection criteria for RapSeq, as compared to rGS, were associated with higher diagnostic yields. We performed rGS for 76 patients in 13 months (August 2019- October 2020), compared to 66 patients over nearly four years with RapSeq. Admission data at PCH show that over 14 months approximately 11% (50/469 patients) of neonates admitted to the NICU received rGS testing. In contrast, in 44 months approximately 2% (41/1736 patients) of admitted neonates received RapSeq. Consistent with these findings, criteria for RapSeq were initially stricter and patient acuity and the suspicion of a monogenic etiology was highly weighted in the decision to offer testing. A higher percentage of RapSeq patients passed away prior to the return of results (12% in RapSeq, 5% in rGS) and during the admittance that testing was sent (26% in RapSeq, 15% in rGS), indicators that the RapSeq group may be enriched for complex and acute cases. Over time, RapSeq and subsequently rGS, were offered more liberally and to a wider spectrum of patients, including outside of the NICU setting. The age and unit during enrollment differed between the two groups, with RapSeq having a higher number of neonates and NICU patients (Table 2).
It is estimated that 10–25% of neonates in the NICU have an underlying genetic etiology3,19,20,21 and it follows that restricting genetic sequencing to those with characteristics most suspicious for an underlying genetic etiology would enrich diagnostic rates. Correspondingly, the NSIGHT2 study, which enrolled approximately 17% of NICU admissions over a 467-day period, showed a diagnostic rate across all patients of 23%, lower than several previous NICU sequencing studies with more restrictive enrollment criteria.3 Given the diversity of disease presentation seen in the inpatient setting, developing detailed inclusion and exclusion criteria for comparative analysis is a challenge. Reporting the percent of total admittances enrolled is an informative albeit imperfect metric for evaluating variance in diagnostic rates across studies. Wide-spread implementation of these platforms will require further analysis of the relative benefit of these technologies across age groups, acuity level, and phenotypes. Of note, the NSIGHT2 study randomized patients to rapid ES and GS groups, without a statistically significant difference in diagnostic yield seen.
Of particular interest within the NICU group is our observation that neonates born before 32 weeks showed a comparatively low diagnostic rate (10%). Given the comorbidities of prematurity, evaluating this group of neonates for underlying health conditions is particularly challenging. Further studies are needed to understand how to effectively implement genomic sequencing in these most premature infants, for example, whether different clinical characteristics in more premature infants are associated with improved diagnostic yields.
Within the PICU group, the robust diagnostic rate for both platforms (Table 2) is consistent with previous observation17 and further supports the growing recognition of the value of these tools in the evaluation of infant and childhood-onset acute disease. Additionally, rGS was utilized in 17 cases in lower acuity units (e.g., medical, neurologic, and cardiac units) with a remarkable diagnostic rate of 42% and several notable cases of change in prognosis and management. Further studies are needed to determine best practices for use of these tools in lower acuity but still medically vulnerable patients that could benefit from comprehensive and expediated genetic evaluation.
Given the shortcomings of comparing diagnostic yields across different studies, the impact of limiting sequencing to select genes in this population is not yet fully appreciated. In our cohort, 5 of the 76 patients (7%) had medically informative variants identified on rGS that would not be identified on the RapSeq panel, whereas, there were no variants identified through RapSeq that would be suspected to be missed on a rGS platform. This is based on the predicted performance of each platform to detect variant type but does not consider exon-level coverage or other unpredicted technical limitations. In the GEMINI study, where both GS and a 1722 gene panel are concurrently completed for acutely ill neonates, 67% of patients with a reportable variant had discordant results, defined as the two laboratories not identifying the same variant or reporting the same variant but with different classifications. 56% of discordant results were due to technical limitations of the gene panel, including missed aneuploidies, CNVs, excluded genes, or genes with limited coverage.12 Our observations affirm that in practice, more diagnoses may be missed by targeted gene panels than GS, even with the use of a more comprehensive targeted gene panel (4900+ genes).
Differences in variant reporting methods used by laboratories likely also contribute to variability in diagnostic rates. Variant reporting discrepancies between laboratories is a well-established issue, with discordance in classification between qualified genomic laboratory analysts ranging from 12 to 71%.22,23,24,25,26 In the GEMINI study, differences in variant interpretation were the second most common cause of discordant results, with 41% (21/51) of discordant results attributed to this.12 Additionally, previous studies of ES and GS have shown that hospital-based laboratories have increased diagnostic rates and decreased false-positive rates in comparison to reference laboratories.27,28 The two laboratories involved in our study, ARUP Laboratories and Rady Children’s Institute for Genomic Medicine, are hospital-based laboratories associated with academic institutions, and both comprehensively evaluate medical records in order to complete a phenotypic-driven analysis. ARUP Laboratories, a University of Utah affiliated lab, integrated routine communication with the clinicians into the analysis process to optimize the resolution of complex questions and elicit additional phenotypic data. Without a study model where patients are tested using both platforms, as with the GEMINI study, it is difficult to fully appreciate the possible impact of variant reporting on diagnostic rates.
The diagnostic results in our cohorts led to numerous changes in clinical management in both testing groups (Table 3), consistent with previous observations.11,29,30 This includes initiation of medical and dietary therapies, avoidance of contra-indicated exposures, and initiation of care to evaluate for associated risks, including initiation of imaging and laboratory work screening and referral to specialists. In several cases, providers documented that identified diagnoses directly resulted in the avoidance of significant procedures, including cardiac transplant, neurosurgical intervention, and lung and muscle biopsies. Studies have demonstrated improved patient outcomes and cost value with rapid diagnosis,17,29,30 and initial evidence suggests that shorter TAT, in the matter of days to weeks instead of months, further increases this effect.3,11,17 Further, there are some conditions, such as treatable metabolic and seizure disorders, for which diagnosis in the 2–3 days following onset are important for improved outcomes compared to diagnosis at 1–2 weeks. Additional studies are planned to evaluate the impact of rapid diagnosis and observed changes in management on patient outcomes and healthcare costs in our cohorts.
As the use of NGS technologies continues to expand, better understanding the benefits and limitations of the different platforms will be imperative for cost-effective widespread adoption. With the diagnostic rate of 39%, based on the current contracted list prices of RapSeq ($4500) and rGS ($12,500) trios, the cost per diagnosis in the RapSeq group and rGS group would be $11,538 and $32,051, respectively. The option for a lower-cost test might be valuable in low-resource settings, especially if the alternative is no testing at all. Lower cost approaches could facilitate the equitable implementation of NGS testing. However, cost considerations also need to factor in the cost of missed diagnoses; cost of delayed diagnosis for sequential testing; provider and family perception of a complete diagnostic workup; and long-term costs (such as continued ES or GS testing if a prior panel test was uninformative).
Future work will need to further delineate optimal strategies for clinical use of NGS, while taking into account patient as well as test characteristics. These studies should include evaluation of diagnostic yields across different presentations; the short- and long-term costs and cost-effectiveness; the effects of diagnosis on providers, patients, and families; and testing in socioeconomically and racially diverse patient cohorts. In summary, our findings demonstrate that real-world use of NGS in pediatric settings is similar to clinical studies, with diagnostic rates of 39% and impacts on patient management.
References
Malam, F. et al. Benchmarking outcomes in the Neonatal Intensive Care Unit: cytogenetic and molecular diagnostic rates in a retrospective cohort. Am. J. Med. Genet. A 173, 1839–1847 (2017).
Daoud, H. et al. Next-generation sequencing for diagnosis of rare diseases in the neonatal intensive care unit. CMAJ Can. Med. Assoc. J. 188, E254–E260 (2016).
Kingsmore, S. F. et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in ill infants. Am. J. Hum. Genet 105, 719–733 (2019).
Ng, S. B. et al. Exome sequencing identifies the cause of a Mendelian disorder. Nat. Genet. 42, 30–35 (2010).
Taylor, J. C. et al. Factors influencing success of clinical genome sequencing across a broad spectrum of disorders. Nat. Genet. 47, 717–726 (2015).
Saunders, C. J. et al. Rapid whole-genome sequencing for genetic disease diagnosis in neonatal intensive care units. Sci. Transl. Med. 4, 154ra135 (2012).
Soden, S. E. et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci. Transl. Med. 6, 265ra168 (2014).
Willig, L. K. et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir. Med. 3, 377–387 (2015).
Meng, L. et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 171, e173438 (2017).
van Diemen, C. C. et al. Rapid targeted genomics in critically ill newborns. Pediatrics 140, e20162854 (2017).
Brunelli, L. et al. Targeted gene panel sequencing for the rapid diagnosis of acutely ill infants. Mol. Genet. Genom. Med. 7, e00796 (2019).
Maron, J. L. et al. Novel variant findings and challenges associated with the clinical integration of genomic testing: an interim report of the Genomic Medicine for Ill Neonates and Infants (GEMINI) Study. JAMA Pediatr. 175, e205906 (2021).
Belkadi, A. et al. Whole-genome sequencing is more powerful than whole-exome sequencing for detecting exome variants. Proc. Natl Acad. Sci. USA 112, 5473–5478 (2015).
Dimmock, D. et al. Project Baby Bear: rapid precision care incorporating rWGS in 5 California children’s hospitals demonstrates improved clinical outcomes and reduced costs of care. Am. J. Hum. Genet. 108, 1231–1238 (2021).
Brunelli, L. et al. A rapid gene sequencing panel strategy to facilitate precision neonatal medicine. Am. J. Med. Genet. A 173, 1979–1982 (2017).
Petrikin, J. E. et al. The NSIGHT1-randomized controlled trial: rapid whole-genome sequencing for accelerated etiologic diagnosis in critically ill infants. NPJ Genom. Med. 3, 6 (2018).
Sanford, E. F. et al. Rapid whole genome sequencing has clinical utility in children in the PICU. Pediatr. Crit. Care Med. 20, 1007–1020 (2019).
de Castro, M. J. et al. Rapid phenotype-driven gene sequencing with the NeoSeq panel: a diagnostic tool for critically ill newborns with suspected genetic disease. J Clin Med. 9, 2362 (2020).
Causey, T. N., Bodurtha, J. N. & Ford, N. A genetic perspective on infant mortality. South Med. J. 103, 440–444 (2010).
Holm, I. A. et al. The BabySeq project: implementing genomic sequencing in newborns. BMC Pediatr. 18, 225 (2018).
Kapil, S., Fishler, K. P., Euteneuer, J. C. & Brunelli, L. Many newborns in level IV NICUs are eligible for rapid DNA sequencing. Am. J. Med. Genet. A 179, 280–284 (2019).
Amendola, L. M. et al. Performance of ACMG-AMP variant-interpretation guidelines among nine laboratories in the Clinical Sequencing Exploratory Research Consortium. Am. J. Hum. Genet. 99, 247 (2016).
Harrison, S. M. et al. Clinical laboratories collaborate to resolve differences in variant interpretations submitted to ClinVar. Genet. Med. 19, 1096–1104 (2017).
Balmaña, J. et al. Conflicting interpretation of genetic variants and cancer risk by commercial laboratories as assessed by the prospective registry of multiplex testing. J. Clin. Oncol. 34, 4071–4078 (2016).
Pepin, M. G. et al. The challenge of comprehensive and consistent sequence variant interpretation between clinical laboratories. Genet. Med. 18, 20–24 (2016).
Hoskinson, D. C., Dubuc, A. M. & Mason-Suares, H. The current state of clinical interpretation of sequence variants. Curr. Opin. Genet. Dev. 42, 33–39 (2017).
Baldridge, D. et al. The Exome Clinic and the role of medical genetics expertise in the interpretation of exome sequencing results. Genet. Med. 19, 1040–1048 (2017).
Clark, M. M. et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. Npj Genom. Med. 3, 1–10 (2018).
French, C. E. et al. Whole genome sequencing reveals that genetic conditions are frequent in intensively ill children. Intensive Care Med. 45, 627–636 (2019).
Farnaes, L. et al. Rapid whole-genome sequencing decreases infant morbidity and cost of hospitalization. Npj Genom. Med. 3, 1–8 (2018).
Acknowledgements
We would like to acknowledge and express our gratitude to the Primary Children’s Foundation and Primary Children’s leadership, including Lisa Vitkus, Seth Andrews, and Dustin Lipson, whose support of the Primary Children’s Center for Personalized Medicine and rapid genome sequencing program has made this research possible.
Author information
Authors and Affiliations
Contributions
R.P., S.M.J., D.B., C.M., M.R., B.M., P.B.-T., T.T., L.N., S.B.B., B.O., J.F.-D., N.L., M.T.F., J.L.B., and L.B. provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; R.P., S.M.J., D.B., C.M., M.R., B.M., P.B.-T., S.C., J.L.B., and L.B. drafted or revised the article critically for important intellectual content; and R.P., S.M.J., J.L.B., and L.B. provided final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
J.L.B. has served as a consultant to Bluebird Bio, Inc., Calico, Inc., Denali, Neurogene, Inc., Enzyvant, Inc., and Passage Bio and owns stock in Orchard Therapeutics. S.B.B. holds stock options in Genome Medical, Inc. There are no other disclosures.
Ethics approval and consent to participate
The analysis and publication of data related to this program were approved by the Institutional Review Boards at the University of Utah and Primary Children’s Hospital with a waiver of consent and authorization. Informed consent for the clinical test was obtained in all cases from at least one parent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Palmquist, R., Jenkins, S.M., Bentley, D. et al. Evaluating use of changing technologies for rapid next-generation sequencing in pediatrics. Pediatr Res 92, 1364–1369 (2022). https://doi.org/10.1038/s41390-022-01965-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-01965-5
This article is cited by
-
Genomes in clinical care
npj Genomic Medicine (2024)
-
Evidence review and considerations for use of first line genome sequencing to diagnose rare genetic disorders
npj Genomic Medicine (2024)