Abstract
Chronic pain and post-traumatic stress disorder (PTSD) are co-occurring conditions that exacerbate the risk of opioid misuse. In this secondary analysis of a randomized clinical trial (NCT02602535), we examined the efficacy of Mindfulness-Oriented Recovery Enhancement (MORE) for reducing PTSD symptoms in patients with chronic pain who misused opioids (N = 241) and who were randomized to MORE or supportive group psychotherapy. Self-reported cognitive reappraisal and skin conductance during an emotion regulation task were tested as mediators of the effect of MORE on changes in PTSD symptoms, and changes in PTSD symptoms were tested as a mediator of the effect of MORE on opioid misuse. MORE led to larger improvements in PTSD symptoms than supportive group psychotherapy across 9 months of follow-up, with 59% of those meeting criteria for a PTSD diagnosis showing clinically significant reductions in PTSD symptoms following treatment with MORE. Changes in reappraisal mediated the effect of MORE on PTSD symptoms, which in turn mediated reduced opioid misuse following MORE. Enhancing reappraisal through MORE may be efficacious for reducing PTSD in opioid-treated chronic pain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data are available from the corresponding author upon reasonable request with an approved data sharing agreement. Requests will be responded to in 30 days. Data will be restricted to de-identified participant data (demographics, summary outcome variables).
Code availability
Coding used for analyses will be shared upon reasonable request. Code will be made available upon publication of this manuscript.
References
Moeller-Bertram, T., Keltner, J. & Strigo, I. A. Pain and post traumatic stress disorder—review of clinical and experimental evidence. Neuropharmacology 62, 586–597 (2012).
Fishbain, D. A., Pulikal, A., Lewis, J. E. & Gao, J. Chronic pain types differ in their reported prevalence of post-traumatic stress disorder (PTSD) and there is consistent evidence that chronic pain is associated with PTSD: an evidence-based structured systematic review. Pain Med. 18, 711–735 (2017).
Åkerblom, S., Perrin, S., Rivano Fischer, M. & McCracken, L. M. The Impact of PTSD on functioning in patients seeking treatment for chronic pain and validation of the posttraumatic diagnostic scale. Int. J. Behav. Med. 24, 249–259 (2017).
Bair, M. J., Outcalt, S. D., Ang, D., Wu, J. & Yu, Z. Pain and psychological outcomes among Iraq and Afghanistan veterans with chronic pain and PTSD: ESCAPE trial longitudinal results. Pain Med. 21, 1369–1376 (2020).
Benedict, T. M., Keenan, P. G., Nitz, A. J. & Moeller-Bertram, T. Post-traumatic stress disorder symptoms contribute to worse pain and health outcomes in veterans with PTSD compared to those without: a systematic review with meta-analysis. Mil. Med. 185, e1481–e1491 (2020).
Langford, D. J. et al. Number and type of post-traumatic stress disorder symptom domains are associated with patient-reported outcomes in patients with chronic pain. J. Pain 19, 506–514 (2018).
Li, H. et al. Relationship between post-traumatic stress disorder symptoms and chronic pain-related symptom domains among military active duty service members. Pain Med. 22, 2876–2883 (2021).
Outcalt, S. D. et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J. Behav. Med. 38, 535–543 (2015).
Ruiz-Párraga, G. T. & López-Martínez, A. E. The contribution of posttraumatic stress symptoms to chronic pain adjustment. Health Psychol. 33, 958–967 (2014).
López-Martínez, A. E., Reyes-Pérez, Á., Serrano-Ibáñez, E. R., Esteve, R. & Ramírez-Maestre, C. Chronic pain, posttraumatic stress disorder, and opioid intake: a systematic review. World J. Clin. Cases 7, 4254–4269 (2019).
Vowles, K. E. et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain 156, 569–576 (2015).
McCance-Katz, E. F. The National Survey on Drug Use and Health (NSDUH): 2020 (Substance Abuse and Mental Health Service Administration, 2020).
Badour, C. L. & Feldner, M. T. Trauma-related reactivity and regulation of emotion: associations with posttraumatic stress symptoms. J. Behav. Ther. Exp. Psychiatry 44, 69–76 (2013).
Chesney, S. A. & Gordon, N. S. Profiles of emotion regulation: understanding regulatory patterns and the implications for posttraumatic stress. Cogn. Emot. 31, 598–606 (2017).
Seligowski, A. V., Lee, D. J., Bardeen, J. R. & Orcutt, H. K. Emotion regulation and posttraumatic stress symptoms: a meta-analysis. Cogn. Behav. Ther. 44, 87–102 (2015).
Tull, M. T., Barrett, H. M., McMillan, E. S. & Roemer, L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behav. Ther. 38, 303–313 (2007).
Wolkenstein, L., Sommerhoff, A. & Voss, M. Positive emotion dysregulation in posttraumatic stress disorder. J. Anxiety Disord. 86, 102534 (2022).
Asmundson, G. J., Coons, M. J., Taylor, S. & Katz, J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can. J. Psychiatry 47, 930–937 (2002).
Bedford, C. E., Nakamura, Y., Marchand, W. R. & Garland, E. L. Heightened autonomic reactivity to negative affective stimuli among active duty soldiers with PTSD and opioid-treated chronic pain. Psychiatry Res. 309, 114394 (2022).
Bosco, M. A., Gallinati, J. L. & Clark, M. E. Conceptualizing and treating comorbid chronic pain and PTSD. Pain Res. Treat. 2013, 174728 (2013).
Jenewein, J., Wittmann, L., Moergeli, H., Creutzig, J. & Schnyder, U. Mutual influence of posttraumatic stress disorder symptoms and chronic pain among injured accident survivors: a longitudinal study. J. Trauma. Stress 22, 540–548 (2009).
Sharp, T. J. & Harvey, A. G. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin. Psychol. Rev. 21, 857–877 (2001).
Ehlers, A. et al. The nature of intrusive memories after trauma: the warning signal hypothesis. Behav. Res. Ther. 40, 995–1002 (2002).
Franke, L. K. et al. Neuroscientific evidence for pain being a classically conditioned response to trauma- and pain-related cues in humans. Pain 163, 2118–2137 (2022).
Macdonald, B., Salomons, T. V., Meteyard, L. & Whalley, M. G. Prevalence of pain flashbacks in posttraumatic stress disorder arising from exposure to multiple traumas or childhood traumatization. Can. J. Pain 2, 48–56 (2018).
Khantzian, E. J. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv. Rev. Psychiatry 4, 231–244 (1997).
Leeies, M., Pagura, J., Sareen, J. & Bolton, J. M. The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depress. Anxiety 27, 731–736 (2010).
Garland, E. L., Hanley, A. W., Thomas, E. A., Knoll, P. & Ferraro, J. Low dispositional mindfulness predicts self-medication of negative emotion with prescription opioids. J. Addict. Med. 9, 61–67 (2015).
Groenewald, C. B., Law, E. F., Fisher, E. Beals-Erickson, S. E. & Palermo, T. M. Associations between adolescent chronic pain and prescription opioid misuse in adulthood. J. Pain 20, 28–37 (2019).
Zvolensky, M. J., Rogers, A. H., Shepherd, J. M., Vujanovic, A. A. & Bakhshaie, J. Anxiety sensitivity and opioid misuse and dependence among trauma-exposed adults with chronic pain. J. Behav. Med. 43, 174–184 (2020).
Bilevicius, E., Sommer, J. L., Asmundson, G. J. G. & El-Gabalawy, R. Posttraumatic stress disorder and chronic pain are associated with opioid use disorder: results from a 2012–2013 American nationally representative survey. Drug Alcohol Depend. 188, 119–125 (2018).
Baker, T. B., Piper, M. E., McCarthy, D. E., Majeskie, M. R. & Fiore, M. C. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol. Rev. 111, 33–51 (2004).
Garland, E. L., Froeliger, B., Zeidan, F., Partin, K. & Howard, M. O. The downward spiral of chronic pain, prescription opioid misuse, and addiction: cognitive, affective, and neuropsychopharmacologic pathways. Neurosci. Biobehav. Rev. 37, 2597–2607 (2013).
Koob, G. F. Neurobiology of opioid addiction: opponent process, hyperkatifeia, and negative reinforcement. Biol. Psychiatry 87, 44–53 (2020).
Koob, G. F., Powell, P. & White, A. Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19. Am. J. Psychiatry 177, 1031–1037 (2020).
Elman, I. & Borsook, D. Common brain mechanisms of chronic pain and addiction. Neuron 89, 11–36 (2016).
Elman, I. & Borsook, D. The failing cascade: comorbid post traumatic stress- and opioid use disorders. Neurosci. Biobehav. Rev. 103, 374–383 (2019).
Baldacchino, A., Balfour, D. J. K., Passetti, F., Humphris, G. & Matthews, K. Neuropsychological consequences of chronic opioid use: a quantitative review and meta-analysis. Neurosci. Biobehav. Rev. 36, 2056–2068 (2012).
Hudak, J. et al. Neurophysiological deficits during reappraisal of negative emotional stimuli in opioid misuse. Biol. Psychiatry. 91, 1070–1078 (2022).
Garland, E. L., Bryan, C. J., Nakamura, Y., Froeliger, B. & Howard, M. O. Deficits in autonomic indices of emotion regulation and reward processing associated with prescription opioid use and misuse. Psychopharmacology 234, 621–629 (2017).
Hudak, J. et al. The temporal dynamics of emotion dysregulation in prescription opioid misuse. Prog. Neuropsychopharmacol. Biol. Psychiatry 104, 110024 (2021).
Baker, K. S., Gibson, S., Georgiou-Karistianis, N., Roth, R. M. & Giummarra, M. J. Everyday executive functioning in chronic pain: specific deficits in working memory and emotion control, predicted by mood, medications, and pain interference. Clin. J. Pain 32, 673–680 (2016).
Ng, S. K. et al. Neural activity during cognitive reappraisal in chronic low back pain: a preliminary study. Scand. J. Pain 21, 586–596 (2021).
Fitzgerald, J. M. et al. An electrocortical investigation of voluntary emotion regulation in combat-related posttraumatic stress disorder. Psychiatry Res. Neuroimaging 249, 113–121 (2016).
Fitzgerald, J. M., DiGangi, J. A. & Phan, K. L. Functional neuroanatomy of emotion and its regulation in PTSD. Harv. Rev. Psychiatry 26, 116–128 (2018).
Rabinak, C. A. et al. Focal and aberrant prefrontal engagement during emotion regulation in veterans with posttraumatic stress disorder. Depress. Anxiety 31, 851–861 (2014).
Pole, N. The psychophysiology of posttraumatic stress disorder: a meta-analysis. Psychol. Bull. 133, 725–746 (2007).
Hopwood, T. L. & Schutte, N. S. A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clin. Psychol. Rev. 57, 12–20 (2017).
Polusny, M. A. et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA 314, 456–465 (2015).
Cherkin, D. C. et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA 315, 1240–1249 (2016).
Hilton, L. et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann. Behav. Med. 51, 199–213 (2017).
Garland, E. L. et al. Mind-body therapies for opioid-treated pain: a systematic review and meta-analysis. JAMA Intern. Med. 180, 91–105 (2020).
Goldberg, S. et al. Mindfulness-based interventions for substance use disorders. Cochrane Database Syst. Rev. 10, CD011723 (2021).
Li, W., Howard, M. O., Garland, E. L., McGovern, P. & Lazar, M. Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J. Subst. Abuse Treat. 75, 62–96 (2017).
Garland, E. L. Mindfulness-Oriented Recovery Enhancement for Addiction, Stress, and Pain (National Association of Social Workers, 2013).
Gross, J. J. & John, O. P. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 85, 348–362 (2003).
Kangaslampi, S. & Peltonen, K. Mechanisms of change in psychological interventions for posttraumatic stress symptoms: a systematic review with recommendations. Curr. Psychol. 41, 258–275 (2022).
Boden, M. T., Bonn-Miller, M. O., Kashdan, T. B., Alvarez, J. & Gross, J. J. The interactive effects of emotional clarity and cognitive reappraisal in posttraumatic stress disorder. J. Anxiety Disord. 26, 233–238 (2012).
Boden, M. T. et al. Emotion regulation and posttraumatic stress disorder: a prospective investigation. J. Soc. Clin. Psychol. 32, 296–314 (2013).
Garland, E., Hanley, A., Goldin, P. & Gross, J. Testing the mindfulness-to-meaning theory: evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLoS ONE 12, e0187727 (2017).
Garland, E., Kiken, L., Faurot, K., Palsson, O. & Gaylord, S. Upward spirals of mindfulness and reappraisal: testing the mindfulness-to-meaning theory with autoregressive latent trajectory modeling. Cogn. Ther. Res. 41, 381–392 (2017).
Hanley, A. W. et al. Modeling the mindfulness-to-meaning theory’s mindful reappraisal hypothesis: replication with longitudinal data from a randomized controlled study. Stress Health. 37, 778–779 (2021).
Garland, E. L. et al. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. J. Consult. Clin. Psychol. 82, 448–459 (2014).
Roberts, R. L., Ledermann, K. & Garland, E. L. Mindfulness-oriented recovery enhancement improves negative emotion regulation among opioid-treated chronic pain patients by increasing interoceptive awareness. J. Psychosom. Res. 152, 110677 (2022).
Parisi, A., Roberts, R. L., Hanley, A. W. & Garland, E. L. Mindfulness-Oriented Recovery Enhancement for addictive behavior, psychiatric distress, and chronic pain: a multilevel meta-analysis of randomized controlled trials. Mindfulness 13, 2396–2412 (2022).
Garland, E. L. et al. Mind-body therapies for opioid-treated pain: a systematic review and meta-analysis. JAMA Intern. Med. 180, 91–105 (2020).
Garland, E. L. et al. Mindfulness-oriented recovery enhancement reduces opioid misuse risk via analgesic and positive psychological mechanisms: a randomized controlled trial. J. Consult. Clin. Psychol. 87, 927–940 (2019).
Garland, E. L. et al. Mindfulness-Oriented Recovery Enhancement vs supportive group therapy for co-occurring opioid misuse and chronic pain in primary care: a randomized clinical trial. JAMA Intern. Med. 182, 407–417 (2022).
Garland, E. L., Roberts-Lewis, A., Tronnier, C. D., Graves, R. & Kelley, K. Mindfulness-Oriented Recovery Enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: proximal outcomes from a pragmatic randomized trial. Behav. Res. Ther. 77, 7–16 (2016).
Cicchetti, D. & Dawson, G. Multiple levels of analysis. Dev. Psychopathol. 14, 417–420 (2002).
Weathers, F. W. et al. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. In Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX (1993).
Weathers, F. W., Huska, J. A., & Keane, T. M. PCL-C for DSM-IV (National Center for PTSD-Behavioral Science Division, 1994).
Butler, S. F., Fernandez, K., Benoit, C., Budman, S. H. & Jamison, R. N. Validation of the revised Screener and Opioid Assessment Measure for Patients with Pain (SOAPP-R). J. Pain 9, 360–372 (2008).
Harrington, T. & Newman, E. The psychometric utility of two self-report measures of PTSD among women substance users. Addict. Behav. 32, 2788–2798 (2007).
Kuyken, W. et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet 386, 63–73 (2015).
Teasdale, J. D. et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J. Consult. Clin. Psychol. 68, 615–23 (2000).
Monson, C. M. et al. Change in posttraumatic stress disorder symptoms: do clinicians and patients agree? Psychol. Assess. 20, 131–138 (2008).
Jamison, R. N. et al. Substance misuse treatment for high-risk chronic pain patients on opioid therapy: a randomized trial. Pain 150, 390–400 (2010).
Lawrence, R., Mogford, D. & Colvin, L. Systematic review to determine which validated measurement tools can be used to assess risk of problematic analgesic use in patients with chronic pain. Br. J. Anaesth. 119, 1092–1109 (2017).
Garland, E. L., Farb, N. A., Goldin, P. R. & Fredrickson, B. L. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol. Inq. 26, 293–314 (2015).
Cuthbert, B. N., Schupp, H. T., Bradley, M. M., Birbaumer, N. & Lang, P. J. Brain potentials in affective picture processing: covariation with autonomic arousal and affective report. Biol. Psychol. 52, 95–111 (2000).
Kreibig, S. D. Autonomic nervous system activity in emotion: a review. Biol. Psychol. 84, 394–421 (2010).
McRae, K., Ciesielski, B. & Gross, J. J. Unpacking cognitive reappraisal: goals, tactics, and outcomes. Emotion 12, 250–255 (2012).
Delgado, M. R., Nearing, K. I., LeDoux, J. E. & Phelps, E. A. Neural circuitry underlying the regulation of conditioned fear and its relation to extinction. Neuron 59, 829–838 (2008).
Zhang, S. et al. Ventromedial prefrontal cortex and the regulation of physiological arousal. Soc. Cogn. Affect. Neurosci. 9, 900–908 (2014).
Hinrichs, R. et al. Mobile assessment of heightened skin conductance in posttraumatic stress disorder. Depress. Anxiety 34, 502–507 (2017).
Hinrichs, R. et al. Increased skin conductance response in the immediate aftermath of trauma predicts PTSD risk. Chronic Stress 3, 247054701984444 (2019).
Back, S. E., Brady, K. T., Sonne, S. C. & Verduin, M. L. Symptom improvement in co-occurring ptsd and alcohol dependence. J. Nerv. Ment. Dis. 194, 690–696 (2006).
McLean, C. P., Su, Y.-J. & Foa, E. B. Mechanisms of symptom reduction in a combined treatment for comorbid posttraumatic stress disorder and alcohol dependence. J. Consult. Clin. Psychol. 83, 655–661 (2015).
Hien, D. A. et al. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s clinical trials network. Am. J. Psychiatry 167, 95–101 (2010).
Davis, T. A. et al. Substance use attenuates physiological responses associated with PTSD among individuals with co-morbid PTSD and SUDs. J. Psychol. Psychother. https://doi.org/10.4172/2161-0487.S7-006 (2013).
Hawn, S. E., Cusack, S. E. & Amstadter, A. B. A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. J. Trauma. Stress 33, 699–708 (2020).
Lane, A. R., Waters, A. J. & Black, A. C. Ecological momentary assessment studies of comorbid PTSD and alcohol use: a narrative review. Addict. Behav. Rep. 10, 100205 (2019).
Roberts, N. P., Roberts, P. A., Jones, N. & Bisson, J. I. Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: a systematic review and meta-analysis. Clin. Psychol. Rev. 38, 25–38 (2015).
Simpson, T. L. et al. Efficacy and acceptability of interventions for co-occurring PTSD and SUD: a meta-analysis. J. Anxiety Disord. 84, 102490 (2021).
McDonald, S. D. & Calhoun, P. S. The diagnostic accuracy of the PTSD checklist: a critical review. Clin. Psychol. Rev. 30, 976–987 (2010).
van Rooij, S. J. H. et al. Impaired right inferior frontal gyrus response to contextual cues in male veterans with PTSD during response inhibition. J. Psychiatry Neurosci. 39, 330–338 (2014).
Zweerings, J. et al. Rt-fMRI neurofeedback-guided cognitive reappraisal training modulates amygdala responsivity in posttraumatic stress disorder. NeuroImage Clin. 28, 102483 (2020).
Jackson, D. C., Malmstadt, J. R., Larson, C. L. & Davidson, R. J. Suppression and enhancement of emotional responses to unpleasant pictures. Psychophysiology 37, 515–522 (2000).
Ochsner, K. N. & Gross, J. J. The cognitive control of emotion. Trends Cogn. Sci. 9, 242–249 (2005).
Wolf, E. J., Miller, M. W. & McKinney, A. E. Emotional processing in PTSD: heightened negative emotionality to unpleasant photographic stimuli. J. Nerv. Ment. Dis. 197, 419–426 (2009).
Hanley, A. W., Garland, E. L. & Tedeschi, R. G. Relating dispositional mindfulness, contemplative practice, and positive reappraisal with posttraumatic cognitive coping, stress, and growth. Psychol. Trauma 9, 526–536 (2017).
Tedeschi, R. G. & Calhoun, L. G. Posttraumatic growth: conceptual foundations and empirical Evidence. Psychol. Inq. https://doi.org/10.1207/s15327965pli1501_01 (2004).
Garland, E. L. Restructuring reward processing with Mindfulness-Oriented Recovery Enhancement: novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Ann. N. Y. Acad. Sci. 1373, 25–37 (2016).
Garland, E. L. et al. Mindfulness-oriented recovery enhancement remediates anhedonia in chronic opioid use by enhancing neurophysiological responses during savoring of natural rewards. Psychol. Med. 53, 2085–2094 (2023).
Elman, I. et al. Functional neuroimaging of reward circuitry responsivity to monetary gains and losses in posttraumatic stress disorder. Biol. Psychiatry 66, 1083–1090 (2009).
Elman, I. et al. Reward and aversion processing in patients with post-traumatic stress disorder: functional neuroimaging with visual and thermal stimuli. Transl. Psychiatry 8, 240 (2018).
Nawijn, L. et al. Reward functioning in PTSD: a systematic review exploring the mechanisms underlying anhedonia. Neurosci. Biobehav. Rev. 51, 189–204 (2015).
Boyd, J. E., Lanius, R. A. & McKinnon, M. C. Mindfulness-based treatments for posttraumatic stress disorder: a review of the treatment literature and neurobiological evidence. J. Psychiatry Neurosci. 43, 7–25 (2018).
King, A. P. et al. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress. Anxiety 30, 638–645 (2013).
Sheehan, D. The MINI International Neuropsychiatric Interview, (Version 7.0. 2) for DSM-5 (Harm Research Institute, 2016).
Gaylord, S. A. et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am. J. Gastroenterol 106, 1678–1688 (2011).
Weathers, F. W., Huska, J. A., & Keane, T. M. PCL-C for DSM-IV (National Center for PTSD-Behavioral Science Division, 1991).
Wu, S. M. et al. The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J. Pain Symptom Manag. 32, 342–351 (2006).
Benedek, M. & Kaernbach, C. A continuous measure of phasic electrodermal activity. J. Neurosci. Methods 190, 80–91 (2010).
Critchley, H. D., Elliott, R., Mathias, C. J. & Dolan, R. J. Neural activity relating to generation and representation of galvanic skin conductance responses: a functional magnetic resonance imaging study. J. Neurosci. 20, 3033–3040 (2000).
Lang, P., Bradley, M. & Cuthbert, B. International Affective Picture System (IAPS): Technical Manual and Affective Ratings (NIMH Center for the Study of Emotion and Attention, 1997).
Hanley, A. W. & Garland, E. L. The Mindfulness-Oriented Recovery Enhancement Fidelity Measure (MORE-FM): development and validation of a new tool to assess therapist adherence and competence. J. Evid. Based J. Evid. Based 18, 308–322 (2021).
IBM SPSS Statistics for Windows (IBM, 2020).
Little, R. J. A. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 83, 1198–1202 (1988).
Newman, D. A. Longitudinal modeling with randomly and systematically missing data: a simulation of ad hoc, maximum likelihood, and multiple imputation techniques. Organ. Res. Methods 6, 328–362 (2003).
Kline, R. B. Principles and Practice of Structural Equation Modeling (Guilford, 2005).
Hayes, A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis: a Regression-Based Approach (Guilford, 2013).
Felder, J. N. et al. Neural mechanisms of subclinical depressive symptoms in women: a pilot functional brain imaging study. BMC Psychiatry 12, 152 (2012).
Danielsen, A. et al. Effects of diazepam and ethanol on heart rate and galvanic skin responses. Acta Pharmacol. Toxicol. 36, 113–122 (1975).
Mahmud, M. S., Fang, H., Wang, H., Carreiro, S. & Boyer, E. Automatic detection of opioid intake using wearable biosensor. In 2018 International Conference on Computing, Networking and Communications (ICNC) 784–788 (IEEE, 2018); https://doi.org/10.1109/ICCNC.2018.8390334
Wade, D. et al. Gender difference in outcomes following trauma-focused interventions for posttraumatic stress disorder: systematic review and meta-analysis. Psychol. Trauma Theory Res. Pract. Policy 8, 356–364 (2016).
West, S. G., Taylor, A. B. & Wu, W. in Handbook of Structural Equation Modeling (ed Hoyle, R. H.) 209–231 (Guilford, 2012).
Lee, T. & Shi, D. A comparison of full information maximum likelihood and multiple imputation in structural equation modeling with missing data. Psychol. Methods 26, 466–485 (2021).
Rosseel, Y. Lavaan: an R package for structural equation modeling and more. Version 0.5–12 (BETA). J. Stat. Softw. 48, 1–36 (2012).
Preacher, K. J., Zyphur, M. J. & Zhang, Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol. Methods 15, 209–233 (2010).
Muthén, L. K. & Muthén, B. O. Mplus User’s Guide 8th edn (Muthén & Muthén, 1998).
Asparouhov, T. & Muthén, B. Advances in Bayesian model fit evaluation for structural equation models. Struct. Equ. Model. https://doi.org/10.1080/10705511.2020.1764360 (2021).
Acknowledgements
Research reported in this article was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number R01DA042033 (principal investigator: E.L.G.). E.L.G. was also supported by R01AT011772, R01DA056537 and R01DA057631 during the preparation of this article. The National Institute on Drug Abuse had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
E.L.G. conceived and designed the study and acquired funding. E.L.G., as principal investigator, had overall responsibility for the management of the study. B.F. developed the emotion regulation task, and J.H. processed the psychophysiological data. A.P. conducted the data analyses. A.P. and E.L.G. wrote the first draft of the report with input from J.H. and B.F. E.L.G. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
E.L.G. is the director of the Center on Mindfulness and Integrative Health Intervention Development. The center provides MORE, mindfulness-based therapy and CBT in the context of research trials at no cost to research participants. However, E.L.G. has received honoraria and payment for delivering seminars, lectures and teaching engagements (related to training clinicians in mindfulness) sponsored by institutions of higher education, government agencies, academic teaching hospitals and medical centers. E.L.G. also receives royalties from the sale of books related to MORE. E.L.G. has also been a consultant and licensor to BehaVR. The other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Alicja Binkowska, Annett Lotzin and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
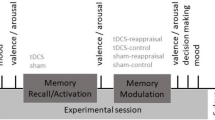
Supplementary Fig. 1.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Parisi, A., Hudak, J., Froeliger, B. et al. Mindfulness-Oriented Recovery Enhancement reduces post-traumatic stress via reappraisal among patients with chronic pain and co-occurring opioid misuse. Nat. Mental Health 1, 489–500 (2023). https://doi.org/10.1038/s44220-023-00084-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00084-2