Abstract
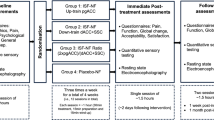
Chronic low back pain (cLBP) is the most prevalent chronic pain condition. There are no treatments that haven been found to directly assuage evoked cLBP. To this extent, mindfulness-meditation is a promising pain therapy. Yet, it is unclear if meditation can be utilized to directly attenuate evoked chronic pain through endogenous opioids. A double-blind, randomized, and placebo-controlled clinical trial with a drug crossover design examined if mindfulness-meditation, as compared to sham mindfulness-meditation, attenuated straight leg-raise test evoked chronic pain during intravenous (0.15 mg/kg bolus + 0.15 mg/kg/hour maintenance) naloxone (opioid antagonist) and placebo-saline infusion. Fifty-nine individuals with cLBP (mean age = 46 years; 30 females) completed all study procedures. After the pre-intervention pain testing session, patients were randomized to a four-session (20-min/session) mindfulness (n = 30) or sham mindfulness-meditation (n = 29) intervention. After the interventions, mindfulness and sham mindfulness-meditation were associated with significant reductions in back pain during saline and naloxone infusion when compared to rest (non-meditation) in response to the cLBP-evoking straight leg-raise test. These results indicate that meditation directly reduces evoked chronic pain through non-opioidergic processes. Importantly, after the interventions, the mindfulness group reported significantly lower straight leg-raise induced pain than the sham mindfulness-meditation group during rest (non-meditation) and meditation. Mindfulness and sham mindfulness-meditation training was also associated with significantly lower Brief Pain Inventory severity and interference scores. The pain-relieving effects of mindfulness meditation were more pronounced than a robust sham-mindfulness meditation intervention, suggesting that non-reactive appraisal processes may be uniquely associated with improvements in chronic low-back pain.
Trial Registration: ClinicalTrials.gov identifier: NCT04034004
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Andersson GB. Epidemiological features of chronic low-back pain. lancet. 1999;354:581–5.
Graven-Nielsen T, Arendt-Nielsen L. Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat Rev Rheumatol. 2010;6:599–606.
Corbett DB, Simon CB, Manini TM, George SZ, Riley JL III, Fillingim RB. Movement-evoked pain: transforming the way we understand and measure pain. Pain. 2019;160:757.
Esteve R, Ramírez-Maestre C, López-Martínez AE. Adjustment to chronic pain: the role of pain acceptance, coping strategies, and pain-related cognitions. Ann Behav Med. 2007;33:179–88.
Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA. 2016;315:1240–9.
Wells RE, O’Connell N, Pierce CR, Estave P, Penzien DB, Loder E, et al. Effectiveness of mindfulness meditation vs headache education for adults with migraine: a randomized clinical trial. JAMA Intern Med. 2021;181:317–28.
Colloca L, Petrovic P, Wager TD, Ingvar M, Benedetti F. How the number of learning trials affects placebo and nocebo responses. Pain®. 2010;151:430–39.
De Pascalis V, Chiaradia C, Carotenuto E. The contribution of suggestibility and expectation to placebo analgesia phenomenon in an experimental setting. Pain. 2002;96:393–402.
Kaptchuk TJ. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med. 2002;136:817–25.
Wager TD, Atlas LY, Leotti LA, Rilling JK. Predicting individual differences in placebo analgesia: contributions of brain activity during anticipation and pain experience. J Neurosci. 2011;31:439–52.
Zeidan F, Johnson SK, Gordon NS, Goolkasian P. Effects of brief and sham mindfulness meditation on mood and cardiovascular variables. J Alter Complement Med. 2010;16:867–73.
Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, et al. Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. J Neurosci. 2015;35:15307–25.
Wells RE, Collier J, Posey G, Morgan A, Auman T, Strittmatter B, et al. Attention to breath sensations does not engage endogenous opioids to reduce pain. Pain. 2020;161:1884–93.
Adler-Neal AL, Waugh CE, Garland EL, Shaltout HA, Diz DI, Zeidan F. The role of heart rate variability in mindfulness-based pain relief. J pain. 2020;21:306–23.
Zubieta J-K, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, et al. Regional mu opioid receptor regulation of sensory and affective dimensions of pain. Science. 2001;293:311–15.
Mayer DJ, Price DD, Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Res. 1977;121:368–72.
Watkins LR, Mayer DJ. Organization of endogenous opiate and nonopiate pain control systems. Science. 1982;216:1185–92.
Eippert F, Bingel U, Schoell ED, Yacubian J, Klinger R, Lorenz J, et al. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron. 2009;63:533–43.
Levine JD, Gordon NC, Fields HL. The mechanism of placebo analgesia. Lancet. 1978;2:654–7.
Zubieta J-K, Bueller JA, Jackson LR, Scott DJ, Xu Y, Koeppe RA, et al. Placebo effects mediated by endogenous opioid activity on μ-opioid receptors. J Neurosci. 2005;25:7754–62.
Sprenger C, Eippert F, Finsterbusch J, Bingel U, Rose M, Büchel C. Attention modulates spinal cord responses to pain. Curr Biol. 2012;22:1019–22.
Taylor JJ, Borckardt JJ, Canterberry M, Li X, Hanlon CA, Brown TR, et al. Naloxone-reversible modulation of pain circuitry by left prefrontal rTMS. Neuropsychopharmacology. 2013;38:1189–97.
Oliva V, Hartley-Davies R, Moran R, Pickering AE, Brooks JC. Simultaneous brain, brainstem, and spinal cord pharmacological-fMRI reveals involvement of an endogenous opioid network in attentional analgesia. Elife. 2022;11:e71877.
Zeidan F, Adler-Neal AL, Wells RE, Stagnaro E, May LM, Eisenach JC, et al. Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. J Neurosci. 2016;36:3391–7.
Martikainen IK, Pecina M, Love TM, Nuechterlein EB, Cummiford CM, Green CR, et al. Alterations in endogenous opioid functional measures in chronic back pain. J Neurosci. 2013;33:14729–37.
Harris RE, Clauw DJ, Scott DJ, McLean SA, Gracely RH, Zubieta J-K. Decreased central μ-opioid receptor availability in fibromyalgia. J Neurosci. 2007;27:10000–06.
Bruehl S, Chung OY, Burns JW, Diedrich L. Trait anger expressiveness and pain-induced beta-endorphin release: support for the opioid dysfunction hypothesis. Pain. 2007;130:208–15.
Thompson SJ, Pitcher MH, Stone LS, Tarum F, Niu G, Chen X, et al. Chronic neuropathic pain reduces opioid receptor availability with associated anhedonia in rat. Pain. 2018;159:1856.
Schrepf A, Harper DE, Harte SE, Wang H, Ichesco E, Hampson JP, et al. Endogenous opioidergic dysregulation of pain in fibromyalgia: a PET and fMRI study. Pain. 2016;157:2217.
Willoch F, Schindler F, Wester HJ, Empl M, Straube A, Schwaiger M, et al. Central poststroke pain and reduced opioid receptor binding within pain processing circuitries: a [11C] diprenorphine PET study. Pain. 2004;108:213–20.
Wasan AD, Loggia ML, Chen LQ, Napadow V, Kong J, Gollub RL. Neural correlates of chronic low back pain measured by arterial spin labeling. J Am Soc Anesthesiologists. 2011;115:364–74.
May LM, Kosek P, Zeidan F, Berkman ET. Enhancement of meditation analgesia by opioid antagonist in experienced meditators. Psychosom Med. 2018;80:807.
Loggia ML, Kim J, Gollub RL, Vangel MG, Kirsch I, Kong J, et al. Default mode network connectivity encodes clinical pain: an arterial spin labeling study. PAIN®. 2013;154:24–33.
Cleeland CS, Ryan K. Pain assessment: global use of the Brief Pain Inventory. Annals of the Academy of Medicine, Singapore. 1994;23:129–38.
Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychological Assess. 1995;7:524.
Roland M, Morris R. A study of the natural history of low-back pain: part II: development of guidelines for trials of treatment in primary care. Spine. 1983;8:145–50.
Trøstheim M, Eikemo M, Haaker J, Frost JJ, Leknes S. Opioid antagonism in humans: a primer on optimal dose and timing for central mu-opioid receptor blockade. Neuropsychopharmacology. 2023;48:299–307.
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19.
Garland EL, Gaylord SA, Palsson O, Faurot K, Douglas Mann J, Whitehead WE. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. J Behav Med. 2012;35:591–602.
Harrison R, Zeidan F, Kitsaras G, Ozcelik D, Salomons TV. Trait mindfulness is associated with lower pain reactivity and connectivity of the default mode network. J Pain. 2019;20:645–54.
Riegner G, Posey G, Oliva V, Jung Y, Mobley W, Zeidan F. Disentangling self from pain: mindfulness meditation-induced pain relief is driven by thalamic-default mode network decoupling. Pain. 2023;164:280–91.
Creswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosom Med. 2007;69:560–5.
Farb NA, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, et al. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci. 2007;2:313–22.
Zeidan F, Salomons T, Farris SR, Emerson NM, Adler-Neal A, Jung Y, et al. Neural mechanisms supporting the relationship between dispositional mindfulness and pain. Pain. 2018;159:2477–85.
Berna C, Leknes S, Ahmad AH, Mhuircheartaigh RN, Goodwin GM, Tracey I. Opioid-independent and opioid-mediated modes of pain modulation. J Neurosci. 2018;38:9047–58.
Garland EL, Hanley AW, Nakamura Y, Barrett JW, Baker AK, Reese SE, et al. Mindfulness-oriented recovery enhancement vs supportive group therapy for co-occurring opioid misuse and chronic pain in primary care: a randomized clinical trial. JAMA Intern Med. 2022;182:407–17.
Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. 2008;134:310–19.
Seminowicz DA, Burrowes SA, Kearson A, Zhang J, Krimmel SR, Samawi L, et al. Enhanced mindfulness based stress reduction (MBSR+) in episodic migraine: a randomized clinical trial with MRI outcomes. Pain. 2020;161:1837.
Garland EL, Roberts RL, Hanley AW, Zeidan F, Keefe FJ. The mindful reappraisal of pain scale (MRPS): validation of a new measure of psychological mechanisms of mindfulness-based analgesia. Mindfulness. 2023;14:192–204.
Kjaer TW, Bertelsen C, Piccini P, Brooks D, Alving J, Lou HC. Increased dopamine tone during meditation-induced change of consciousness. Cogn Brain Res. 2002;13:255–9.
Jinich-Diamant A, Garland E, Baumgartner J, Gonzalez N, Riegner G, Birenbaum J, et al. Neurophysiological mechanisms supporting mindfulness meditation–based pain relief: an updated review. Curr Pain Headache Rep. 2020;24:1–10.
Benedetti F, Thoen W, Blanchard C, Vighetti S, Arduino C. Pain as a reward: changing the meaning of pain from negative to positive co-activates opioid and cannabinoid systems. PAIN®. 2013;154:361–7.
Vajirā, Maha Bodhi society Calcutta. The Sutta-nipāta, one of the oldest canonical books of the Buddhists … (English translation with Pāli text). Maha Bodhi society: Sarnath, U.P.; 1941.
Adler A, Wells R, Stagnaro E, Barber L, Porter A, Garcia K, et al. Mindfulness meditation-induced pain relief does not require endogenous opioidergic systems. J Pain. 2016;17:S112.
Gard T, Holzel BK, Sack AT, Hempel H, Vaitl D, Ott U. Pain attenuation through mindfulness is associated with decreased cognitive control and increased sensory processing in the brain. Cereb Cortex. 2011;191:36–43.
Funding
This work was supported by the National Center for Complementary and Integrative Health (Zeidan R21-AT010352, R01-AT009693, R00-AT008238) and the UC San Diego Denny T. Sanford Institute for Empathy and Compassion.
Author information
Authors and Affiliations
Contributions
Concept and Design: F.Z. Acquisition of Data: LK, NEG, JGD, GR, JB, VO, GC, KC, JM, MP, H-CK. Statistical Analysis, Interpretation of Data, and Drafting of the Manuscript: LK, JGD, FZ. Critical Revision of the Manuscript: LK, JGD, FZ. Supervision: FZ.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khatib, L., Dean, J.G., Oliva, V. et al. The role of endogenous opioids in mindfulness and sham mindfulness-meditation for the direct alleviation of evoked chronic low back pain: a randomized clinical trial. Neuropsychopharmacol. (2023). https://doi.org/10.1038/s41386-023-01766-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41386-023-01766-2