Abstract
Background
Monitoring of heart rate characteristics (HRC) index may improve outcomes of late-onset neonatal sepsis (LOS) through early detection. We aimed at describing the association between LOS and elevated HRC index.
Methods
This single-center retrospective case–control study included neonates who presented with blood culture-proven hospital-acquired LOS. Controls were matched to cases (ratio 1:2) based on gestational age, postnatal age, and birthweight. We compared the highest HRC indexes in the 48 h preceding blood culture sampling in LOS cases to the highest HRC indexes at the same postnatal days in controls.
Results
In 59 LOS cases and 123 controls, an HRC index > 2 was associated with LOS (OR 7.1, 95% CI 2.6–19.0). Sensitivity and specificity of an HRC index > 2 to predict LOS were 53% (32/59) and 79% (98/123). Sensitivity increased from 25% in infants born > 32 weeks to 76% in infants born < 28 weeks. Specificity decreased from 97% in infants > 32 weeks to 63% in those born < 28 weeks.
Conclusions
An increase of HRC index > 2 has a significant association with the diagnosis of LOS, supporting the use of HRC monitoring to assist early detection of LOS. Clinicians using HRC monitoring should be aware of its diagnostic accuracy and limitations in different gestational age groups.
Impact
-
There is a paucity of data regarding the predictive value of heart rate characteristics (HRC) monitoring for early diagnosis of late-onset neonatal sepsis (LOS) in daily clinical practice.
-
Monitoring of heart rate characteristics provides valuable information to assist the early diagnosis of LOS across all gestational age groups.
-
However, the strong influence of gestational age on positive and negative predictive values adds complexity to the interpretation of HRC indexes.
Similar content being viewed by others
Introduction
Infection is a leading cause of death and disability in newborns.1 Late-onset sepsis (LOS) occurs mainly in hospitalized neonates, and in up to 30% of very preterm newborns.2,3,4 As initial signs are often subtle and/or non-specific, diagnosis and treatment can be delayed, resulting in an increased risk of adverse outcomes. Early detection of sepsis is key to guide the initial management and improve outcome.5 Reduced variability in heart rate and transient decelerations have been observed in the hours to days before diagnosis of LOS. Characterization of these abnormal heart rate characteristics (HRC) through mathematical models has led to the development of an HRC index, representing the fold-increase in risk of sepsis during the next 48 h.6,7 This tool can be used as a non-invasive early physiomarker of sepsis, to alert neonatologists before overt clinical deterioration. A large randomized control trial has demonstrated a reduction of mortality with continuous real-time HRC monitoring in very low birthweight preterm infants.8
Despite the benefit shown in the trial by Moorman et al., the predictive value of HRC monitoring in daily clinical practice has been questioned.9 An increase in HRC is associated with other conditions than sepsis, including focal infections, necrotizing enterocolitis (NEC), surgery, respiratory deterioration, brain hemorrhage, and use of anticholinergic drugs.10,11,12 An observational descriptive study reported that HRC scores are often elevated in newborns who do not have bloodstream infection, and infrequently elevated in those with culture-proven sepsis.13
Given the limited data available in the literature regarding the predictive value of HRC monitoring outside the controlled setting of a trial, we conducted a study to determine the association between blood culture-proven LOS and elevated HRC index.
Patients and methods
This retrospective case–control study was conducted in patients hospitalized between September 2014 and December 2018 at the tertiary care neonatal unit of the University Hospital of Lausanne, Switzerland. The study was approved by the Cantonal Ethics Committee of Vaud (Lausanne, Switzerland, ID 2018-01411). The need for informed consent was waived, as the potential difficulties in obtaining consent were considered disproportionate to the low risk and observational nature of the study.
Infants were included if they developed microbiologically documented hospital-acquired LOS, defined by a positive blood culture collected at a postnatal age greater than 72 h in infants hospitalized for more than 48 h before the sepsis episode.4 Contaminated blood cultures were excluded based on the following criteria: pathogens usually considered as contaminants, Coagulase-negative staphylococci (CoNS) in the absence of a peripheral or central catheter at the time of blood culture collection, blood cultures growing a mixed flora of CoNS, or decision of the physician in charge to treat the patient with antibiotics for less than 5 days. Only the first episode of hospital-acquired LOS was included for each patient. For each case, we identified one to three controls matched for gestational age (±2 weeks), postnatal age (±2 days), and birth weight (±20%) who did not develop LOS or necrotizing enterocolitis, and who were not under antibiotic treatment during the period of observation.
Hourly HRC indexes were acquired using the HRC monitor system from Medical Predictive Science Corporation. Physicians and nurses were instructed that an HRC index > 2 or an increase of >1 point compared to the preceding hour should prompt a clinical evaluation of the patient by a physician, in order to decide whether or not additional investigations and/or treatment should be conducted. HRC indexes recorded during an observation period defined as the 48 h preceding blood culture sampling in LOS cases, and at the corresponding postnatal age in controls were analyzed. The primary predictive variable was the HRC index, dichotomized into elevated vs non-elevated. In the main analysis, HRC index was considered elevated if its maximum value (HRCMAX) measured over the observation period was above two.6 The analysis was then repeated after dichotomizing HRCMAX ≥ 5 vs <5, and HRCMAX = 7 vs <7. We estimated the optimal HRCMAX cut-off point, that best discriminates between LOS cases and controls, by finding the HRCMAX value that maximizes the Youden index (specificity plus sensitivity). HRC indexes measured after administration of drugs affecting HRC (anticholinergics and neuromuscular blocking agents) and after surgery were not included in analyses.14 Clinical and microbiological data were obtained from the database of the microbiology laboratory, electronic medical charts and through the clinical information system Metavision®.
Patient characteristics were summarized by descriptive statistics reporting proportions, means, standard deviations, medians, and interquartile ranges. Univariate analyses were used to assess differences between cases and controls for all demographic and clinical variables. We applied association tests (Pearson chi-square or Fisher’s exact) for binary variables, and Wilcoxon–Mann Whitney tests to compare quantitative variables. Conditional logistic regressions were used to test whether the dichotomized HRCMAX index measured in the 48 h preceding blood culture sampling-predicted LOS. Areas under the ROC curve (AUROC) from unconditional logistic regressions, sensitivity, specificity, positive predictive values and negative predictive value were calculated for each of the three dichotomizations of HRCMAX. Finally, a linear mixed regression model was estimated to assess whether the HRC trajectories differed over time between cases and controls. Mixed models take into account the lack of independence of data measured repeatedly on the same subjects. Our model estimated the effect of group (case vs control), time (48 h preceding blood culture sampling) and the statistical interaction between group and time. Since HRC indexes followed a highly skewed distribution they were log-transformed for this analysis. Statistical analyses were carried out using Stata/IC software, versions 15.1 and 16.0 (StataCorp LLC, College Station, Texas).
Results
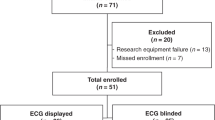
Among the 2274 patients hospitalized in the tertiary care neonatal unit of the University Hospital of Lausanne during the study period, 67 presented with at least one episode of blood culture-proven hospital-acquired LOS. We excluded six episodes for which the HRC index was not monitored, and two that could not be matched to controls due to a birthweight <500 g. Fifty-nine LOS episodes were analyzed. Median postnatal age at sepsis was 13 days (IQR 12). Infants with LOS had a median gestational age of 29 weeks (IQR 8) and a median birth weight of 1056 g (IQR 1344), while controls had a median gestational age of 28 weeks (IQR 4) and a median birthweight of 1000 g (IQR 600) (Table 1). The main pathogens were CoNS (28/59, 47%), Escherichia coli (9/59, 15%), Klebsiella pneumoniae (7/59, 12%), and Staphylococcus aureus (6/59, 10%) (Table 2).
We compared 1811 hourly-recorded HRC indexes and HRC index trajectories in the 48 h preceding sepsis evaluation in 59 cases of LOS with 3402 HRC indexes and HRC index trajectories in 123 controls of the same postnatal age (Fig. 1). HRCMAX was higher in LOS (median 2.77, IQR 5.16) compared to controls (median 1.05, IQR 1.20, P < 0.001) (Table 2). An HRCMAX > 2 was found in 54% (31/59) of LOS cases and 20% (25/123) of controls, and an HRCMAX of 7 was found in 19% (11/59) of LOS cases and <1% (1/123) of controls. HRCMAX was higher in the infants born < 32 weeks than in those ≥32 weeks (Supplementary Fig. 1).
a Hourly HRC indexes in the 48 h preceding blood culture sampling for sepsis evaluation in 59 late-onset sepsis cases, and at a similar postnatal age in 123 controls. The medians (brown lines), 25th and 75th percentiles (orange lines) are shown. b Individual HRC index trajectories in the 48 h preceding sepsis evaluation in 59 late-onset sepsis cases, and at a similar postnatal age in 123 controls.
Conditional logistic regressions indicated that an HRCMAX > 2 and an HRCMAX of 7 were associated with LOS, with ORs of 7.1 (95% CI 2.6–19; AUROC = 0.66) and 24.3 (95% CI 3–191.7; AUROC = 0.55). An HRCMAX > 2 was associated with a combined outcome of the requirement for invasive ventilation and/or hemodynamic support with catecholamines within 7 days after sepsis onset and/or death before discharge (P < 0.001). The sensitivity and specificity of an HRCMAX > 2 to predict LOS were 52% (32/61) and 79% (101/127) (Table 3). Sensitivity increased from 24% in infants born > 32 weeks to 76% in infants born < 28 weeks, and specificity decreased from 97% in infants > 32 weeks to 63% in those born < 28 weeks. Setting the threshold of HRCMAX at ≥5 or =7 increased specificity, but reduced sensitivity to predict LOS (Supplementary Table 1). An HRCMAX of 2.76 was the optimal cut-off point to discriminate between sepsis cases and controls, with an AUROC of 0.70, a sensitivity of 0.51, and a specificity of 0.89.
When analyzing LOS cases according to pathogen, we found that the sensitivity, specificity, positive and negative predictive values of an HRCMAX > 2 to diagnose LOS were 53.6%, 79.7%, 37.5% and 88.3% for CoNS cases (n = 28). For other pathogens (n = 31), the sensitivity, specificity, positive and negative predictive values of an HRCMAX > 2 to diagnose LOS were 51.6%, 79.7%, 39.0%, and 86.7%.
A linear mixed regression model estimated that 48 h before blood culture sampling, the average HRC index was higher in LOS cases than in controls (mean difference on log scale 0.56, 95% CI 0.32 to 0.81, p < 0.001). The average values did not change during the 48 h observation period (mean increase per hour on log scale independently of group 0.00016, 95% CI −0.0028 to 0.0032, p = 0.92), and the difference between the two groups remained constant over time (mean difference between time slopes 0.003, 95% CI −0.008-0.002, p = 0.26) (Supplementary Fig. 2).
Discussion
In this retrospective case–control study, we observed an association between an elevated HRC index (>2) and LOS. The association with LOS was stronger with an HRC index > 5 or =7, but the optimal cutoff to discriminate LOS from controls was estimated at 2.76.
Early detection of sepsis followed by timely intervention is key to prevent mortality and morbidity.5 Studies performed in children and adults indicate that delays in antimicrobial treatment are associated with prolonged organ dysfunction and increased risk of death.15,16,17 Given the high mortality and morbidity associated with neonatal sepsis, an approach allowing to detect of sepsis before the appearance of clinical signs may allow optimization of the early management and could lead to better outcomes. Based on the results of a randomized control trial and subsequent publications on the same cohort, HRC monitoring was identified as a promising tool for the early diagnosis of LOS in preterm newborns.8 However, these results were challenged by a study of 2384 infants hospitalized in a tertiary care neonatal unit, including 46 infants with LOS.13 LOS was observed only in 5% of neonates with scores ≥ 2. Among infants with LOS, only 37% had at least one score ≥ 2, and 11% had at least one score ≥ 5 in the 48 h period prior to sepsis evaluation by blood culture. The proportion of HRC scores ≥ 2 and ≥ 5 in LOS cases was 1.5 and 3-fold higher in our study compared to the findings by Coggins et al., suggesting a better diagnostic performance of HRC monitoring in our setting. Coggins et al. did not have access to hourly HRC indexes, but only to those transcribed in electronic medical records, which could have impacted their estimation of the diagnostic performance of HRC monitoring.13 Moreover, differences in patient populations and infection prevention and management practices could account for the discrepancies between the two studies.
In our study, diagnostic accuracy of HRC index was strongly influenced by gestational age. This was not unexpected, given that this tool was initially designed, tested, and validated in very low birthweight preterm infants.8,18 LOS is more prevalent in extremely preterm newborns.1,2 In this subgroup, we found high sensitivity and negative predictive value of HRC index, which may be useful for early detection. However, the relatively low specificity and positive predictive value in extremely preterm newborns might trigger unnecessary antibiotic treatments. Yet, HRC monitoring was not associated with an increased exposure to antibiotics in the trial by Moorman et al.8 In infants born > 32 weeks, for which nosocomial sepsis is less prevalent, we observed a relatively low sensitivity and negative predictive value of HRC index, but a high specificity and positive predictive value. Therefore, our findings indicate that HRC monitoring provides valuable information for the early recognition of LOS in all gestational age groups. But the strong influence of gestational age on positive and negative predictive values adds complexity to its interpretation.
Analysis of individual patient’s HRC index trajectories indicates important fluctuations of HRC indexes during the 48 h prior to sepsis evaluation and multiple different patient trajectories. This is consistent with the spikes in the HRC index and divergent trajectories that have been described in previous reports,14,19 and the heterogeneous nature of sepsis. Interestingly, HRC index was higher in LOS cases compared to controls throughout the 48 h observation period preceding the sepsis evaluation by blood culture, suggesting that the clinicians’ response to elevated HRC indexes did not always involve immediate sampling for blood cultures. This is in line with the approach proposed in the trial by Moorman et al.8, where a rising HRC index required a bedside evaluation of the patient and consideration for additional blood testing, but no mandatory investigations or treatment. As the elevation of HRC index might be the earliest and only sign of imminent clinical deterioration leading to sepsis, and given the non-negligible proportion of false alarms, finding the adequate response to an elevated HRC index can be challenging for clinicians. Traditionally, early recognition of sepsis is based on the assessment of risk factors, symptoms and clinical signs, vital signs, and biomarkers.1 Models based on machine learning, integrating data on patient demographics, vital signs and biomarkers have been recently developed to improve the capacity to detect LOS.20,21,22 These algorithms have a superior sensitivity (74–84%) and positive predictive values (57–82%), but similar specificity (80%) and negative predictive values compared to HRC index. Given the complexity to make an early and reliable diagnosis of LOS, it is expected that multimodal approaches will perform better than single biomarkers or physiologic markers. Therefore, it will be important to determine the value of HRC monitoring in future multimodal prediction models for the early recognition of sepsis. Importantly, an elevated HRC index was also associated with a combined outcome of death or dysfunction of the respiratory or cardiovascular systems in infants with LOS, in line with the results from a recent study.23
This study has limitations, as it was conducted at a single center with a retrospective design and a relatively small sample size. However, we report on a large number of HRC indexes in well-defined LOS cases, with the inclusion of all gestational age groups, and analysis of sensitivity, specificity, positive and negative predictive values. Moreover, HRC indexes that could have been modified by drugs or medical conditions were excluded.24
Conclusion
Elevated HRC indexes are associated with LOS in newborn infants of all gestational ages. Clinicians using HRC monitoring should be aware of its diagnostic accuracy and limitations in different gestational age groups. Monitoring of HRC indexes has its place in the surveillance and management of newborns at risk of LOS together with evaluation of risk factors, clinical signs symptoms, vital signs, and biomarkers, and should be considered in future multimodal sepsis prediction models.
References
Shane, A. L., Sanchez, P. J. & Stoll, B. J. Neonatal sepsis. Lancet 390, 1770–1780 (2017).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD neonatal research network. Pediatrics 110, 285–291 (2002).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD neonatal research network. Pediatrics 126, 443–456 (2010).
Giannoni, E. et al. Neonatal sepsis of early onset, and hospital-acquired and community-acquired late onset: a prospective population-based cohort study. J. Pediatr. 201, 106–114.e104 (2018).
Giannoni, E. & Schlapbach, L. J. Editorial: sepsis in neonates and children. Front. Pediatr. 8, 621663 (2020).
Griffin, M. P. et al. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr. Res. 53, 920–926 (2003).
Griffin, M. P. et al. Abnormal heart rate characteristics are associated with neonatal mortality. Pediatr. Res. 55, 782–788 (2004).
Moorman, J. R. et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 159, 900–906 e901 (2011).
Groves, A. M. & Edwards, A. D. Heart rate characteristic monitoring-hero or villain? J. Pediatr. 159, 885–886 (2011).
Stone, M. L. et al. Abnormal heart rate characteristics before clinical diagnosis of necrotizing enterocolitis. J. Perinatol. 33, 847–850 (2013).
Sullivan, B. A. et al. Early heart rate characteristics predict death and morbidities in preterm infants. J. Pediatr. 174, 57–62 (2016).
Weitkamp, J. H. The role of biomarkers in suspected neonatal sepsis. Clin. Infect. Dis. 73, e391–e393 (2021).
Coggins, S. A. et al. Heart rate characteristic index monitoring for bloodstream infection in an NICU: a 3-year experience. Arch. Dis. Child Fetal Neonatal Ed. 101, F329–F332 (2016).
Sullivan, B. A., Grice, S. M., Lake, D. E., Moorman, J. R. & Fairchild, K. D. Infection and other clinical correlates of abnormal heart rate characteristics in preterm infants. J. Pediatr. 164, 775–780 (2014).
Kumar, A. et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit. Care Med. 34, 1589–1596 (2006).
Weiss, S. L. et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit. Care Med. 42, 2409–2417 (2014).
Schmatz, M. et al. Surviving sepsis in a referral neonatal intensive care unit: association between time to antibiotic administration and in-hospital outcomes. J. Pediatr. 217, 59–65.e51 (2020).
Swanson, J. R. et al. Neonatal intensive care unit length of stay reduction by heart rate characteristics monitoring. J. Pediatr. 198, 162–167 (2018).
Zimmet, A. M., Sullivan, B. A., Moorman, J. R., Lake, D. E. & Ratcliffe, S. J. Trajectories of the heart rate characteristics index, a physiomarker of sepsis in premature infants, predict neonatal icu mortality. JRSM Cardiovasc. Dis. 9, 2048004020945142 (2020).
Fairchild, K. D. et al. Vital signs and their cross-correlation in sepsis and nec: a study of 1,065 very-low-birth-weight infants in two nicus. Pediatr. Res 81, 315–321 (2017).
Masino, A. J. et al. Machine learning models for early sepsis recognition in the neonatal intensive care unit using readily available electronic health record data. PLoS ONE 14, e0212665 (2019).
Mani, S. et al. Medical decision support using machine learning for early detection of late-onset neonatal sepsis. J. Am. Med. Inf. Assoc. 21, 326–336 (2014).
Zeigler, A. C., Ainsworth, J. E., Fairchild, K. D., Wynn, J. L. & Sullivan, B. A. Sepsis and mortality prediction in very low birth weight infants: analysis of HeRO and nSOFA. Am. J. Perinatol. https://doi.org/10.1055/s-0041-1728829 (2021). Online ahead of print.
Chiera, M. et al. Heart rate variability in the perinatal period: a critical and conceptual review. Front. Neurosci. 14, 561186 (2020).
Acknowledgements
Eric Giannoni is supported by the Leenaards Foundation.
Author information
Authors and Affiliations
Contributions
L.R.: Conception or design of the work; data acquisition; data analysis and interpretation; drafting the article; critical revision of the article and final approval of the version to be published. A.-S.R.: Conception or design of the work; data analysis and interpretation; drafting the article; critical revision of the article and final approval of the version to be published. P.B.: Data analysis and interpretation; drafting the article; critical revision of the article and final approval of the version to be published. C.S.: Data acquisition; drafting the article and final approval of the version to be published. S.A.: Conception or design of the work; data analysis and interpretation; drafting the article; critical revision of the article and final approval of the version to be published. E.G.: Conception or design of the work; data acquisition; data analysis and interpretation; drafting the article; critical revision of the article and final approval of the version to be published.
Corresponding author
Ethics declarations
Consent statement
Patient consent was not required for this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rio, L., Ramelet, AS., Ballabeni, P. et al. Monitoring of heart rate characteristics to detect neonatal sepsis. Pediatr Res 92, 1070–1074 (2022). https://doi.org/10.1038/s41390-021-01913-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01913-9