Abstract
Background
Metabolic regulation plays a significant role in energy homeostasis, and adolescence is a crucial life stage for the development of cardiometabolic disease (CMD). This study aims to investigate the genetic determinants of metabolic biomarkers—adiponectin, leptin, ghrelin, and orexin—and their associations with CMD risk factors.
Methods
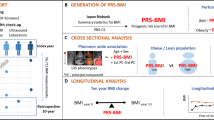
We characterized the genetic determinants of the biomarkers among Hispanic/Latino adolescents of the Santiago Longitudinal Study (SLS) and identified the cumulative effects of genetic variants on adiponectin and leptin using biomarker polygenic risk scores (PRS). We further investigated the direct and indirect effect of the biomarker PRS on downstream body fat percent (BF%) and glycemic traits using structural equation modeling.
Results
We identified putatively novel genetic variants associated with the metabolic biomarkers. A substantial amount of biomarker variance was explained by SLS-specific PRS, and the prediction was improved by including the putatively novel loci. Fasting blood insulin and insulin resistance were associated with PRS for adiponectin, leptin, and ghrelin, and BF% was associated with PRS for adiponectin and leptin. We found evidence of substantial mediation of these associations by the biomarker levels.
Conclusions
The genetic underpinnings of metabolic biomarkers can affect the early development of CMD, partly mediated by the biomarkers.
Impact
-
This study characterized the genetic underpinnings of four metabolic hormones and investigated their potential influence on adiposity and insulin biology among Hispanic/Latino adolescents.
-
Fasting blood insulin and insulin resistance were associated with polygenic risk score (PRS) for adiponectin, leptin, and ghrelin, with evidence of some degree of mediation by the biomarker levels. Body fat percent (BF%) was also associated with PRS for adiponectin and leptin. This provides important insight on biological mechanisms underlying early metabolic dysfunction and reveals candidates for prevention efforts.
-
Our findings also highlight the importance of ancestrally diverse populations to facilitate valid studies of the genetic architecture of metabolic biomarker levels.
Similar content being viewed by others
Introduction
Obesity in early life and subsequent cardiometabolic disease (CMD) is a major public health concern. In 2015–2016 in the US, 1 out of 5 adolescents aged 12–19 years were affected by obesity1 with a prevalence of 25.8% among self-identified Hispanic/Latino (H/L) youth (aged 2–19 years) compared to 14.1% among non-Hispanic white youth.1 Such alarming data are not restricted to the US H/L population, as many self-identified H/L populations in South and Central America are also suffering. For example, Chilean citizens also suffer from an increasing burden of obesity due to the epidemiological and nutritional transition that began in the 1980s.2,3
Energy homeostasis is particularly critical in obesity biology4 since its related hormones play significant roles in balancing energy expenditure and energy intake by exchanging physiological information between the central nervous system and other parts of the body.4,5 In this regard, appetite-related metabolic hormones function as signaling molecules, and malfunction of this system may interrupt energy homeostasis and consequently contribute to the development of obesity.
Four such metabolic hormones—adiponectin, leptin, ghrelin, and orexin—are involved in diverse cardiometabolic pathways. Adiponectin is well known for its protective roles in appetite regulation, energy metabolism, diabetes, and inflammation.6 Leptin shows anorexigenic and proinflammatory roles; individuals with obesity tend to have higher levels of circulating leptin together with leptin resistance.7 Ghrelin is an appetite-stimulating gut hormone that has been associated with glucose metabolism, which is closely linked to diabetes.8,9,10,11 Orexin is a hypothalamic neuropeptide that regulates feeding behaviors and arousal status12,13,14 and is ubiquitously expressed in different body sites,15 including plasma.16
There is a paucity of information on the genetic determinants of metabolic biomarkers, particularly among adolescents and in H/L. Such work is critical as H/L have continental ancestry and admixture that is different than that found in European populations. Moreover, the inter-relations among the genetic underpinnings of metabolic biomarkers, phenotypic variability, and downstream CMD risk factors (e.g., body fat percent (BF%) and insulin resistance (IR)) among adolescents have also been understudied. Previous studies have revealed that some obesity-associated genetic factors are associated with appetite regulation17,18 and Mendelian randomization studies have suggested causal relationships between metabolic biomarkers and CMD risk factors. However, studies focusing on the mediating roles of metabolic biomarkers in the relationship between the genetic underpinnings of metabolic biomarkers and CMD risk factors are lacking.
We sought to address these important gaps in the literature by first describing the known and novel large-effect genetic determinants of the four metabolic biomarkers among H/L adolescents (Fig. S1) and second by assessing the influence of aggregated genetic contributions to each biomarker by constructing polygenic risk scores (PRS) based on both known and novel genetic loci. Lastly, we aimed to investigate the relationship between the aggregated effects of biomarker-influencing genetic factors on obesity and glycemic traits and to estimate the degree to which this association is mediated by these biomarker levels. Investigating these relationships among adolescents with a high burden of obesity could provide critical insight into the biological mechanisms of obesity and downstream CMD during adolescence.
Methods
Study population
The Santiago Longitudinal Study (SLS) originally began as a preventive trial for infancy iron deficiency anemia, funded by National Institutes of Health (NIH-R01 HD014122).19 From 1991 to 1996, a total of 1792 infants were recruited at community clinics in lower-/middle-class neighborhoods in Santiago, Chile. Inclusion criteria for the infancy study were term singleton birth, vaginal delivery, birth weight ≥3 kg, and absence of major perinatal health problems.19 Follow-up studies occurred at 5, 10, and 16 years and included anthropometric measurement, psychosocial data, and developmental assessments.20,21 At 16 years, 679 adolescents completed a study of risk for obesity and CMD that targeted participants with the most comprehensive data in childhood. Data collected included anthropometric measures, cardiovascular risk, and metabolic biomarkers from fasting blood samples and self-reported health-related behaviors. Complete phenotype and genotype data were available for 543 (80%) of these participants. The study was reviewed and approved or found to be exempt by Institutional Review Boards of the University of California at San Diego, University of Michigan, University of North Carolina at Chapel Hill, and the Institute of Nutrition and Food Technology, University of Chile.
Genetic data and quality control
Participants were genotyped on the Illumina Multiethnic Genotyping Array with imputation to the 1000 Genomes Phase III AMR reference panel. Quality control included individual call rate of >90%, assessment of sex mismatch, relatedness, and ancestry outliers. Single-nucleotide polymorphisms (SNPs) with effect allele frequency <0.05, indels, and imputation quality score <0.5 were excluded, resulting in ~6 million SNPs that were assessed for their association with the biomarkers.
Measurement
Metabolic biomarkers
Fasting blood samples were obtained, stored at −80 °C, and analyzed. Enzyme-linked immunosorbent assay was used to measure adiponectin and leptin levels (R&D Systems, Minneapolis, MN and DRG International, Inc., New Jersey, NJ, respectively). The radioimmunoassay (RIA) technique was utilized to quantify ghrelin and orexin-A levels (Phoenix Pharmaceuticals, Inc., Burlingame CA).
BF%
Dual energy x-ray absorptiometry scan was used to measure body fat mass (Lunar Prodigy Corp. Software: Lunar iDXA ENCORE 2011, Version 13.60.033, Madison, WI). BF% was calculated as [100 (%) × fat mass (kg)/total body mass (kg)].
Glycemic traits
From overnight fasting blood, glucose and insulin levels were quantified with an enzymatic colorimetric assay (QCA S.A., Amposta, Spain) and RIA (RIA DCP Diagnostic Products Corporation, LA), respectively. In addition, IR was assessed based on continuous measure of homeostatic model assessment of insulin resistance (HOMA-IR; calculated as [(glucose (mg/dL) × insulin (μUI/dL))/405]; a value of HOMA-IR ≥ 2.6 can be diagnosed as IR).22
Analytical approach
Genome-wide association tests
We regressed four metabolic biomarkers on SNPs using SUGEN,23 assuming an additive genetic model and adjusting for sex and population substructure using the first five principal components (PCs). PCs were constructed by EIGENSTRAT24 using genetic information of the participants. Serum adiponectin, ghrelin, and orexin levels were natural log-transformed before regression analyses. Due to a detection limit issue in measuring leptin levels, rank-based normalized residuals of a Tobit regression model adjusting for sex were used in the genome-wide association analyses for leptin levels. To correct for multiple testing, we considered SNPs with p value <5 × 10−8 as demonstrating genome-wide significance and those with a p value <5 × 10−6 as demonstrating suggestive significance. We identified putative novel loci and reported the lead SNP from all 1 MB regions of the genome-wide significant and/or suggestive significant associations where no previous GWAS signal had been reported.
Validation of the genome-wide association study (GWAS) findings
For adiponectin and leptin levels, we investigated whether the SNPs identified from SLS demonstrated similar associations in a separate Mexican American validation data set (see Supplementary Material for more information). We considered a signal to be validated if the same SNP was associated with the metabolic biomarker level at a Bonferroni-corrected significance level (p < 0.05/the number of SNPs tested for validation for each biomarker) with directional consistency.
Functional interrogation of putative novel signals
Among the validated SNPs, we interrogated the potential candidate genes in each locus, selected based on (1) the evidence of functional link to a genetic locus (SNP) and (2) the previous reports on plausible gene functions. To examine the functional connection between a SNP and a gene, we queried the expression quantitative trait loci (eQTLs) from NIH Genotype-Tissue Expression (GTEx) project25 and biologically plausible gene functions using databases such as PubMed (https://pubmed.ncbi.nlm.nih.gov/), Online Mendelian Inheritance in Man (https://www.ncbi.nlm.nih.gov/omim), and GeneCards (https://www.genecards.org/).
Transferability of known associations
We described the transferability of known associations for adiponectin and leptin in SLS, defined when the association was reported with the exact SNP at nominal statistical significance (p < 0.05) and directional consistency. As of 15 December 2020, there were 48 and 15 previously reported SNPs associated with adiponectin and leptin, respectively, at the genome-wide significance level. There were no previously reported SNPs associated with ghrelin or orexin levels at genome-wide significance.
Constructing PRS of adiponectin and leptin based on known and putative novel loci
Given our small sample size and our desire to assess the evidence of mediated effects of genetic variants for these biomarkers on obesity and glycemic traits, we assessed the aggregated effects of previously reported genetic loci for adiponectin and leptin levels by constructing PRS. Since the previously reported SNPs were tag SNPs primarily identified in the studies of Europeans, we considered three different approaches to PRS construction: (1) PRS constructed only by the previously reported SNPs (PRSReported), (2) PRS constructed by the SLS-specific tagging SNPs of the known loci (i.e., the lowest p value within +/−500 kb of the previously reported SNPs) (PRSSLS), and (3) PRS constructed by both SLS-specific previous signals and putatively novel signals from the current study (PRSSLS + Novel). PRSReported was calculated by summing the number of biomarker-increasing alleles of the previously reported SNPs. If there were more than two SNPs in linkage disequilibrium (LD) (AMR r2 > 0.2), we only included one tag SNP that was directionally consistent and had the lowest p value among directionally consistent SNPs. If any of them were not directionally consistent, we included the SNP with the lowest p value. PRSSLS was defined as the number of biomarker-increasing alleles of the SLS-specific SNPs with the lowest p values from the current study among variants within +/−500 kb of the known SNPs. When we observed correlated SLS-specific SNPs (AMR r2 > 0.2), we only included the SNP with the lower p value for the association with the biomarker. PRSSLS + Novel was derived by summing up the PRSSLS and the number of biomarker-increasing alleles of the SNPs with genome-wide significance or suggestive significance from the current study.
Investigating the associations between the adiponectin and leptin levels and the constructed PRS for the biomarker in the H/L population
We evaluated the aggregated genetic effects on adiponectin and leptin levels among SLS by regressing each biomarker (for adiponectin, ghrelin, and orexin, natural log-transformed values; for leptin, rank-based inverse normalized residuals of a Tobit regression adjusting for sex) on each PRS assuming a linear relationship and assessing prediction model by comparing R2 (or adjusted R2 for the models with covariates). Specifically, we compared four separate models for each biomarker as follows: a model only including PRS of the biomarker (Model 1), a model additionally including sex as a covariate (Model 2), a model additionally including the first five PCs as covariates (Model 3), and a model additionally including the body mass index (BMI) Z-score (Model 4).
Investigating the relationship between the aggregated effects of biomarker-influencing genetic factors on BF% and glycemic traits
Adjusting for sex and the first five PCs, we estimated the total effect of the metabolic biomarker PRS on BF% and glycemic traits (fasting blood glucose (FBG), fasting blood insulin (FBI), and IR) and the percent mediated through the biomarker levels using causal mediation analysis (PROC CAUSALMED) in SAS 9.4 (SAS Institute Inc., Cary, NC).26,27 The proposed pathways, both direct and indirect, from PRS to BF% and glycemic traits are shown in Fig. S2. For adiponectin and leptin levels, all three types of PRS were investigated; for ghrelin and orexin levels, only those suggestive signals identified in the GWAS herein were used. All pathways, including those to the biomarker and those to the cardiometabolic trait, were adjusted for sex and the first five PCs. To further account for the potential heterogeneities by sex, sex-stratified sensitivity analyses were conducted. In each stratified analysis, age and the first five PCs were included as covariates. For leptin, rank-based inverse normalized residuals of leptin from a Tobit regression adjusting for age were included as mediator. And for the other biomarkers, natural log-transformed biomarker levels were used as mediators. Statistical significance was determined using Bonferroni-corrected p values. The results of sex-stratified analyses were presented in Tables S12–15.
Results
Descriptive statistics
Table 1 reports the descriptive statistics from the 543 SLS participants (259 females) included in the current analyses. The average levels of adiponectin, leptin, ghrelin, and orexin were 11.3 μg/mL (SD: 5.3), 11.7 ng/mL (SD:13.5), 239.6 pg/mL (SD: 151.0), and 16.7 pg/mL (SD: 4.2), respectively. The descriptive characteristics of the validation sample are shown in Table S1.
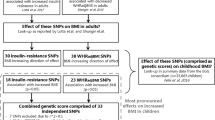
Identification of novel signals
No SNP–metabolic biomarker associations displayed genome-wide statistically significant evidence of association. However, 8, 5, 13, and 8 loci displayed suggestive associations with adiponectin, leptin, ghrelin, and orexin, respectively. The lead SNPs, nearest genes, and corresponding p values for adiponectin, leptin, ghrelin, and orexin are reported in Table 2.
Validation of putative novel signals
Ten of the 13 adiponectin- or leptin-associated SNPs were available in the validation set. Of the examined genetic markers for validation (6 for adiponectin and 4 for leptin), only the marker rs12066716 was found to be significantly associated (Bonferroni-corrected p < 0.00625 (=0.05/8)) with adiponectin with directional consistency [β(±SE) in the discovery set: −0.181 ± 0.039, β(±SE) in the validation set: −0.191 ± 0.065]. Seven signals for adiponectin and leptin levels were directionally consistent but not statistically significant (Table S2).
Functional interrogation of putative novel signals
For our validated adiponectin-associated SNP (rs12066716), we identified a candidate gene demonstrating both functional links to an index SNP and plausible biological functions in determining adiponectin level. The index SNP (rs12066716) is an eQTL for C1QTNF12 (C1q/TNF-related protein 12, CTRP12) in visceral adipose tissue (p for eQTL = 8.1 × 10−5) (https://www.gtexportal.org/home/snp/rs12066716). CTRPs, including CTRP12 (the product of C1QTNF12), are a family of adiponectin paralogs,28,29,30 thus the association between the gene and adiponectin is highly feasible.
Transferability of known associations
For adiponectin, a total of 48 different SNPs have been reported for association with adiponectin from 11 studies,31,32,33,34,35,36,37,38,39,40,41 44 of which were available in the current study (Table S3). Thirty-five of these 44 SNPs displayed directionally consistent associations with adiponectin levels, 8 of which displayed nominal statistical significance (p < 0.05). Fifteen variants have been associated with leptin levels with genome-wide significance from 3 studies42,43,44; 13 of these variants were available in the current study (Table S4). Six of these 13 associations were directionally consistent, but none were nominally significant (p < 0.05).
Aggregated genetic influence on adiponectin and leptin levels
Adiponectin
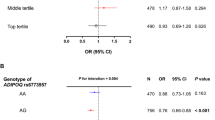
As some of the 44 available known SNPs are in LD with one another, we selected 29 independent SNPs (AMR LD r2 < 0.2) and constructed PRSReported for adiponectin (Table S5). We also identified 24 independent SLS-specific tagging SNPs in the known loci by selecting the SNPs with lowest p value for the association with adiponectin levels within +/−500 kb of the reported SNPs (Table S7). All the 24 SLS-specific tagging SNPs were independent of each known SNP (AMR LD r2 < 0.2). Using these 24 SLS-specific tagging SNPs for the known loci, we generated PRSSLS. Lastly, we additionally summed up the number of adiponectin-increasing alleles of the eight putative novel variants from the PRSSLS and generated adiponectin PRSSLS + Novel. The prediction results of the natural log-transformed adiponectin levels by PRS are reported in Table 3. While the proportion of variance explained by PRSReported was 0.035, the proportion of variance explained by PRSSLS was 0.253 (Table 3). We further estimated the proportion of variance explained by PRSSLS + Novel from the current study as 0.367. While the estimated variance explained is likely to be biased upward because of winner’s curse, it is obvious that the SLS-specific tagging SNPs better characterized the genetic effects of these loci on this biomarker (also below for leptin) for our SLS population.45
Leptin
Among the 13 available known SNPs, we selected 7 independent SNPs (AMR LD r2 < 0.2) and constructed PRSReported for leptin levels (Table S6). We also identified 8 SLS-specific tagging SNPs of the known loci—i.e., SNPs with the lowest p values within +/−500 kb of the known variant—and constructed PRSSLS for leptin levels (Table S8). All the 8 SLS-specific tagging SNPs are independent of the known SNPs (AMR LD r2 < 0.2). Then we summed up the number of leptin-increasing alleles of the five putative novel variants from the PRSSLS and calculated PRSSLS + Novel. We predicted the rank-based normalized residuals of Tobit regressed leptin level (sex as an explanatory variable) by using the three PRS (Table 3). Whereas the variance explained by PRSReported was 0.001 (and the regression coefficient was not significant with a significance level of 0.05), the variance explained by PRSSLS was 0.082 and by PRSSLS + Novel was 0.206 (Table 3). It is possible that the R2 for leptin was lower than for adiponectin partly due to fewer previous GWAS of leptin than of adiponectin.
Effects of the biomarker-associated genetic determinants on downstream BF% and glycemic traits
Adiponectin
FBI (p = 0.0037), IR (p = 0.0064) and BF% (p < 0.0001) were significantly associated with PRSSLS + Novel (Table 4). For FBI and IR, significant indirect effects (i.e., mediated through adiponectin levels) were noted. The mediated effects of adiponectin PRSSLS + Novel on FBI and IR accounted for 79.0% (95% confidence limit (CL): 2.4, 155.5; p = 0.04) and 83.2% (95% CL: −0.5, 166.8; p = 0.05) of the overall effects, respectively. For BF%, we also found evidence of mediation, but the proportion of mediated effects over the total effects was only 46.7% (95% CL: 2.4, 90.9; p = 0.04). Given the wide confidence interval (CI) of these estimates, point estimate should be interpreted with caution. In terms of direction of effects, both directly and indirectly the adiponectin-increasing effects appeared to be metabolically protective (decrease in FBI, IR, and BF%). For PRSSLS, the total effects on FBI and BF% were estimated as being significant as for PRSSLS + Novel, but for PRSReported, none of them was significantly affected by the PRS (Table S9).
Leptin
FBI (p = 0.0014), IR (p = 0.0043), and BF% (p < 0.0001) were significantly affected by the leptin PRSSLS + Novel (Table 4). The total effect of leptin-increasing PRS was associated with poorer metabolic outcomes (i.e., increase in FBI, IR, and BF%). For FBI and IR, the estimate of the direct effect of PRS on leptin was negative and the estimate of the indirect effect of PRS on the CMD health outcome through leptin was positive. Therefore, the indirect pathway through leptin accounted for most of this association between FBI and IR. For BF%, where both direct and indirect associations were positive, the proportion of mediated effects was 96.9% (95% CL: 65.2, 128.5; p < 0.01). For PRSSLS, only the total effect on BF% was significant (also associated with worse metabolic outcomes); none of the hypothetical downstream BF% and glycemic traits were significantly associated with PRSReported (Table S10). According to the results from sex-stratified analyses, the total effects of leptin PRSSLS + Novel on FBI and IR are largely driven by females; however, the indirect effects mediated through leptin are comparable—in terms of direction, magnitude, and significance—among females and males (Table S13).
Ghrelin
FBI (p < 0.0001) and IR (p < 0.0001) were significantly affected by the ghrelin PRS based on the putative novel variants from the current study (Table 4) with ghrelin-increasing PRS associated with overall decreases in IR. As with leptin, we found differences in the direction of the association between direct and indirect effects. Higher PRS were indirectly related with lower FBG (−0.223 [95% CI: (−0.286, −0.161)]) and IR (−0.232 [95% CI: (−0.295, −0.169)]), and the total association was similar in magnitude even after accounting for the direct effects.
Orexin
None of the cardiometabolic traits were affected by the orexin-increasing PRS (Table 4).
Discussion
The identification of genetic mechanisms influencing metabolic biomarkers has the potential to identify important pathways for obesity and its downstream consequences. Yet, the bulk of obesity research has focused on how genes relate to BMI and waist circumference, instead of on relationships with eating behaviors and/or mechanistic biomarkers, which may have early influences on the development of obesity, through appetite for example. Further still, most extant data have primarily focused on homogeneous middle-aged adults, with very few genetic studies on culturally and ancestrally diverse adolescents. The current study identified 34 suggestive novel genetic signals associated with 4 metabolic biomarkers and validated 1 novel signal associated with adiponectin level. In addition, we revealed that associations between biomarkers and aggregated genetic effects based on known variants were improved when study-specific tag SNPs for known loci and novel variants were included in the PRS. This implicates the need for ancestry-specific studies to validly capture aggregated genetic effects across populations. Lastly, we demonstrated that metabolic biomarker-influencing genetic factors were also associated with some CMD risk factors, especially with FBI and IR (for adiponectin, leptin, and ghrelin) and BF% (for adiponectin and leptin), implicating causal roles of these biomarkers in obesity and IR as early as adolescence.
Although our study did not demonstrate novel genome-wide significant signals for appetite markers, likely due to insufficient power, 34 putative novel signals with suggestive evidence for association with metabolic biomarkers were mapped, with the rs12066716 adiponectin association validated in a H/L adult population (p < 0.00625) despite the age differences between the two study populations. While the SNP is intronic to TTL10, it is associated with gene expression in several other nearby genes in adipose tissue. Notably, rs12066716 is an eQTL for C1QTNF12, which encodes CTRP12 (also called adipolin), a member of the family of adiponectin paralogs.28,30,46,47 CTRP12 improves insulin sensitivity29 and has been shown to correlate with adiponectin levels (r = 0.34).48 In addition, CTRP12 levels are currently being evaluated as a diagnostic biomarker for T2D.49 Finally, other studies have demonstrated that CTRP12 levels were lower among patients with coronary artery disease.48
We found that little to none of the variance in adiponectin and leptin levels were explained by PRS based on the exact reported SNPs from the literature, likely due to the ancestral difference between our population (i.e., mainly European vs. H/L) and published studies. Once we substituted SLS-specific tagging SNPs of the known loci for the reported SNPs, the prediction performance of the PRS improved substantially (R2 from 0.035 to 0.253 for adiponectin and from 0.001 to 0.082 for leptin). We conducted permutation testing to place our adiponectin PRSSLS findings in context. We randomly selected 24 SNPs among all SNPs that displayed significant association (p < 0.05) with adiponectin in our GWAS. We then constructed the PRS (the number of risk alleles) from each these SNPs and calculated the R-square values from each model. Repeating this simulation 1000 times, we observed the distribution of R-square values (maximum: 0.220; range: 0.125–0.220; Fig. S4). All R-square values were of smaller magnitude than our adiponectin PRSSLS estimate (0.253). Thus, our results demonstrate that the proportion of variation explained by adiponectin PRSSLS was greater than chance, likely an overestimation as well. This finding demonstrates the need for valid ancestry-specific tagging SNPs for PRS. Furthermore, since we identified additional improvement of PRS’ performance after incorporating the putative novel signals, large-scale studies for diverse populations to discover additional genetic loci associated with metabolic biomarker are warranted. However, it should be noted that the predictions by PRSSLS and PRSSLS + Novel were likely to be overestimated because of the overlap between the discovery set of the associations and the validation set for the association. Nonetheless, as illustrated in our previous study,45 the current findings also underscore the importance of considering genetic diversity across different cohorts and the influence of this diversity on unique underpinnings to disease in future application of PRS to diverse ethnic groups.50
For adiponectin, leptin, and ghrelin, PRS of biomarkers were simultaneously associated with FBI, IR, and BF% (except for ghrelin) among H/L adolescents. These common associations may suggest shared genetic pathways, at least to a certain degree, between metabolic biomarkers and CMD as early as adolescence. Many of the significant overall effects included significant mediated effect by metabolic biomarkers (FBI, IR, and BF% for leptin and adiponectin, and FBI and IR for ghrelin), and this implies that each metabolic biomarker might be somewhere on the causal pathways from the biomarker-determining genetic factors to the CMD risk factors—i.e., the metabolic biomarkers are causally associated with the CMD risk factors—if our assumption on the hypothetical causal relationship (see Fig. S2) is valid. Notably, FBI and IR are closely associated with PRS for adiponectin, leptin, and ghrelin through indirect effects. Since IR is considered a root cause of various CMD,51 it is crucial to elucidate the roles of these metabolic biomarkers in developing IR. For the significant mediated effects on BF% for adiponectin and leptin, our findings also suggest an early causal effect of adiponectin and leptin on body fat, suggesting an importance of these biomarkers for the development of obesity at a very young age. Such findings may have relevance for the timing of planning interventions.
The observed significant indirect effects on FBI, IR, and BF% support the protective roles of adiponectin in cardiometabolic health. While inverse associations of plasma adiponectin with IR and adiposity have been well established,52,53 the findings from Mendelian randomization studies to assess the causal relationships between adiponectin and IR (or insulin sensitivity) and between adiponectin and BMI have been contradictory54,55,56,57,57 or unsupported.58. Although our analysis has not formally assessed causal relationships between these biomarkers, our data support a potential influence of adiponectin on FBI, IR, and BF% by the presence of significant indirect effects of adiponectin-associated genetic factors mediated by adiponectin levels. In addition, for BF%, the effect sizes of the direct (β = −0.072 despite not meeting the significance criteria; p = 0.084) and indirect effect (β = −0.063, p = 0.018) were comparable. This implies the presence of other pathways from the adiponectin-associated genes to BF% independent of adiponectin. Further studies investigating potential common pathways shared between BF% and adiponectin levels are needed.
For the downstream effect of leptin-influencing genetic variants on adiposity, a previous study reported that a leptin-decreasing allele (rs17151919-A) was associated with higher BMI during early childhood (under 8 years).44 However, our results demonstrated that leptin-increasing PRS were associated with higher BF%. Such results may be understood in the context of distinct leptin effects across the life course and in the context of poor cardiometabolic health. Although leptin typically inhibits appetite and increases energy expenditure,59 individuals with poor cardiometabolic health tend to have higher circulating leptin levels due to low leptin sensitivity60—i.e., leptin resistance. Since the previous study and our results focused on early childhood and late adolescence, respectively, the opposite direction of the association between leptin-influencing genetic variants and adiposity might have been driven by the development of leptin resistance.
For ghrelin, similar patterns with adiponectin were demonstrated except for BF%. This implicates the potential protective roles of circulating ghrelin in cardiometabolic traits especially for insulin biology. In line with this finding, many previous studies including a meta-analysis61 on the association between ghrelin and IR in obesity reported the negative correlation among people with obesity. Thus, our study adds to the body of literature that supports ghrelin’s role in glucose metabolism, but the mechanisms by which circulating ghrelin levels play roles in regulating insulin sensitivity need to be further studied.
Overall, as previously reported,18 our results contribute to the mechanistic evidence that obesity-associated genetic determinants can affect adiposity through appetite-related homeostasis systems. Together with the evidence of the longitudinal relationship between impaired satiety regulations and subsequent weight gain,62,63,64 the current findings also imply the importance of individuals’ genetic susceptibility to appetite-related metabolic homeostasis in risk of obesity in the current obesogenic environment, as previously suggested.18
The major strength of this study is the availability of four metabolic biomarkers in an adolescent H/L population at high risk for obesity and downstream CMD. In particular, genome-wide studies of ghrelin and orexin are rare. For adiponectin and leptin, we also leveraged the known information from the previous studies to assess the aggregated genetic effects. Lastly, we extensively investigated cross-trait associations of biomarker-influencing genetic loci with other CMD risk factors. There are notable limitations to our study, including the modest sample size and the lack of availability of studies to replicate our findings. Nine out of 10 putative novel signals for adiponectin and leptin level were not replicated from the validation data set, which could be related to the distinct admixture patterns across Mexican Americans and Chileans, the differences in age across the data sets, or small sample sizes. In addition, PRSSLS and PRSSLS + Novel may have overestimated the aggregated genetic effects and cross-trait associations with BF%, FBI, and IR. Furthermore, as analyses were conducted cross-sectionally, it is difficult to determine temporality among traits, e.g., metabolic biomarkers and cardiometabolic traits, and the possibilities of reverse causation between biomarker level and cardiometabolic traits.
In conclusion, our study identified several putatively novel genetic variants associated with the metabolic biomarkers with substantial phenotypic variance explained by SLS-specific PRS. We also demonstrated that some of the aggregated genetic factors may be directly linked to BF%, FBI, and IR or mediated through metabolic biomarkers. Our findings reinforce a need for longitudinal analyses to confirm the genetic determinants regulating metabolic homeostasis and their further influence on cardiometabolic disorder development. From a public health standpoint, such findings are critical, as once cardiometabolic health is established in adolescence, it is very difficult to reverse. Thus, findings from this study yielded important information on biological mechanisms and candidates for prevention efforts, especially relevant in this high-risk ancestrally diverse population.
References
Hales, C. M., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief 1–8 (2017).
Albala, C., Vio, F., Kain, J. & Uauy, R. Nutrition transition in Chile: determinants and consequences. Public Health Nutr. 5, 123–128 (2002).
Muzzo, S., Burrows, R., Cordero, J. & Ramirez, I. Trends in nutritional status and stature among school-age children in Chile. Nutrition 20, 867–872 (2004).
Ghanemi, A., Yoshioka, M. & St-Amand, J. Broken energy homeostasis and obesity pathogenesis: the surrounding concepts. J. Clin. Med. 7, 453–453 (2018).
Richard, D. Cognitive and autonomic determinants of energy homeostasis in obesity. Nat. Rev. Endocrinol. 11, 489–501 (2015).
Nigro, E. et al. New insight into adiponectin role in obesity and obesity-related diseases. Biomed. Res. Int. 2014, 658913 (2014).
Abella, V. et al. Leptin in the interplay of inflammation, metabolism and immune system disorders. Nat. Rev. Rheumatol. 13, 100–109 (2017).
Chabot, F., Caron, A., Laplante, M. & St-Pierre, D. H. Interrelationships between ghrelin, insulin and glucose homeostasis: physiological relevance. World J. Diabetes 5, 328–341 (2014).
Gray, S. M., Page, L. C. & Tong, J. Ghrelin regulation of glucose metabolism. J. Neuroendocrinol. 31, e12705 (2019).
Klok, M. D., Jakobsdottir, S. & Drent, M. L. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes. Rev. 8, 21–34 (2007).
Poher, A. L., Tschöp, M. H. & Müller, T. D. Ghrelin regulation of glucose metabolism. Peptides 100, 236–242 (2018).
Ebrahim, I. O., Howard, R. S., Kopelman, M. D., Sharief, M. K. & Williams, A. J. The hypocretin/orexin system. J. R. Soc. Med. 95, 227–230 (2002).
Lin, L. et al. The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene. Cell 98, 365–376 (1999).
Sakurai, T. et al. Orexins and orexin receptors: a family of hypothalamic neuropeptides and G protein-coupled receptors that regulate feeding behavior. Cell 92, 573–585 (1998).
Heinonen, M. V., Purhonen, A. K., Makela, K. A. & Herzig, K. H. Functions of orexins in peripheral tissues. Acta Physiol 192, 471–485 (2008).
Arihara, Z. et al. Immunoreactive orexin-A in human plasma. Peptides 22, 139–142 (2001).
Cecil, J. E., Tavendale, R., Watt, P., Hetherington, M. M. & Palmer, C. N. An obesity-associated FTO gene variant and increased energy intake in children. N. Engl. J. Med. 359, 2558–2566 (2008).
Llewellyn, C. H., Trzaskowski, M., van Jaarsveld, C. H. M., Plomin, R. & Wardle, J. Satiety mechanisms in genetic risk of obesity. JAMA Pediatr. 168, 338–344 (2014).
Lozoff, B. et al. Behavioral and developmental effects of preventing iron-deficiency anemia in healthy full-term infants. Pediatrics 112, 846–854 (2003).
East, P. et al. Infant iron deficiency, child affect, and maternal unresponsiveness: testing the long-term effects of functional isolation. Dev. Psychol. 53, 2233–2244 (2017).
Pacheco, L. S. et al. Early onset obesity and risk of metabolic syndrome among Chilean adolescents. Prev. Chronic Dis. 14, E93 (2017).
Burrows, R. et al. Healthy Chilean adolescents with HOMA-IR >=2.6 have increased cardiometabolic risk: association with genetic, biological, and environmental factors. J. Diabetes Res. 2015, 783296 (2015).
Lin, D. Y. et al. Genetic association analysis under complex survey sampling: the Hispanic Community Health Study/Study of Latinos. Am. J. Hum. Genet. 95, 675–688 (2014).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909 (2006).
Consortium, G. T. The Genotype-Tissue Expression (GTEx) project. Nat. Genet. 45, 580–585 (2013).
VanderWeele, T. J. Explanation in Causal Inference: Methods for Mediation and Interaction (Oxford University Press, 2015).
VanderWeele, T. J. & Vansteelandt, S. Conceptual issues concerning mediation, interventions and composition. Stat. Interface 2, 457–468 (2009).
Enomoto, T. et al. Adipolin/C1qdc2/CTRP12 protein functions as an adipokine that improves glucose metabolism. J. Biol. Chem. 286, 34552–34558 (2011).
Wei, Z. et al. C1q/TNF-related protein-12 (CTRP12), a novel adipokine that improves insulin sensitivity and glycemic control in mouse models of obesity and diabetes. J. Biol. Chem. 287, 10301–10315 (2012).
Wong, G. W., Wang, J., Hug, C., Tsao, T. S. & Lodish, H. F. A family of Acrp30/adiponectin structural and functional paralogs. Proc. Natl Acad. Sci. USA 101, 10302–10307 (2004).
Chung, C. M. et al. A genome-wide association study reveals a quantitative trait locus of adiponectin on CDH13 that predicts cardiometabolic outcomes. Diabetes 60, 2417–2423 (2011).
Heid, I. M. et al. Clear detection of ADIPOQ locus as the major gene for plasma adiponectin: results of genome-wide association analyses including 4659 European individuals. Atherosclerosis 208, 412–420 (2010).
Morisaki, H. et al. CDH13 gene coding T-cadherin influences variations in plasma adiponectin levels in the Japanese population. Hum. Mutat. 33, 402–410 (2012).
Spracklen, C. N. et al. Exome-derived adiponectin-associated variants implicate obesity and lipid biology. Am. J. Hum. Genet. 105, 15–28 (2019).
Wu, Y. et al. A meta-analysis of genome-wide association studies for adiponectin levels in East Asians identifies a novel locus near WDR11-FGFR2. Hum. Mol. Genet. 23, 1108–1119 (2014).
Dastani, Z. et al. Novel loci for adiponectin levels and their influence on type 2 diabetes and metabolic traits: a multi-ethnic meta-analysis of 45,891 individuals. PLoS Genet. 8, e1002607 (2012).
Qi, L. et al. Novel locus FER is associated with serum HMW adiponectin levels. Diabetes 60, 2197–2201 (2011).
Jee, S. H. et al. Adiponectin concentrations: a genome-wide association study. Am. J. Hum. Genet. 87, 545–552 (2010).
Wu, Y. et al. Genome-wide association study for adiponectin levels in Filipino women identifies CDH13 and a novel uncommon haplotype at KNG1-ADIPOQ. Hum. Mol. Genet. 19, 4955–4964 (2010).
Richards, J. B. et al. A genome-wide association study reveals variants in ARL15 that influence adiponectin levels. PLoS Genet. 5, e1000768 (2009).
Ling, H. et al. Genome-wide linkage and association analyses to identify genes influencing adiponectin levels: the GEMS Study. Obesity 17, 737–744 (2009).
Folkersen, L. et al. Genomic and drug target evaluation of 90 cardiovascular proteins in 30,931 individuals. Nat. Metab. 2, 1135–1148 (2020).
Kilpelainen, T. O. et al. Genome-wide meta-analysis uncovers novel loci influencing circulating leptin levels. Nat. Commun. 7, 10494 (2016).
Yaghootkar, H. et al. Genetic studies of leptin concentrations implicate leptin in the regulation of early adiposity. Diabetes 69, 2806–2818 (2020).
Justice, A. E. et al. Genetic determinants of BMI from early childhood to adolescence: the Santiago Longitudinal Study. Pediatr. Obes. 14, e12479 (2019).
Sargolzaei, J., Chamani, E., Kazemi, T., Fallah, S. & Soori, H. The role of adiponectin and adipolin as anti-inflammatory adipokines in the formation of macrophage foam cells and their association with cardiovascular diseases. Clin. Biochem. 54, 1–10 (2018).
Schaffler, A. & Buechler, C. CTRP family: linking immunity to metabolism. Trends Endocrinol. Metab. 23, 194–204 (2012).
Fadaei, R. et al. Decreased serum levels of CTRP12/adipolin in patients with coronary artery disease in relation to inflammatory cytokines and insulin resistance. Cytokine 113, 326–331 (2019).
Bai, B. et al. Circulating C1q complement/TNF-related protein (CTRP) 1, CTRP9, CTRP12 and CTRP13 concentrations in Type 2 diabetes mellitus: In vivo regulation by glucose. PLoS ONE 12, e0172271 (2017).
Carlson, C. S. et al. Generalization and dilution of association results from European GWAS in populations of non-European ancestry: the PAGE study. PLoS Biol. 11, e1001661 (2013).
Ginsberg, H. N. Insulin resistance and cardiovascular disease. J. Clin. Investig. 106, 453–458 (2000).
Arita, Y. et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. 1999. Biochem. Biophys. Res. Commun. 425, 560–564 (2012).
Tilg, H. & Moschen, A. R. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat. Rev. Immunol. 6, 772–783 (2006).
Borges, M. C. et al. Metabolic profiling of adiponectin levels in adults: Mendelian randomization analysis. Circ. Cardiovasc. Genet. 10, e001837 (2017).
Yaghootkar, H. et al. Mendelian randomization studies do not support a causal role for reduced circulating adiponectin levels in insulin resistance and type 2 diabetes. Diabetes 62, 3589–3598 (2013).
Mente, A. et al. Causal relationship between adiponectin and metabolic traits: a Mendelian randomization study in a multiethnic population. PLoS ONE 8, e66808 (2013).
Gao, H. et al. Evidence of a causal relationship between adiponectin levels and insulin sensitivity: a Mendelian randomization study. Diabetes 62, 1338–1344 (2013).
Nielsen, M. B., Colak, Y., Benn, M. & Nordestgaard, B. G. Causal relationship between plasma adiponectin and body mass index: one- and two-sample bidirectional Mendelian randomization analyses in 460,397 individuals. Clin. Chem. https://doi.org/10.1093/clinchem/hvaa227 (2020).
Farooqi, I. S. et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N. Engl. J. Med. 341, 879–884 (1999).
Myers, M. G., Cowley, M. A. & Munzberg, H. Mechanisms of leptin action and leptin resistance. Annu. Rev. Physiol. 70, 537–556 (2008).
Zhang, C. S. et al. The correlation between circulating ghrelin and insulin resistance in obesity: a meta-analysis. Front. Physiol. 9, 1308 (2018).
van Jaarsveld, C. H., Boniface, D., Llewellyn, C. H. & Wardle, J. Appetite and growth: a longitudinal sibling analysis. JAMA Pediatr. 168, 345–350 (2014).
van Jaarsveld, C. H., Llewellyn, C. H., Johnson, L. & Wardle, J. Prospective associations between appetitive traits and weight gain in infancy. Am. J. Clin. Nutr. 94, 1562–1567 (2011).
Parkinson, K. N., Drewett, R. F., Le Couteur, A. S., Adamson, A. J. & Gateshead Milennium Study Core Team. Do maternal ratings of appetite in infants predict later Child Eating Behaviour Questionnaire scores and body mass index? Appetite 54, 186–190 (2010).
Acknowledgements
We thank the participants of the Santiago Longitudinal Study, the San Antonio Family Heart Study and the San Antonio Family Diabetes/Gallbladder Study for their continued cooperation and participation in our research programs.
Funding
This work was funded in part by University of North Carolina Nutrition Research Institute internal pilot grant, AHA grant 15GRNT25880008, and NIH award K99/R00HL130580-02. We thank the participants and their family members from the Santiago Longitudinal Study (SLS) (R01 HL088530, R01 HD33487). K.E.N. is additionally supported by R01HL151152 and R01 DK122503. Work for the validation study was supported in part by National Institutes of Health (NIH) grants P01 HL045522, R01 DK047482, DK053889, R01 HL113323, R37 MH059490, and T2D-GENES Consortium grants (U01 DK085524, U01 DK085584, U01 DK085501, U01 DK085526, and U01 DK085545).
Author information
Authors and Affiliations
Contributions
D.K. and K.E.N. designed the study and drafted the initial manuscript; E.B. and R.B. collected the data; A.E.J., G.C., M.G., and Y.W. carried out genetic data cleaning; D.K., M.G., A.G.H., Y.W., R.R., and V.L.B. conducted statistical analysis; M.A., J.P., D.M.L., J.E.C., A.G.C., R.D., and J.B. were involved in the validation study; D.K., K.E.N., M.G., A.G.H., A.E.J., and G.C. were involved in interpretation of the results; all authors revised the manuscript and contributed to the content and approved the submission and publication of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The research conducted herein constitutes an analysis of de-identified existing data and therefore is not considered human subject research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kim, D., Justice, A.E., Chittoor, G. et al. Genetic determinants of metabolic biomarkers and their associations with cardiometabolic traits in Hispanic/Latino adolescents. Pediatr Res 92, 563–571 (2022). https://doi.org/10.1038/s41390-021-01729-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01729-7