Abstract
Background
Oxidative stress in children with type 1 DM (T1DM) may negatively affect the bone.
Methods
This study included 40 children with T1DM as the patient group and 40 healthy children of matched age and sex as the control group. Plasma alkaline phosphatase, procollagen type-1 amino-terminal propeptide (P1NP), and urinary deoxypyridinoline (DPD) were measured to assess bone turnover. Glutathione, superoxide dismutase (SOD), and malondialdehyde (MDA) were measured to assess oxidative stress.
Results
Patients with T1DM had a significantly lower P1NP level but a significantly higher urinary DPD level compared to the control group. Moreover, there were significantly lower glutathione and SOD levels with significantly higher MDA levels in patients with T1DM. We found a significant positive correlation between P1NP level and both glutathione and SOD levels but a significant negative correlation between P1NP and MDA in patients with T1DM. There was a significant negative correlation between DPD levels and both glutathione and SOD levels and a significant positive correlation between DPD and MDA. Moreover, glutathione was a significant predictor for both P1NP and DPD levels, while MDA was a significant predictor for P1NP levels.
Conclusions
There is an association between oxidative stress and bone turnover markers in children with T1DM.
Impact
-
Oxidative stress can negatively affect bone but the exact relationship between oxidative stress and bone turnover in T1DM has not been previously studied in pediatrics.
-
For the best of our knowledge, our study was the first to assess the relationship between oxidative stress and bone turnover in children with T1DM.
-
We revealed that increased oxidative stress in children and adolescents with T1DM may be involved in the impairment of bone turnover process, so treatment strategies toward better glycemic control and decreasing oxidative stress may be beneficial in preventing and treating diabetic bone disease in these children.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is a chronic metabolic disease that may affect bone and skeletal integrity. Low bone mineral density (BMD), bone fractures, and delayed fracture healing were reported in both children and adults with type 1 DM (T1DM).1,2,3,4
Bone turnover is a balanced coordinated relationship between bone formation process by osteoblasts and bone resorption process by osteoclasts.5 Alkaline phosphatase (ALP) and osteocalcin are widely used bone formation markers.4,6,7 Recently, procollagen type-1 N-terminal propeptide (P1NP) was recommended by the International Osteoporosis Foundation as a more specific bone formation marker originating from osteoblast and released during the formation of collagen type 1,8,9 while deoxypyridinoline (DPD) is a specific bone resorption biomarker.10
T1DM-related bone changes were explained by various mechanisms, including altered calcium and vitamin D metabolism due to hyperglycemia,11 glycation of type I collagen in bone, lower insulin-like growth factor-1 (IGF-1) level, deposition of lipids in bone marrow, increased osteoblastic transformation to adipocytes, and increased oxidative stress.12,13
Oxidative stress occurs when there is an imbalance between free radical production and antioxidant production. Oxidative stress increases in DM due to hyperglycemia via different ways, including increased production of reactive oxygen species (ROS) in mitochondria, glucose auto-oxidation, enhanced polyol pathway, and formation of advanced glycation end products (AGE).14 Oxidative stress can negatively affect bone by increasing bone resorption by osteoclasts and inhibiting osteoblastic differentiation. Moreover, ROS enhances lipid peroxidation with a resultant increase of malondialdehyde (MDA), the end product of lipid peroxidation.15
The exact relationship between oxidative stress and bone turnover markers in children with T1DM has not been previously studied. This research aimed to investigate the relationship between bone turnover markers and oxidative stress indices in children and adolescents with T1DM.
Methods
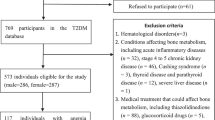
This cross-sectional study was carried out on 40 children and adolescents with T1DM enrolled from those attending the outpatient endocrinology clinic of the Pediatric Department of Tanta University Hospitals as the patient group and 40 healthy children and adolescents of matched age and sex as the control group. The study was approved by the ethical committee of the Faculty of Medicine, Tanta University. Informed consent was obtained from the parents of all participants.
Inclusion criteria: children and adolescents aged <18 years with T1DM. T1DM was diagnosed when fasting blood sugar was >126 mg/dl, random blood sugar was >200 mg/dl, glycated hemoglobin level was >6.5% on two separate tests, plus positive autoantibodies markers of beta cell autoimmunity such as islet cell antibodies, antibodies to glutamic acid decarboxylase (GAD-65), and insulin autoantibodies. Exclusion criteria: children with chronic diseases, such as renal disease, liver disease, thyroid or parathyroid dysfunction, and autoimmune diseases; children with gastrointestinal malabsorptive disorders, including ulcerative colitis and Crohn’s disease; children receiving drugs that can affect bone, such as steroids; and children having present or recent fractures were excluded from our study.
A full medical history was obtained from all participants in our study and they were subjected to thorough clinical examination. Fasting blood sample after overnight fasting for at least 8 h was obtained from all participants for measurement of the following biochemical parameters:
(1) Fasting blood glucose (FBG) levels and hemoglobin A1c (HbA1c) were measured using commercial chemical reagent kits (Spinreact, Spain and Biosystems reagents, Spain).
(2) Oxidative stress indices:
(i) Glutathione: total blood glutathione was measured using the method of Chavan et al.16 that depends on reductive cleavage of 5,5’-dithiobis-2-nitrobenzoic acid reagent.
(ii) MDA: plasma MDA was measured using thiobarbituric acid reactive substance method according to Draper and Hadly method.17
(iii) superoxide dismutase (SOD): Plasma SOD was measured by using commercial reagent kits (Biodiagnostic, Egypt).
(3) Bone turnover markers:
(i) Plasma P1NP was measured using commercial enzyme-linked immunosorbent assay kits (Novus Biologicals, USA).
(ii) Serum ALP was measured using commercial chemical reagent kits (Biodiagnostic, Egypt)
(iii) Urinary DPD was measured by enzyme immunoassay using commercial kits (Microvue, Quidel Corporation, USA) and expressed in relation to urinary creatinine.
Statistical analysis
Results were analyzed using the SPSS software version 20. Continuous data were presented as mean ± standard deviation (SD). Categorical data were presented as numbers and percentages. Chi-square test was used for comparing qualitative data of the two groups. A comparison of quantitative data of the two groups was carried out using Student’s t test. Association between bone turnover markers and oxidative stress parameters was evaluated using Pearson correlation coefficient and multiple regression analysis. A p value <0.05 was considered statistically significant.
Results
Our study was conducted on 40 children with T1DM and 40 healthy controls with a mean age of 11.6 ± 1.9 vs 11.1 ± 1.7 years, respectively. The mean duration of DM in children with T1DM was 3.7 ± 2.5 years.
Table 1 presents the anthropometric and clinical data of the children with T1DM and control group. There were no significant differences between children with T1DM and healthy control as regards age, sex, height, weight, or body mass index. However, FBG and HbA1c were significantly higher in children with T1DM compared to the control group.
Bone turnover and oxidative stress markers of both the groups are presented in Table 2. Children with TIDM had comparable ALP levels (75.8 ± 13.3 IU/L) with that of the control group (72.3 ± 11.8 IU/L). However, P1NP was significantly lower in children with T1DM compared to the control group (756.3 ± 41.7 vs 920.3 ± 82.3). DPD level was significantly higher in children with T1DM (18.6 ± 1.8 nmol/mmol Cr) compared to the control group (15.6 ± 2.6 nmol/mmol Cr). Moreover, children with T1DM had significantly lower glutathione and SOD levels compared to their respective values in the control group, while MDA level was significantly higher in children with T1DM compared to the control group (Table 2).
The duration of DM was not significantly correlated with P1NP or DPD. HbA1c had a significant negative correlation with P1NP but a significant positive correlation with DPD. Concerning oxidative stress indices, glutathione and SOD had a significant positive correlation with P1NP and a significant negative correlation with DPD as shown in Table 3. However, MDA had a significant negative correlation with P1NP and a significant positive correlation with DPD.
The role of oxidative stress indices as predictors of bone turnover markers was also assessed using multiple regression analysis considering diabetes duration and HbA1c as confounding factors as shown in Table 4. Glutathione was a significant predictor for P1NP and DPD levels (p = 0.001 and p = 0.02, respectively). On the other hand, MDA was a significant predictor for P1NP levels (p = 0.04).
Discussion
Biochemical bone turnover markers reflect the bone formation and resorption processes and are considered as a mirror image for bone health. Several studies showed that various biochemical bone turnover markers in diabetic patients differ from healthy non-diabetic controls.18,19,20 For the best of our knowledge, this study is the first to assess the relationship between bone turnover markers and oxidative stress in children with T1DM.
Our results showed that P1NP level was significantly lower in children with T1DM compared with healthy control, which is in agreement with other studies.8,21,22,23 This decrease in P1NP level reflects reduced bone formation in patients with T1DM that was previously explained by the decrease in IGF-1 level that leads to decreased stimulation of osteoblast with subsequent decrease of bone formation in patients with T1DM.24,25
On the other hand, there was no significant difference in the ALP level between children with T1DM and healthy children, which is going with the results of some studies26 and contradictory to other studies27,28 that reported an increase in ALP level in diabetic patients compared to the control. This variation in the level of total ALP may be due to intestinal or hepatic involvement rather than due to bone as other studies that measured bone-specific alkaline phosphatase (BAP) showed a non-significant change in BAP level in diabetic patients compared to the healthy control.18
Several studies assumed that the cause of impaired bone turnover in diabetes is due to a decrease in bone formation more than an increase in bone resorption19,29; however, our results found that the urinary level of DPD was significantly higher in children with T1DM compared to the control group reflecting a parallel increase of bone resorption. Our results are going with the results of other studies30,31 but contradictory to the results of Miazgowski and Czekalski,27 which may be due to the difference in age between our patients and theirs.
We also found a significant negative correlation between P1NP and HbA1c but a significant positive correlation between DPD and HbA1c, which is consistent with other studies.8,32 This finding suggests that better glycemic control may help to keep bone health in patients with diabetes. While there was no significant correlation between the duration of diabetes and both P1NP and DPD indicating that bone health depends on the glycemic control more than the duration of DM, it is also possible that the short duration of T1DM (3.7 ± 2.5 years) in our study population may explain the absence of significant correlation between the duration of DM and bone turnover markers.
Our children with T1DM had significantly low levels of the antioxidant indices (glutathione and SOD) and a significantly high level of MDA (the lipid peroxidation marker), which reveals an increase in oxidative stress in diabetic patients as reported in other studies.33,34
The significant positive correlation between P1NP and both glutathione and SOD and the significant negative correlation between P1NP and MDA reflects the negative effect of oxidative stress on the bone formation process. Oxidative stress may impair bone formation due to inhibition of osteoblast differentiation, impairing osteoblast function, and increasing osteoblast apoptosis.35,36,37,38 Besides, oxidative stress increases the level of AGE that leads to non-enzymatic glycation of collagen fibers and increases the production of inflammatory cytokines through binding to its receptor and enhancing the activation of nuclear factor kappa-B, with a subsequent decrease in osteoblast activity and proliferation.19,29,39,40,41
On the other hand, we found a significant negative correlation between DPD and both glutathione and SOD but a significant positive correlation between DPD and MDA, which reflect the role of oxidative stress in increasing bone resorption in patients with T1DM. Oxidative stress may increase the bone resorption process by increasing the number of osteoclasts,42 activating the differentiation of pro-osteoclast to osteoclast,43 and increasing osteoclast activity.44,45
Finally, our study revealed that increased oxidative stress in children and adolescents with T1DM may be involved in the impairment of bone turnover process, so treatment strategies toward better glycemic control and decreasing oxidative stress may be beneficial in preventing and treating diabetic bone disease.
Conclusion
There is an association between oxidative stress and bone turnover in children with T1DM. Oxidative stress in children with T1DM can negatively affect the bone by decreasing bone formation and increasing bone resorption.
References
Heilman, K., Zilmer, M., Zilmer, K. & Tillmann, V. Lower bone mineral density in children with type 1 diabetes is associated with poor glycemic control and higher serum ICAM-1 and urinary isoprostane level. J. Bone Min. Metab. 27, 598–604 (2009).
Weber, D. R. & Schwartz, G. Epidemiology of skeletal health in type 1 diabetes. Curr. Osteoporos. Rep. 14, 327–336 (2016).
Weber, D. R., Haynes, K., Leonard, M. B., Willi, S. M. & Denburg, M. R. Type 1 diabetes is associated with an increased risk of fracture across the life span: a population based cohort study using The Health Improvement Network (THIN). Diabetes Care 38, 1913–192 (2015).
Franceschi, R. et al. Bone geometry, quality, and bone markers in children with type 1 diabetes mellitus. Calcif. Tissue Int. 102, 657–665 (2018).
Garnero, P. Bone markers in osteoporosis. Curr. Osteoporos. Rep. 7, 84–90 (2009).
Amin, S., El Amrousy, D., Elrifaey, S., Gamal, R. & Hodeib, H. Serum osteocalcin levels in children with nonalcoholic fatty liver disease. J. Pediatr. Gastroenterol. Nutr. 66, 117–121 (2018).
El Amrousy, D. & El-Afifi, D. Osteocalcin and osteoprotegerin levels and their relationship with adipokines and proinflammatory cytokines in children with nonalcoholic fatty liver disease. Cytokine 135, 155215 (2020).
Madesen, J. O. B. et al. Decreased marker of bone turnover in children and adolescents with type 1 diabetes. Pediatr. Diabetes 20, 510–522 (2019).
Vaslkaran, S. et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos. Int. 22, 391–420 (2011).
Seibel, M. J. Biochemical markers of bone turnover part I: biochemistry and variability. Clin. Biochem. Rev. 26, 97 (2005).
Tanaka, H. et al. The impact of diabetes mellitus on vitamin D metabolism in predialysis patients. Bone 45, 949–955 (2009).
Al-Hariri, M. Sweet bones: the pathogenesis of bone alteration in diabetes. J. Diabetes Res. 2016, 6969040 (2016).
Hamada, Y. et al. Thioredoxin-1 overexpression in transgenic mice attenuates streptozotocin-induced diabetic osteopenia: a novel role of oxidative stress and therapeutic implications. Bone 44, 936–941 (2009).
Giacco, F. & Brownlee, M. Oxidative stress and diabetic complications. Circ. Res. 107, 1058–1070 (2010).
Sheweita, S. A., Al Samghan, A. S. & Khoshhal, O. K. Osteoporosis in children: possible risk factors and role of antioxidants. J. Musculoskelet. Surg. Res. 3, 319–325 (2019).
Chavan, S. et al. Reduced glutathione: importance of specimen collection. Indian J. Clin. Biochem. 20, 150–152 (2005).
Draper, H. & Hadly, M. Malonaldehyde determination as an index of lipid peroxidation. Methods Enzymol. 186, 421–431 (1990).
Starup-Linde, J. Diabetes, biochemical markers of bone turnover, diabetes control, and bone. Front. Endocrinol. 8, 4–21 (2013).
Hygum, K., Starup-Linde, J., Harsløf, T., Vestergaard, P. & Langdahl, B. L. Mechanisms in endocrinology: diabetes mellitus, a state of low bone turnover: a systematic review and meta-analysis. Eur. J. Endocrinol. 176, R137–R157 (2017).
Starup-Linde, J., Eriksen, S. A., Lykkeboe, S., Handberg, A. & Vestergaard, P. Biochemical markers of bone turnover in diabetes patients: a meta-analysis and a methodological study on the effects of glucose on bone markers. Osteoporos. Int. 25, 1697–1708 (2014).
Safarova, S. S. Alteration of bone metabolism in patients with diabetes mellitus. Int. J. Endocrinol. 2019, 5984681 (2019).
Elhabashy, S. A., Said, O. M., Agaiby, M. H., Abdelrazek, A. A. & Abdelhamid, S. Effect of physical exercise on bone density and remodeling in Egyptian type 1 diabetic osteopenic adolescent. Diabetol. Metab. Syndr. 3, 25 (2011).
Koshhal, K. I., Sheweita, S. A., Al-Maghamsi, M. S. & Habeb, A. M. Does type 1 diabetesmellitus affect bone quality in pre-pubertal children? J. Taibah Univ. Med. Sci. 10, 300–305 (2015).
Keenan, H. A. & Maddaloni, E. Bone microarchitecture in type 1 diabetes: it’s complicated. Curr. Osteoporos. Rep. 14, 351–358 (2016).
Neve, A., Corrado, A. & Cantatore, F. P. Osteoblast physiology in normal and pathological conditions. Cell Tissue Res. 343, 289–302 (2011).
Joshi, A., Varthakavi, P., Chadha, M. & Bhagwat, N. A study of bone mineral density and its determinants in type 1 diabetes mellitus. J. Osteoporos. 2013, 397814 (2013).
Miazgowski, T. & Czekalski, S. A 2-year follow-up study on bone mineral density and markers of bone turnover in patients with long-standing insulin-dependent diabetes mellitus. Osteoporos. Int. 8, 399–403 (1998).
Bouillon, R. et al. Influence of age, sex, and insulin on osteoblast function: osteoblast dysfunction in diabetes mellitus. J. Clin. Endocrinol. Metab. 80, 1194–1202 (1995).
Kanazawa, I. & Sugimoto, T. Diabetes mellitus-induced bone fragility. Intern. Med. 57, 2773–2785 (2018).
Bjørgaas, M., Haug, E. & Johnsen, H. J. The urinary excretion of deoxypyridinium cross-links is higher in diabetic than in non-diabetic adolescents. Calcif. Tissue Int. 65, 121–124 (1999).
Sav, N. M., Kendirci, M., Akin, L. & Kurtoglu, S. Urinary levels of pyridinoline and deoxypyridinoline and bone mineral density in children with type 1 diabetes mellitus. Endocr. Res. 42, 281–286 (2017).
Valerio, G. et al. Increased urinary excretion of collagen crosslinks in type 1 diabetic children in the first 5 years of disease. Horm. Res. 51, 173–177 (1999).
Vallea, L. G. et al. Altered redox status in patients with Diabetes Mellitus type I. Pharmacol. Res. 51, 375–380 (2005).
Firoozrai, M., Nourbakhsh, M. & Razzaghy-Azar, M. Erythrocyte susceptibility to oxidative stress and antioxidant status in patients with type 1 diabetes. Diabetes Res. Clin. Pract. 77, 427–432 (2007).
Alikhani, M. et al. Advanced glycation end products stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone 40, 345–353 (2007).
Hamada, Y., Fujii, H. & Fukagawa, M. Role of oxidative stress in diabetic bone disorder. Bone 45, S35–S38 (2009).
Manolagas, S. C. & Almeida, M. Gone with the Wnts: beta-catenin, T-cell factor, fork-head box O, and oxidative stress in age-dependent diseases of bone, lipid, and glucose metabolism. Mol. Endocrinol. 21, 2605–2614 (2007).
Mody, N., Parhami, F., Sarafian, T. A. & Demer, L. L. Oxidative stress modulates osteoblastic differentiation of vascular and bone cells. Free Radic. Biol. Med. 31, 509–519 (2011).
Murray, C. E. & Coleman, C. M. Impact of diabetes mellitus on bone health. Int. J. Mol. Sci. 20, 4873–4896 (2019).
Rathinavelu, S., Guidry-Elizondo, C. & Banu, J. Molecular modulation of osteoblasts and osteoclasts in type 2 diabetes. J. Diabetes Res. 2018, 1–11 (2018).
Xie, J., Mendez, J. D., Mendez-Valenzuela, V. & Aguilar-Hernandez, M. M. Cellular signalling of the receptor for advanced glycation end products (RAGE). Cell. Signal. 25, 2185–2197 (2013).
Baek, K. H. et al. Association of oxidative stress with postmenopausal osteoporosis and the effects of hydrogen peroxide on osteoclast formation in human bone marrow cell cultures. Calcif. Tissue Int. 87, 226–235 (2010).
Savasky, B. J., Mascotti, D. P., Patel, N. & Rodriguez-Collazo, E. Nutritional and pharmacological effects on oxidative stress in soft tissue and bone remodeling. J. Nutr. Metab. 2018, 1–9 (2018).
Wauquier, F., Leotoing, L., Coxam, V., Guicheux, J. & Wittrant, Y. Oxidative stress in bone remodelling and disease. Trends Mol. Med. 15, 468–477 (2009).
Kalaitzoglou, E., Popescu, I., Bunn, R. C., Fowlkes, J. L. & Thrailkill, K. M. Effects of type 1 diabetes on osteoblasts, osteocytes and osteoclasts. Curr. Osteoporos. Rep. 14, 310–319 (2016).
Author information
Authors and Affiliations
Contributions
D.E.: acquisition of data, recruitment of patients, drafting and final approval of the manuscript. D.E.-A.: idea of the research, performing the statistical analysis, drafting and final approval of the manuscript. A.S.: acquisition of data, help in the statistical analysis, drafting and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
IRB approval
The study was approved by the local ethics committee of Faculty of Medicine, Tanta University, Egypt.
Patient consent
The patients were enrolled after obtaining an informed written consent from their parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Amrousy, D., El-Afify, D. & Shabana, A. Relationship between bone turnover markers and oxidative stress in children with type 1 diabetes mellitus. Pediatr Res 89, 878–881 (2021). https://doi.org/10.1038/s41390-020-01197-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01197-5
This article is cited by
-
Assessment of biochemical bone markers of osteoporosis in children with thalassemia major
Italian Journal of Pediatrics (2022)