Abstract
Background
The neonatal resuscitation program (NRP) recommends interrupted chest compressions (CCs) with ventilation in the severely bradycardic neonate. The conventional 3:1 compression-to-ventilation (C:V) resuscitation provides 90 CCs/min, significantly lower than the intrinsic newborn heart rate (120–160 beats/min). Continuous CC with asynchronous ventilation (CCCaV) may improve the success of return of spontaneous circulation (ROSC).
Methods
Twenty-two near-term fetal lambs were randomized to interrupted 3:1 C:V (90 CCs + 30 breaths/min) or CCCaV (120 CCs + 30 breaths/min). Asphyxiation was induced by cord occlusion. After 5 min of asystole, resuscitation began following NRP guidelines. The first dose of epinephrine was given at 6 min. Invasive arterial blood pressure and left carotid blood flow were continuously measured. Serial arterial blood gases were collected.
Results
Baseline characteristics between groups were similar. Rate of and time to ROSC was similar between groups. CCCaV was associated with a higher PaO2 (partial oxygen tension) (22 ± 5.3 vs. 15 ± 3.5 mmHg, p < 0.01), greater left carotid blood flow (7.5 ± 3.1 vs. 4.3 ± 2.6 mL/kg/min, p < 0.01) and oxygen delivery (0.40 ± 0.15 vs. 0.13 ± 0.07 mL O2/kg/min, p < 0.01) compared to 3:1 C:V.
Conclusions
In a perinatal asphyxiated cardiac arrest lamb model, CCCaV showed greater carotid blood flow and cerebral oxygen delivery compared to 3:1 C:V resuscitation.
Impact
-
In a perinatal asphyxiated cardiac arrest lamb model, CCCaV improved carotid blood flow and oxygen delivery to the brain compared to the conventional 3:1 C:V resuscitation.
-
Pre-clinical studies assessing neurodevelopmental outcomes and tissue injury comparing continuous uninterrupted chest compressions to the current recommended 3:1 C:V during newborn resuscitation are warranted prior to clinical trials.
Similar content being viewed by others
Introduction
Perinatal asphyxia occurs in ≈1 per 1000 term births in the United States and is responsible for almost 25% of the >4 million neonatal deaths worldwide.1,2 Newborn infants requiring chest compressions (CCs) and/or epinephrine are at high risk for hypoxic–ischemic encephalopathy (HIE), leading to neurological morbidity or death. Early return of spontaneous circulation (ROSC) may decrease mortality and improve the outcome among survivors of HIE.
The current pediatric and adult basic life support guidelines emphasize priority in initiating early CCs and to minimize interruptions.3,4 Adult animal models with a ventricular fibrillation-induced cardiac arrest that received uninterrupted CC have shown improved hemodynamics and neurologic outcomes.5,6,7,8 A few clinical studies have reported on improved survival when providing uninterrupted CC.9,10,11 However, a large randomized clinical trial did not demonstrate higher rates of survival or favorable neurologic outcomes in individuals with out-of-hospital cardiac arrest who were randomized to continuous CC.12 The applicability of these findings to the neonatal population is limited, as the presence of the ductus arteriosus might prevent the build-up of diastolic pressure and coronary perfusion pressure with continuous CC in newly born infants in the delivery room.13
In contrast to adults, where sudden cardiac arrest leads to an abrupt cessation in cardiac output in the setting of well-oxygenated blood, neonatal cardiac arrest arises from profound bradycardia as a result of oxygen depletion, carbon dioxide accumulation, and increasing lactic acidosis secondary to asphyxia. Severe metabolic acidosis and substrate depletion can lead to profound vasodilation in the asphyxiated state as opposed to sudden cardiac arrest, which can influence the effect of CCs on hemodynamic parameters in the asphyxiated newborn. In the asphyxiated neonate with cardiac arrest due to severe hypoxemia and hypercarbia, ventilation remains critical in establishing ROSC and resuscitation with exclusive CC in asphyxiated piglet models has not shown to be effective in achieving ROSC.14,15 Ventilation of the lungs is, therefore, a critical component of neonatal resuscitation. Furthermore, in the presence of extreme bradycardia or cardiac arrest, pulmonary blood flow cannot be sustained and gas exchange does not occur with ventilation alone. The optimal ventilation strategy immediately after birth has not been determined and different compression-to-ventilation (C:V) ratios have not shown improved outcomes or higher quality compressions in pre-clinical and neonatal manikin models, respectively.16,17,18,19,20 In addition, the pediatric and adult CC rate in individuals with a secure airway is 100 CC/min, which is higher than the intrinsic baseline heart rate at rest (≈70–90 beats per minute (b.p.m.)). Interestingly, the current recommendation of 90 CC/min in neonatal resuscitation is considerably lower than the normal newborn resting heart rate (≈120–160 b.p.m.).
Our understanding and knowledge of resuscitative medicine in newborns is limited to postnatal animal and simulation manikin models that do not adequately depict the transitioning fetal circulation, fluid-filled alveoli, patent ductus arteriosus, and ductus venosus inherent to newborn infants.21,22,23 Taking into consideration that adult patients in cardiac arrest who receive uninterrupted CC may have improved survival, that the evidence behind the current recommended C:V ratio in newborn resuscitation is weak, and that heart rate is the predominant factor in determining cardiac output in neonates, we hypothesize that uninterrupted, continuous CC with asynchronous ventilations (CCCaVs) in a perinatal asphyxiated cardiac arrest newborn lamb model with transitioning circulation leads to quicker ROSC and better hemodynamic variables compared to the 3:1 C:V ratio recommended by the neonatal resuscitation program (NRP).
Methods
Animal preparation
The study protocol has been approved by the Institutional Animal Care and Use Committee (IACUC, protocol #20734) at the University of California Davis. All experiments were performed according to animal ethical guidelines, in compliance with the ARRIVE guidelines.24 Time-dated near-term (139–141 day gestation; term is 145 days) pregnant ewes (Dorper-cross) were procured by Van Laningham Farm (Arbuckle, CA). Following an overnight fast, the ewe was medicated with intravenous diazepam and ketamine. The ewe was intubated with a 10.0-mm cuffed endotracheal tube (ETT) and general anesthesia was provided by 2–3% inhaled isoflurane. The ewe was continuously monitored with a pulse oximeter and an end-tidal CO2 monitor. Following a cesarean section, the fetal lamb was partially exteriorized and intubated with a 4.5-mm cuffed ETT. The fetal lung fluid in the ETT was partially drained passively by gravity by tilting the head to the side and, thereafter, the ETT was occluded to prevent gas exchange. A catheter was placed in the right carotid artery to measure blood pressures and collect blood samples. The right jugular vein was catheterized for fluid and medication administration. A left carotid flow probe (2 mm) was placed to measure blood flow. A pulse oximeter was placed on the right forelimb for continuous capillary oxyhemoglobin saturation monitoring. Following instrumentation, the umbilical cord was tied and cut. In the rare event that a lamb would have a complication related to the instrumentation and needed to be euthanized prior to the experiment, the lamb would not count toward the total number.
Experimental protocol
After the cord was cut, the lamb was delivered onto a radiant warmer. During the asphyxial period, an umbilical arterial catheter was placed for blood collection (invasive blood pressure monitoring continued to be obtained by transducing the right carotid artery catheter to avoid interruptions in data during blood draws). A three-lead electrocardiogram was applied to the lamb. Asystole was defined by the absence of carotid blood flow, flat tracing in the arterial blood pressure waveform, and absent heart rate (assessed by auscultation). Resuscitation was started 5 min from the time of asystole. The initiation of resuscitation was defined by the onset of positive pressure ventilation (PPV) with 21% oxygen by means of a T-piece resuscitator.25 After 30 s of effective PPV through the ETT, CCs were initiated and inspired oxygen was increased to 100%.26 The first dose of epinephrine (0.03 mg/kg) was administered intravenously at 6 min from the onset of resuscitation if ROSC had not been achieved. This time point is chosen to approximate the time taken to administer intravenous epinephrine in clinical scenarios.27,28 Subsequent epinephrine administration at the same dose was given every 3 min until ROSC or for a total of four doses. ROSC was defined by a sustained heart rate >100 b.p.m. and a mean arterial blood pressure >40 mmHg. Arterial blood gases (ABGs) were collected approximately every 1–2 min during active resuscitation and at the time of ROSC, 5, 10, and 15 min post ROSC. Content of arterial oxygen (CaO2) was calculated using the equation: (1.34 × Hgb [g/dL] × SaO2 %/100%) + (partial oxygen tension (PaO2) [mmHg] × 0.0031). Oxygen delivery to the brain was estimated by multiplying CaO2 and left carotid blood flow.
Lambs have a keel-shaped chest that is different from humans, which could hamper CCs in the anterio-posterior direction. CCs were, therefore, given manually in the medio-lateral direction. CCs were provided by one individual (P.V.) for all experiments. An adaptor was attached between the ETT and T-piece resuscitator and connected to a respiratory function monitor (NM3, Respironics, Philips, Andover, MA) that would display the respiratory rate and which was visible to the individual who was providing PPV. The individuals participating in the code were unable to see the hemodynamic parameters displayed on the laptop screen by the acquisition software. As per the NRP guidelines, the resuscitators chanted “one and two and three and breathe” during resuscitation. We only gave PPV during the “breathe” phase in the 3:1 C:V arm. For lambs randomized to CCCaV, the individual tasked to give PPV provided a breath every 2 s, and the one giving CC, compressed the chest twice every second.
Lambs were randomized into two groups using opaque sealed envelopes and we did not control for confounders:
3:1 C:V (control) group: at the onset of resuscitation, PPV with set pressures of 35/5 cm H2O with 21% oxygen were provided by a T-piece resuscitator.25,29 After 30 s of PPV, CCs were initiated at a C:V ratio of 3:1 to achieve 90 compressions and 30 breaths/min, and inspired oxygen was increased to 100%. The breath was administered during a pause in compressions as recommended by NRP.
CCCaV group: at the onset of resuscitation, PPV with set pressures of 35/5 cm H2O with 21% oxygen was provided by a T-piece resuscitator. After 30 s, continuous CCs were given at a rate of 120 compressions/min and PPV was continued at 30 breaths/min and inspired oxygen was increased to 100%. CCs were not paused during breaths and were administered asynchronously with breaths.
Given the nature of the experiments, the investigators could not be blinded. A dedicated scribe who could monitor the calculated heart rate from the arterial blood pressure tracing on the data acquisition software would provide feedback to the resuscitator on the CC rate.
Sample size calculation
Data from previous experiments from six lambs with cardiac arrest induced by umbilical cord occlusion resuscitated by 3:1 C:V demonstrated a mean time to ROSC of 5.9 min (standard deviation 2.2 min). One experiment with CCCaV resulted in ROSC at 3.1 min (difference in time to ROSC of 2.8 min). We planned a study of a continuous response variable (time to ROSC) from independent control (3:1 C:V) and experimental lambs (CCCaV) with one control per experimental subject. In our previous studies, the time to ROSC with 3:1 C:V resuscitation was normally distributed with a standard deviation of 2.2 min. If the true difference in the experimental and control means is 2.8 min, we will need to study 11 experimental lambs and 11 control lambs (for a total of 22 lambs) to be able to reject the null hypothesis that the population means of the experimental and control groups are equal with probability (power) 0.8. The Type I error probability associated with this test of this null hypothesis is 0.05.
This sample size of 22 lambs will have adequate power (0.8) to evaluate a 2.5 mL/kg/min difference in carotid blood flow during CCs based on a standard deviation of 2 mL/kg/min from previous studies. Given the high incidence of ROSC in this model (~80%), we may not have adequate power to show a difference in the incidence of ROSC.
Data analysis
Hemodynamic variables were continuously recorded using a computer with acquisition and analysis software (BIOPAC Systems, Goleta, CA). Hemodynamic data were acquired using BIOPAC AcqKnowledge software, which has an acquisition sample rate of 2000 Hz. Data were extracted by 10 s increments and averaged over 1 min. Continuous variables are expressed as mean and standard deviation (SD). Categorical variables are analyzed using χ2 test with Fisher’s exact test as required. Continuous variables are analyzed by one‐way analysis of variance between groups with Fisher’s post hoc test within groups. Cox proportional hazards model was used to analyze time variables. SPSS 24 (IBM, Armonk, NY) was used for statistical analysis. Statistical significance was defined as p < 0.05. All lambs were included in the analysis.
Results
A total of 22 lambs were studied with 11 lambs in each group (3:1 C:V vs. CCCaV). Characteristics of the lambs, including baseline hemodynamic parameters, weight, sex distribution, and ABG analysis, were similar between the groups (Table 1). Cord occlusion caused severe metabolic and respiratory acidosis in all lambs and the time to cardiac arrest (asystole) was not significantly different between the groups.
Success of ROSC and epinephrine
The incidence of ROSC was similar at 91% (10/11 lambs in each group) as was the median (interquartile range [IQR]) time to achieve ROSC at 6.1 (2.9–7.1) min in the 3:1 C:V group compared to 6.2 (4.2–6.9) min in the CCCaV group (p = 0.84; Table 2). Successful resuscitation without the need for epinephrine was the same with 4/11 lambs (36%) in each group achieving ROSC prior to epinephrine administration. All lambs that achieved ROSC after epinephrine did so after a single dose.
Hemodynamic parameters
The average (SD) CC rate was 88 (7) CC/min in the 3:1 C:V group and 122 (6) CC/min in the CCCaV group. There was no difference in the systolic, diastolic, and mean blood pressures during CC between the groups (Table 3). The mean left carotid blood flow (SD) was significantly higher during CC in the lambs that received CCCaV at 7.5 (3.1) mL/kg/min compared to 4.2 (2.6) mL/kg/min in the 3:1 C:V group (p < 0.01).
ABG analysis
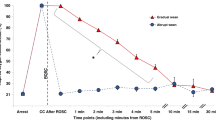
The PaO2 in the blood during CC was significantly greater in the CCCaV vs. the 3:1 C:V group at 22 (5.3) vs. 15 (3.5) mmHg (p < 0.01; Table 3). CaO2 was also significantly higher in the CCCaV group at 5.3 (2.1) mL O2/dL vs. 3.0 (1.4) mL O2/dL in the 3:1 C:V group (p = 0.03). Fetal baseline left carotid oxygen delivery (C-DO2, calculated by multiplying the oxygen content in blood by the left carotid blood flow) was similar between the groups at 2.4 (1.7) mL O2/kg/min and 2.6 (1.5) mL O2/kg/min in the CCCaV and 3:1 C:V group, respectively (Table 1). The C-DO2 was improved with continuous uninterrupted CCs at 0.4 (0.15) mL O2/kg/min compared to 0.13 (0.07) mL O2/kg/min in the 3:1 C:V group (Fig. 1).
ROSC vs. non-ROSC
The two lambs that did not achieve ROSC had similar systolic, diastolic, and mean blood pressures during CCs [26 (3.8), 9 (2.1) and 16 (3.2) mmHg, respectively, with CCCaV vs. 24 (2.3), 6 (1.6), and 13 (1.9) mmHg, respectively, with 3:1 C:V]. Thus, the blood pressures in the two lambs that did not achieve ROSC were similar to the blood pressures observed in the lambs that were successfully resuscitated. The mean left carotid blood flow was also similar between the two lambs that did not achieve ROSC at 1.6 (0.4) vs. 1.9 (0.4) mL/kg/min in the 3:1 C:V and CCCaV groups, respectively.
There was no difference in the hemodynamic variables at the time of ROSC and for the following hour post ROSC (Fig. 2). The oxygen delivery to the brain at the time of ROSC was similar between groups (~2.4 mL O2/kg/min) and comparable to the baseline values (Tables 1 and 2).
a There was no difference in heart rate during the study period. By study design, chest compression rates were significantly different between groups. b There was no difference in diastolic blood pressure between the two groups during the study period. Diastolic blood pressure ranged between 7 and 10 mmHg during chest compressions. c There was no difference in mean blood pressure between the two groups during the study period. d Mean left carotid blood flow was significantly higher with CCCaV compared to 3:1 C:V. DBP diastolic blood pressure, C:V compression-to-ventilation, CCCaV continuous chest compressions with asynchronous ventilation, MBP mean blood pressure, Qca carotid blood flow. *P value <0.05. ^ at 1–3 min, n = 9 lambs in the CCCaV group and at 6 min, n = 7 lambs in the 3:1 C:V and CCCaV groups.
Discussion
In the severely asphyxiated newborn not responding to ventilation, optimal cardiovascular support with CC + PPV is vital to improve survival without neurological morbidity. The optimal C:V ratio that efficiently delivers oxygen to the brain and heart and hastens ROSC, however, remains unknown. In adult cardiopulmonary resuscitation, coronary perfusion pressure (estimated by subtracting diastolic aortic pressure from right atrial pressure) >20 mmHg has been shown to be a strong predictor of achieving ROSC.30 Experiments on adult pigs with cardiac arrest induced by ventricular fibrillation have demonstrated a stepwise increase in diastolic blood pressure with each successive CC and an abrupt drop in blood pressure following interruption of CC.8 In the resuscitation of the newly born in the delivery room with a patent ductus arteriosus, it is not clear if this relationship is maintained. In fact, we have demonstrated in the current experiments that newborn lambs with a transitioning circulation and a patent ductus arteriosus were successfully resuscitated despite maintaining mean diastolic blood pressures at ~7–10 mmHg (Fig. 2b). The relatively low diastolic aortic pressures must be sufficient to adequately perfuse the coronary arteries of the newborn heart and an attempt to maintain higher diastolic blood pressures may not be necessary.13
Optimizing oxygen delivery to the brain during resuscitation may potentially be associated with better neurological outcomes. An important finding in the current study highlights that the left carotid blood flow is significantly greater when providing continuous uninterrupted CCs with asynchronous ventilation compared to 3:1 C:V resuscitation in spite of attaining comparable systolic, diastolic, and mean aortic blood pressures during compressions. This is possibly secondary to higher CC rate in lambs from the CCCaV group. The carotid flows in the two lambs that did not achieve ROSC (1.6 mL/kg/min with 3:1 C:V vs. 1.9 mL/kg/min with CCCaV) were considerably lower than what was observed in the lambs that achieved ROSC (4.2 mL/kg/min in 3:1 C:V vs. 7.5 mL/kg/min with CCCaV). No conclusions can be drawn from such a small number, but we speculate that greater coronary blood flow would be observed with greater left carotid blood flow, which may explain ROSC success. Furthermore, serial ABG analyses during CC demonstrated that CCCaV achieved a greater PaO2 (22 ± 5.3 mmHg) compared to 3:1 C:V (15 ± 3.5 mmHg), which implies improved pulmonary blood flow during CCCaV. With fetal hemoglobin with a P50 of 19 mmHg, these values fall along the steep portion of the hemoglobin–oxygen dissociation curve resulting in significant differences in SaO2 and oxygen content between the two groups. Severe acidosis results in a rightward shift in the hemoglobin–oxygen dissociation curve and explains how a PaO2 of 22 mmHg has a SaO2 of 33% (Fig. 3).31
Fetal hemoglobin (open squares) has a higher affinity for oxygen compared to adult hemoglobin (small pink circles). Acidosis causes a rightward shift in the oxygen hemoglobin dissociation curve (dashed line). During resuscitation and at the time of return of spontaneous circulation (ROSC), the range of PaO2 is on the steep part of the curve and a small change in PaO2 results in a greater change in SaO2 and CaO2. CaO2 content of arterial oxygen, C:V compression-to-ventilation, CCCaV continuous chest compressions with asynchronous ventilation, PaO2 partial tension of arterial oxygen, SaO2 saturation of arterial oxygen. Modified from Moraga et al.31.
In a newborn piglet asphyxia model with cleared lung fluid and a closed ductus arteriosus comparing CCCaV to 3:1 C:V, 29% of CC overlapped with ventilation in the CCCaV group as opposed to 25% in the 3:1 C:V group with no effect on hemodynamic parameters.20 There is no evidence, therefore, to suggest that overlapping CC and ventilation adversely affect hemodynamics or ventilation. The aforementioned study showed a similar incidence of ROSC and hemodynamics. However, notable differences exist between the piglet study and the current study: (1) the mode of asphyxia was by hypoxic ventilation and tracheal tube occlusion, (2) the degree of asphyxia did not lead to cardiac arrest, and (3) epinephrine was administered intravenously 1 min after CCs were commenced and hence the duration of CC was relatively short.
In the current study, improved left carotid blood flow and a greater PaO2 resulted in more oxygen delivery (DO2) to the brain with CCCaV. When assessing C-DO2 compared to fetal baseline values, lambs that received CCCaV maintained a considerably greater C-DO2 at 17% (0.4/2.4 mL O2/kg/min) compared to 5% (0.13/2.6 mL O2/kg/min) in the 3:1 C:V group. The neonatal heart is structurally and functionally very different from the pediatric and adult heart. The neonatal heart is less compliant and cardiac output is predominantly influenced by the frequency of contractions (heart rate) rather than by the volume of blood in the ventricles (preload/stroke volume). A study using a mathematical model of the human cardiopulmonary system has demonstrated that the most effective CC frequency depends upon body size and weight with higher CC frequency conferring optimal perfusion in newborns.32 Achieving a higher CC rate (i.e., continuous CC at 120 CC/min with asynchronous ventilation at 30 breaths/min) is likely to increase blood flow to essential organs compared to the traditional 90 CC/min and 30 breaths/min during resuscitation.
Fetuses and newborn animals of many species have been shown to survive for much longer periods in the absence of oxygen compared to adults of the same species.33 The median time to asystole in this study is comparable to asystole times (median 12–18 min) in previous publications by our group.25,34 The relative length of time required to induce severe bradycardia and cardiac arrest in the newly born explains why the majority of severely asphyxiated newborns have a heart rate. We acknowledge several limitations in the current study. Neurologic outcomes were not assessed. Pulmonary arterial blood flow was not measured because an incomplete seal following a thoracotomy may have impacted the adequacy of CCs and ventilation. The current model is of asystolic cardiac arrest and the response to CCs in severe bradycardia was not explored. In spite of the prolonged asphyxial period and time in asystole, an extended period of cardiac arrest may have decreased ROSC success and revealed a difference between the resuscitation techniques. The hemodynamic parameters observed in this study may not directly translate to the human newborn owing to the interspecies differences in chest anatomy and CC method. Nonetheless, such fundamental questions as the hemodynamic effects of CC in the context of fetal shunts and fluid-filled lungs and the optimal C:V ratio in newborns underscore the large knowledge gap in neonatal resuscitation. The asphyxiated newborn lamb with transitioning physiology closely mimics the newborn in the delivery room and is the ideal model to study newborn physiology. This study provides accurate real-time measurement of invasive physiologic parameters and frequent ABG analysis; valuable information that cannot be obtained from clinical studies.
Conclusion
In a perinatal asphyxial cardiac arrest lamb model, CCCaV showed higher PaO2, greater carotid blood flow and oxygen delivery to the brain compared to the conventional 3:1 C:V resuscitation. No difference between groups was observed in the time to ROSC, the rate of ROSC or the number of epinephrine doses administered. Experimental studies surviving animals up to 24 h to assess short-term neurologic outcomes and assessment of brain injury by immunohistochemistry are necessary before conducting clinical trials.
References
Black, R. E. et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375, 1969–1987 (2010).
Bairoliya, N. & Fink, G. Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: an observational study. PLoS Med. 15, e1002531 (2018).
Kleinman, M. E. et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S414–S435 (2015).
Atkins, D. L. et al. Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S519–S525 (2015).
Kern, K. B., Hilwig, R. W., Berg, R. A., Sanders, A. B. & Ewy, G. A. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation 105, 645–649 (2002).
Ewy, G. A. et al. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation 116, 2525–2530 (2007).
Xanthos, T. et al. Continuous chest compressions improve survival and neurologic outcome in a swine model of prolonged ventricular fibrillation. Am. J. Emerg. Med. 30, 1389–1394 (2012).
Berg, R. A. et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation 104, 2465–2470 (2001).
Bobrow, B. J. et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 304, 1447–1454 (2010).
Kitamura, T. et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet 375, 1347–1354 (2010).
Rea, T. D. et al. CPR with chest compression alone or with rescue breathing. N. Engl. J. Med. 363, 423–433 (2010).
Nichol, G. et al. Trial of continuous or interrupted chest compressions during CPR. N. Engl. J. Med. 373, 2203–2214 (2015).
Vali, P. et al. Hemodynamics and gas exchange during chest compressions in neonatal resuscitation. PLoS ONE 12, e0176478 (2017).
Berg, R. A., Hilwig, R. W., Kern, K. B., Babar, I. & Ewy, G. A. Simulated mouth-to-mouth ventilation and chest compressions (bystander cardiopulmonary resuscitation) improves outcome in a swine model of prehospital pediatric asphyxial cardiac arrest. Crit. Care Med. 27, 1893–1899 (1999).
Berg, R. A., Hilwig, R. W., Kern, K. B. & Ewy, G. A. “Bystander” chest compressions and assisted ventilation independently improve outcome from piglet asphyxial pulseless “cardiac arrest”. Circulation 101, 1743–1748 (2000).
Barber, C. A. & Wyckoff, M. Neonatal cardiac compressions following asystole from asphyxia: beneficial or futile? [Abstract 7932.7]. In Pediatric Academic Societies Meeting, Toronto, Canada (2007).
Solevåg, A. L., Dannevig, I., Wyckoff, M., Saugstad, O. D. & Nakstad, B. Extended series of cardiac compressions during CPR in a swine model of perinatal asphyxia. Resuscitation 81, 1571–1576 (2010).
Solevag, A. L., Dannevig, I., Wyckoff, M., Saugstad, O. D. & Nakstad, B. Return of spontaneous circulation with a compression:ventilation ratio of 15:2 versus 3:1 in newborn pigs with cardiac arrest due to asphyxia. Arch. Dis. Child Fetal Neonatal Ed. 96, F417–F421 (2011).
Hemway, R. J., Christman, C. & Perlman, J. The 3:1 is superior to a 15:2 ratio in a newborn manikin model in terms of quality of chest compressions and number of ventilations. Arch. Dis. Child Fetal Neonatal Ed. 98, F42–F45 (2013).
Schmölzer, G. M. et al. 3:1 compression to ventilation ratio versus continuous chest compression with asynchronous ventilation in a porcine model of neonatal resuscitation. Resuscitation 85, 270–275 (2014).
Solevåg, A. L. & Schmölzer, G. M. Optimal chest compression rate and compression to ventilation ratio in delivery room resuscitation: evidence from newborn piglets and neonatal manikins. Front. Pediatr. 5, 3 (2017).
Solevåg, A. L. et al. Chest compressions in newborn animal models: a review. Resuscitation 96, 151–155 (2015).
Wyckoff, M. H. & Berg, R. A. Optimizing chest compressions during delivery-room resuscitation. Semin. Fetal Neonatal Med. 13, 410–415 (2008).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving Bioscience Research Reporting: the ARRIVE Guidelines for Reporting Animal Research. PLoS Biol. 8, e1000412 (2010).
Vali, P. et al. Evaluation of timing and route of epinephrine in a neonatal model of asphyxial arrest. J. Am. Heart Assoc. 6, 2 (2017).
Wyckoff, M. H. et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S543–S560 (2015).
McKinsey, S. & Perlman, J. M. Resuscitative interventions during simulated asystole deviate from the recommended timeline. Arch. Dis. Child Fetal Neonatal Ed. 101, F244–F247 (2016).
Halling, C., Sparks, J. E., Christie, L. & Wyckoff, M. H. Efficacy of intravenous and endotracheal epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. J. Pediatr. 185, 232–236 (2017).
Vali, P. et al. The perinatal asphyxiated lamb model: a model for newborn resuscitation. J. Vis. Exp. 138, 57553 (2018).
Paradis, N. A. et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 263, 1106–1113 (1990).
Moraga, F., Monge, C., Riquelme, R. & Llanos, A. J. Fetal and maternal blood oxygen affinity: a comparative study in llamas and sheep. Comp. Biochem. Physiol. A 115, 111–115 (1996).
Babbs, C. F., Meyer, A. & Nadkarni, V. Neonatal CPR: room at the top-a mathematical study of optimal chest compression frequency versus body size. Resuscitation 80, 1280–1284 (2009).
Dawes, G. S., Mott, J. C. & Shelley, H. J. The importance of cardiac glycogen for the maintenance of life in foetal lambs and newborn animals during anoxia. J. Physiol. 146, 516–538 (1959).
Vali, P. et al. Continuous chest compressions during sustained inflations in a perinatal asphyxial cardiac arrest lamb model. Pediatr. Crit. Care Med. 18, e370–e377 (2017).
Acknowledgements
The work has been supported by NIH grants HD096299 (P.V.) and HD072929 (S.L.).
Author information
Authors and Affiliations
Contributions
P.V. made substantial contributions to conception and design, acquisition, analysis and interpretation of data. and drafting the manuscript. A.L., M.H., Z.A., P.C., H.J., and D.S. made substantial contributions to data acquisition and extraction. All authors critically revised and approve the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vali, P., Lesneski, A., Hardie, M. et al. Continuous chest compressions with asynchronous ventilations increase carotid blood flow in the perinatal asphyxiated lamb model. Pediatr Res 90, 752–758 (2021). https://doi.org/10.1038/s41390-020-01306-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01306-4
This article is cited by
-
Neonatal resuscitation with continuous chest compressions and high frequency percussive ventilation in preterm lambs
Pediatric Research (2024)
-
Laryngeal mask ventilation with chest compression during neonatal resuscitation: randomized, non-inferiority trial in lambs
Pediatric Research (2022)
-
Neonatal chest compressions: time to act
Pediatric Research (2021)