Abstract
Background
Heart rate characteristics aid early detection of late-onset sepsis (LOS), but respiratory data contain additional signatures of illness due to infection. Predictive models using cardiorespiratory data may improve early sepsis detection. We hypothesized that heart rate (HR) and oxygenation (SpO2) data contain signatures that improve sepsis risk prediction over HR or demographics alone.
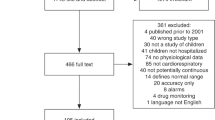
Methods
We analyzed cardiorespiratory data from very low birth weight (VLBW, <1500 g) infants admitted to three NICUs. We developed and externally validated four machine learning models to predict LOS using features calculated every 10 m: mean, standard deviation, skewness, kurtosis of HR and SpO2, and cross-correlation. We compared feature importance, discrimination, calibration, and dynamic prediction across models and cohorts. We built models of demographics and HR or SpO2 features alone for comparison with HR-SpO2 models.
Results
Performance, feature importance, and calibration were similar among modeling methods. All models had favorable external validation performance. The HR-SpO2 model performed better than models using either HR or SpO2 alone. Demographics improved the discrimination of all physiologic data models but dampened dynamic performance.
Conclusions
Cardiorespiratory signatures detect LOS in VLBW infants at 3 NICUs. Demographics risk-stratify, but predictive modeling with both HR and SpO2 features provides the best dynamic risk prediction.
Impact
-
Heart rate characteristics aid early detection of late-onset sepsis, but respiratory data contain signatures of illness due to infection.
-
Predictive models using both heart rate and respiratory data may improve early sepsis detection.
-
A cardiorespiratory early warning score, analyzing heart rate from electrocardiogram or pulse oximetry with SpO2, predicts late-onset sepsis within 24 h across multiple NICUs and detects sepsis better than heart rate characteristics or demographics alone.
-
Demographics risk-stratify, but predictive modeling with both HR and SpO2 features provides the best dynamic risk prediction.
-
The results increase understanding of physiologic signatures of neonatal sepsis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Moorman, J. R. et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 159, 900–906 (2011). e1.
King, W. E., Carlo, W. A., O’Shea, T. M. & Schelonka, R. L., HRC neurodevelopmental follow-up investigators. Heart rate characteristics monitoring and reduction in mortality or neurodevelopmental impairment in extremely low birthweight infants with sepsis. Early Hum. Dev. 159, 105419 (2021).
Greenberg, R. G. et al. Prolonged duration of early antibiotic therapy in extremely premature infants. Pediatr. Res 85, 994–1000 (2019).
Lu, J. & Claud, E. C. Connection between gut microbiome and brain development in preterm infants. Dev. Psychobiol. 61, 739–751 (2019).
Ting, et al. Duration of initial empirical antibiotic therapy and outcomes in very low birth weight infants. Pediatrics. 143, e20182286 (2019).
Dardas, M. et al. The impact of postnatal antibiotics on the preterm intestinal microbiome. Pediatr. Res 76, 150–158 (2014).
Sullivan B. A., Kausch S. L., Fairchild K. D. Artificial and human intelligence for early identification of neonatal sepsis. Pediatr Res. 2022. https://doi.org/10.1038/s41390-022-02274-7 Epub ahead of print.
Fairchild, K. D. et al. Vital signs and their cross-correlation in sepsis and NEC: a study of 1,065 very-low-birth-weight infants in two NICUs. Pediatr. Res 81, 315–321 (2017).
Griffin, M. P. et al. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr. Res 53, 920–926 (2003).
Sullivan, B. A. et al. Clinical and vital sign changes associated with late-onset sepsis in very low birth weight infants at 3 NICUs. J. Neonatal Perinat. Med 14, 553–561 (2021).
Sullivan, B. A. et al. Early pulse oximetry data improves prediction of death and adverse outcomes in a two-center cohort of very low birth weight infants. Am. J. Perinatol. 35, 1331–1338 (2018).
Kovatchev, B. P. et al. Sample asymmetry analysis of heart rate characteristics with application to neonatal sepsis and systemic inflammatory response syndrome. Pediatr. Res 54, 892–898 (2003).
Lake, D. E., Richman, J. S., Griffin, M. P. & Moorman, J. R. Sample entropy analysis of neonatal heart rate variability. Am. J. Physiol. Regul. Integr. Comp. Physiol. 283, R789–R797 (2002).
Griffin, M. P. et al. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics 116, 1070–1074 (2005).
Fairchild, K. D. et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr. Res. 74, 570–575 (2013).
Fairchild, K. et al. Clinical associations of immature breathing in preterm infants: part 1-central apnea. Pediatr. Res 80, 21–27 (2016).
Herlenius, E. An inflammatory pathway to apnea and autonomic dysregulation. Respir. Physiol. Neurobiol. 178, 449–457 (2011).
Joshi, R. et al. Predicting neonatal sepsis using features of heart rate variability, respiratory characteristics, and ECG-derived estimates of infant motion. IEEE J. Biomed. Health Inf. 24, 681–692 (2020).
Cabrera-Quiros, L. et al. Prediction of late-onset sepsis in preterm infants using monitoring signals and machine learning. Crit. Care Explor 3, e0302 (2021).
Peng Z., et al. A continuous late-onset sepsis prediction algorithm for preterm infants using multi-channel physiological signals from a patient monitor. IEEE J Biomed Health Inform. 2022. https://doi.org/10.1109/JBHI.2022.3216055 Epub ahead of print.
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. M. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann. Intern Med 162, 55–63 (2015).
Moons, K. G. M. et al. Transparent reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann. Intern. Med. 162, W1–W73 (2015).
Lake, D. E., Fairchild, K. D., Kattwinkel, J. & Moorman, J. R. Reply to: Heart rate predicts sepsis. J. Pediatr. 161, 770–771 (2012).
CRAN - Package rms [Internet]. [cited 2022 Mar 15]. Available from: https://cran.r-project.org/web/packages/rms/index.html
Harrell F. E. rms: Regression Modeling Strategies. 2015;4.3-0.
Harrell F. E. rms: Regression Modeling Strategies. R package version 5.1-0.1. [Internet]. R package version 5.1-0.1. 2018 [cited 2022 Oct 17]. Available from: https://CRAN.R-project.org/package=rms
Harrell, F. E. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Cham: Springer International Publishing; 2015.
Srivastava N., Hinton G., Krizhevsky A. Dropout: a simple way to prevent neural networks from overfitting. J. Mach. 2014;15:1929–58.
LeCun, Y., Bengio, Y. & Hinton, G. Deep learning. Nature 521, 436–444 (2015).
Chen T., Guestrin C. XGBoost: A Scalable Tree Boosting System. Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining - KDD’ ‘ ’16. New York, New York, USA: ACM Press; 2016. p. 785–794.
Breiman L. Random Forests. Springer Science and Business Media LLC. 2001;
van Ravenswaaij-Arts, C. M., Hopman, J. C., Kollée, L. A., Stoelinga, G. B. & van Geijn, H. P. The influence of artificial ventilation on heart rate variability in very preterm infants. Pediatr. Res 37, 124–130 (1995).
Di Fiore, J. M., Poets, C. F., Gauda, E., Martin, R. J. & MacFarlane, P. Cardiorespiratory events in preterm infants: etiology and monitoring technologies. J. Perinatol. 36, 165–171 (2016).
Jean-Baptiste, N. et al. Coagulase-negative staphylococcal infections in the neonatal intensive care unit. Infect. Control Hosp. Epidemiol. 32, 679–686 (2011).
Cantey, J. B., Anderson, K. R., Kalagiri, R. R. & Mallett, L. H. Morbidity and mortality of coagulase-negative staphylococcal sepsis in very-low-birth-weight infants. World J. Pediatr. 14, 269–273 (2018).
Downey, L. C., Smith, P. B. & Benjamin, D. K. Risk factors and prevention of late-onset sepsis in premature infants. Early Hum. Dev. 86, 7–12 (2010). Suppl 1.
Dong, Y. & Speer, C. P. Late-onset neonatal sepsis: recent developments. Arch. Dis. Child Fetal Neonatal Ed. 100, F257–F263 (2015).
Sullivan, B. A. & Fairchild, K. D. Predictive monitoring for sepsis and necrotizing enterocolitis to prevent shock. Semin Fetal Neonatal Med 20, 255–261 (2015).
Lake, D. E., Fairchild, K. D. & Moorman, J. R. Complex signals bioinformatics: evaluation of heart rate characteristics monitoring as a novel risk marker for neonatal sepsis. J. Clin. Monit. Comput 28, 329–339 (2014).
Griffin, M. P. & Moorman, J. R. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics 107, 97–104 (2001).
Lake, D. E., Griffin, M. P. & Moorman, J. R. New mathematical thinking about fetal heart rate characteristics. Pediatr. Res 53, 889–890 (2003).
Moorman, J. R. The principles of whole-hospital predictive analytics monitoring for clinical medicine originated in the neonatal ICU. npj Digital Med. 5, 41 (2022).
Fairchild, K. D. & Lake, D. E. Cross-correlation of heart rate and oxygen saturation in very low birthweight infants: association with apnea and adverse events. Am. J. Perinatol. 35, 463–469 (2018).
Zimmet A. M. et al. Vital sign metrics of VLBW infants in three NICUs: implications for predictive algorithms. Pediatr Res. 90, 125–130 (2021).
Song, W. et al. A predictive model based on machine learning for the early detection of late-onset neonatal sepsis: development and observational study. JMIR Med. Inf. 8, e15965 (2020).
Masino, A. J. et al. Machine learning models for early sepsis recognition in the neonatal intensive care unit using readily available electronic health record data. PLoS One 14, e0212665 (2019).
Joshi, R. et al. A ballistographic approach for continuous and non-obtrusive monitoring of movement in neonates. IEEE J. Transl. Eng. Health Med 6, 2700809 (2018).
Mani, S. et al. Medical decision support using machine learning for early detection of late-onset neonatal sepsis. J. Am. Med Inf. Assoc. 21, 326–336 (2014).
Griffin, M. P., Lake, D. E. & Moorman, J. R. Heart rate characteristics and laboratory tests in neonatal sepsis. Pediatrics 115, 937–941 (2005).
Griffin, M. P., Lake, D. E., O’Shea, T. M. & Moorman, J. R. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr. Res. 61, 222–227 (2007).
Sullivan, B. A. & Fairchild, K. D. Vital signs as physiomarkers of neonatal sepsis. Pediatr. Res. 91, 273–282 (2022).
Monfredi O. J. et al. Continuous ECG monitoring should be the heart of bedside AI-based predictive analytics monitoring for early detection of clinical deterioration. J Electrocardiol. 76, 35–38 (2022).
Henry, C. J. et al. Neonatal sepsis: a systematic review of core outcomes from randomised clinical trials. Pediatr. Res. 91, 735–742 (2022).
Hayes R. et al. Neonatal sepsis definitions from randomised clinical trials. Pediatr Res. 2021. https://doi.org/10.1038/s41390-021-01749-3 Epub ahead of print.
McGovern, M. et al. Challenges in developing a consensus definition of neonatal sepsis. Pediatr. Res 88, 14–26 (2020).
Funding
We acknowledge the following grants for funding the work presented in this manuscript: K23 HD097254 [PI: B Sullivan]; R01 HD092071 [Co-PIs KD Fairchild & JR Moorman, Co-I DE Lake] K23NS111086 [PI: Z Vesoulis].
Author information
Authors and Affiliations
Contributions
S.L.K., B.S., K.F., D.L., R.S., Z.V., and J.R.M. have made substantial contributions to the conception or design of the work; S.L.K., J.Q., J.B., A.P., A.B., and J.I. made substantial contributions to the acquisition, analysis, or interpretation of data; SK and BS drafted the work and all other authors have substantively revised it. All authors have approved the submitted version. All authors have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
Some authors have financial conflicts of interest. J.R.M. and D.E.L. own stock in Medical Prediction Sciences Corporation. J.R.M. is a consultant for Nihon Kohden Digital Health Solutions. Z.A.V. is a consultant for Medtronic. All other authors have no financial conflicts to disclose. No authors have any non-financial conflicts of interest to disclose.
Consent statement
This study was approved by the IRB at each site with waiver of consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kausch, S.L., Brandberg, J.G., Qiu, J. et al. Cardiorespiratory signature of neonatal sepsis: development and validation of prediction models in 3 NICUs. Pediatr Res 93, 1913–1921 (2023). https://doi.org/10.1038/s41390-022-02444-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02444-7
This article is cited by
-
Transforming neonatal care with artificial intelligence: challenges, ethical consideration, and opportunities
Journal of Perinatology (2024)