Abstract
Background
Neonates may be exposed to lead (Pb) through blood transfusions from donors. Pb exposure has neurological, cardiovascular, renal, and other adverse effects. The study aimed to (i) determine the blood lead levels (BLLs) in different blood product units (whole blood, packed red blood cells (pRBCs), platelets, and plasma transfused to neonates) and (ii) estimate the proportion of units with high BLLs.
Methods
Residual blood from blood bank bags that were used for neonatal transfusion were collected: 25 samples from each type of blood product except for whole blood (10 samples). The Pb analysis was performed using the atomic absorption method. The study was conducted at the Suez Canal University Hospital, Egypt.
Results
The mean of BLL in pRBCs, platelets, plasma, and whole blood were 136, 199, 108, and 130 µg/L, respectively; 60% contained Pb above 50 µg/L. The highest BLLs were in platelet units.
Conclusions
The present study showed for the first time that platelets and plasma in addition to whole blood and pRBCs used for neonatal transfusions are sources of Pb. Re-evaluation of the guidelines is mandatory for the safety of the neonates. Long-term neurodevelopment assessment of neonates exposed to high Pb is warranted.
Similar content being viewed by others
Introduction
Lead (Pb) exposure is a child health concern worldwide; this problem is intensified in developing countries.1 Preterm neonates comprise the most heavily transfused group of patients.2 The critical stages of growth and cellular differentiation that occur in fetuses and neonates represent periods of greatest vulnerability to the adverse effects of environmental toxicants.3 Pb exposure in neonates has particularly been associated with long-term neurotoxic effects during the critical period of rapid brain development.4 Based on Canadian health risk assessment study, the maximum level of Pb in a blood donation that could safely be given to the vulnerable patients should not exceed 30 µg/L.5 Nevertheless, another study recommended that blood units used for young children should be screened for Pb to warrant concentrations <18.6 µg/L, and achieve the lowest possible Pb exposure.6
Pb is a potent irreversible neurotoxicant and exposure leads to developmental delay with effects on cognition, behavior, and intelligence quotient (IQ) with an unexpectedly great impact even at low levels.7 This has prompted the Centers for Disease Control and Prevention (CDC) not only to further decrease the reference cut-off value for toxic blood lead levels (BLLs) (from 100 to 50 μg/L) in children, but also to question the term “blood lead level of concern” under the assumption that there is no safe BLL.8 Pb neurotoxicity occurs at a cellular level on several parts of neurite growth in the developing brain. It causes direct damage to neuron synaptic development and myelin formation. The effect of Pb may be through interference in the cell to cell connectivity.9,10 Pb moves from the blood into soft tissues and bone with slow release over time.4 The amount of Pb absorbed is inversely related to chronological age.8 Both gastrointestinal absorption of Pb and its accumulation in bone are higher in infants (potentially causing growth impairment and calcium deficiency) than in adults.11 Moreover, children retain more Pb in soft tissues as compared to adults,3 and selective brain accumulation in the hippocampus can occur. Little to no information is available for the burden and impact of Pb exposure in preterm infants.12
Recently, two studies measured the BLLs in transfused whole blood and packed red blood cells (pRBCs) in USA and Canada.6,12 They found significant BLLs in transfusion products. As a consequence, Zubairi et al, recommended and invited the researcher to investigate BLLs in the other transfusion products (such as platelets and plasma) to obtain an accurate measurement of exposure.12
Up to authors' knowledge, no previous study was performed in Egypt to assess the prevalence of Pb exposure among blood product units that are prepared for neonatal transfusion. Moreover, no previous study measured Pb in blood products other than whole blood and pRBCs. Therefore, the aim of the study was to (i) determine the BLLs in various blood products (whole blood, platelets, pRBCs, and plasma) which are prepared for blood transfusion for neonates (ii) estimate the proportion of units with high BLLs, (iii) explore predictive factors of high BLLs, and, (iv) calculate the expected Pb load per transfusion.
Materials and methods
The samples were obtained from residual blood units of different blood products in the Suez Canal University Hospital (SCUH) blood bank. The SCUH is a referral center and receives donors from different eastern regions of Egypt, mostly Ismailia and Sinai governorates. The blood units were prepared for transfusion to the neonates in the neonatal intensive care unit (NICU). The total number of collected samples was 85 which were divided into 25 samples from each type of blood product (pRBCs, platelets, and plasma), except for whole blood (10 samples). The samples were transferred into trace-mineral-free vacutainers and subsequently stored at −20 °C before analysis. Routinely collected data from blood donors in SCUH blood bank were obtained by chart review, it included, age, sex, residence, blood group type, and type of blood product obtained.
The digestions of samples were done as suggested by the National Institute for Occupational Safety and Health using HNO3/HClO4 /H2SO4, and heat. The analysis of extracted samples was performed using atomic absorption (AAS) (Thermo S4AASystem "GE711838").13,14 Analysis of each sample was conducted using a replication procedure (three replicates), and the mean of the repeated measurements was taken as the result value. The replicates had good reproducibility (intra- and inter-day coefficient of variations (CVs) and bias less than 10%). The limit of detection was 20 μg/L. The AAS is routinely calibrated before any batch of samples. The mean recovery rate is 90%. To ensure the quality of results, quality control (QC) samples were blindly inserted every 20 samples. It is recommended that the BLLs in transfused units would be less than 30 µg/L;5 with probable risk if the donor’s BLL was more than 60 µg/L.11
Data entry was performed using windows operating system, and data analysis was performed using the statistical package for social sciences (SPSS version 22). Descriptive statistics: median and mean are calculated for the detectable values of Pb concentrations to determine the distributions of blood product Pb levels (BLLs). Kruskal–Wallis (KW) test was used to compare BLLs which were not normally distributed. Multivariable linear regression and logistic regression analysis were performed to identify the independent BLL predictors and explore the associations with these factors at BLLs of different high levels (≥150, ≥100, and ≥50 μg/L).
The quantity of transfused Pb was estimated using transfused volumes. The study was approved by the Research Ethics Committee (REC) at the Faculty of Medicine, Suez Canal University.
Results
The mean of BLLs in different blood products ranged from 108 to 199 µg/L. The highest mean and median BLL recorded among platelet units were 199 and 140 µg/L, respectively. Estimated proportion of BLLs above 150 µg/L in different blood products varied from 20 to 48 % (Table 1).
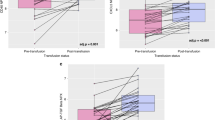
The frequency distributions of BLLs in the four studied blood products are presented in Fig. 1. BLLs above 150 µg/L were found in 27 (31.8 %) of the participants. The number of participants with BLLs above 100 µg/L and 50 µg/L were 37 (43.5 %) and 51 (60 %), respectively.
Distribution of blood lead levels (BLL) among various blood product units; data are shown as median values (horizontal lines), interquartile ranges (the box lengths), extreme values (whiskers), outliers (o), and statistical significance (*). The difference between four blood products is statistically significant (p = 0.032)
The average total Pb load per transfusion of each blood product is presented in Table 2. The highest Pb load per transfusion was associated with whole-blood exchange transfusion and platelets transfusions.
The distributions of BLLs according to age, sex, residence, blood groups (ABO & Rhesus (Rh) factor), and blood products are shown in Table 1. The mean age of donor participants was 30 years (SD, ±8.9 years). In summary, 82.4% of the participants were males, 66% reside in an urban area, 38.8% were blood group type B, and 80% were Rh factor positive.
The results of the univariate analysis are shown in Table 1. Statistically significant differences in BLLs were found between subgroups for sex, residence, and the type of transfused blood products (P < 0.05). Estimated proportion of BLLs above 150 µg/L ranged from 25 to 48.3% depending on an urban or rural residence of blood donors with higher BLLs among those who live in the rural area.
The logistic regression analysis for variables that are independently associated with BLLs above 50, 100, 150 µg/L is presented in Table 3. The adjusted odds ratios (ORs) at BLL≥ 100 and 150 µg/L ranked the highest for age but did not reach statistical significance, followed by blood group type A which was statistically significant at BLL ≥ 100 and 150 µg/L. Results of the multiple regression analysis are presented in Table 4. All variables except for age justified 15.89% of the statistically significant variance observed.
Discussion
The present study is the first to our knowledge that examined the BLLs in blood products other than whole blood and pRBCs. The results revealed that both platelets and plasma were other significant sources of Pb in blood prepared for neonatal transfusion. We also demonstrated that platelets exhibited higher Pb levels compared to other blood products. These findings are in contrast to the previously reported conclusions that most of the lead load was from the pRBCs.12,15
In this study, the means of BLLs in different blood products ranged from 108 to 199 µg/L with 43.5% and 31.8% of the samples’ BLL more than 100 and 150 µg/L, respectively. A previous study of Egyptian children revealed mean BLLs of 48 µg/L, which ranged from 11 to 143 µg/L.16 The mean BLLs in the general Canadian population was 17 µg/L,6 which was comparable to a reported rate of 16.6 µg/L in the United States.17 Similarly, Zubairi et al, reported the mean Pb load per transfusion was 13 µg with a range from 0 to 86 µg.12 However, in a metropolitan population in the United States; 2 and 0.5% of blood bags contained BLL of more than 50 and 100 µg/L, respectively.18 Another study including Pb levels in pRBC units transfused to extremely low birth weight neonates, reported concentrations that exceeded the estimated upper limit of acceptable concentration (ETC) in 26% pRBC units; which comprised 84% of units with at least one heavy metal above the ETC (aluminum, arsenic, beryllium, cadmium, manganese, mercury, nickel, lead, and polonium).19 Lead exposure had been an environmental problem in the Southern regions of China secondary to the high e-waste disposal and occupational exposure.2,20,21 A study in China revealed that the average BLLs in children was more than 60 μg/L, with 7–10 % of children having BLLs above 100 μg/L.1 Higher BLL mostly related to high environmental exposure were reported in developing countries. A regional study in Morocco reported a mean BLLs of 87 µg/L.22 A Brazilian survey among blood donors demonstrated 5% of tested BLLs contained 100 µg/L.23 However, BLL as low as 4 µg/L were reported from a small sample study of blood donors in Poland.24 In comparison to the reported BLL in the literature, the present study demonstrated a higher mean Pb load per transfusion that ranged from 64.8 to 156 µg within different blood products. This observation strongly suggests an alarmingly high Pb exposure in this study population. It is noteworthy to mention that 82.4% of blood donors were males in the present study which is in line with previously reported gender rates for blood donation in Egypt.25 Males are more likely than females to donate blood as most females in the age interval 20–40 years—the most common donation age interval in the present study—are childbearing or lactating. Besides, females are deferred if they were found to be anemic in the blood donation screening process.25
The high BLL in plasma in the present study could be due to a high level of exposure which corresponds to a relatively more substantial change in plasma Pb concentration, with a small change in whole-blood Pb concentration. This is due to the non-linear relation between whole-blood lead and plasma Pb at a high level of exposure.26 Moreover, it is important to mention that the increase in the Pb plasma level could be due to potential Pb contamination from hemolyzed RBCs.27 It is essential to be cognizant when deciding on plasma transfusion, as plasma Pb is the main biologically active compartment with greater bio-availability (diffusible form). Thus, it is available to cross cell membranes and influence other tissues’ concentrations more directly, which in turn burdens the newborn body. Pb is bound in a slow-diffusible form with RBCs.28,29
Previous studies reported that BLL in plasma comprises about 0.06–0.5%,30 0.1 to 0.4%,29 and 0.2–0.8 % of whole BLLs.27 The Pb concentration in RBCs is 2–3.5 times that in the blood.15 Moreover, the estimated RBCs-to-plasma lead ratio was 26.4:0.66 (about 40:1).28 Those ratios were not estimated in the present study as not all four blood products’ units were prepared from the same donor, unlike other studies that used corresponding donors with blood products.15,26,27,28,29,30 It is also notable to state that plasma-to-blood Pb ratio can vary quite widely within and among individuals.31 This may be owing to differences in toxicokinetics with respect to δ-aminolaevulinic acid dehydratase (ALAD) gene polymorphisms.32 In addition, BLLs in plasma and RBCs of different samples could vary according to the storage capacity of their RBCs, and/or to the binding capacity of some ligands in plasma.28 The wide range of variance was also noticed regarding the ratio between Pb concentrations in RBCs and blood.15 By the estimation of Pb loading per transfusion, the whole blood and platelets could be of higher risk compared to other blood products due to the high volume required per transfusion in case of whole blood transfusion.
A unique finding of the present study is the significant higher BLLs reported from platelet units in comparison to other transfused blood products. This sheds light on transfused platelet units which may carry an equivalent or higher risk of Pb exposure compared to pRBCs and other blood products. The elevation in cytosolic calcium (Ca2+) concentrations is essential for platelet activation in thrombosis and hemostasis. It occurs through Ca2+ release from intracellular stores and Ca2+ entry through the plasma membrane. Lead mimics Ca2+ and enters the platelets, thus impairing calcium regulation.33 The entry of Pb in the platelets could follow a similar mechanism, contributing to the high Pb levels in the platelet units. However, the exact means whereby Pb is high in platelets is unclear. Elevated BLL also can cause activation of protein kinase and reduction of nitric oxide. This lead to endothelial injury and impaired coagulation,34 which poses a potential risk of transfusing Pb-laden platelets to thrombocytopenic neonates. Several studies have demonstrated that Pb caused alteration of platelet counts and indices in Pb-exposed workers35,36 and pre-school children living in Guiyu; one of the highest electronic waste and recycling areas in the world.20,21
The results of this study are presented with several caveats. First, the small sample size of the different blood product units. Second, the four studied blood products were not consistently obtained from the same donor; thus, we were unable to calculate plasma and platelets to whole-blood ratios. Third, there is a possibility of contamination of plasma and platelets units with red blood cells. Nevertheless, the RBCs are strictly checked in the centrifuged plasma and platelets units. Besides visual assessment,37 the blood bank at the SCUH38 routinely measure RBCs on a cell counter to ensure RBC counts <2 ml, adopting the guidelines of American Association of Blood Banks (AABB).39 Overall, it is unlikely that minute volume contamination with RBC would cause the high reported Pb levels in the plasma and platelet units. Another factor to consider is, the limit of detection of our analytical method was 20 ug/L. This limit may underestimate the burden of lower BLL that could pose a potential threat to the transfused neonates.
In conclusion platelets and plasma in addition to pRBCs and whole blood used for neonatal transfusions are significant sources of Pb. Sixty percent of blood units had BLLs higher than the CDC defined toxic cut-off levels. The highest BLLs were in the platelet units. This could be reflective of the magnitude of this potential health problem in developing countries. Screening blood donors and the analysis of Pb in blood are recommended. Future long-term neurodevelopment assessment of neonates exposed to lead is warranted to determine the actual impact and health burden of this toxic heavy metal.
References
Liu, J. et al. Blood lead levels and associated sociodemographic factors among preschool children in the South Eastern region of China. Paediatr. Perinat. Epidemiol. 26, 61–69 (2012).
Portugal, C. A. A. et al. Transfusion practices in a neonatal intensive care unit in a city in Brazil. Rev. Bras. De. Hematol. e Hemoter. 36, 245–249 (2014).
Falck, A. J. et al. Developmental exposure to environmental toxicants. Pediatr. Clin. North Am. 62, 1173–1197 (2015).
Newman, N. & Carey, P. M. Donor blood lead levels and transfusion safety in a vulnerable population. Transfusion 55, 2544–2546 (2015).
Rhainds, M. & Delage, G. Health risk assessment of lead exposure from blood transfusion. Epidemiology 17, S492 (2006).
Delage, G., Gingras, S. & Rhainds, M. A population-based study on blood lead levels in blood donors. Transfusion 55, 2633–2640 (2015).
Sanders, T., Liu, Y., Buchner, V. & Tchounwou, P. B. Neurotoxic effects and biomarkers of lead exposure: a review. Rev. Environ. Health 24, 15–46 (2009).
Centers for Disease Control and Prevention. Low Level Lead Exposure Harms in Children: A renewed call for primary prevention. Report of the Adivisory Committee on Childhood Lead Poisonining Prevention of the Centers for Disease Control and Prevention. Atlanta, GA: Centers for Disease Control and Prevention, 2012:1–54. https://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf. Accessed on 30 November 2017.
Lidsky, T. I. & Schneider, J. S. Lead neurotoxicity in children: basic mechanisms and clinical correlates. Brain 126, 5–19 (2003).
Schneider, J., Huang, F. & Vemuri, M. Effects of low-level lead exposure on cell survival and neurite length in primary mesencephalic cultures. Neurotoxicology Teratol. 25, 555–559 (2003).
Bearer, C. F., O’riordan, M. A. & Powers, R. Lead exposure from blood transfusion to premature infants. J. Pediatr. 137, 549–554 (2000).
Zubairi, H., Visintainer, P., Fleming, J., Richardson, M. & Singh, R. Lead exposure in preterm infants receiving red blood cell transfusions. Pediatr. Res. 77, 814-818 (2015).
World Health Organization. Brief guide to analytical methods for measuring lead in blood, 2011. http://apps.who.int/iris/bitstream/10665/77912/1/9789241502139_eng.pdf. Accessed on 30 November 2017.
NIOSH. NIOSH manual of analytical methods (NMAM). 4th edn. Cincinnati, OH: National Institute for Occupational Safety and Health, 1994. https://www.cdc.gov/niosh/nmam.pdf. Accessed on 30 November 2017.
Angle, C. R. & McIntire, M. S. Red cell lead, whole blood lead, and red cell enzymes. Environ. Health Perspect. 7, 133‒137 (1974).
Sharaf, N. E., Abdel-Shakour, A., Amer, N. M., Abou-Donia, M. A. & Khatab, N. Evaluation of children's blood lead level in Cairo, Egypt. American-Eurasian. J. Agric. & Environ. Sci. 3, 414–419 (2008).
Muntner, P., Menke, A., DeSalvo, K. B., Rabito, F. A. & Batuman, V. Continued decline in blood lead levels among adults in the United States: the National Health and Nutrition Examination Surveys. Arch. Intern. Med. 165, 2155–2161 (2005).
Bulleova, S., Rothenberg, S. J. & Manalo, M. A. Lead levels in blood bank blood. Arch. Environ. Health. 56, 312–313 (2001).
Sundarajan S., et al. Toxic metal contamination of banked blood designated for neonatal transfusion. J. Clin. Toxic. 5, 267 (2015). DOI: https://doi.org/10.4172/2161-0495.1000267.
Zeng, X. et al. Decreased lung function with mediation of blood parameters linked to e-waste lead and cadmium exposure in preschool children. Environ. Pollut. 230, 838–848 (2017).
Zhang, Y. et al. Elevated lead levels and adverse effects on natural killer cells in children from an electronic waste recycling area. Environ. Pollut. 213, 143–150 (2016).
Khassouani, C., Allain, P. & Soulaymani, R. Lead impregnation in inhabitants of the Rabat region (Morocco). Presse Med 26, 1714–1716 (1997).
Freire, C. et al. Reference values of lead in blood and related factors among blood donors in the Western Amazon, Brazil. J. Toxicol. Environ. Health A 77, 426–440 (2014).
Janicka, M. et al. Cadmium, lead and mercury concentrations and their influence on morphological parameters in blood donors from different age groups from southern Poland. J. Trace Elem. Med Biol. 29, 342–346 (2015).
Messih, I. Y. A., Ismail, M. A., Saad, A. A. & Azer, M. R. The degree of safety of family replacement donors versus voluntary non-remunerated donors in an Egyptian population: a comparative study. Blood Transfus. 12, 159‒165 (2014).
Sommar, J. N. et al. Investigation of lead concentrations in whole blood, plasma and urine as biomarkers for biological monitoring of lead exposure. J. Expo. Sci. Environ. Epidemiol. 24, 51‒57 (2014).
Smith, D. R., Ilustre, R. P. & Osterloh, J. D. Methodological considerations for the accurate determination of lead in human plasma and serum. Am. J. Ind. Med. 33, 430–438 (1998).
Cavalleri, A., Minoia, C., Pozzoli, L., Polatti, F. & Bolis, P. F. Lead in red blood cells and in plasma of pregnant women and their offspring. Environ. Res. 17, 403–408 (1978).
Ettinger, A. S. et al. Maternal blood, plasma, and breast milk lead: lactational transfer and contribution to infant exposure. Environ. Health Perspect. 122, 87‒92 (2014).
Juárez-Pérez, C. A. et al. Predictors of plasma lead among lithographic print shop workers in Mexico City. Am. J. Ind. Med. 46, 245–252 (2004).
Smith, D., Hernandez-Avila, M., Téllez-Rojo, M. M., Mercado, A. & Hu, H. The relationship between lead in plasma and whole blood in women. Environ. Health Perspect. 110, 263‒268 (2002).
Montenegro, M. F., Barbosa, F.Jr. & Tanus‐Santos, J. E. Assessment of how pregnancy modifies plasma lead and plasma/whole blood lead ratio in ALAD 1‐1 genotype women.Basic Clin. Pharmacol. Toxicol. 102, 347–351 (2008).
Varga-Szabo, D., Braun, A. & Nieswandt, B. Calcium signaling in platelets. J. Thromb. Haemost. 7, 1057–1066 (2009).
Chwalba, A. et al. The effect of occupational chronic lead exposure on the complete blood count and the levels of selected hematopoietic cytokines. Toxicol. Appl. Pharmacol. 15, 174–179 (2018).
Barman, T., Kalahasthi, R. & Rajmohan, H. Effects of lead exposure on the status of platelet indices in workers involved in a lead-acid battery manufacturing plant. J. Expo. Sci. Environ. Epidemiol. 24, 629‒633 (2014).
Dobrakowski, M. et al. Cytokines related to three major types of cell-mediated immunity in short-and long-term exposures to lead compounds. J. Immunotoxicol. 13, 770–774 (2016).
Canadian Blood Services. Transfusion. Visual Assessment Guide. https://professionaleducation.blood.ca/en/transfusion/best-practices/visual-assessment-guide. Accessed 30 July 2018.
Hosny N., Goubran F., BadrEldin Hasan B., Kamel N. Assessment of vascular endothelial growth factor in fresh versus frozen platelet rich plasma. Journal of blood transfusion. 2015,1‒5 (2015).
AABB Standards for Blood Banks and Transfusion Services, 30th edition. http://hospitals.unitedbloodservices.org/Portals/0/HUBS/Documents/education/current-topics/Red-Cell-Contamination-in-Platelets-and-Apheresis-Granulocytes.pdf. Accessed on 30 July 2018.
Authors contributions
J.G.: revised the article critically for important intellectual content and final approval of the version to be published. S.A.: study design, acquisition of data, data analysis & interpretation, drafting the article and final approval of the version to be published. AO: conception, design, acquisition of data, drafting the article, and final approval of the version to be published. M.O.A.: collection and analysis of samples, final approval of the version to be published. D.M. data interpretation, editing and final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aly, S.M., Omran, A., Abdalla, M.O. et al. Lead: a hidden “untested” risk in neonatal blood transfusion. Pediatr Res 85, 50–54 (2019). https://doi.org/10.1038/s41390-018-0175-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0175-9
This article is cited by
-
Fetal exposure to mercury and lead from intrauterine blood transfusions
Pediatric Research (2019)