Abstract
Background
Cerebral oxygen delivery (cDO2) is low during chest compressions (CC). We hypothesized that gas exchange and cDO2 are better with continuous CC with high frequency percussive ventilation (CCC + HFPV) compared to conventional 3:1 compressions-to-ventilation (C:V) resuscitation during neonatal resuscitation in preterm lambs with cardiac arrest induced by umbilical cord compression.
Methods
Fourteen lambs in cardiac arrest were randomized to 3:1 C:V resuscitation (90CC + 30 breaths/min) per the Neonatal Resuscitation Program guidelines or CCC + HFPV (120CC + HFPV continuously). Intravenous epinephrine was given every 3 min until return of spontaneous circulation (ROSC).
Results
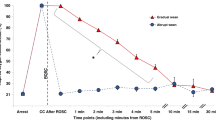
There was no difference in the incidence and time to ROSC between both groups. Median (IQR) PaCO2 was significantly lower with CCC + HFPV during CC, at ROSC and 15 min post-ROSC-[104 (99–112), 83 (77–99), and 43 (40–64)], respectively compared to 3:1 C:V-[149 (139–167), 153 (143–168), and 153 (138–178) mmHg. PaO2 and cDO2 were higher with CCC + HFPV during CC and at ROSC. PaO2 was similar 15 min post-ROSC with a lower FiO2 in the CCC + HFPV group 0.4 (0.4–0.5) vs. 1 (0.6–1).
Conclusion
In preterm lambs with perinatal cardiac-arrest, continuous chest compressions with HFPV does not improve ROSC but enhances gas exchange and increases cerebral oxygen delivery compared to 3:1 C:V during neonatal resuscitation.
Impact statement
-
Ventilation is the most important intervention in newborn resuscitation.
-
Currently recommended 3:1 compression-to-ventilation ratio is associated with hypercarbia and poor oxygen delivery to the brain.
-
Providing uninterrupted continuous chest compressions during high frequency percussive ventilation is feasible in a lamb model of perinatal cardiac arrest, and demonstrates improved gas exchange and oxygen delivery to the brain.
-
This is the first study in premature lambs evaluating high frequency percussive ventilation with asynchronous chest compressions and lays the groundwork for future clinical studies to optimize gas exchange and hemodynamics during chest compressions in newborns.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and analyzed from the current study are available from the corresponding author on request.
References
Tingay, D. G. et al. Imaging the respiratory transition at birth: unraveling the complexities of the first breaths of life. Am. J. Respir. Crit. Care Med. 204, 82–91 (2021).
Lakshminrusimha, S. & Steinhorn, R. H. Pulmonary vascular biology during neonatal transition. Clin. Perinatol. 26, 601–619 (1999).
Ramachandran, S., Bruckner, M., Kapadia, V. & Schmolzer, G. M. Chest Compressions and Medications During Neonatal Resuscitation. Semin Perinatol 46, 151624 (2022).
Dargaville, P. A. & Tingay, D. G. Lung protective ventilation in extremely preterm infants. J. Paediatr. Child Health 48, 740–746 (2012).
Solevåg, A. L., Dannevig, I., Wyckoff, M., Saugstad, O. D. & Nakstad, B. Extended series of cardiac compressions during Cpr in a swine model of perinatal asphyxia. Resuscitation 81, 1571–1576 (2010).
Vali, P. et al. Continuous Chest Compressions with Asynchronous Ventilations Increase Carotid Blood Flow in the Perinatal Asphyxiated Lamb Model. Pediatr Res 90, 752–758 (2021).
Schmölzer, G. M. et al. Cardiopulmonary resuscitation with chest compressions during sustained inflations: a new technique of neonatal resuscitation that improves recovery and survival in a neonatal porcine model. Circulation 128, 2495–2503 (2013).
Kirpalani, H. et al. Effect of sustained inflations vs intermittent positive pressure ventilation on bronchopulmonary dysplasia or death among extremely preterm infants: the sail randomized clinical trial. JAMA 321, 1165–1175 (2019).
Vali, P. et al. Hemodynamics and gas exchange during chest compressions in neonatal resuscitation. PLoS One 12, e0176478 (2017).
Aziz, K. et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142, S524–S550 (2020).
Wyckoff, M. H. et al. Neonatal life support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 142, S185–S221 (2020).
Weiner, G. (editor). Textbook of Neonatal Resuscitation 8th edn. (American Academy of Pediatrics, Itasca, IL, USA, 2021).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the arrive guidelines for reporting animal research. PLOS Biol. 8, e1000412 (2010).
Roberts, B. W. et al. Association between postresuscitation partial pressure of arterial carbon dioxide and neurological outcome in patients with post-cardiac arrest syndrome. Circulation 127, 2107–2113 (2013).
Pyrds O, G. G., Lou, H. & Friis-Hansen, B. Vasoparalysis associated with brain damage in asphyxiated term infants. J. Pediatr. 117, 119–125 (1990).
Pryds, O., Greisen, G., Skov, L. L. & Friis-Hansen, B. Carbon dioxide-related changes in cerebral blood volume and cerebral blood flow in mechanically ventilated preterm neonates: comparison of near infrared spectrophotometry and 133xenon clearance. Pediatr. Res. 27, 445–449 (1990).
Buchmayer, J. et al. Cardiopulmonary resuscitation of a very preterm infant using high-frequency oscillation ventilation. Resuscitation Plus 11, 100265 (2022).
Shah, P. S., Shah, P. & Tai, K. F. Chest compression and/or epinephrine at birth for preterm infants <32 weeks gestational age: matched cohort study of neonatal outcomes. J. Perinatol. 29, 693–697 (2009).
Fischer, N. et al. Extensive cardiopulmonary resuscitation of preterm neonates at birth and mortality and developmental outcomes. Resuscitation 135, 57–65 (2019).
Saugstad, O. D., Oei, J. L., Lakshminrusimha, S. & Vento, M. Oxygen therapy of the newborn from molecular understanding to clinical practice. Pediatr. Res 85, 20–29 (2019).
Altaany, D., Natarajan, G., Gupta, D., Zidan, M. & Chawla, S. Severe intraventricular hemorrhage in extremely premature infants: are high carbon dioxide pressure or fluctuations the culprit? Am. J. Perinatol. 32, 839–844 (2015).
Rawat, M. et al. Oxygenation and hemodynamics during chest compressions in a lamb model of perinatal asphyxia induced cardiac arrest. Children 6 (2019).
Vali, P. et al. Continuous Chest Compressions During Sustained Inflations in a Perinatal Asphyxial Cardiac Arrest Lamb Model. Pediatr Crit Care Med 18, e370–e377 (2017).
Giusto, E. et al. Comparison of synchronized and asynchronized chest compressions in the term and preterm ovine perinatal cardiac arrest. Pediatric Academic Societies Meeting, Washington D.C. 701.445 (2023).
Ayoub, D., Elmashad, A., Rowisha, M., Eltomey, M. & El Amrousy, D. Hemodynamic effects of high-frequency oscillatory ventilation in preterm neonates with respiratory distress syndrome. Pediatr. Pulmonol. 56, 424–432 (2021).
Honey, G., Bleak, T., Karp, T., MacRitchie, A. & Null, D. Jr. Use of the duotron transporter high frequency ventilator during neonatal transport. Neonatal Netw. 26, 167–174 (2007).
Oddi, M. The Safety and Efficacy of Utilization of High-Frequency Ventilation During Transport of Neonates Suffering from Severe Respiratory Disease. Doctoral Dissertation, Northerncentral University 10825259. (ProQuest Dissertations and Theses Global, Ann Arbor, MI, USA, 2017)
Acknowledgements
This research was funded by Children’s Miracle Network at University of California, Davis (S-CMNEG22).
Author information
Authors and Affiliations
Contributions
Contributed to study design, study conduction, and data analysis: E.G, D.S., A.L., H.J., M.H., V.H., L.Z., S.L., P.V. Drafted and provided critique of manuscript: E.G., D.S., A.L., S.L., P.V. Final approval: E.G., D.S., S.L., P.V.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest. S.L. is a member of the AAP-NRP steering committee. The views expressed in this article are his own and does not represent the official position of AAP or NRP. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giusto, E., Sankaran, D., Lesneski, A. et al. Neonatal resuscitation with continuous chest compressions and high frequency percussive ventilation in preterm lambs. Pediatr Res 95, 160–166 (2024). https://doi.org/10.1038/s41390-023-02820-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02820-x