Abstract
Background
The Neonatal Resuscitation Program (NRP) recommends using 100% O2 during chest compressions and adjusting FiO2 based on SpO2 after return of spontaneous circulation (ROSC). The optimal strategy for adjusting FiO2 is not known.
Methods
Twenty-five near-term lambs asphyxiated by umbilical cord occlusion to cardiac arrest were resuscitated per NRP. Following ROSC, lambs were randomized to gradual decrease versus abrupt wean to 21% O2 followed by FiO2 titration to achieve NRP SpO2 targets. Carotid blood flow and blood gases were monitored.
Results
Three minutes after ROSC, PaO2 was 229 ± 32 mmHg in gradual wean group compared to 57 ± 13 following abrupt wean to 21% O2 (p < 0.001). PaO2 remained high in the gradual wean group at 10 min after ROSC (110 ± 10 vs. 67 ± 12, p < 0.01) despite similar FiO2 (~0.3) in both groups. Cerebral O2 delivery (C-DO2) was higher above physiological range following ROSC with gradual wean (p < 0.05). Lower blood oxidized/reduced glutathione ratio (suggesting less oxidative stress) was observed with abrupt wean.
Conclusion
Weaning FiO2 abruptly to 0.21 with adjustment based on SpO2 prevents surge in PaO2 and C-DO2 and minimizes oxidative stress compared to gradual weaning from 100% O2 following ROSC. Clinical trials with neurodevelopmental outcomes comparing post-ROSC FiO2 weaning strategies are warranted.
Impact
-
In a lamb model of perinatal asphyxial cardiac arrest, abrupt weaning of inspired oxygen to 21% prevents excessive oxygen delivery to the brain and oxidative stress compared to gradual weaning from 100% oxygen following return of spontaneous circulation.
-
Clinical studies assessing neurodevelopmental outcomes comparing abrupt and gradual weaning of inspired oxygen after recovery from neonatal asphyxial arrest are warranted.
Similar content being viewed by others
Introduction
Asphyxiated newly born infants often require resuscitation immediately after birth.1,2 Cerebral ischemia and hypoxia during perinatal asphyxia initiates a cascade of deleterious biochemical events including a switch to anaerobic metabolism and secondary energy failure leading to neuronal death within hours to days after birth.3 Generation of reactive oxygen species at a rate that exceeds the capacity of the endogenous antioxidant systems to neutralize them results in oxidative stress and tissue damage.4 The developing brain is extremely vulnerable to free radical damage due to its lipid content, relatively high oxygen (O2) consumption, and low activity of antioxidant enzymes.5,6 Previous studies have shown that brief exposure to 100% O2 increases brain tissue O2 tension,7 systemic oxidative stress and lung oxidative injury in ventilated term newborn lambs.8 Furthermore, the combination of perinatal asphyxia and early hyperoxemia is associated with higher incidence of moderate to severe hypoxic ischemic encephalopathy (HIE).9 Approximately half of the infants with severe HIE are at risk for death or moderate to severe disability even in the era of therapeutic hypothermia.10,11 Newborn infants who undergo intensive resuscitation and survive are at significant risk for neurodisability.12 Minimizing the risk of reperfusion injury with post-resuscitation hyperoxia13 may potentially be associated with short-term and long-term reduction in mortality and morbidity.
The American Academy of Pediatrics/American Heart Association (AAP/AHA) Neonatal Resuscitation Program (NRP) provides guidance for preductal O2 saturations (SpO2) during resuscitation.14 The Textbook of Neonatal Resuscitation recommends 100% O2 use during chest compressions (CC).14,15 The 2020 American Heart Association—Neonatal Resuscitation guidelines suggest that it is reasonable to use higher concentrations of O2 when CC are needed.16 Due to poor perfusion during cardiac arrest in spite of CC, PaO2 concentrations are very low (23.9 ± 6.8 mmHg with 100% O2) in animal studies.17 Moreover, it is clinically difficult to reliably monitor oxygenation status with pulse oximetry while delivering CC. After return of spontaneous circulation (ROSC) and heart rate is above 60 bpm, inspired O2 is adjusted to meet target SpO2 to reduce the risks associated with hyperoxia.16 This recommendation is based on expert opinion and is not based on scientific evidence. Inspired O2 can be weaned gradually from 100% or abruptly to 21% and then titrated based on preductal SpO2.
We hypothesized that abrupt weaning of inspired O2 to 21% after ROSC will prevent a surge in cerebral O2 delivery (C-DO2), minimize oxygen toxicity, and reduce oxidative stress as measured by oxidized to reduced glutathione (GSSG/GSH) ratio in whole blood samples compared to gradual weaning from 100% O2 with titration based on preductal SpO2 ranges recommended by NRP.
Methods
Animal preparation
The study protocol was approved by the Institutional Animal Care and Use Committee (IACUC) at the University of California, Davis. All experiments were performed according to animal ethical guidelines, in compliance with the ARRIVE guidelines.18 Time-dated healthy pregnant ewes at near-term gestation (139–141 days gestation; term is 145 days) were procured from Van Laningham Farm, Arbuckle, CA, USA. Following an overnight fast, the ewe was medicated with intravenous diazepam and ketamine, and intubated with a 10.0 mm cuffed endotracheal tube (ETT). The ewe was ventilated with 21% O2 and general anesthesia was provided with 2–3% inhaled isoflurane as previously described.19 The ewe was continuously monitored with a pulse oximeter and an end-tidal CO2 (ETCO2) monitor. Following a cesarean section, the fetal lamb was partially exteriorized and intubated with a 4.5 mm cuffed ETT. After draining the fetal lung fluid passively by gravity, the ETT was occluded to prevent entry of air. A left carotid arterial flow probe was placed to measure blood flow. A catheter was placed in the right carotid artery for invasive arterial blood pressure monitoring and to collect blood samples. The right jugular vein was catheterized for blood draws and for fluid and medication administration respectively. A pulse oximeter was placed on the right forelimb for continuous SpO2 monitoring.
Experimental protocol
The umbilical cord was occluded until asystole when the lamb’s heart rate was zero and the carotid arterial pressure and flow waveforms were absent. The umbilical cord was then tied and cut. The lamb was transferred to a radiant warmer and weighed and a three-lead EKG applied. After 5 min of asystole, resuscitation was initiated with positive pressure ventilation (PPV) using peak inflation pressures (PIPs) of 30–35 cm H2O and PEEP of 5 cm H2O with a rate of 40 breaths/min and 21% O2 via a T-piece resuscitator.19 After 30 s of effective PPV through the ETT, CC were initiated and coordinated with PPV (3:1 ratio of CC:PPV) and the inspired O2 was increased to 100%.16 In the lambs that did not achieve ROSC with CC and PPV, a dose of epinephrine (0.01–0.03 mg/kg) was administered intravenously by umbilical venous route at 3–5 min from the onset of resuscitation.1,20 Epinephrine administration at the same dose was repeated every 3 min until ROSC or for a total of four doses. ROSC was defined as sustained heart rate greater than 100 bpm and systolic arterial blood pressure more than 40 mmHg. Following ROSC, the lambs were randomized into two groups using opaque sealed envelopes:
Gradual wean (control) group
After ROSC, inspired O2 was weaned down from 100% O2 by 5% if preductal SpO2 was 96–98% and by 10% if SpO2 was ≥99% every 30 s as needed to maintain preductal SpO2 within NRP recommended ranges (85–95%).
Abrupt decrease to 21% O2/abrupt wean (experimental) group
Following ROSC, the inspired O2 was abruptly weaned to 21% from 100%. Subsequently inspired O2 was titrated up from 21% by 5% if preductal SpO2 was 80–84% or by 10% if SpO2 was <80% every 30 s as needed to maintain preductal SpO2 within 85–95%.
Monitoring
The lambs were placed on a conventional ventilator with settings adjusted to maintain PaCO2 between 45 and 55 mmHg. Ventilator settings during the study period were PIP of 25–35 cm H2O, PEEP of 5 cm H2O, and rate of 30–40/min, targeting exhaled tidal volume of 6–8 ml/kg/min in both the groups. Carotid arterial blood flow and SpO2 were continuously monitored until 30 min after ROSC. Arterial blood gas samples were collected at fetal baseline, during cardiac arrest at the start of PPV, during CC, immediately after ROSC, every minute after ROSC for the first 5 min, and at 10, 15, and 30 min after ROSC. Venous blood gases were obtained at fetal baseline, during cardiac arrest, during CC, immediately after ROSC, and at 1, 2, 5, and 10 min after ROSC, respectively. Each sample of blood drawn was replaced with equal volume of normal saline as flush. Arterial blood samples were obtained at fetal baseline and at 10 min after ROSC to measure the ratio of oxidized to reduced glutathione (GSSG:GSH ratio) in whole blood per manufacturer’s instructions (Glutathione colorimetric detection kit, InvitrogenTM, Thermo Fisher Scientific, MA USA) as a measure of oxidative stress.
Cerebral O2 delivery and cerebral O2 consumption (extraction) were calculated at various time points during resuscitation and after ROSC, as shown below:
C-DO2 (ml/kg/min) = Qca × [(1.39 × Hb × SaO2/100) + (PaO2 × 0.003)]
Cerebral O2 consumption (ml/kg/min), cerebral AV-DO2 = [carotid arterial O2 content (CaO2)−jugular venous O2 content (CvO2)] × Qca = [1.39 × Hb × (SaO2 − SvO2)/100] × Qca
where Qca is the carotid arterial blood flow (ml/kg/min); Hb the hemoglobin concentration (g/dl); SaO2 the carotid arterial O2 saturation (%); SvO2 the jugular venous O2 saturation (%); and PaO2 the partial pressure of O2 in carotid arterial blood (mmHg).
Sample size calculation
Sample size was calculated for the primary outcome of C-DO2. Based on published and pilot data from our laboratory, C-DO2 in lambs 15–30 min after birth was normally distributed with standard deviation of 0.9 ml/kg/min.21 If the true difference in the experimental and control means was 1.25 ml/kg/min, we needed a total of 24 lambs with 12 lambs in each group to be able to reject the null hypothesis that the population means of C-DO2 in the experimental groups (abrupt wean) and control (gradual wean) groups are equal with a probability (power) of 0.9. The Type I error probability associated with this test of null hypothesis is 0.05.
Data collection and analysis
Hemodynamic variables were continuously monitored and recorded using a computer with data acquisition software (BIOPAC systems, Goleta, CA, USA). Continuous variables are expressed as mean and standard deviation (SD). Categorical variables are analyzed using χ2 test with Fisher’s exact test as required. Continuous variables are analyzed by ANOVA repeated measures between groups with Fisher’s post hoc test within groups. Paired t-test was used to compare the whole blood oxidized and reduced glutathione and the ratio between the fetal baseline and at 10 min after ROSC. Unpaired t-test was used to compare the difference between GSSG/GSH ratio, GSSG, and GSH concentrations at fetal baseline and at 10 min after ROSC, between the two study groups. Statview 5.0.1 (SAS institute Inc., New York) was used for statistical analysis. Statistical significance was defined as p < 0.05.
Results
Perinatal asphyxial arrest was induced by umbilical cord occlusion in 25 lambs. The lambs were resuscitated as per AHA Neonatal Resuscitation guidelines. All lambs achieved ROSC and were included in data analysis. Following ROSC, as per randomization, 12 lambs underwent gradual wean and 13 lambs had their FiO2 abruptly weaned to 0.21. Characteristics of these lambs, including birth weight, sex, baseline hemodynamic parameters, and arterial blood gas analyses were similar between the groups at fetal baseline and during cardiac arrest (Table 1). The time to cardiac arrest was also similar between groups. One lamb in each group achieved ROSC without epinephrine. Eight out of 12 lambs in the gradual-wean group and 11/13 lambs in the abrupt-wean group received epinephrine at 0.03 mg/kg, and the remainder of lambs in each group received 0.01 mg/kg. The mean (SD) of inspired O2 concentration that was provided during resuscitation and after ROSC was significantly different between the two groups by design (Fig. 1). There was no statistically significant difference in the left carotid arterial blood flow at fetal baseline, during resuscitation, and after ROSC between the two groups (Fig. 2).
Blood gas analyses
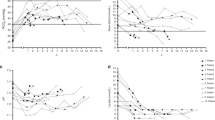
The arterial PaO2 was significantly higher with gradual wean compared to abrupt wean during the 1–10 min period following ROSC (p < 0.05, Fig. 3a). Mean PaO2 values were more than 200 mmHg within a few minutes after ROSC and remained greater than 100 mmHg at 10 min after ROSC with gradual weaning. With abrupt weaning to 21% O2, mean preductal PaO2 remained stable and less than 100 mmHg from 1 to 10 min after ROSC (Fig. 3a). Arterial hemoglobin O2 saturation (SaO2) measured by blood gas analysis was significantly higher with gradual wean compared to abrupt wean between 1 and 4 min after ROSC (p < 0.05, Fig. 3b). Jugular venous partial pressure of O2 (PvO2) and venous hemoglobin O2 saturation (SvO2) obtained from venous blood gases were not different in the two weaning strategies (Figs. 4a and 4b respectively). Preductal arterial partial pressure of carbon dioxide (PaCO2) was not different between gradual and abrupt wean strategies (Fig. 5).
Preductal arterial partial pressure of O2 (PaO2, a) and arterial hemoglobin O2 saturation (SaO2, b) obtained from serial blood gases in gradual wean and abrupt wean groups. These values were significantly higher with gradual wean compared to abrupt wean following ROSC. *p < 0.01, p < 0.05 by ANOVA repeated measures. Data presented as mean and SEM.
Cerebral oxygen delivery and cerebral oxygen consumption
Cerebral O2 delivery during CC was low compared to baseline (0.03 ± 0.06 vs. 0.07 ± 0.10 ml/kg/min) despite 100% inspired O2 in both groups (Fig. 6). The first blood gas and C-DO2 measurement obtained immediately after ROSC were similar between the two weaning strategies. However, during the 1–15 min period after ROSC, the C-DO2 was higher and above the physiological range (in healthy term newborn lambs: median [interquartile range] of 2.6 [1.98–3.55] ml/kg/min) with gradual wean compared to abrupt wean (Fig. 6). The range of C-DO2 in healthy term lambs was obtained from unpublished historical data from our laboratory. These values are similar to published data from asphyxiated lambs with meconium aspiration syndrome targeted to maintain preductal SpO2 of 85–95%.21 In contrast, the C-DO2 was more stable and within the physiological range with abrupt weaning to 21% O2. Cerebral AV-DO2 was not different between the two groups following ROSC (0.71 ± 0.32 vs. 0.47 ± 0.05 ml/dl with gradual wean and abrupt wean, respectively, at 5 min after ROSC).
Cerebral oxygen delivery (C-DO2) was significantly higher with gradual wean compared to abrupt wean, potentially resulting in cerebral hyperoxia from supra-physiological C-DO2. Data represented as mean and SEM. *p < 0.01, □ p < 0.05 by ANOVA repeated measures. ROSC return of spontaneous circulation. The median (interquartile range) for C-DO2 in normal term lambs breathing room air is shown by the shaded area (median = 2.6 ml/kg/min; IQR −1.98 to 3.55 ml/kg/min).
Effect on glutathione metabolism
The GSSG/GSH ratio and oxidized glutathione (GSSG) concentration in whole blood samples were significantly lower at 10 min following ROSC compared to fetal baseline with abrupt weaning to 21% O2 (Table 2). The concentration of reduced glutathione (GSH) was significantly lower with gradual weaning from 100% O2 at 10 min after ROSC compared to fetal baseline.
Discussion
The Textbook of Neonatal Resuscitation suggests increasing inspired O2 concentration to 100% when CC are started.14 Once heart rate is greater than 60 bpm, and a reliable SpO2 signal is achieved, adjusting the oxygen concentration to maintain target SpO2 is suggested.16 The current study demonstrates that abrupt weaning to 21% O2 immediately following an increase in heart rate minimizes cerebral hyperoxemia and oxidative stress compared to gradual weaning over 5 min.
Normal postnatal transition at birth results in a gradual increase in PaO2 from 25 to 30 mmHg in the fetus to 45-80 mmHg in the newborn infant over several minutes. This increase in alveolar and arterial O2 results in pulmonary vasodilation22 but may lead to a small increase in free radical production.23,24,25 When O2 supplementation is needed during and after resuscitation, it adds to the prevailing vulnerability of the newborn to oxidative stress.23,26 Following recovery from asphyxial arrest, the combination of reperfusion from increased cerebral blood flow and hyperoxia can result in cerebral oxidative injury in addition to hypoxic ischemic and reperfusion injury.7,27,28 Hyperoxic blood reperfusing the ischemic tissue can form free radicals, worsen oxidative stress, and exacerbate tissue injury.29,30,31 High PaO2 (>140 mmHg) within 1 h after birth has been shown to be associated with higher incidence of moderate to severe HIE.9 Hyperoxemia following ROSC was associated with higher mortality when compared to normoxemia in a large registry-based study of pediatric cardiac arrest.32 The 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations (CoSTR) for pediatric life support guidelines suggest targeting normoxemia after ROSC, with target SpO2 of 94–99% as an alternative to measuring PaO2, for titrating inspired O2 when feasible to achieve normoxia.33 How to utilize oxygen following resuscitation in newborn infants is listed as a major gap in knowledge in the most recent neonatal resuscitation guidelines.16 The International Liaison Committee Neonatal Life Support Task Force is planning a future systematic review of this topic.2
Several previous publications have compared the use of room air and pure O2 during resuscitation in asphyxiated newborns.34,35,36 Linner et al.37 reported high brain tissue PaO2 with 100% O2 during CC and similar time to ROSC with 21% O2 in one-day-old piglets. Solevåg et al.38,39 observed higher SpO2 and higher left ventricular GSSG/GSH ratio after CC using 100% O2. Rawat et al.17 reported that lambs ventilated with 100% O2 during CC had marked increase in PaO2 and pulmonary blood flow immediately following ROSC compared to those ventilated with room air. C-DO2 was significantly lower during CC with both room air and pure O2 comparable to that in the fetal lamb. However, following ROSC, C-DO2 was significantly higher with 100% O2. Rosenberg et al.40 observed decreased cerebral O2 consumption and fractional O2 extraction immediately after recovery from asphyxia compared to control animals with no asphyxia. However, none of these studies evaluated optimal O2 weaning strategies following successful recovery with CC for perinatal cardiac arrest.
The presence of high PaCO2 following prolonged asphyxia results in increased cerebral blood flow.41 Initial PPV with 100% O2 and gradual weaning of inspired O2 based on SpO2 can be associated with ischemia–reperfusion compounded by hyperoxia17 and a potential for cerebral tissue injury due to free radical exposure.42,43 Recently, Badurdeen et al. described the cerebral O2 kinetics and hemodynamics immediately after ROSC in an asphyxiated term lamb model. Similar to our study, they demonstrated marked increase in C-DO2 with gradual weaning of FiO2 over 10–12 min targeting SpO2 of 88–95%. Additionally, they noted a decrease in cerebral fractional O2 extraction between 3 and 9 min after ROSC in comparison to fetal baseline, and fluctuations in cerebral blood flow and arterial blood pressure following ROSC. This study confirms that the gradual wean strategy for FiO2 following ROSC results in excess C-DO2 compared to consumption.13
The present study has shown that abrupt weaning of inspired O2 to room air immediately following ROSC could be protective against cerebral hyperoxia by limiting C-DO2 while allowing for stable changes in PaO2 and SaO2 without compromising AV-DO2. Furthermore, we report a decrease in the GSSG and GSSG/GSH ratio in whole blood with abrupt weaning to room air and decrease in GSH concentration with gradual weaning from 100% O2 at 10 min after ROSC compared to fetal baseline prior to cord occlusion. Glutathione (γ glutamyl-cysteinyl-glycine, GSH) is a crucial tripeptide involved in intracellular defense against reactive oxygen species mediated cell injury.44 In its reduced form, GSH combines with reactive oxygen species and functions as a free radical scavenger. Our findings may indicate preservation of antioxidant mechanisms with abrupt weaning to 21% O2 and excessive oxidative stress with gradual weaning from pure O2.
We acknowledge many limitations in the current study. Pulmonary artery blood flow and pressure were not measured. Tissues were not collected and analyzed to assess brain injury. Neurologic outcomes were not assessed. Even though the lambs were randomized by opaque envelopes, the resuscitation team was not blinded. Most lambs received 0.03 mg/kg dose of epinephrine, but two lambs had spontaneous ROSC with CC without epinephrine and three lambs received 0.01 mg/kg. We did not evaluate intermediate concentrations of inspired O2 (e.g., 30–50%) which may be more relevant in the presence of lung disease or pulmonary hypertension. However, this is the first study to evaluate abrupt weaning to 21% O2 after recovery from perinatal asphyxial arrest and compare to gradual weaning from 100% O2. Real-time monitoring of physiological parameters including invasive blood flows and blood gases were performed. This model of perinatal asphyxial arrest by umbilical cord occlusion in lambs is a well-established large animal model, with similar size and physiology as human neonates that allows for instrumentation and resuscitation.45
Conclusion
In a term ovine model of perinatal asphyxial cardiac arrest, weaning down from 100% O2 after ROSC resulted in cerebral hyperoxia and oxidative stress during the first 10 min after ROSC. The simple intervention of abrupt weaning to 21% inspired O2 immediately after ROSC followed by titrating up not only limits excessive PaO2 and C-DO2 but also limits oxidative stress in the post-resuscitation period. Clinical studies assessing neurodevelopmental outcomes with different weaning strategies are warranted.
References
Halling, C., Sparks, J. E., Christie, L. & Wyckoff, M. H. Efficacy of intravenous and endotracheal epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. J. Pediatr 185, 232-236 (2017).
Wyckoff, M. H. et al. Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 142(Suppl 1), S185–s221 (2020).
Gunn, A. J. et al. Hypothermia: an evolving treatment for neonatal hypoxic ischemic encephalopathy. Pediatrics 121, 648–649 (2008); author reply 9–50.
Black, R. E. et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375, 1969–1987 (2010).
Vento, M., Escobar, J., Cernada, M., Escrig, R. & Aguar, M. The use and misuse of oxygen during the neonatal period. Clin. Perinatol. 39, 165–176 (2012).
Miller, S. L., Wallace, E. M. & Walker, D. W. Antioxidant therapies: a potential role in perinatal medicine. Neuroendocrinology 96, 13–23 (2012).
Perez-de-Sa, V. et al. High brain tissue oxygen tension during ventilation with 100% oxygen after fetal asphyxia in newborn sheep. Pediatr. Res. 65, 57–61 (2009).
Kumar, V. H. et al. Exposure to supplemental oxygen and its effects on oxidative stress and antioxidant enzyme activity in term newborn lambs. Pediatr. Res. 67, 66–71 (2010).
Kapadia, V. S. et al. Perinatal asphyxia with hyperoxemia within the first hour of life is associated with moderate to severe hypoxic-ischemic encephalopathy. J. Pediatr. 163, 949–954 (2013).
Shankaran, S. et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl. J. Med. 353, 1574–1584 (2005).
Azzopardi, D. V. et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med. 361, 1349–1358 (2009).
Foglia, E. E. et al. Duration of resuscitation at birth, mortality, and neurodevelopment: a systematic review. Pediatrics 146, e20201449 (2020).
Badurdeen, S. et al. Excess cerebral oxygen delivery follows return of spontaneous circulation in near-term asphyxiated lambs. Sci. Rep. 10, 16443 (2020).
American Academy of Pediatrics, Weiner, G. M., American Heart Association & Zaichkin J. Textbook of Neonatal Resuscitation. 7th edn (American Academy of Pediatrics, 2016).
Wyckoff, M. H. et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132(Suppl 2), S543–S560 (2015).
Aziz, K. et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142(Suppl 2), S524–S550 (2020).
Rawat, M. et al. Oxygenation and hemodynamics during chest compressions in a lamb model of perinatal asphyxia induced cardiac arrest. Children (Basel) 6, 52 (2019).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 8, e1000412 (2010).
Vali, P. et al. Evaluation of timing and route of epinephrine in a neonatal model of asphyxial arrest. J. Am. Heart Assoc. 6, e004402 (2017).
Isayama, T. et al. The route, dose, and interval of epinephrine for neonatal resuscitation: a systematic review. Pediatrics 146, e20200586 (2020).
Rawat, M. et al. Optimal oxygen targets in term lambs with meconium aspiration syndrome and pulmonary hypertension. Am. J. Respir. Cell Mol. Biol. 63, 510–518 (2020).
Lakshminrusimha, S. & Steinhorn, R. H. Pulmonary vascular biology during neonatal transition. Clin. Perinatol. 26, 601–619 (1999).
Patel, A. et al. Exposure to supplemental oxygen downregulates antioxidant enzymes and increases pulmonary arterial contractility in premature lambs. Neonatology 96, 182–192 (2009).
Soothill, P. W., Nicolaides, K. H., Rodeck, C. H. & Campbell, S. Effect of gestational age on fetal and intervillous blood gas and acid-base values in human pregnancy. Fetal Ther. 1, 168–175 (1986).
Koch, G. & Wendel, H. Adjustment of arterial blood gases and acid base balance in the normal newborn infant during the first week of life. Biol. Neonat. 12, 136–161 (1968).
Saugstad, O. D., Oei, J.-L., Lakshminrusimha, S. & Vento, M. Oxygen therapy of the newborn from molecular understanding to clinical practice. Pediatr. Res. 85, 20–29 (2019).
Østerholt, H. C. et al. Antioxidant protects against increases in low molecular weight hyaluronan and inflammation in asphyxiated newborn pigs resuscitated with 100% oxygen. PLoS ONE 7, e38839 (2012).
Solberg, R., Andresen, J. H., Escrig, R., Vento, M. & Saugstad, O. D. Resuscitation of hypoxic newborn piglets with oxygen induces a dose-dependent increase in markers of oxidation. Pediatr. Res. 62, 559–563 (2007).
Shalak, L. & Perlman, J. M. Hypoxic-ischemic brain injury in the term infant-current concepts. Early Hum. Dev. 80, 125–141 (2004).
Koch, J. D., Miles, D. K., Gilley, J. A., Yang, C.-P. & Kernie, S. G. Brief exposure to hyperoxia depletes the glial progenitor pool and impairs functional recovery after hypoxic-ischemic brain injury. J. Cereb. Blood Flow Metab. 28, 1294–1306 (2008).
Lakshminrusimha, S. et al. Pulmonary hemodynamics and vascular reactivity in asphyxiated term lambs resuscitated with 21 and 100% oxygen. J. Appl Physiol. (1985) 111, 1441–1447 (2011).
Ferguson, L. P., Durward, A. & Tibby, S. M. Relationship between arterial partial oxygen pressure after resuscitation from cardiac arrest and mortality in children. Circulation 126, 335–342 (2012).
Maconochie, I. K. et al. Pediatric Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 142(Suppl 1), S140–S84 (2020).
Saugstad, O. D., Ramji, S., Soll, R. F. & Vento, M. Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology 94, 176–182 (2008).
Saugstad, O. D., Rootwelt, T. & Aalen, O. Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 102, e1 (1998).
Ramji, S. et al. Resuscitation of asphyxic newborn infants with room air or 100% oxygen. Pediatr. Res. 34, 809–812 (1993).
Linner, R., Werner, O., Perez-de-Sa, V. & Cunha-Goncalves, D. Circulatory recovery is as fast with air ventilation as with 100% oxygen after asphyxia-induced cardiac arrest in piglets. Pediatr. Res. 66, 391–394 (2009).
Solevag, A. L., Dannevig, I., Nakstad, B. & Saugstad, O. D. Resuscitation of severely asphyctic newborn pigs with cardiac arrest by using 21% or 100% oxygen. Neonatology 98, 64–72 (2010).
Solevåg, A. L. et al. Myocardial perfusion and oxidative stress after 21% vs. 100% oxygen ventilation and uninterrupted chest compressions in severely asphyxiated piglets. Resuscitation 106, 7–13 (2016).
Rosenberg, A. A. Cerebral blood flow and O2 metabolism after asphyxia in neonatal lambs. Pediatr. Res. 20, 778–782 (1986).
Chandrasekharan, P. K. et al. Continuous end-tidal carbon dioxide monitoring during resuscitation of asphyxiated term lambs. Neonatology 109, 265–273 (2016).
Perez, M., Robbins, M. E., Revhaug, C. & Saugstad O. D. Oxygen radical disease in the newborn, revisited: oxidative stress and disease in the newborn period. Free Radic. Biol. Med. 142, 61–72 (2019).
Thornton, C., Baburamani, A. A., Kichev, A. & Hagberg, H. Oxidative stress and endoplasmic reticulum (ER) stress in the development of neonatal hypoxic-ischaemic brain injury. Biochem. Soc. Trans. 45, 1067–1076 (2017).
Giustarini, D., Milzani, A., Dalle-Donne, I. & Rossi, R. Red blood cells as a physiological source of glutathione for extracellular fluids. Blood Cells Mol. Dis. 40, 174–179 (2008).
Vali, P. et al. The perinatal asphyxiated lamb model: a model for newborn resuscitation. J. Vis. Exp. 57553 (2018).
Acknowledgements
The work has been supported by NIH grants HD096299 (to P.V.), HD072929 (to S.L.), American Academy of Pediatrics- Neonatal Resuscitation Program Research Grant (to S.L.), UC Davis Child Health Research Grant and First Tech Federal Credit Union (to D.S.), Children’s Miracle Network at UC Davis Children’s Hospital Research Grant (to D.S.), and NRP Research Grant from Canadian Pediatric Society. Presented in an abstract form at the American Academy of Pediatrics, National Conference and Exhibition (AAP-NCE) 2020 and received the Young Investigator Award (D.S.).
Author information
Authors and Affiliations
Contributions
D.S. and S.L. made substantial contributions to conception and design, acquisition, extraction, analysis and interpretation of data and drafting the manuscript. P.V., P.C., A.L.L., M.E.H., Z.A., M.H.W., and S.W. made substantial contributions to data acquisition and extraction. All authors critically revised and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interest.
Consent
Patient consent was not required
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sankaran, D., Vali, P., Chen, P. et al. Randomized trial of oxygen weaning strategies following chest compressions during neonatal resuscitation. Pediatr Res 90, 540–548 (2021). https://doi.org/10.1038/s41390-021-01551-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01551-1
This article is cited by
-
Neonatal chest compressions: time to act
Pediatric Research (2021)