Abstract
Background
We aimed to assess remote ischemic postconditioning (RIPC) as a neuroprotective strategy after perinatal hypoxia–ischemia (HI) in a piglet model.
Methods
Fifty-four newborn piglets were subjected to global HI for 45 min. One hour after HI, piglets were randomized to four cycles of 5 min of RIPC or supportive treatment only. The primary outcome was brain lactate/N-acetylaspartate (Lac/NAA) ratios measured by magnetic resonance spectroscopy at 72 h. Secondary outcomes included diffusion-weighted imaging and neuropathology.
Results
RIPC was associated with a reduction in overall and basal ganglia Lac/NAA ratios at 72 h after HI, but no effect on diffusion-weighted imaging, neuropathology scores, neurological recovery, or mortality.
Conclusions
The selective effect of RIPC on Lac/NAA ratios may suggest that the metabolic effect is greater than the structural and functional improvement at 72 h after HI. Further studies are needed to address whether there is an add-on effect of RIPC to hypothermia, together with the optimal timing, number of cycles, and duration of RIPC.
Impact
-
RIPC after HI was associated with a reduction in overall and basal ganglia Lac/NAA ratios at 72 h, but had no effect on diffusion-weighted imaging, neuropathology scores, neurological recovery, or mortality.
-
RIPC may have a selective metabolic effect, ameliorating lactate accumulation without improving other short-term outcomes assessed at 72 h after HI.
-
We applied four cycles of 5 min RIPC, complementing existing data on other durations of RIPC.
-
This study adds to the limited data on RIPC after perinatal HI and highlights that knowledge gaps, including timing and duration of RIPC, must be addressed together with exploring the combined effects with hypothermia.
Similar content being viewed by others
Introduction
The incidence of neonatal encephalopathy (NE) due to perinatal hypoxia–ischemia (HI) is between 1.5 and 8 per 1000 live births,1 and some 1.15 million babies suffer from NE annually worldwide. The mortality is 10–50%, and NE survivors have a 40% risk of neurodevelopmental impairment.2 NE caused by HI is referred to as hypoxic–ischemic encephalopathy (HIE). Therapeutic hypothermia (TH) is the only treatment option for HIE other than supportive care.
Neuroprotection by TH was initially shown in a piglet model, and because of similarities in brain development and cardiovascular system between piglets and humans, the piglet is a good model for clinical HIE. Piglet studies demonstrated that TH was accompanied by up to 50% reduction in injuries of the cortex, white matter (WM), cerebellum, and hippocampus following moderate, but not severe, HI insults.3 Cochrane meta-analysis of 11 randomized controlled clinical trials found a relative risk reduction of 25% for death or major disability with TH, with number needed to treat of 7.4 However, despite TH many infants with HIE still die or survive with major disabilities. Part of this treatment gap may be explained by the fact that HIE is a clinically heterogeneous condition. In the Cochrane meta-analysis, the effect of TH was more pronounced in moderate HIE than in severe HIE. It has further been speculated that the effect of TH is abolished by inflammation, coexisting in many newborns with HIE. Importantly, controlled TH may not be available to the estimated 96% of affected infants born in low- and middle-income countries.2 Thus, development of both add-on and less complicated neuroprotective strategies remains important.
Remote ischemic postconditioning (RIPC) is suggested to be a potent activator of endogenous protection after HI. RIPC refers to transient repeated remote limb skeletal muscle ischemia, initiated after a hypoxic–ischemic insult. The protective effects of RIPC are thought to be mediated via neuronal, humoral, and systemic pathways and result in changes in gene expression and cellular function.5 RIPC for HIE in a rat study significantly reduced infarct volume at 48 h and improved functional outcomes at 4 weeks.6 A piglet study of RIPC after neonatal HI induced by carotid artery occlusion and hypoxia found preferential cerebral WM protection by magnetic resonance spectroscopy (MRS) with increased cell survival in the corpus callosum, internal capsule, and periventricular WM following RIPC.7
To substantiate the limited data on the neuroprotective effects of RIPC after HI, we set out to study RIPC in a piglet model of global HI. The aim of this study was to compare the effect of RIPC vs. supportive treatment on brain injury caused by HI. Outcome measures were clinically used bridging biomarkers of cerebral MRS8 and diffusion-weighted MR imaging together with neuropathology at 72 h after HI.
Methods
Ethics statement
The study was conducted under the Danish Animal Experiments Inspectorate license (2012–15–2934–00036) in accordance with national ethics and animal welfare guidelines. Reporting complies with ARRIVE guidelines for reporting of bioscience research.9
Study design
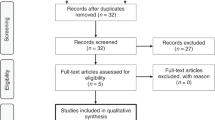
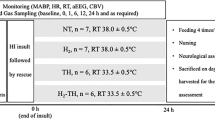
The study was designed as a randomized controlled experiment (Fig. 1). Animal technicians caring for the animals were blinded to randomization group at all times. Investigators were blinded to randomization group when assessing outcomes. Fifty-four piglets were included in the experiment. Fifty piglets were exposed to global HI. One hour after the end of HI, they were randomized with an allocation ratio of 1:1 to either RIPC (HI + RIPC, n = 25) or supportive treatment only (HI, n = 25) in randomly sized blocks of 4–8. Sham controls (Sham, n = 4) were exposed to the experimental protocol, but without HI.
Sample size
Sample size was calculated for the outcome of MRS. Previous neuroprotection studies in HI piglet models have suggested a difference in lactate/N-acetylaspartate (Lac/NAA) ratio between groups randomized to normothermia and hypothermia by 1.0 U with a standard deviation of 0.75 U (log scale), that is, an effect size as measured by MRS in the order of 1.3 times the standard deviation (SD).10 Based on pilot experiments, we expected an effect in the order of 1.0 SD. For detection of a difference between groups of 1.0 SD with a 5% two-sided significance level and 80% power, 22 animals were needed in each group. To allow for 10% attrition, we opted for n = 25 in each group.
Experimental animal preparation
Newborn Danish Landrace piglets of both sexes were anesthetized and subjected to a global HI insult as previously described.11,12,13 Studies were started at 8 a.m. Anesthesia was initiated with sevoflurane (Air Liquide, France), minimum alveolar concentration 1–2% in air delivered via a mask, followed by intravenous bolus injections of propofol 5 mg/kg, fentanyl 10 µg/kg, and rocuronium 1 mg/kg for intubation. Sevoflurane was discontinued after intubation and maintenance anesthesia given by continuous intravenous (i.v.) infusion of propofol (4–12 mg/kg/h) and fentanyl (10 μg/kg/h), and then weaned in the hours after HI. Mechanical ventilation settings were adjusted to maintain partial arterial pressure of CO2 between 4.5 and 5.5 kPa. Umbilical venous 5 Fr and arterial 3.5 Fr catheters were placed. The umbilical venous catheter was used for fluid and drug administration. An i.v. infusion of 5% dextrose with 0.45% NaCl was started at 10 ml/kg/h. During and after HI, the infusion rate was reduced to 5 ml/kg/h and adjusted to maintain blood glucose between 3 and 10 mmol/L. Procaine benzylpenicillin (15.000 IU/kg, subcutaneously (s.c.)) was given once daily. A probe measuring oxygen saturation was placed on a leg. The piglet was placed in the supine position on a heated inflatable air mattress to maintain a normal rectal temperature at 38.5 ± 0.5 °C. Electrocardiogram electrodes were placed for continuous heart rate monitoring. Mean arterial blood pressure (MABP) was measured continuously using the arterial umbilical catheter. Arterial blood gases (PaO2 (partial pressure of oxygen), PaCO2 (partial pressure of carbon dioxide), pH, standard base excess) and serum electrolytes, blood glucose, and lactate were analyzed at baseline, after 30 min of HI, at the end of 45 min HI, 3 h after HI start, and 72 h after HI start (Radiometer Medical, Denmark). A single-channel biparietal amplitude-integrated electroencephalography (aEEG) was continuously recorded during HI, the recovery period, and again at day 3 (Niculet monitor, Natus Medical Incorporated, USA).
Global HI
Piglets were allowed to stabilize for 60 min prior to HI. Global hypoxia was induced over a 45-min period by switching to a 4% O2/96% N2 gas mixture (Air Liquide, France) and lowering the respiratory rate to 16 to further decrease both the mean airway pressure and the oxygenation, while also decreasing CO2 removal to mimic the universal decrease in gas exchange in a perinatal HI event. Once the aEEG trace upper margin was below 7 µV, oxygenation (FiO2 and mean airway pressure) was adjusted to the level of oxygen maintaining the aEEG trace between 3 and 5 µV. Similar to clinical HI characteristics, the global hypoxia in this model resulted in cardiovascular depression and hypotension producing an HI insult. We aimed for 10 min with MABP below 70% of the baseline. In case of severe hypotension (MABP <25 mmHg), the piglet was treated stepwise by briefly increasing FiO2 by 1–5%, saline bolus (10 ml/kg), infusion of dopamine (5–20 μg/kg/min). After 45 min, FiO2 was increased to 21%, and if oxygen saturations remained <95%, FiO2 was increased up to 30% as needed. The time with aEEG <7 µV within the 45 min of HI was recorded. Seizures (clinical or electroencephalographic lasting >10 min) were treated with phenobarbitone 20 mg/kg, repeat phenobarbitone 20 mg/kg, and midazolam 0.5 mg/kg.
Remote ischemic postconditioning
RIPC was induced 1 h after HI by occluding blood flow to both hind limbs using an external plastic strip for 5 min, followed by 5 min reperfusion repeated for a total of four cycles of occlusion/reperfusion.14 The strip was tightened until complete occlusion of arterial blood flow was verified by Doppler ultrasound, indicating supra-systolic pressure. The exact pressure applied by the plastic strip was not measured.
Seventy-two-hour survival period
Anesthesia was weaned after HI, and piglets were extubated when sufficient breathing effort was present. Piglets with persistent flat aEEG tracing, no spontaneous breathing, and a neurological score of 0–2 (see “Functional assessment” below) after discontinuation of anesthesia were considered brain dead, and were euthanized prior to 72 h. During the survival period, piglets were kept in pairs at an animal facility with surveillance at all times. They received fluids equivalent to 5–10 ml/kg/h either by bottle-feeding every 3 h or by i.v. 10% dextrose infusions if unable to bottle-feed.
Magnetic resonance imaging and MRS
At 72 h after HI, piglets were anesthetized using the same protocol as day 1 for magnetic resonance imaging (MRI)/MRS using a clinical 3 Tesla system (Siemens Medical Systems). A scout T2-weighted spin-echo sequence was initially employed to locate the brain and was used to prepare subsequent sequences. Next, a diffusion-weighted spin-echo sequence with fat saturation encoding was employed (parameters: field of view = 160 × 160 mm2, resolution = 1.1 × 1.1 × 3.0 mm3, repetition time (TR) = 3300 ms, echo time (TE) = 108 ms, and diffusion b values = 0 and 800 s/mm2). A decrease in the apparent diffusion coefficient (ADC) reflects cellular swelling. A STEAM (stimulated echo acquisition mode)-based fat-saturated spectroscopy protocol was employed to measure the intracerebral metabolites (parameters: voxel of interest = 8 × 8 × 8 mm3, TR = 2000 ms, TE = 135 ms, and repetitions = 128). After zero-filling, multiplication with a filter, and eddy-current correction, signal intensities of lactate and NAA were measured from the proton spectra of metabolites. MRI and MRS quantitative measures were calculated using Mistar (Apollo Imaging Technology, Melbourne, Australia) and Siemens Syngo (Siemens Medical Systems). Based on previous studies15 and clinical relevance,16 regions of interest were basal ganglia (BG), thalamus (TH), and WM. The mean value of the specific area bilaterally was calculated for each piglet and used as the measure for statistical analysis. Image data was analyzed without knowledge of the randomization category of the piglets.
Neuropathology
Piglets were euthanized with a lethal dose of pentobarbital following brain imaging. The brain was removed from the skull and fixed by immersion in 4% paraformaldehyde in phosphate-buffered saline. Coronal paraffin-embedded blocks from the formalin-fixed brain tissue were sectioned at 5 μm and stained with hematoxylin and eosin. BG, TH, hippocampus, cerebellum, brainstem, and cortex were examined. Tissue sample evaluations were performed or supervised by an experienced neuropathologist blinded to the treatment group. Irreversibly damaged neurons were identified by a clearly eosinophilic cytoplasm and a pyknotic hyperchromatic nucleus with condensed chromatin. These changes were distinguished from “dark neurons” representing artifacts caused by fixation.17 The extent of damage in each region was graded on a 9-step scale (between 0 and 4 and intervals of 0.5), using a previously published grading system.18
Functional assessment
Piglets were neurologically evaluated using a modified version of a previously published scoring system18 at baseline, after extubation, and at 24, 48, and 72 h. Piglets were scored in 11 areas, each with a score of 0–2, resulting in a scale from 0 to 22 points, with 22 being the optimal score in a healthy animal. During scoring, the piglet was observed/filmed (1) in active state, if possible standing, walking, and feeding; (2) laid supine to see how it rights itself (righting reflex function); (3) during gentle stimulation by the caretaker. For each of the 11 areas, a score of 2 was given for normal behavior, 1 for mildly abnormal, 0.5 for moderately abnormal, and 0 for very abnormal. Neurological areas scored were: (1) normal respiration, without apnea, retractions, or need for supplemental oxygen; (2) consciousness; (3) orientation. Looking around and investigating the surroundings; (4) ability to walk on all four limbs in one direction without falling; (5) use of forelimbs to rise from lying position; (6) use of hind limbs to rise from lying position; (7) tone steady and equal in hind- and forelimbs; (8) almost continuous activity when awake; (9) sucking; (10) vocalization; (11) pathological movements (2: none; 1: occasional cycling movements or jerks; 0: sustained clonic movements or tonic postures).
Statistics
Two-sided p values for difference between groups were calculated with Student’s t test, one-way ANOVA (analysis of variance) (normally distributed data: physiologic parameters and Lac/NAA ratios), Mann–Whitney test (non-normally distributed data: ADC values, neuropathology, and functional scores), or Fischer’s exact test (dichotomous survival data). The level of significance was set at a two-sided p < 0.05. Datasets were tested for normality prior to analysis. Neuropathology data was missing for two animals, and MRS data from 14 of 15 dead/brain-dead animals. The n for each outcome is specified under “Results,” disregarding missing values from dead animals, as changes in the brain of dead animals cannot be predicted. Two piglets without available outcome data were excluded due to equipment failure, resulting in extended HI and temperature deregulation, respectively. Stata version 14.1 was used for all analyses.
Results
Baseline data, physiologic variables, and HI insult
Treatment groups were comparable at baseline with respect to postnatal age, weight, sex, physiological, and biochemical measures (Table 1). Insult severity measured as duration of aEEG <7 μV and MABP <70% of baseline, and arterial pH at the end of HI was also similar between groups. After HI, piglets treated with RIPC had a lower blood lactate at 72 h (2.2 ± 1.1 vs. 3.5 ± 1.3 (mean ± SD), p = 0.01). All other physiologic and biochemical values were similar between treatment groups after HI when measured at 2, 2–12, and 72 h. Use of volume replacement, inotropes, and phenobarbitone after HI did not differ between groups. Induction of RIPC by occlusion with plastic strips uniformly resulted in complete occlusion of arterial blood flow measured by Doppler ultrasound. No unintended reperfusion during the 5-min periods of RIPC was seen, and no limb injury was observed with RIPC.
Magnetic resonance spectroscopy
Brain Lac/NAA ratios were lowest in the sham controls. Lac/NAA ratios in the HI + RIPC group (n = 18) vs. HI group (n = 16) were lower for the average of all brain areas assessed (brain average) (p = 0.02) and BG (p = 0.03), while there was no statistically significant difference for TH or WM (Fig. 2).
Diffusion-weighted MRI
Brain edema results in lower ADC values. ADC values were highest in sham animals and lower in animals subjected to HI, but with no differences between HI + RIPC (n = 18) and HI groups (n = 16) (Fig. 3).
Neuropathology
Sham piglets did not show brain injury. Following HI, 85% of all piglets showed brain injury by histology, but with no differences between HI + RIPC (n = 24) and HI groups (n = 22). Results from individual brain areas are shown in Fig. 4. The highest pathology scores were found in the hippocampus, cerebellum, and cortex. The most damaged neurons in the cerebellum were the Purkinje cells, whereas it was the CA1 and CA3 pyramidal neurons in the hippocampus. In the cortex, the most damaged areas were found at the base of the sulci supplied by end arteries. The most severe damage caused neurons to disappear leaving a vacuolated area. Representative images for pathology grades 2 to 4 are shown in Fig. 5.
Grade 1: <10% of the areas are affected by complete or incomplete infarcts. Grade 2: 20–30% affected. Partly confluent complete or incomplete infarcts. Grade 3: 40–60% large confluent complete infarcts. Grade 4: >75% in the cortex: total disintegration of the tissue, in the thalamus and basal ganglia; large complete infarcts, in the hippocampus; neuronal necrosis.18 a Grade 2 in the cerebral cortex, at the base of the sulcus. An area with eosinophilic neurons (circle). b Grade 3 in the cerebellar hemisphere. Some of the Purkinje neurons have disappeared and others have eosinophilic cytoplasm and pyknotic nuclei (arrow). c Grade 4 in the cerebral cortex, at the base of the sulcus. Almost all neurons are eosinophilic, and a large number have disappeared. d Grade 4 in the hippocampus. All CA1 and CA3 pyramidal neurons are eosinophilic. Scale bar: 100 µm.
Mortality
Mortality in the HI + RIPC group was 6/24 (25%) vs. 9/24 (37.5%) in the HI group, with no statistically significant difference between groups (p = 0.53). Causes of death in the two groups did not differ: brain death/flat trace aEEG (HI = 4, HI + RIPC = 2), insufficient respiratory drive (HI = 4, HI + RIPC = 3), and other (HI = 1, HI + RIPC = 1).
Neurological assessment
Sham controls had normal neuroscores of 22 before and after anesthesia. In all animals exposed to HI, neuroscores were lowest immediately after extubation, and then increased over time. Neuroscores did not differ between the HI + RIPC (baseline n = 24, 72 h n = 18) and HI (baseline n = 24, 72 h n = 15) group at any time point (Fig. 6).
Discussion
Four cycles of 5 min of RIPC applied to the lower limbs of newborn piglets was a simple and safe intervention, with no local or systemic adverse events. The main finding of this study was that RIPC was associated with a reduction in average Lac/NAA and BG Lac/NAA ratios. No difference after RIPC was seen for diffusion-weighted imaging, neuropathology, functional assessment, or mortality. This may suggest a selective effect of RIPC where the metabolic effect is greater than the structural and functional improvement. A possible explanation is that RIPC may rescue cells on the verge of survival, whereas cellular structural injury will manifest itself regardless of attempts to intervene. However, a number of limitations must be taken into account when interpreting the results. To increase translatability, there has been a call for animal studies with behavioral long-term outcomes.19 In the absence of this, we chose Lac/NAA ratios at 72 h as the main outcome. While brain injury evolves beyond 72 h, MRS of the BG and TH is currently considered the best known early bridging biomarker for neurodevelopmental outcome.8,20 The evolving nature of HI brain injury means that the timing of assessment of short-term outcomes is crucial. The optimal timing for evaluating lactate accumulation, diffusion changes, and histologic changes may not be identical, which complicates interpretation of results and warrants further investigation. While the Lac/NAA ratios found in this study capture a range of neurological injury, we speculate that at 72 h, there may have been a pseudo-normalization of ADC values, making it difficult to discriminate different levels of injury. Likewise, in this study, the scale used for neuropathological injury may not capture subtle differences as data were very skewed, making it difficult to interpret the median value of injury.
We chose the piglet because brain growth and brain maturation is a good model for that of the human newborn. Still, translating results from RIPC animal studies to the human population raises a number of questions, for example, how powerful should the RIPC stimuli be in terms of one or more extremities, duration of each cycle, and number of cycles? We tested early RIPC at 1 h after HI, and chose four cycles of 5 min based on the RIPC literature on adult humans. Delays in treatment initiation may be caused by prolonged resuscitation, in or between hospital transfers, or obtaining parental consent. The average time of randomization in RCTs of TH was 4.5 to 5.5 h,4 and in the Toby-Xe trial, ventilation with xenon was started at a median of 10 h.21 Thus, while RIPC is a simple, mechanical intervention, a delay of several hours may occur in the clinical setting and should be considered in the design of future studies. There are indications that RIPC initiated later or repeated RIPC may have protective properties.22 Whereas RIPC will always be postnatal, timing, duration, and intensity of the HI insult may vary in the clinical situation. An HIE rat study found that delayed RIPC initiated 24 h after HI failed to attenuate neuropathological brain injury, but improved long-term sensory motor deficits at 5 weeks after HI.23 Thus, later treatment in cases where HIE was not initially treated may also be a possibility.
RIPC has been proposed to act via the opioid receptor/Akt pathway.6 Therefore, the use of fentanyl may have abolished some of the RIPC effect. Also, a study on cardioprotection in a perfused rat heart model suggested an additive effect of sevoflurane and RIPC.14 The use of various anesthetics may thus in itself be neuroprotective, and obscure the effect of RIPC. To minimize this possible confounding effect, mechanical ventilation and anesthesia was weaned in the hours after HI, resulting in the shortest possible duration of anesthesia. Four sham animals were included to investigate the effects of supportive care, including anesthesia and mechanical ventilation. Sham animals had pathology scores of 0 and uniformly low Lac/NAA ratios compared to HI and HI + RIPC animals. The same was the case for ADC values, which were highest in the sham animals, and within a narrow range. There was no indication that supportive care in this model caused brain injury in itself, but the small number of sham animals did not allow for formal statistical comparison. All piglets were normothermic at 2–12 and 72 h after HI, but temperature was not documented between 12 and 72 h, and it is possible that secondary hypothermia or pyrexia or both in the interim period may have caused interaction effects. Similarly, due to practical limitations, there were no aEEG recordings during recovery. The proportion of bottle-fed animals in each group during recovery would have been a useful supplement to functional evaluation, but was not registered as it was not a yes or no phenomenon.
The strength of our model is the induction of global HI, allowing for the multi-organ influence, which will accompany HIE in most clinical situations, which again may impact on the resulting brain injury. Global hypoxia, if sufficiently severe, leads to ischemia and mimics the clinical acute interruption of fetal gas exchange in, for instance, placental abruption, uterine rupture, umbilical cord prolapse, and other acute obstetric events, rather than the regional ischemia potentially induced by animal models combining hypoxia with vessel occlusion.7,10 The model’s external validity is supported by the successful translation of TH from piglet studies to clinical guidelines.24
Ischemia–reperfusion injury is common in a variety of clinical conditions, including HIE, myocardial infarction, stroke, and procedures such as organ transplantation, where blood flow is interrupted. Reperfusion results in oxidative stress adding to the pathology from the initial HI, and innate defense mechanisms exist to ameliorate injury. RIPC has emerged as a strategy for neuroprotection after stroke25 and improves motor and cognitive outcomes in a rodent model of germinal matrix hemorrhage.26 Our findings in newborn HI are supported by a study of RIPC, where both common carotid arteries were occluded in combination with a milder hypoxic insult starting at 6% oxygen and increasing.7 In that study, RIPC reduced WM Lac/NAA, increased cell survival measured by TUNEL (terminal deoxynucleotidyl transferase dUTP nick-end labeling) staining, and resulted in higher whole-brain nucleotide triphosphate/exchangeable phosphate pool by MRS, indicating improved mitochondrial metabolism after RIPC.7 The same study found preferential WM protection, possibly related to the preservation of vascular watershed areas most susceptible to ischemia from compromised arterial perfusion. However, a follow-up study addressing oxidative stress found that RIPC reduced nitrotyrosine deposits across the brain, showing both gray and WM protection in moderate HI.27
A majority of infants suffering from NE do so in low- and middle-income countries, where administering TH may be difficult.28,29 In addition to the practical difficulties, which will also make the implementation of early RIPC challenging, infants with NE typically develop spontaneous hypothermia for varying periods.30 It has also been proposed that the neuroprotective effect of TH may be diminished in inflammation-sensitized HI.31 Other situations where TH may be harmful include severe persistent pulmonary hypertension, thrombocytopenia, and other conditions with increased bleeding tendency. Add-on interventions such as RIPC may have greater impact on neuroprotection in these settings. However, RIPC must first be tested in combination with TH to address whether there is an additive neuroprotective effect.
In conclusion, we found that early RIPC was associated with a reduction in overall and BG Lac/NAA, but no effect on diffusion-weighted imaging, neuropathology scores, or neurological recovery measured at 72 h after HI. RIPC should be further investigated for the potential benefits as an add-on treatment to TH. Future directions of research include the knowledge gaps identified above, including timing and duration of RIPC.
References
Kurinczuk, J. J., White-Koning, M. & Badawi, N. Epidemiology of neonatal encephalopathy and hypoxic–ischaemic encephalopathy. Early Hum. Dev. 86, 329–338 (2010).
Lee, A. C. et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr. Res. 74(Suppl. 1), 50–72 (2013).
Haaland, K., Loberg, E. M., Steen, P. A. & Thoresen, M. Posthypoxic hypothermia in newborn piglets. Pediatr. Res. 41, 505–512 (1997).
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. 1, CD003311 (2013).
Hassell, K. J., Ezzati, M., Alonso-Alconada, D., Hausenloy, D. J. & Robertson, N. J. New horizons for newborn brain protection: enhancing endogenous neuroprotection. Arch. Dis. Child. Fetal neonatal Ed. 100, F541–F552 (2015).
Zhou, Y. et al. Remote limb ischemic postconditioning protects against neonatal hypoxic–ischemic brain injury in rat pups by the opioid receptor/Akt pathway. Stroke 42, 439–444 (2011).
Ezzati, M. et al. Immediate remote ischemic postconditioning after hypoxia ischemia in piglets protects cerebral white matter but not grey matter. J. Cereb. Blood Flow Metab. 36, 1396–1411 (2015).
Groenendaal, F. & de Vries, L. S. Fifty years of brain imaging in neonatal encephalopathy following perinatal asphyxia. Pediatr. Res. 81, 150–155 (2017).
Kilkenny, C., Browne, W. J., Cuthi, I., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. Vet. Clin. Pathol. 41, 27–31 (2012).
Faulkner, S. et al. Xenon augmented hypothermia reduces early lactate/N-acetylaspartate and cell death in perinatal asphyxia. Ann. Neurol. 70, 133–150 (2011).
Kyng, K. J. et al. A Piglet model of neonatal hypoxic–ischemic encephalopathy. J. Vis. Exp. 99, e52454 (2015).
Bjorkman, S. T. et al. Hypoxic/ischemic models in newborn piglet: comparison of constant FiO2 versus variable FiO2 delivery. Brain Res. 1100, 110–117 (2006).
Foster, K. A. et al. An improved survival model of hypoxia/ischaemia in the piglet suitable for neuroprotection studies. Brain Res. 919, 122–131 (2001).
Zhou, C., Li, H., Yao, Y. & Li, L. Delayed remote ischemic preconditioning produces an additive cardioprotection to sevoflurane postconditioning through an enhanced heme oxygenase 1 level partly via nuclear factor erythroid 2-related factor 2 nuclear translocation. J. Cardiovasc. Pharm. Ther. 19, 558–66. (2014).
Alderliesten, T., de Vries, L. S., Benders, M. J., Koopman, C. & Groenendaal, F. MR imaging and outcome of term neonates with perinatal asphyxia: value of diffusion-weighted MR imaging and (1)H MR spectroscopy. Radiology 261, 235–242 (2011).
Boichot, C. et al. Term neonate prognoses after perinatal asphyxia: contributions of MR imaging, MR spectroscopy, relaxation times, and apparent diffusion coefficients. Radiology 239, 839–848 (2006).
Jortner, B. S. The return of the dark neuron. A histological artifact complicating contemporary neurotoxicologic evaluation. Neurotoxicology 27, 628–634 (2006).
Thoresen, M. et al. A piglet survival model of posthypoxic encephalopathy. Pediatr. Res. 40, 738–748 (1996).
Robertson, N. J. et al. Which neuroprotective agents are ready for bench to bedside translation in the newborn infant? J. Pediatr. 160, 544–552. e4 (2012).
Thayyil, S. et al. Cerebral magnetic resonance biomarkers in neonatal encephalopathy: a meta-analysis. Pediatrics 125, e382–e395 (2010).
Azzopardi, D. et al. Moderate hypothermia within 6 h of birth plus inhaled xenon versus moderate hypothermia alone after birth asphyxia (TOBY-Xe): a proof-of-concept, open-label, randomised controlled trial. Lancet Neurol. 15, 145–153 (2016).
Wei, M. et al. Repeated remote ischemic postconditioning protects against adverse left ventricular remodeling and improves survival in a rat model of myocardial infarction. Circ. Res. 108, 1220–1225 (2011).
Drunalini Perera, P. N. et al. Delayed remote ischemic postconditioning improves long term sensory motor deficits in a neonatal hypoxic ischemic rat model. PLoS ONE 9, e90258 (2014).
Committee on F. et al. Hypothermia and neonatal encephalopathy. Pediatrics 133, 1146–1150 (2014).
Zhao, H. Ischemic postconditioning as a novel avenue to protect against brain injury after stroke. J. Cereb. Blood Flow. Metab. 29, 873–885 (2009).
Lekic, T. et al. Remote ischemic postconditioning (RIPC) after GMH in rodents. Acta Neurochir. Suppl. 121, 63–67 (2016).
Rocha-Ferreira, E. et al. Immediate remote ischemic postconditioning reduces brain nitrotyrosine formation in a piglet asphyxia model. Oxid. Med. Cell Longev. 2016, 5763743 (2016).
Lawn, J. E., Cousens, S. & Zupan, J. Lancet neonatal survival steering T. 4 million neonatal deaths: When? Where? Why? Lancet 365, 891–900 (2005).
Thayyil, S. et al. Hypothermia for encephalopathy in low and middle-income countries (HELIX): study protocol for a randomised controlled trial. Trials 18, 432 (2017).
Enweronu-Laryea, C. et al. Core temperature after birth in babies with neonatal encephalopathy in a sub-Saharan African hospital setting. J. Physiol. 597, 4013–4024 (2019).
Osredkar, D. et al. Hypothermia is not neuroprotective after infection-sensitized neonatal hypoxic–ischemic brain injury. Resuscitation 85, 567–572 (2014).
Acknowledgements
This study was supported by the Lundbeck Foundation, the Laerdal Foundation for Acute Medicine, the Central Denmark Region’s Research Foundation, the Augustinus Foundation, Aase and Ejnar Danielsens Foundation, Aarhus University Research Foundation, Brødrene Hartmanns Foundation, Karen Elise Jensens Foundation, Fonden til Lægevidenskabens Fremme and Marie Dorthea og Holger From, and Haderslevs Foundation.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. Each author completed all of the following criteria: (1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
This preclinical animal study did not involve patients or require patient consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kyng, K.J., Kerrn-Jespersen, S., Bennedsgaard, K. et al. Short-term outcomes of remote ischemic postconditioning 1 h after perinatal hypoxia–ischemia in term piglets. Pediatr Res 89, 150–156 (2021). https://doi.org/10.1038/s41390-020-0878-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0878-6