Abstract
Background
Difficulty in obtaining peripheral vascular access is a common problem in patients admitted to the pediatric intensive care unit (PICU). The use of ultrasound guidance can improve the overall success in obtaining vascular access. This study evaluated the success and longevity of PIV placement by nurses pre- and post-implementation of an USGPIV curriculum.
Methods
PICU nurses participated in a prospective quality improvement study. Each participating nurse attempted 10 PIVs by using landmark (LM) methods. The same nurses then received individual instruction in an USGPIV placement curriculum. Following the educational intervention, each nurse attempted 10 USGPIVs.
Results
A total of 150 LM PIVs and 143 USGPIVs were attempted. The first stick success in the post-intervention (USGPIV) group was 85.9% compared to 47.3% in the pre-intervention (LM) group (p < 0.001). Overall success was also superior in the USGPIV group (94.3 versus 57.3%, respectively; p < 0.001). PIVs placed by US lasted longer with a median survival time of 4 ± 3.84 days versus 3 ± 3.51 days for LM PIVs (p < 0.050, log-rank test).
Conclusions
Successful implementation of a standardized curriculum for USGPIV placement for PICU nurses improves first stick, overall success, and longevity of PIV catheter placement.
Impact
-
An ultrasound-guided IV curriculum can be successfully implemented resulting in increased first stick success and increased longevity.
-
Registered nurses can be trained in placement of ultrasound-guided IV placement.
-
This study provides a training curriculum for ultrasound-guided IV placement that can be applied to other settings or institutions.
Similar content being viewed by others
Introduction
Peripheral intravenous (PIV) access is arguably the most commonly performed invasive procedure in a hospital. However, the procedure may be challenging in some patients, particularly in children. In children, obtaining intravenous access is often complicated by smaller vascular architecture and limited patient cooperation. It may pose an even more significant challenge in children with a history of difficult intravenous access.
Traditionally, landmarks (LMs) and palpation methods are used to place an IV. At times, placement of an IV can be challenging even for the most experienced providers causing treatment delays, patient discomfort, and at times inability to secure an IV at all. Success rates in obtaining PIVs in pediatric patients by traditional LMs are variable and range from 50 to 90% in the experienced provider cohort. Success rates are even lower (44–50%) for inexperienced providers.1,2,3 Frey evaluated the success of PIV placement in children and reported an overall success rate of 44% for staff nurses. The success rate for physicians was even lower at 23%.1 Lininger’s study also evaluated the success rate of PIV placement in children by nurses. Medical/surgical nurses with variable years of experience placed most of the PIVs in this study.2 The first stick success in this cohort with self-reported data was similar to the previous study with 53% success on first attempt, which improved to 67% with two attempts. Higher success rates have been reported in experienced nurses placing PIVs. Friedland and Brown cited first attempt success ranging from 73 to 86% in a cohort of experienced nurses with >5 years of experience in obtaining vascular access.4
The improvement in efficacy and safety of ultrasound (US)-guided central venous cannulation and the endorsement of this modality by multiple patient safety organizations has led to the growing interest and demand for US guidance for PIV (USGPIV) placement.5,6 It improves first attempt and overall success of placement, decreases mean number of attempts needed for successful cannulation, and increases longevity with fewer complications in pediatric patients in the emergency department.7,8,9,10 However, the widespread use of this useful skill is limited by the availability of educational curricula and their implementation. While educational curricula for USGPIV placement exist in the emergency department for nurses and physicians, there is a wide variability in the duration of training, implementation of the skill, and assessment of proficiency. Adhikari et al. described a simulation-based curriculum for 40 adult emergency department nurses.11 This 2-h curriculum consisted of didactic lectures followed by practical sessions. The nurses demonstrated proficiency at the end of the course by demonstrating successful PIV placement on the simulation model and a written test. Anderson et al. evaluated a similar educational curriculum in placing USGPIV in the pediatric emergency department.12 Their findings suggested that 9 USGPIVs are required to achieve competency.12 Thus, while USGPIV placement is a skill that can be acquired by nurses, training and credentialing pathways still need to be studied and established.
This quality improvement study was initiated to examine whether institution of an educational curriculum in USGPIV placement in the pediatric intensive care unit (PICU) could improve procedural success and catheter longevity. The hypothesis was that implementation of an USGPIV placement program in the PICU would improve first stick success and longevity of PIV placement when US guidance was used. The primary outcomes measured were first stick and overall success of PIV placement. The secondary outcomes measured were longevity of PIVs placed and adoption of this technique by the staff.
Methods
This prospective quality improvement study was completed at a 30-bed quaternary medical and surgical academic PICU. The Institute for Healthcare Improvement’s model for improvement was used to guide this initiative.13 Plan Do Study Act (PDSA) cycles were used to plan and study the effects of the intervention. One PICU faculty, fellow, and advanced practice provider facile in US education, along with the vascular access team, nursing leadership, and the PICU nursing educator, assessed causes of underutilization of USGPIV placement and analyzed contributing factors via a fishbone diagram as shown in Fig. 1. Five primary causes were identified as most problematic and amendable to intervention, including lack of an educational curriculum and workflow to train nurses in USGPIV placement, lack of nurse US education, lack of established competency guidelines for USGPIV placement for nurses, the high cost of nursing education time, and the process for documenting PIV placement was not rigorous. In this PICU, bedside nurses place PIVs. The bedside nurses are limited to no more than two attempts at PIV placement per patient, with support from a vascular access team comprised of nurses specializing in vascular access with and without US when initial attempts fail. We performed the PDSA cycle in four phases.
In Phase 1 (Plan), a volunteer cohort of PICU nurses was enrolled on a first-come-first-serve basis for PIV placement. A pre-intervention survey was completed to understand the practice pattern of nurses in regard to PIV placement (Table 1A). Data were collected on pre-intervention (LM) PIV insertions between April and December 2018 using the hospital electronic medical record (EMR), Epic (Epic Systems Corporation, Verona, WI). Information documented in the EMR included placement date, time, provider placing the catheter, size of the catheter, side and site, number of insertion attempts, number of providers attempted, and PIV technique used. PIV removal date, time, and reason were collected separately using catheter device data in the EMR. During this phase, each nurse was required to attempt placement of ten PIVs using the LM method. An attempt was defined as a needle entry through the skin with or without blood return. If needle redirections were made without taking out the needle, then it was still considered as the same attempt. Successful placement was defined by the ability to secure and flush the IV without any resistance or blanching of the skin. The choice of size of catheter, type of catheter, and site of placement were at the discretion of the operator in both groups. B-Braun (B. Braun Medical Inc., Bethlehem, PA) and Becton Dickinson (Becton, Dickinson and Company, Franklin Lakes, NJ) PIV catheters are routinely used in this PICU. Catheters of different sizes (16–24 G) are available to the nurses. However, only traditional catheters <1.25” in length are available to them. Longer catheters are available to the institution’s vascular access team but not to the PICU nurses.
During this phase, the number of PIVs attempted by the study nursing group per week was lower than that expected and email reminders were sent weekly to participating nurses. To increase PIV placement opportunities for nurses participating in the study, reminders were made twice daily in the PICU nursing huddle to notify participating nurses if PIV access was needed. Participating nurses were reminded weekly via email to ensure data collection forms were complete when missing data were noted during this phase.
In Phase 2 (Do), the same nurses then individually participated in an USGPIV placement training curriculum that involved a 1-h presentation and hands-on US practice using a vessel simulator. The training team for USGPIV placement consisted of a senior fellow with dual training in pediatric critical care medicine and US (V.B.), a nurse practitioner with extensive experience in placement of USGPIVs (D.D.), and the vascular access team with a minimum experience of 6 months in USGPIV and US-guided peripherally inserted central catheter (PICC) placement. One of the members of the training team proctored nurses until successful placement of 5 USGPIVs. Each nurse was then required to further attempt placement and document ten USGPIVs. The training curriculum discussed:
Operation of machine
This included discussion of basic US physics, including optimization of depth and gain, positioning of machine such that it was placed across from the operator in direct line of sight, and the appropriate disinfection of the probes and machines prior to use.
Transducer selection and orientation
This included selection of a linear-array probe and the correct method of holding the probe. Orientation of the probe marker and screen marker in the same direction were discussed.
Recognition of vessels
Recognition of vessels was by using compressibility and color Doppler. Vessel evaluation for thrombi and patency and confirmation of PIV after placement were discussed.
Techniques
Short axis view of the vessel was used with dynamic placement of the needle as follows: (1) the vessel is identified with the US probe in short axis view, (2) the needle is advanced through the skin and identified as a bright echogenic spot under the US, and (3) the probe and needle are then advanced simultaneously or one after the other to always maintain visualization of the needle tip. Complete insertion of PIVs to the hub under real-time US guidance was recommended (Fig. 2).
The vessel is identified with the ultrasound probe (blue arrow) in short axis view. The needle (red line) is advanced through the skin and identified as a bright echogenic spot under the ultrasound. The probe and needle are then advanced simultaneously or one after the other to always maintain visualization of the needle tip.
The training was performed on a Sonosite X-Porte US machine (Fujifilm-Sonosite; Bellevue, WA) using a L25x/13-6 MHz linear array transducer. The nurses were encouraged to avoid utilizing larger vessels above the elbow and below the knee that are reserved for PICC placement by the institution’s vascular access team. During this phase, it was realized that there is a substantial opportunity cost for the nursing time required to complete this training. The training was deemed a professional development opportunity, and ICU nursing leadership permitted use of their annual continuing medical education (CME) hours to undergo the training.
In Phase 3 (Study), the nurses placed USGPIVs and information was collected between December 2018 and September 2019. To capture the efficacy of the training curriculum, the primary outcome measured was the first stick success of PIV placement. A modest improvement of 10% in first stick success was estimated with the use of US guidance based on previous studies.7,8,14 Based on this estimated improvement with 80% power and 0.05 alpha, we performed sample size calculations and estimated 150 sticks per cohort. Secondary outcomes included overall success of placement, mean attempts per successful placement, and longevity of PIV placement, defined as median survival time (days). An anonymous post-intervention survey of the participating nurses was conducted to seek feedback on the USGPIV placement curriculum, and a self-reported assessment of the individual’s skills as well as intentions for future use of the new skill was also conducted.
The statistical analysis was performed using STATA version 12.1 (STATA Corp LLC, College Station, TX). Chi square test/Fischer’s exact test was used to compare categorical data, i.e., first stick success and overall success. Wilcoxon’s sum test was used to compare the mean number of attempts per successful placement. Kaplan–Meier survival analysis was used to compare longevity of PIVs placed.
Finally, in Phase 4 (Act) data collection and interpretation was completed. The results were shared with the PICU leadership and plans to establish competency pathway in future were discussed. The Stanford University Institutional Review Board waived their need for protocol given the quality improvement nature of the study, as both LM and USGPIV placement are validated modalities of securing IV access. The study results are reported in compliance with SQUIRE 2.0 framework.15
Results
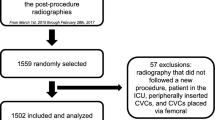
A time-line diagram (Fig. 3) depicts key steps in the implementation of this intervention during the study period. Two hundred and ninety-three sticks were attempted and reported (150 in the pre-intervention [LM] group and 143 in the post-intervention [USGPIV] group). The EMR captured data for all PIV placements; however, data for PIV removal was captured for 56% (84/150) of all PIVs in the LM group and 81% (116/143) in the USGPIV group. When evaluating the patient characteristics (Table 2), there were no significant differences in age, sex, the sites used for PIV placement, and the preferred gauge of needle used between the LM and USGPIV groups. There were 53% (80/150) males in the LM group with a median age of 9.2 ± 6.9 years compared to 55% (79/143) males in the USGPIV group with a median age of 9.8 ± 6.8 years. In all, 5% (8/150) patients in the LM group and 12% (18/143) patients in the USGPIV group were infants. The two most commonly used sites with the LM group were the hand (35%) and the foot (18%), compared to the forearm (58%) and the antecubital fossa (16%) with the USGPIV group. The 2 most commonly used sizes of IVs were 22 gauge (57%) and 24 gauge (29%) in the LM group compared with 22 gauge (56%) and 20 gauge (34%) in the USGPIV group.
The first stick success for LM method was 47.3%, which improved modestly to an overall success rate of 54% after second attempt (Table 3). The first stick success with the USGPIV method was 85.9%, which improved to 92.2% after second stick (p < 0.001). The mean number of attempts per successful placement in the two groups were also evaluated. A total of 106 attempts were made for 86 successful PIVs in the LM group with a mean of 1.23 ± 0.55 attempts per successful placement compared to a total of 145 attempts for 134 successful PIVs in the USGPIV group with a mean of 1.08 ± 0.35 attempts (p = 0.006). The PIVs placed with US guidance also lasted longer with a median survival time of 4 ± 3.84 versus 3 ± 3.51 days for the LM group (p = 0.009). A Kaplan–Meier PIV survival analysis curve (Fig. 4) showed a statistically significant difference between the two groups (p < 0.050, log-rank test). The infant subgroup in this study was small. In this subgroup, the first stick and overall success for LM method was 37%. The first stick success improved to 70.6% and the overall success improved to 76.5% using USGPIV placement. One of these infants required three attempts while the rest of the infants requires a single attempt for PIV placement. The median survival time in the LM group was 3.67 ± 2.89 days as compared to 4.73 ± 3.64 days in the USGPIV group.
Fifteen PICU nurses participated in and completed the study. The pre-intervention survey showed that the minimum clinical experience in the cohort was at least 2 years, with 71% of the nurses with >5 years of clinical experience. In all, 71% of the nurses reported placing <5 PIVs per week prior to starting the study, with 21% placing no PIVs per week. (Table 1A) None of the nurses enrolled in the study had previous experience with the use of US. All nurses enrolled in the study completed the training and successfully adopted the skill in their practice. The post-intervention survey was completed by 14/15 participating nurses. Table 1B summarizes the results of the post-intervention survey. The nurses were asked to rate the US course as below average, good, or excellent, with 57% of the cohort reporting the course to be excellent. None of the nurses reported the course to be below average. In all, 93% of the nurses self-reported their USGPIV skill placement to be good or excellent. Finally, majority of the cohort (79%) expressed that they would continue to use the USGPIV placement for all their future PIVs while the rest of the cohort expressed reserving the skill only for their difficult PIV placement.
Discussion
This study demonstrates that the institution of a training curriculum for USGPIV placement improves first stick and overall success for PIV placement as well as catheter longevity and that such a program can be successfully implemented in a PICU. None of the enrolled nurses had any previous US training but 100% of the cohort self-reported that they would adopt the use of USGPIV placement in their future practice.
The first stick and overall success of PIV placement improved significantly following implementation of USGPIV placement curriculum. While the overall success is similar to data previously reported by other studies,7,16,17 this study uniquely demonstrates the efficacy of a standardized nursing education program for USGPIV placement. One notable observation in this study was the higher rate of first stick success when compared to previous publications. Vinograd et al. reported a first stick success rate of 68% and an overall success rate of 91%, while Doniger et al. and Bahl et al. reported overall success rates of 80 and 76%, respectively, with USGPIV. This difference is potentially due to differences in patient population studied, proportion of difficult IV access patients, clinical setting in which these studies were performed (emergency room versus PICU), the US technology used, and USGPIV placement methodology could have also contributed to differences in first stick success in these studies.8 Interestingly, different findings were reported by Otani et al.18 in a study examining USGPIV placement in the pediatric emergency department. After one failed LM attempt, success in the USG (65%) group was significantly lower when compared to the LM technique (84%) (p = 0.002). Methodology for this study differed, however, from other published studies in that two individuals performed the USGPIV procedure, an US operator and the person inserting the PIV.
The higher first stick success in this study may be explained by multiple factors. First, all providers received similar training with emphasis on dynamic placement in the short axis and advancement of needle under direct US visualization until the catheter was inserted to the hub. Previously reported studies utilized a single operator, short axis (transverse) view, and dynamic technique of insertion. However, these studies do not specify whether the catheter was advanced under US guidance till it was completely at the hub.7,8 Many of the failed USGPIV attempts in this study were related to failure to advance needle under dynamic guidance until the catheter hub was at the skin. Second, while there is a lack of evidence regarding the superiority of a single operator versus dual operator technique,19 it is possible that following the needle tip visualization is easier for a single operator versus dual operators.
The mean attempts per successful cannulation was lower in the USGPIV group compared to the LM group. The improvement in first stick success and mean attempts in USGPIV placement are likely unrelated to skill improvement of placing ten PIVs over a period of several months, as nurses were placing PIVs at a similar frequency prior to starting the study.
The longevity of the PIVs placed by US guidance was longer than those placed by LM method (USGPIV = 4 days, LM = 3 days), which may be explained by placement of the USGPIVs in demonstrably patent and perhaps larger veins.20,21 While the study did not evaluate the depth of placement, the overall size of catheters placed by US guidance was larger compared to the LM method and likely were inserted in larger vessels.
A substantial number of patients admitted to PICUs are infants. We looked at this subgroup of patients separately. The improvement in first stick success, overall success, longevity of PIVs placed, and a decrease in the number of attempts per successful placement using USGPIV placement was also noted in the infant subgroup. However, the total number of patients in both the LM group and USGPIV infant subgroup was small. The nurses in the study were not restricted from attempting PIVs on any patient admitted to the PICU. Thus, the reason for low number of infants in the study is unclear.
The presence of providers with training and expertise in USGPIV placement allowed an opportunity for staff nurses to acquire and implement this skill in their practice. A lack of trained individuals may prevent the generalizability of this educational curriculum. We also learned that there was a significant opportunity cost associated with nursing time. The staff nurses at this institution receive annual CME hours that covered the cost of time required for training. Several staff nurses also volunteered their time to learn this new skill. Such educational opportunities may not be present at other institutions.
There are a few limitations to the study. Operators self-reported insertion data in the EMR and may have been biased by the perception that USGPIV placement is a more advanced technique; however, study resources for data collection by a separate observer were not available and bias may be present in either direction. Larger studies are necessary to further distill the results. The current study did not stratify patients based on the difficulty of their vascular access. However, this was maintained for both LM and USGPIV methods and is unlikely to have changed during the study period. US guidance was originally described as a rescue technique for patients with difficult vascular access and hence comparing the impact of a structured curriculum for USGPIV placement in patients with difficult vascular access is of interest for future studies. Lastly, the PIV removal data were not available from patient documentation for 44% of the patients in the LM group and 19% of the patients in the USGPIV group. In the remainder of the study population, we were unable to record whether the PIVs were removed due to device failure or planned removal, as these are not routinely documented in the EMR at the study institution.
Conclusion
The implementation of a standardized curriculum for USGPIV placement can improve first stick and overall success and longevity of peripherally inserted venous catheter placement. It can be successfully implemented in a PICU and enhances staff satisfaction through acquisition of a new skill. A 1-h standardized curriculum with a 5 PIV credentialing requirement was sufficient to establish this program. A standardized curriculum in USGPIV placement may be utilized in training other pediatric providers (physicians, nurse practitioners, residents) and in other clinical areas (acute care, the emergency department) in the future.
References
Frey, A. M. Success rates for peripheral i.v. insertion in a children’s hospital. Financial implications. J. Intraven. Nurs. 21, 160–165 (1998).
Lininger, R. A. Pediatric peripheral i.v. insertion success rates. Pediatr. Nurs. 29, 351–354 (2003).
Barton, A. J., Danek, G., Johns, P. & Coons, M. Improving patient outcomes through CQI: vascular access planning. J. Nurs. Care Qual. 13, 77–85 (1998).
Friedland, L. R. & Brown, R. Introduction of a “safety” intravenous catheter for use in an emergency department: a pediatric hospital’s experience. Infect. Control Hosp. Epidemiol. 13, 114–115 (1992).
The Joint Commission. Preventing Central Line–Associated Bloodstream Infections: A Global Challenge, a Global Perspective (Joint Commission Resources, 2012).
AHRQ. AHRQ quality indicators toolkit: selected best practices and suggestions for improvement. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/qitoolkit/d4a-crbsi-bestpractice.pdf (2017).
Vinograd, A. M., Zorc, J. J., Dean, A. J., Abbadessa, M. K. F. & Chen, A. E. First-attempt success, longevity, and complication rates of ultrasound-guided peripheral intravenous catheters in children. Pediatr. Emerg. Care 34, 376–380 (2018).
Bahl, A., Pandurangadu, A. V., Tucker, J. & Bagan, M. A randomized controlled trial assessing the use of ultrasound for nurse-performed IV placement in difficult access ED patients. Am. J. Emerg. Med. 34, 1950–1954 (2016).
Samoya, S. W. Real-time ultrasound-guided peripheral vascular access in pediatric patients. Anesth. Analg. 111, 823–825 (2010).
Triffterer, L. et al. Ultrasound-guided cannulation of the great saphenous vein at the ankle in infants. Br. J. Anaesth. 108, 290–294 (2012).
Adhikari, S., Schmier, C. & Marx, J. Focused simulation training: emergency department nurses’ confidence and comfort level in performing ultrasound-guided vascular access. J. Vasc. Access 16, 515–520 (2015).
Anderson, A. P. et al. Ultrasound guided peripheral IV placement: an observational study of the learning curve in pediatric patients. J. Vasc. Access https://doi.org/10.1177/1129729820987958 (2021).
Langley, G. L. et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (Jossey-Bass, 2009).
Kantor, D. B., Su, E., Mill;iren, C. E. & Conlon, T. W. Ultrasound guidance and other determinants of successful peripheral artery catheterization in critically ill children. Pediatr. Crit. Care Med. 17, 1124–1130 (2016).
Ogrinc, G., Davies, L., Goodman, D., Batalden, P., Davidoff, F. & Stevens, D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual. Saf. 25, 986–992 (2016).
Doniger, S. J., Ishimine, P., Fox, J. C. & Kanegaye, J. T. Randomized controlled trial of ultrasound-guided peripheral intravenous catheter placement versus traditional techniques in difficult-access pediatric patients. Pediatr. Emerg. Care 25, 154–159 (2009).
Avelar, A. F., Peterlini, M. A. & da Luz Goncalves Pedreira, M. Ultrasonography-guided peripheral intravenous access in children: a randomized controlled trial. J. Infus. Nurs. 38, 320–327 (2015).
Otani, T. et al. Ultrasound-guided peripheral intravenous access placement for children in the emergency department. Eur. J. Pediatr. 177, 1443–1449 (2018).
Milling, T., Holden, C., Melniker, L., Briggs, W. M., Birkhahn, R. & Gaeta, T. Randomized controlled trial of single-operator vs. two-operator ultrasound guidance for internal jugular central venous cannulation. Acad. Emerg. Med. 13, 245–247 (2006).
Panebianco, N. L., Fredette, J. M., Szyld, D., Sagalyn, E. B., Pines, J. M. & Dean, A. J. What you see (sonographically) is what you get: vein and patient characteristics associated with successful ultrasound-guided peripheral intravenous placement in patients with difficult access. Acad. Emerg. Med. 16, 1298–1303 (2009).
Witting, M. D., Schenkel, S. M., Lawner, B. J. & Euerle, B. D. Effects of vein width and depth on ultrasound-guided peripheral intravenous success rates. J. Emerg. Med. 39, 70–75 (2010).
Author information
Authors and Affiliations
Contributions
V.B. substantially contributed to study conception and design and acquisition, analysis, and interpretation of data. He was also involved in drafting and revising the article. E.S. substantially contributed to study conception and design and analysis and interpretation of data. He was also involved in revising the content and final approval of the version to be published. B.H. substantially contributed to analysis and interpretation of data. He was also involved in revising the content and final approval of the study manuscript. D.D. substantially contributed to acquisition of data. He was also involved in revising the content and final approval of the study manuscript. K.M.S. substantially contributed to study conception and design and analysis and interpretation of data. She was also involved in revising the content and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Patient consent was not required for the completion of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bhargava, V., Su, E., Haileselassie, B. et al. Ultrasound education improves safety for peripheral intravenous catheter insertion in critically ill children. Pediatr Res 91, 1057–1063 (2022). https://doi.org/10.1038/s41390-021-01568-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01568-6
This article is cited by
-
POCUS increases successful placement of peripheral arterial lines in neonates by less experienced providers
European Journal of Pediatrics (2023)
-
Point-of-Care Ultrasound-Guided Procedures in the Pediatric Cardiac Intensive Care Unit
Current Treatment Options in Pediatrics (2022)