Abstract
Background
Morphine is commonly used for postoperative analgesia in children. Here we studied the pharmacodynamics of morphine in children after cardiac surgery receiving protocolized morphine.
Methods
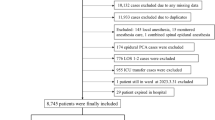
Data on morphine rescue requirements guided by validated pain scores in children (n = 35, 3–36 months) after cardiac surgery receiving morphine as loading dose (100 μg kg−1) with continuous infusion (40 μg kg−1 h−1) from a previous study on morphine pharmacokinetics were analysed using repeated time-to-event (RTTE) modelling.
Results
During the postoperative period (38 h (IQR 23–46)), 130 morphine rescue events (4 (IQR 1–5) per patient) mainly occurred in the first 24 h (107/130) at a median morphine concentration of 29.5 ng ml−1 (range 7–180 ng ml−1). In the RTTE model, the hazard of rescue morphine decreased over time (half-life 18 h; P < 0.001), while the hazard for rescue morphine (21.9% at 29.5 ng ml−1) increased at higher morphine concentrations (P < 0.001).
Conclusions
In this study on protocolized morphine analgesia in children, rescue morphine was required at a wide range of morphine concentrations and further increase of the morphine concentration did not lead to a decrease in hazard. Future studies should focus on a multimodal approach using other opioids or other analgesics to treat breakthrough pain in children.
Impact
-
In children receiving continuous morphine infusion, administration of rescue morphine is an indicator for insufficient effect or an event.
-
Morphine rescue events were identified at a wide range of morphine concentrations upon a standardized pain protocol consisting of continuous morphine infusion and morphine as rescue boluses.
-
The expected number of rescue morphine events was found to increase at higher morphine concentrations. Instead of exploring more aggressive morphine dosing, future research should focus on a multimodal approach to treat breakthrough pain in children.
Similar content being viewed by others
Introduction
Even though opioids are commonly used for pain treatment after major surgery in children, there is no consensus on the type and dose of analgesics to be used. Ineffective postoperative pain management increases the risk of delayed recovery and adverse behavioural and physiological responses.1 A recent international survey of management of pain and sedation after paediatric cardiac surgery showed a large worldwide variability in choice and dosing of analgesics and sedatives after cardiac surgery in children.2 The most commonly used drug was morphine, with a wide variation in continuous infusion dose from 10 to 60 µg kg−1 h−1 in children aged 0–36 months.
The pharmacokinetics (PK) of morphine have been studied extensively across the paediatric population in different kind of settings,3 including cardiac surgery.4,5 Morphine is primarily metabolized through glucuronidation by UGT2B7.6 Elimination of morphine directly reflects the formation of its two pharmacologically active metabolites morphine-3-glucuronide (M3G) and morphine-6-glucuronide (M6G). Even though cardiac surgery is associated with changes in hepatic blood flow and tissue perfusion, no difference was reported in elimination clearance in children after major cardiac surgery compared to non-cardiac surgery.4 Despite all the PK data of morphine, there are only a handful of reports studying morphine pharmacodynamics by relating morphine concentrations to pharmacodynamic endpoints. Two studies investigated the effect of morphine on pain during endotracheal tube suctioning in preterm neonates.7,8 One study did not find a relation between morphine concentrations and changes in heart rate or the preterm infant pain profile, while the other study with the use of Item Response Theory modelling found a weak relationship between morphine concentrations and procedural pain reduction, as established with COMFORT-Behaviour scale (COMFORT-B) and VAS assessments. Recently, Elkomy et al. described the pharmacodynamics of morphine when given as repeated bolus doses in infants and young children after cardiac surgery, by modelling the repeated time-to-event (RTTE) of morphine administration.9 This methodology quantifies the hazard for events, with in this study the hazard being defined as the expected number of rescue morphine doses per hour in an individual patient. Translating these events into a hazard allows us to demonstrate whether factors like time, morphine concentrations or age have impact on the efficacy of morphine reflected by the expected number of rescue doses.
To date, there is a paucity of data on the pharmacodynamics of morphine in young children after cardiac surgery when given as continuous infusion with rescue boluses. The objective of this study is to analyse using RTTE modelling the analgesic efficacy of morphine when given as maintenance and rescue analgesic within the context of a standardized postoperative pain protocol with regular pain and distress measurements.
Methods
Clinical study
Data were collected during an observational, prospective study in 3–36-month-old children, which was performed at the Department of Anaesthesia and Intensive Care Medicine of Our Lady’s Children’s Hospital, Dublin.5 The study protocol was approved by the local ethics committee and written informed consent for the study was obtained from the parents preoperatively. The main results including the population PK analysis of the morphine concentration time samples of 35 children have been reported before.5
In short, patients with and without Down syndrome were included when between 3 and 36 months of age and scheduled for cardiac surgery with cardiopulmonary bypass for atrial septal defect, ventricular septal defect, atrioventricular septal defect or tetralogy of Fallot repair. Exclusion criteria were epilepsy, cerebral palsy or birth asphyxia, history of cardiothoracic surgery through sternotomy, preoperative mechanical ventilation, preoperative treatment with morphine or midazolam and extracorporeal membrane oxygenation treatment after cardiopulmonary bypass.
All patients received standardized anaesthesia during cardiac surgery as well as standardized postoperative pain and distress management guided by pain and distress assessments by the caregiving nurse with a numeric rating scale (NRS) and the COMFORT-B. Morphine was administered as the primary analgesic agent at the end of surgery as a loading dose (100 μg kg−1), followed by a continuous infusion of 40 μg kg−1 h−1. In addition to morphine, intravenous acetaminophen was administered three times daily in the first 24 h after surgery in a dose of 7.5 or 15 mg kg−1, depending on weight (i.e. below or above 10 kg, respectively). In case of unacceptable pain (i.e. score combinations of COMFORT-B > 16 and NRS > 3), additional morphine boluses (20–40 μg kg−1) were administered, and/or morphine maintenance infusion rates were increased. For rescue sedation, midazolam boluses (0.05–0.1 μg/kg) as needed were available. If further escalation for sedation was needed, midazolam infusion (0.06–0.15 mg/kg/h) or enteral chloral hydrate (25–50 mg/kg every 6 h) was started. During the stay at the paediatric intensive care unit (PICU), the morphine dose was gradually decreased. Data collection was stopped when intravenous morphine was switched to oral morphine or on discharge from the PICU. Further details are described in the original article.5
RTTE modelling
In the present study, we used a RTTE model to estimate the hazard for a morphine rescue event during protocolized analgesia after cardiac surgery. The input data for a RTTE analysis consists of the times at which patients experience a morphine rescue event, which was defined as an additional bolus of morphine, an increase in infusion rate of the morphine infusion or a restart of the infusion after a minimum break of 15 min and the times at which patient follow-up stops (i.e. censoring event). Depending on the hazard model, the likelihood (L) of the observed event and censoring data is defined by:
where h(t) is the hazard of needing rescue for an individual patient at the time of the event and cumh(t) is the area under the hazard–time curve between the time of the previous event (or the time of follow-up start if the patient did not experience an event before time t) and the time t (the time of the event or the time of censoring).
Structural hazard model and covariate model
For the structural hazard model, baseline hazard models such as the constant hazard, Gompertz and Weibull models were tested to describe the effect of time after surgery on the hazard throughout the study period.10 In addition, circadian variation of the hazard after surgery was explored.11 Morphine, M3G and M6G concentrations as measured in the participants of the study and published before5 were tested for their influence on the effect on the hazard for a morphine rescue event using immediate or delayed (i.e. with an effect compartment) drug effect models based on Emax or exponential functions. Finally, we explored the influence of covariates age, Down syndrome (yes/no) and mechanical ventilation (yes/no) as predictors of inter-individual variability of the hazard. Potential covariates were tested in the RTTE model using the likelihood ratio test in a stepwise forward inclusion (α = 0.05) and backwards elimination (α = 0.01) procedure.12
Model evaluation
Modelling was performed using NONMEM 7.3. Discrimination between models was made by the likelihood ratio test using the objective function value (OFV, i.e. −2 log likelihood). A decrease of 3.84 in the OFV value between nested models with one degree of freedom, representing a P value of ≤0.05, was considered statistically significant. In addition, the kernel-based visual hazard comparison (kbVHC) was used to evaluate the model’s ability to characterize the mean hazard over time.13 In this method, CVtarget controls the smoothness of the non-parametric hazard estimate of the kbVHC and this was set to 30%.
Results
Clinical study results
An overview of patient characteristics is shown in Table 1. The median age of the 35 children at surgery was 5.7 months (interquartile range (IQR) 4.3–8.3 months). The median postoperative study period at the PICU was 38 h (IQR 23–46). During the first 24 h, the median total dose of morphine was 940 μg kg−1 (IQR 116–183) or 31.3 μg kg−1 h−1 (24–36). On day 2, the median morphine dose was 320 μg kg−1 (IQR 102–524) or 16 μg kg−1 h−1.
Figure 1 illustrates the median individual concentrations of morphine in the children over time. The figure shows that, as a result of the postoperative pain protocol consisting of a loading dose with continuous infusion, the morphine concentrations are the highest directly after surgery and reached steady state after about 200 min. In the first 3–4 h after surgery, morphine concentrations decreased from an average of 60 to 25 ng ml−1 (Fig. 1). Overall, these concentrations are, particularly in the first 24 h, higher than a previously proposed target range for morphine of 10–20 ng ml−1.
The whiskers indicate interquartile range. The number of patients is decreasing over time according to protocol when patients were switched to oral morphine or discharged from the PICU. The grey area indicates an earlier proposed therapeutic range of morphine (10–20 ng ml−1).15 Data were derived from the earlier published PK model5 that was based on the patients of the current study. The median postoperative study period at the PICU was 38 h (IQR 23–46).
Over the study period, a total of 130 rescue morphine events were identified. The majority of events (n = 107) occurred in the first 24 h, while the remaining events (n = 23) were in the second 24 h. A total of 30 (86%) patients received a rescue dose of morphine, with a median of 4 rescue events (IQR 1–5) per patient. Of the 130 rescue events, 114 events (88%) concerned rescue boluses, 9 events (7%) were an increase in infusion rate and 7 patients (5%) received a bolus followed by an increase in infusion rate. Median time between events was 2.6 h (IQR 1.1–4.5 h). Of the 100 events that occurred after a previous event, 24% occurred within 1 h of the previous event. Figure 2 shows the time points of the rescue morphine events with the corresponding morphine concentrations. Median morphine concentrations immediately prior to a rescue event were 29.5 ng ml−1 (IQR 23–43) with a range of 7–180 ng ml−1. In total, 111 (85%) events occurred above a concentration of 20 ng ml−1.
Solid black circle: rescue event that was defined as an additional bolus of morphine, an increase in infusion rate of the morphine infusion, or a restart of the infusion after a minimum break of 15 min. The grey area indicates an earlier proposed therapeutic range of morphine (10–20 ng ml−1).15
RTTE modelling
For the structural model describing the base hazard for a morphine rescue event, a Gompertz model was identified of which the parameters can be found in Table 2. The addition of morphine concentration as a predictor of individual deviations in the hazard resulted in a statistical significant improvement of the model fit (P < 0.001, Table 2). The hazard for rescue morphine increased at higher morphine concentrations (21.9% at the median concentration of 29.5 ng ml−1). Figure 3 illustrates the identified exponential influence of morphine on the hazard showing that only small changes are expected below a morphine concentration of 100 ng ml−1. At higher concentrations, the hazard for rescue medication increases more rapidly; however, the number of observations is small. This results in a wider confidence interval at morphine concentrations >50 ng ml−1, indicating large uncertainty of the obtained function at higher concentrations (Fig. 3). For morphine and metabolite concentrations, adding an effect compartment or other drug effect models (i.e. Emax or exponential) did not improve the model (deltaOFV > 3.84). The model did also not improve significantly when circadian variation or the concentration of M3G or M6G were implemented as predictors for variability (P > 0.05). Covariates such as age, Down syndrome and mechanical ventilation were not identified as a covariate with statistically significant impact on the model fit. The parameter estimates of the final model describing the hazard for rescue morphine in children after cardiac surgery are listed in Table 2.
Figure 4 shows the results of the model validation plot kbVHC, which illustrates that the hazard directly after surgery (HAZbase) decreases over time after surgery (HAZslope, P < 0.001) with a half-life of 18 h. The figure also shows the comparison of the mean individual predicted hazard obtained with the final model versus the non-parametric kernel-based hazard. While the model-predicted and the non-parametric hazard both decreased over time, implying a good description of the data, the peak in the non-parametric hazard at 24 h is not captured well by the model (Fig. 4).
Discussion
In this study, data were analysed from 35 children aged 3–31 months after cardiac surgery who were treated according to a postoperative pain protocol consisting of a morphine loading dose of 100 µg kg−1 at the end of surgery followed by a continuous infusion of 40 µg kg−1 h−1. Morphine rescue doses were given as bolus doses and/or increased continuous infusions. Prior research on the pharmacodynamics has mainly focussed on the relation between morphine concentrations and pain scores, experimental pain models or surrogate endpoints, such as pupil size.14 In contrast, the current analysis uses the administration of rescue morphine as a clinically relevant event or indicator for lack of effect of the current morphine dose. To this end, rescue events were identified and related to the corresponding morphine concentration, which was found to vary widely. RTTE modelling revealed that the hazard for rescue morphine decreased over time and increased when the morphine concentration increased (P < 0.05). Here we discuss the occurrence of rescue events in relation to the morphine concentration, the results of the RTTE analysis and the use of morphine for the treatment of breakthrough pain.
In our study, we identified 130 morphine rescue events during which rescue morphine was given following a standardized pain protocol, which was guided by COMFORT-B and NRS scores. These events of confirmed presence of pain were observed upon a standardized loading dose at the end of surgery followed by a continuous infusion. The concentrations of morphine that were found in this study were relatively high (Fig. 1). Previously, a steady-state target plasma concentration of morphine after major surgery in children and neonates of 10–20 ng ml−1 has been suggested.15 The upper limit of 20 ng ml−1 is mainly based on one study where respiratory effects were reported after morphine infusion (median time of 20 h) in 30 children, aged 2 days to 1.6 years, undergoing cardiac surgery.16 In another study in neonates and infants (0–52 weeks) after abdominal or thoracic surgery, it was concluded that adequate analgesia in neonates was provided with morphine trough concentrations between 15.4 and 22 ng ml−1, whereas this was between 1.0 and 7.5 ng ml−1 for infants older than 4 weeks.17 In the current study, concentrations of morphine were on average >20 ng ml−1, particularly in the first 3–4 h after surgery. Comparing these concentrations is difficult without knowledge on the required target for different surgical procedures and populations. In our study, median morphine concentrations immediately prior to an event were 29.5 ng ml−1 with a range of 7–180 ng ml−1 with the majority of events (n = 111 (85%)) occurring above 20 ng ml−1 (Fig. 2). These results indicate that more morphine is unlikely to reduce the number of events in the patients. It therefore seems that, for now, titrating on effect is the only reasonable advice we can provide. In this respect, it would be interesting to investigate what the role is of individuals who are unlikely to respond to morphine rescue (i.e. non-responders). In other fields of research such as cancer patients or postoperative adult patients, non-response to morphine has been described.18,19,20 The underlying mechanism of non-response is not known nor which patients are more prone to have absence of response to morphine or other opioids.
When focussing on the relationship between morphine concentration and the hazard for events that was analysed using RTTE modelling, we could not identify a reduction in hazard for rescue dosing upon an increase in morphine concentration. On the contrary, we identified an increased hazard for rescue medication upon higher morphine concentrations. However, as Fig. 3 shows, the confidence interval in the steep part of the curve is wide, indicating that the actual increase in hazard as a result of increased morphine concentration could in fact also be small and/or confused by the delay in effect of morphine when given for breakthrough pain resulting in repeated dosages without awaiting the full effect. A recent study by Elkomy et al. investigated the pharmacodynamics of morphine in 20 children between 3 days and 5 years of age after cardiac surgery when using morphine boluses only.9 In their study, a morphine concentration of 19.6 ng ml−1 resulted in a 50% reduction of the hazard for redosing with a wide 95% confidence interval of 5.90–49.5 ng ml−1. The difference between their results and the concentration–effect relationship of morphine in our study might be related to the difference in study design, with Elkomy et al. studying morphine effects without continuous morphine infusion. The results of our study were obtained in the context of a morphine protocol consisting of both continuous and rescue doses, which reflects the current practice of postoperative care in children after cardiac surgery. The wide confidence intervals found for the concentration–effect relation of morphine in the two studies may indicate that the relation between the concentration of morphine and its efficacy is likely not very strong when studied in the direct postoperative phase after cardiac surgery in children. Theoretically, opioid tolerance as well as opioid-induced hyperalgesia could have played a role regarding the hazard that increases with increasing morphine concentrations. However, there are no studies in postoperative cardiac surgery infants that support this hypothesis.
Breakthrough pain is ideally treated by a fast-acting and highly effective analgesic. Our data show that, of the 100 events that occurred after a previous event, 24 (24%) events occurred within 1 h of a previous event. This suggests that many of the rescue morphine dose given during the previous event did not adequately address the pain. In line with these observations, the results of our RTTE analysis demonstrated that an increase in morphine concentration does not result in a decrease in the hazard for rescue events and could even result in an increase in hazard for a rescue event. One explanation for these results could be that morphine has a relatively long time to analgesic action, particularly when compared to short-acting opioids such as fentanyl and alfentanil.21 While the concentration of morphine has been reported to reach its maximum as early as 20 min after intravenous bolus injection, the reported delay between peak blood drug concentration and peak pharmacodynamic effect reflected by a t1/2ke0 is 1.6–3.9 h in volunteers and 1.7 h in postoperative patients, while for alfentanil and fentanyl a much shorter t1/2ke0 (i.e. 1 and 6 min, respectively) has been reported.22,23 Administration of more morphine as rescue treatment within a protocol of a continuous infusion of morphine should therefore be reconsidered, particularly in those cases where multiple rescue events occur within a short time frame. Instead, multimodal strategies should be further explored for the treatment of breakthrough pain in children.24
From these results, it seems that studies aiming improving postoperative pain management should compare different dosing strategies (bolus dose versus increasing continuous infusion rate or both), the use of other opioids for breakthrough pain and/or the use of other non-opioid analgesics, such as nonsteroidal anti-inflammatory drugs25 or acetaminophen. Optimal use of intravenous acetaminophen is currently being studied in combination with or as replacement for morphine with the goal of improving postoperative pain management for children.26
This study has potential limitations. First, this was a single-centre, observational study, which has its known limitations. Second, our analysis rests on the assumption that morphine reliefs pain in infants after cardiac surgery while this topic is still under debate, despite morphine being the most used analgesic after cardiac surgery.2 In addition, the effect of morphine in this study is determined by the events that are identified by nurses giving additional morphine rescue according to their protocol. Therefore, adherence to the pain protocol was of extra importance, while pain assessment in children is generally difficult. In our opinion, this reflects daily practice on the PICU and therefore it is not expected that this substantially influences our conclusions. In addition to this, it may well be that other factors such as requirements for sedation during mechanical ventilation and the treatment of discomfort have played a role. Pain assessment in children can be extremely challenging, and while current measurement instruments like the COMFORT scale are validated,27 it is still difficult to differentiate between pain and agitation or distress in infants. Another limitation is that we could not identify a delay in morphine effect in relation to morphine concentration or a diurnal variation in the hazard that is suggested in the observations (Fig. 4). Finally, the original study design has its own limitations such as unknown impact of altered PK after cardiopulmonary bypass, systemic inflammation, haemodilution, low cardiac output or impaired liver/kidney function. Also, the requirements of inotropics/vasopressors were not noted.5
In conclusion, in this study on protocolized morphine analgesia in children, rescue morphine was required at a wide range of morphine concentrations and further increase of the morphine concentration did not lead to a decrease in hazard. Therefore, future research should focus on a multimodal approach using other opioids or other analgesics to treat breakthrough pain in children.
References
Weisman, S. J., Bernstein, B. & Schechter, N. L. Consequences of inadequate analgesia during painful procedures in children. Arch. Pediatr. Adolesc. Med. 152, 147–149 (1998).
Zeilmaker-Roest, G. A. et al. An international survey of management of pain and sedation after paediatric cardiac surgery. BMJ Paediatr. Open 1, e000046 (2017).
Krekels, E. H., Tibboel, D., Danhof, M. & Knibbe, C. A. Prediction of morphine clearance in the paediatric population: how accurate are the available pharmacokinetic models? Clin. Pharmacokinet. 51, 695–709 (2012).
Elkomy, M. H. et al. Pharmacokinetics of morphine and its metabolites in infants and young children after congenital heart surgery. AAPS J. 18, 124–133 (2016).
Valkenburg, A. J. et al. Pharmacodynamics and pharmacokinetics of morphine after cardiac surgery in children with and without Down syndrome. Pediatr. Crit. Care Med. 17, 930–938 (2016).
Coffman, B. L., Rios, G. R., King, C. D. & Tephly, T. R. Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab. Dispos. 25, 1–4 (1997).
Anand, K. J. et al. Morphine pharmacokinetics and pharmacodynamics in preterm and term neonates: secondary results from the NEOPAIN trial. Br. J. Anaesth. 101, 680–689 (2008).
Valitalo, P. A. et al. Morphine pharmacodynamics in mechanically ventilated preterm neonates undergoing endotracheal suctioning. CPT Pharmacometrics Syst. Pharmacol. 6, 239–248 (2017).
Elkomy, M. H. et al. Pharmacodynamic analysis of morphine time-to-remedication events in infants and young children after congenital heart surgery. Clin. Pharmacokinet. 55, 1217–1226 (2016).
Juul, R. V. et al. Repeated time-to-event analysis of consecutive analgesic events in postoperative pain. Anesthesiology 123, 1411–1419 (2015).
Junker, U. & Wirz, S. Influence of circadian rhythms on the therapy of severe pain. J. Oncol. Pharm. Pract. 16, 81–87 (2010).
Hutmacher, M. M. & Kowalski, K. G. Covariate selection in pharmacometric analyses: a review of methods. Br. J. Clin. Pharmacol. 79, 132–147 (2015).
Goulooze, S. C., Valitalo, P. A. J., Knibbe, C. A. J. & Krekels, E. H. J. Kernel-based visual hazard comparison (kbVHC): a simulation-free diagnostic for parametric repeated time-to-event models. AAPS J. 20, 5–9 (2017).
Martini, C. et al. Pharmacokinetic-pharmacodynamic modeling in acute and chronic pain: an overview of the recent literature. Expert Rev. Clin. Pharmacol. 4, 719–728 (2011).
Anderson, B. J. & Holford, N. H. in Pain in Neonates and Infants: Pain Research and Clinical Management Series (eds Anand, K. J., Stevens, P. B. & McGrath, P.) 128 (Elsevier, 2009).
Lynn, A. M., Nespeca, M. K., Opheim, K. E. & Slattery, J. T. Respiratory effects of intravenous morphine infusions in neonates, infants, and children after cardiac surgery. Anesth. Analg. 77, 695–701 (1993).
Bouwmeester, N. J. et al. Age- and therapy-related effects on morphine requirements and plasma concentrations of morphine and its metabolites in postoperative infants. Br. J. Anaesth. 90, 642–652 (2003).
Roberts-Thomson, I. C., Jonsson, J. R., Pannall, P. R. & Frewin, D. B. Morphine responders with unexplained pain after cholecystectomy may have sympathetic overactivity. Clin. Auton. Res 1, 59–62 (1991).
Riley, J. et al. No pain relief from morphine? Individual variation in sensitivity to morphine and the need to switch to an alternative opioid in cancer patients. Support Care Cancer 14, 56–64 (2006).
Gram, M. et al. Prediction of postoperative opioid analgesia using clinical-experimental parameters and electroencephalography. Eur. J. Pain 21, 264–277 (2017).
Aubrun, F., Mazoit, J.-X. & Riou, B. Postoperative intravenous morphine titration. Br. J. Anaesth. 108, 193–201 (2012).
Mazoit, J. X., Butscher, K. & Samii, K. Morphine in postoperative patients: pharmacokinetics and pharmacodynamics of metabolites. Anesth. Analg. 105, 70–78 (2007).
Lötsch, J. Pharmacokinetic-pharmacodynamic modeling of opioids. J. Pain. Symptom Manag. 29, S90–S103 (2005).
Duedahl, T. H. & Hansen, E. H. A qualitative systematic review of morphine treatment in children with postoperative pain. Paediatr. Anaesth. 17, 756–774 (2007).
Saini, A., Maher, K. O. & Deshpande, S. R. Nonopioid analgesics for perioperative and cardiac surgery pain in children: current evidence and knowledge gaps. Ann. Pediatr. Cardiol. 13, 46–55 (2020).
Zeilmaker-Roest, G. A. et al. Intravenous morphine versus intravenous paracetamol after cardiac surgery in neonates and infants: a study protocol for a randomized controlled trial. Trials 19, 318 (2018).
van Dijk, M. et al. The reliability and validity of the COMFORT scale as a postoperative pain instrument in 0 to 3-year-old infants. Pain 84, 367–377 (2000).
Acknowledgements
The authors thank Cormac V Breatnach, Department of Anaesthesia and Critical Care Medicine, Our Lady’s Children’s Hospital, Dublin, Ireland for his contribution to the original study and Ko Hagoort, Department of Pediatric Surgery, Erasmus MC-Sophia Children’s Hospital, Rotterdam, The Netherlands for text editing. No financial support has been received for this study.
Author information
Authors and Affiliations
Contributions
S.d.H., S.C.G., A.J.V.: substantial contributions to overall concept design, data acquisition, analysis and interpretation, article revision, and final approval. E.H.J.K., M.v.D., D.T., C.A.J.K.: substantial contributions to overall concept design, data interpretation, article revision, and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Written informed consent for the study was obtained from the parents preoperatively.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
de Hoogd, S., Goulooze, S.C., Valkenburg, A.J. et al. Postoperative breakthrough pain in paediatric cardiac surgery not reduced by increased morphine concentrations. Pediatr Res 90, 1201–1206 (2021). https://doi.org/10.1038/s41390-021-01383-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01383-z