Abstract
How does craving bias decisions to pursue drugs over other valuable, and healthier, alternatives in addiction? To address this question, we measured the in-the-moment economic decisions of people with opioid use disorder as they experienced craving, shortly after receiving their scheduled opioid maintenance medication and ~24 h later. We found that higher cravers had higher drug-related valuation, and that moments of higher craving within-person also led to higher drug-related valuation. When experiencing increased opioid craving, participants were willing to pay more for personalized consumer items and foods more closely related to their drug use, but not for alternative “nondrug-related” but equally desirable options. This selective increase in value with craving was greater when the drug-related options were offered in higher quantities and was separable from the effects of other fluctuating psychological states like negative mood. These findings suggest that craving narrows and focuses economic motivation toward the object of craving by selectively and multiplicatively amplifying perceived value along a “drug relatedness” dimension.
Similar content being viewed by others
Introduction
The opioid epidemic is a health crisis with disastrous personal and societal costs. Reuse and relapse in opioid use disorder (OUD) is driven in part by craving—the fluctuating, intense, and specific desire for the drug. Craving is an extensively studied and well-established predictor of drug use [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. Yet, we still lack a precise understanding of how the psychological experience of craving translates to pursuit of the drug over other valuable, and healthier, alternatives. Unfortunately, gold-standard OUD treatments (e.g., methadone) do not fully eliminate craving and fail to prevent reuse in many patients [4, 19, 21]. Identifying, and ultimately mitigating, the mechanistic source of craving offers one avenue to monitor and treat OUD more effectively.
We recently developed an experimental approach to quantify how specific craving (e.g., for a chocolate bar) is reflected in decision-making processes [22]. We found that, compared to a baseline of no craving, craving for a specific snack food caused people to pay more for the craved food and for subjectively similar foods, but not for dissimilar options. This shift in subjective valuation was short-lived with a measurable half-life of <1 h. Further, it was well-described by a multiplicative-gain process: craving and amount of the food available were integrated in a nonlinear fashion to “tune” a food’s subjective value. When the craved (and similar) foods were available in larger quantities, willingness-to-pay increased even more, indicating craving selectively and disproportionately increased these options’ values. This suggested (1) craving operates along an attribute-similarity dimension, based on proximity to the object of craving; and that it (2) interacts with valuation (vs. being a separable signal that is “added” to baseline value), by scaling a person’s internal value representation—their utility function in economic terms—for these shared attributes. These characteristics provide an algorithmically precise signature of craving that can explain how, by acting on normal valuation mechanisms, craving modifies specific value and selectively biases decisions toward the object of craving.
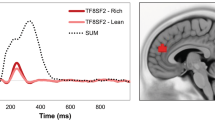
Here, we tested whether the same selective and multiplicative process underlies drug craving, specifically craving for opioids in treatment-engaged OUD patients for whom craving represents a clinically significant barrier to recovery. Given that drug craving is closely tied to cue reactivity, we reasoned that a key attribute dimension in drug craving may be drug associability or relatedness, such that options judged as more related to the drug are imbued with higher value during craving (Fig. 1).
Drug craving in opioid use disorder, like food craving in healthy people, is hypothesized to act on normative valuation mechanisms: opioid craving should selectively amplify the value of options judged as more drug related, and more so when these options are available in higher quantities. This interaction between drug-relatedness, amount, and craving may explain how acute psychological craving biases decisions toward drug seeking and use.
Prior work indicates acute craving for alcohol and nicotine markedly increases behavioral economic demand indices of drug value [23]: people experiencing craving are willing to purchase the craved drug—in a real or hypothetical sense—at higher costs and to consume more of it when it is “free” [24,25,26,27,28,29]. Similar changes in drug value have been observed following 24 h abstinence from opioid medications in OUD [30, 31]. However, these studies have not typically tested whether craving selectively affects drug value nor have they provided a compact model of the underlying process. The few previous studies that have examined the acute impact of craving on alternative nondrug-related outcomes yielded conflicting findings [31,32,33,34,35], and are limited by the use of monetary reward for this purpose (which is associated with drug-seeking and use). The hypothetical nature of many of these studies may also limit inference based on individuals’ “true” preferences as craving evolves.
Craving for drugs, particularly opioids, co-occurs with a mixture of (mostly negative) affective experiences [36,37,38], sometimes referred to as ‘hyperkatifeia’ [39,40,41]. However, negative mood has incidental effects in decision-making [42,43,44], and could be expected to shift value globally rather than specifically for the drug, increasing the attractiveness of both drug- and nondrug-related options. To isolate the specific effect of craving in valuation and advance a mechanistic understanding of how craving biases decisions toward drug-seeking actions in OUD, it may also be necessary to separate craving from negative mood.
In a within-subjects crossover design, here, OUD patients completed a hybrid symptom-capture/willingness-to-pay paradigm, both after receiving their scheduled methadone and ~24 h after the last dose of methadone, a manipulation found previously to promote drug cue reactivity and craving [45]. Willingness-to-pay is related to traditional behavioral economic demand indices but has the key advantage that it can be used to estimate values in a single trial, without the need to summarize data across dozens of trials during which craving levels may be changing. We used this hybrid task to (1) repeatedly sample a person’s “true” (consequential) value for (2) a range of choice options spanning a personalized drug relatedness dimension, orthogonal to key features such as general desirability, while (3) simultaneously and repeatedly assessing their psychological state of craving and other transitory states.
Materials and methods
Participants
Participants were 35 individuals with DSM5-defined OUD, as determined by clinic staff and obtained from patient charts, for whom heroin use was primary and heroin craving was persistent in the past 12 months (i.e., all endorsed the DSM5 “Craving” criterion). All participants were ≥18 years of age, fluent English speakers, and enrolled in an outpatient methadone treatment program, from which they were directly recruited. Informed consent was obtained in accordance with procedures approved by the NYU School of Medicine IRB.
Exclusion criteria were: (1) primary drug of choice other than opioids; (2) head trauma, loss of consciousness >30 min, or neurologic disease; (3) unstable or untreated medical conditions (e.g., late-stage HIV/AIDS); and (4) unstable or untreated psychiatric conditions such as a current manic episode, active psychosis, or suicidal ideation. Inclusion/exclusion criteria and sample characterization were ascertained during a comprehensive interview that included the Addiction Severity Index [46], DSM5 substance use disorders checklist, and Beck Depression [47], and Anxiety [48] Inventories, all administered by the experimenters, and by consulting patient charts. Of the 35 participants consented, 6 were excluded due to problems confirming methadone dosing on testing days/randomization failure, leaving N = 29 included for analysis (age = 47.38 [SD = 11.53] years, 89.7% male, receiving a mean methadone dose = 92.24 [SD = 31.33] mg; Table S1).
Study design
Each participant completed up to three study sessions (Fig. 2). In the first session (Day 1), participants completed clinical assessments, a ratings task that probed multiple dimensions for each of 40 items to be used in the willingness-to-pay task completed at each of two additional sessions, and instructions and practice for the task. In the second and third sessions (Days 2 and 3), participants completed the willingness-to-pay task, followed by two other decision-making tasks (not discussed here). Participants received $20 for the first session and $30 for each of the two task sessions, plus a bonus determined by a single, randomly selected choice made during that session (see below and Supplementary Information). To introduce variability in opioid craving [30, 45], participants were randomized to complete one of the two task sessions after taking their scheduled daily methadone (mean = 1.63 [SD = 1.44] h), and the other ~24 h after the last dose of methadone (mean = 24.84 [SD = 9.28] h), in the window of peak and trough of methadone levels, respectively. Compliance with the treatment manipulation was confirmed via self-report and time-stamped medication dispensing records obtained from the methadone program. The two task sessions were separated by 12.2 (SD = 18.76) days. All N = 29 participants completed the first session and at least one of the two task sessions; 23 completed all three sessions, for a total of 81 sessions included for analysis. Of the 6 participants that completed only one task session, 3 did so 24 h after methadone dosing, and 3 shortly after methadone dosing (randomization preserved). There was no systematic dropout related to the study procedures. Reasons for non-completion included treatment dropout, hospitalization, and/or scheduling conflicts. Apart from a slight increase in withdrawal 24 h after methadone dosing, there were no baseline differences in clinical status across the three study days (Table S2).
A On Day 1, participants rated each of 40 common consumer items and snack foods on their subjective drug relatedness and general desirability, among other dimensions. For each participant, these ratings were used to sub-select a 12-item choice set that (1) provided maximal spread in drug relatedness (that was of main interest here), while (2) de-coupling this dimension from general desirability thus minimizing the possibility of a systematic bias in the desirability of the items chosen as drug-related or nondrug-related (see Supplementary Information for details on selection of the initial 40-item fixed set and the choice set personalization procedure). The final selected choice sets only partly overlapped across participants, revealing a high degree of subjectivity in drug relatedness judgements (Fig. S1). B Following screening and choice set selection on Day 1, participants completed two task sessions, one after taking their daily methadone dose and the other ~24 h since the last dose of methadone (Days 2 and 3, randomized crossover order). Each task session was composed of 4 blocks. Each block was composed of 101 trials. Trials were randomly presented and consisted of 48 willingness-to-pay bid trials for each of the 12 items in the personalized choice set presented in 4 different quantities (depicted in blue), 48 desire rating trials for each of the same 12 items × 4 quantities (gray), 3 mood rating trials for each of happiness, stress, and boredom (teal), and 2 craving rating trials for each of heroin and methadone (red). For purposes of analysis, the three mood state ratings were averaged for each block into a composite negative mood measure and the two craving ratings were averaged into a composite opioid craving measure. To incentivize participants to provide their “true” momentary value (i.e., bid) for each item and to report only on their current subjective experience in each block, the task was structured such that it could end with a fixed (2%) probability after each block in a session, ending regardless after the 4th block. At the end of the session, one bid trial from the last completed block was randomly selected and played out to determine a participant’s bonus.
Choice set selection (Day 1)
Because cues associated with drug use and craving are highly subjective [49, 50], we developed personalized choice sets for each participant, selected from a broader fixed set. Participants rated 40 consumer items and snack foods on five subjective dimensions: drug relatedness, (general) desirability, frequency of use/consumption, tastiness of snacks, and healthiness of snacks. Ratings used a continuous rating scale, which varied based on the dimension probed (e.g., “Not at all likely [to make me think of using heroin and other drugs]” to “Extremely likely [to make me think of using heroin and other drugs]” or “Not at all [desirable]” to “Extremely [desirable]”). Responses from the ratings task were used to sub-select 12 consumer items and snack foods (personalized for each individual) to be offered during the willingness-to-pay task completed in subsequent sessions. Choice sets were selected to ensure maximal spread in the drug relatedness dimension while maintaining little or no correlation between general desirability and drug relatedness, by iteratively and randomly selecting 12-item sets (6 consumer items, 6 snack foods) and computing the correlation between the two ratings until a sub-set met a P > 0.25 cut-off (equivalent to R < | 0.2058 | , or small-to-moderate association). This procedure aimed to minimize potential confounding effects due to differences in the general value/desirability of the more/less drug-related items, as confirmed in post-hoc analyses showing general desirability did not significantly relate to drug relatedness for the final 12-item choice set selected for each participant (B = 0.06, t105.15 = 1.12, P = 0.27). Supplementary Information provides detailed instructions given to participants for the ratings tasks and additional details on the choice set optimization procedure, and Fig. 2A shows an illustrative example of the latter.
Willingness-to-pay task (Days 2 and 3)
Participants completed a modified task [22] composed of bid trials (our measure of subjective value), desire rating trials, and mood/craving rating trials. In bid trials, participants indicated their willingness to pay in the current moment (from $0 to $15 in $0.02 increments) for each item in their 12-item choice set, offered one at a time in one of four quantities (1, 3, 5, or 8 units). For these trials, participants were explicitly instructed to bid the maximum amount they would pay right now for the item(s) shown, for the real chance of getting the item(s) right now. In desire rating trials, participants indicated their desire in the current moment for each item, again offered in different quantities. Specifically, they were instructed to indicate how much they want the item(s) shown right now, without any consequence for whether or not they can have the item(s) right now (non-contingent response). As in our prior study, desire ratings were included to standardize the strategy/cognitive process participants engaged in placing their bids (i.e., they were encouraged to base their bids on their current desire for each item rather than e.g., market prices). In mood rating trials, participants reported on their current feelings of boredom, stress, and happiness. In craving rating trials, current desire for heroin and methadone was used to evaluate overall opioid craving. All rating trials employed a continuous rating scale presented below a picture cue identifying the rating type (see Fig. 2B and Supplementary Information for detailed instructions given to participants for each trial type).
In each task block (maximum of 4 per session), participants submitted one bid and one desire rating for each item and quantity (N = 2 × 12 ×4 = 96), and one rating for each mood/craving (N = 3 + 2 = 5), for 101 trials/block. Trials were self-paced, separated by a variable 0.5–1.0 s inter-trial-interval, and fully randomized within a block (Fig. 2B). To capture participants’ “true” momentary valuation in an incentive-compatible manner, we implemented a fixed hazard rate such that the task had 2% chance of ending after each block, ending after the 4th block regardless. At the end of each session/day, one bid trial was randomly selected from the last completed block and realized using an auction procedure to determine a participant’s bonus, in the form of money, the item(s) shown on that trial, or both. Both the (small) probability of the task ending early and the auction procedure were fully described to participants (see Supplementary Information). In total, participants completed an average of 710 trials (~7 blocks) across the two task sessions/days.
Data analysis
Our primary analytic approach was linear mixed effects regression, with bid for item i, participant j, and trial t as the outcome variable. Because momentary (block-to-block) methadone craving strongly positively correlated with heroin craving (P = 3.9 × 10–15), and to increase robustness of our block-level estimate of craving given only a single randomly interspersed craving rating per drug type was collected in each block, the two ratings were averaged into a composite “opioid craving” measure for analysis. Similarly, block-to-block reported stress, the inverse of happiness, and boredom were correlated (P = 0.04–5.7 × 10–7) and combined into a composite “negative mood” measure. The initial model assessed whether participants’ bids were predicted by an item’s drug relatedness, participant-mean level of reported opioid craving, participant mean-centered craving in the local task block, and the interaction between these factors (Model 1). This permitted separately assessing between-person and within-person contributions of craving to drug-related valuation, respectively [51]. Potential effect modifiers were also explored building on this model, and included study day, item general desirability, and between- and within-person negative mood. To further probe the mechanism of anticipated value change, item quantity and its interactions with drug relatedness and craving were added as additional predictors (Model 2; Table 1). Models were estimated in MATLAB (fitlme) and R (lme4) and included random intercepts and random slopes for drug relatedness (which differed across participants but remained constant across days/blocks; Models 1 and 2) and quantity (Model 2) by participant. Degrees of freedom for significance testing were computed using Satterthwaite approximation.
Results
Opioid craving selectively increases drug-related valuation
Opioid craving was higher 24 h since vs. shortly after methadone dosing (B = 0.20, SE = 0.05, t27.09 = 3.67, P = 0.001; Fig. 3A) and varied substantially person-to-person as well as within-person, block-to-block (intraclass correlation coefficient = 0.56; Fig. 3B). To examine whether both between- and within-person craving effects may be present in participants’ concomitant valuation behavior, we first tested whether trial-by-trial bids varied with an item’s drug relatedness and the interaction of drug relatedness and craving (Model 1a). As expected, given participants were treatment-motivated, bids scaled negatively with drug relatedness: participants bid less for items they rated as more drug-related (B = −1.95, P = 0.0003; Table 1). However, we observed significant positive interactions between drug relatedness and both between- and within-person craving: participants who reported overall more craving bid more for items they rated as more drug-related (B = 2.56, P = 0.03), and moments of higher craving within-person also led to higher drug-related valuation (B = 1.21, P = 0.003; i.e., the negative relationship between bids and drug relatedness was lessened in moments of higher craving, Fig. 4A). These interaction effects were robust to study day (Table 1, Model 1b); they were also qualitatively similar for methadone and heroin craving when considered as separate forms of craving but were not better captured by either alone (Table S3 and Supplementary Information).
A Momentary reported opioid craving (% of scale’s max) by study day (after 24 h from methadone dosing and shortly after dosing; randomized order) and task block (up to four) within a day. Craving was higher 24 h after methadone dosing and varied substantially both between- and within-person across the task blocks (intraclass correlation coefficient = 0.56). B Within-person variability in reported craving (range in opioid craving ratings; gray points show single-participant data) was comparable across blocks within a day to variability across days. ***P = 0.001, n.s. nonsignificant.
A Change in the subjective value (bid) for each of the task items on offer with opioid craving, ranked by the individually rated drug relatedness of each item across participants. B Subjective value (bids) for each quantity of the item with the lowest and highest drug relatedness in the choice set for each participant (shaded areas in A), at the lowest (peach), and highest (dark red) opioid craving task blocks for that participant. For visualization purposes, only data for each participant’s highest vs. lowest craving blocks (both panels) and highest vs. lowest drug-related items (B) are shown. The analyses reported in the text and tables used the full dataset. See Table 1 and Supplementary Information, Tables S3–S5.
Interestingly, while participants assigned higher value to the items they rated as more (generally) desirable (B = 2.73, P = 0.03), opioid craving as assessed between- or within-person did not interact with item desirability to increase bids (B < | 3.90 |, P > 0.18) and controlling for item desirability did not modify the relationship between craving and drug relatedness (P < 0.05; Table S4). That is, craving appears to interact specifically with drug-related valuation and not general valuation.
These effects also appear to be specific to craving and are not explained by global changes in negative mood. While as expected, participants’ momentary negative mood correlated with their reported opioid craving (B = 0.30, SE = 0.08, t175.15 = 3.72, P = 0.0003), negative mood as assessed between- or within-person did not interact with item drug relatedness to increase bids (B < | 0.88 |, P > 0.59) and controlling for negative mood did not modify the relationship between craving and drug relatedness (P < 0.03; Table S4).
Opioid craving increases drug-related valuation through a multiplicative gain-like mechanism
Our earlier work [22] indicated craving operates via a multiplicative-gain process, increasing subjective values placed on a class of goods based on the quantity of those goods (Fig. 1). If that is true for drug craving, then craving would increase not just the value of a single item but would “tilt” the entire curve that relates increasing quantities of drug-related items to subjective value. While somewhat counter-intuitive, this is a specific prediction of our earlier work, and it allows us to make strong mechanistic statements about value representation and craving.
To test this prediction, we included item quantity and its interaction with drug relatedness and craving as additional predictors of participants’ trial-to-trial bids (Model 2, Table 1). We found significant 3-way interactions that were again present at both the between- and within-person levels (B > 0.26, P < 0.04): participants who reported overall more craving bid disproportionately more for items rated as more drug-related specifically when these items were offered in higher quantities, and moments of higher craving also led to higher drug-related valuation for higher quantity offers (Fig. 4B). This suggests craving is reflected in drug-related valuation regardless of quantity but that this effect is stronger with increasing unit size, consistent with a pattern of escalating seeking behavior during craving.
In exploratory analyses, to examine more subtle changes in the relationship between quantity and bids, we fit a power function to participants’ data, for each item at each session and block, which was defined by a linear slope term (ω) and curvature (α). This permitted testing two possible ways that craving might scale drug-related valuation: multiplicatively, as evidenced by a shift in the ω term, or exponentially, as evidenced by a shift in the α term. Assessing these possibilities is important because an exponential shift would indicate craving fundamentally changes the valuation process (akin to a change in the internal value or utility function), while a multiplicative shift would indicate this process is preserved but scaled (akin to a gain-like effect on value). Consistent with a multiplicative shift, we observed a positive interaction between drug relatedness and within-person opioid craving on ω (B = 0.59, P = 0.048): ω was higher for items rated as more drug-related and when participants reported experiencing higher craving. We found nonsignificant between-person effects of craving for ω, and nonsignificant between- and within-person effects for the curvature parameter (α) suggesting that the core mechanism for placing values on goods remains unchanged during craving (Table S5).
Discussion
We examined whether opioid craving, like food craving in health, operates in a selective manner in valuation, which may help to clarify how craving works to bias decisions toward drug-seeking actions and away from other valuable, and healthier, alternatives in treatment-engaged people with OUD. Applying a neuroeconomic framework that captured participants’ in-the-moment valuation of choice options spanning a continuous “drug relatedness” dimension, we found that opioid craving increased the relative subjective value of those options judged as more drug-related, and disproportionately so when they were offered in higher quantities. These effects were observed at both the between- and within-person levels, indicating higher “cravers” had higher drug-related valuation, and that, critically, moments of higher craving within-person also led to higher drug-related valuation. While fluctuation in negative mood state was, as predicted, associated with craving, negative mood did not have a comparable, direct effect in drug-related valuation. Collectively, these data suggest a shared (and outcome-specific) normative valuation process underlies drug and food craving, and provide specific predictions about the mechanism by which craving might interact with subjective valuation behaviorally and neurally.
The concept of “relative value” is central to theories of addiction grounded in behavioral economics [52, 53] and has been the focus of much work in other pertinent domains in addiction such as diagnosis and prognosis [54,55,56,57,58,59,60,61,62,63,64,65]. However, the specific effect of craving in drug- vs. nondrug-related valuation has received comparatively less attention. Using a design that specifically permitted assessing how craving operates along a drug relatedness dimension, we observed that craving positively interacted with this dimension, scaling subjective value for options that were deemed more (personally) drug-related. Further, we observed this effect regardless of an option’s general desirability, which was confirmed by (1) orthogonalizing drug relatedness and desirability in our choice set construction, and by (2) directly assessing value changes as a function of both drug relatedness and desirability. These data suggest craving acts on drug-related associative mechanisms, rather than through a general reinforcement process, and can help explain how craving specifically drives choice behavior toward the object of craving (and cues associated with drug-seeking and use).
Notably, craving had a multiplicative–gain-like–effect, amplifying participants’ assigned value for more drug-related options when these options were available in higher quantities. This can explain escalating drug-seeking behavior seen clinically with craving [4, 7, 19, 20] and in animal models of related constructs [66, 67]. It also provides a specific algorithmic process for future neurobiological work on craving which can be well tied to our basic understanding of the brain’s valuation circuitry. Neural circuits for craving and cue reactivity overlap with those generally involved in value-based decision-making, in particular the ventromedial prefrontal cortex and ventral striatum [68, 69], which receive dense dopaminergic inputs widely implicated in addiction [67], subjective craving responses [70, 71], and neural gain control [72, 73]. Interestingly, the topographical distribution of value codes within this circuitry, and especially ventral prefrontal cortex, appears to be at least partly outcome- (or attribute-category) specific [74,75,76,77]. We can speculate that the behavioral selectivity of craving in drug-related valuation (or similarly rated snacks foods in the case of food craving, as described previously) could stem from (possibly dopamine-dependent) modulation of outcome-specific value representations within this circuitry or at inputs to it, allowing for selective hyper-valuation with craving, as previously found with selective de-valuation [78].
While opioid craving in the current study and food craving in our previous work seem to operate in valuation via a shared mechanism, we also observed some notable differences. In our food study, healthy participants were willing to pay more for craved foods they found generally desirable; in contrast, treatment-engaged patients with OUD showed craving-modulated valuation behavior that was exclusively tied to the drug relatedness of the options on offer, irrespective of their general desirability. Thus, craving in addiction may transiently decouple desirability from valuation, in line with prominent habit-based theories of addiction and drug choice [79, 80] (although see [81, 82]). Further, although drug relatedness was negatively associated with subjective value in our treatment-engaged sample, craving seemed to flatten this beneficial response, highlighting the potential for risk for reuse and relapse during craving even under effective treatment.
Also distinct from food craving, which can be positively motivating [83], opioid craving is typically experienced as a negative affective state [36,37,38,39,40,41]. To determine the influence of concomitant negative mood, we continuously assessed participants’ current stress, happiness, and boredom. Although negative mood correlated positively with opioid craving, mood state shifts did not explain the relationship between craving and drug-related valuation, echoing prior work showing incidental and diffusive effects of mood in decision-making [42, 43], unlike the specific effect we observed with craving, which narrowed and focused motivation specifically toward the object of craving.
Several important limitations should be considered for future research. First, we relied on a single-item measure of craving as a proxy of craving more generally. Such single-item measures, while commonly used to evaluate in-the-moment experience, may fail to capture the multifaceted nature of craving, particularly in treatment-seekers where perceived ability to control want or desire may feature prominently [19, 84]. It would be prudent for future research to capture these additional facets in drug-related valuation, as well as determine how craving-modulated valuation changes over the treatment cycle from active use through treatment stabilization and in relation to actual drug-use behavior. Second, our sample was primarily male, reflecting known biases in treatment utilization and availability for women [85]. Given research suggesting sex-specific susceptibility to opioid craving and reuse [86], this sampling bias may contribute to an overall underestimation of the reported effects in women.
In summary, our results point to a signature of craving that can be applied to addiction specifically but used to describe craving more generally—one that is selective, operates on dimensional attribute-based similarity, and that is multiplicative of subjective value. Selectivity is indicated by the increased valuation of options closely associated with the object of craving (i.e., drugs or food), dimensionality by the way these options are valued based on their features (i.e., proximity to what is being craved), and multiplication by the scaling effect of quantity. From a clinical viewpoint, our experimental approach may be useful to uncover the cognitive processes underlying persistent craving in patients receiving gold-standard OUD treatments. Given the recent push for craving to be more clearly defined, measured, and incorporated into treatment targets for OUD [19, 84], our experimental approach presents a promising step in the development of measures that can both track craving over time and assess the effectiveness of interventions that aim to selectively block its effect on drug-related valuation.
References
Northrup TF, Stotts AL, Green C, Potter JS, Marino EN, Walker R, et al. Opioid withdrawal, craving, and use during and after outpatient buprenorphine stabilization and taper: a discrete survival and growth mixture model. Addict Behav. 2015;41:20–8.
Weiss RD, Potter JS, Griffin ML, McHugh RK, Haller D, Jacobs P, et al. Reasons for opioid use among patients with dependence on prescription opioids: the role of chronic pain. J Subst Abus Treat. 2014;47:140–5.
Konova AB, Lopez-Guzman S, Urmanche A, Ross S, Louie K, Rotrosen J, et al. Computational markers of risky decision-making for identification of temporal windows of vulnerability to opioid use in a real-world clinical setting. JAMA Psychiatry. 2020;77:368–77.
Kakko J, Alho H, Baldacchino A, Molina R, Nava FA, Shaya G. Craving in opioid use disorder: From neurobiology to clinical practice. Front Psychiatry. 2019;10:592.
Garland EL, Howard MO. Opioid attentional bias and cue-elicited craving predict future risk of prescription opioid misuse among chronic pain patients. Drug Alcohol Depend. 2014;144:283–7.
Wasan AD, Ross EL, Michna E, Chibnik L, Greenfield SF, Weiss RD, et al. Craving of prescription opioids in patients with chronic pain: A longitudinal outcomes trial. J Pain. 2012;13:146–54.
Tiffany ST, Wray JM. The clinical significance of drug craving. Ann N. Y Acad Sci. 2012;1248:1–17.
Martel MO, Dolman AJ, Edwards RR, Jamison RN, Wasan AD. The association between negative affect and prescription opioid misuse in patients with chronic pain: The mediating role of opioid craving. J Pain. 2014;15:90–100.
Hulse GK, Ngo HT, Tait RJ. Risk factors for craving and relapse in heroin users treated with oral or implant naltrexone. Biol Psychiatry. 2010;68:296–302.
Tsui JI, Anderson BJ, Strong DR, Stein MD. Craving predicts opioid use in opioid-dependent patients initiating buprenorphine treatment: A longitudinal study. Am J Drug Alcohol Abus. 2014;40:163–9.
McHugh RK, Fitzmaurice GM, Carroll KM, Griffin ML, Hill KP, Wasan AD, et al. Assessing craving and its relationship to subsequent prescription opioid use among treatment-seeking prescription opioid dependent patients. Drug Alcohol Depend. 2014;145:121–6.
Moore TM, Seavey A, Ritter K, McNulty JK, Gordon KC, Stuart GL. Ecological momentary assessment of the effects of craving and affect on risk for relapse during substance abuse treatment. Psychol Addict Behav. 2014;28:619–24.
Marhe R, Waters AJ, van de Wetering BJ, Franken IH. Implicit and explicit drug-related cognitions during detoxification treatment are associated with drug relapse: an ecological momentary assessment study. J Consult Clin Psychol. 2013;81:1–12.
Epstein DH, Willner-Reid J, Vahabzadeh M, Mezghanni M, Lin JL, Preston KL. Real-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Arch Gen Psychiatry. 2009;66:88–94.
Phillips KA, Epstein DH, Preston KL. Daily temporal patterns of heroin and cocaine use and craving: relationship with business hours regardless of actual employment status. Addict Behav. 2013;38:2485–91.
Fatseas M, Serre F, Alexandre JM, Debrabant R, Auriacombe M, Swendsen J. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: a comparison of substance- and person-specific cues. Addiction 2015;110:1035–42.
Epstein DH, Marrone GF, Heishman SJ, Schmittner J, Preston KL. Tobacco, cocaine, and heroin: Craving and use during daily life. Addict Behav. 2010;35:318–24.
Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin JL, et al. Before and after: craving, mood, and background stress in the hours surrounding drug use and stressful events in patients with opioid-use disorder. Psychopharmacol (Berl). 2018;235:2713–23.
Kleykamp BA, De Santis M, Dworkin RH, Huhn AS, Kampman KM, Montoya ID, et al. Craving and opioid use disorder: A scoping review. Drug Alcohol Depend. 2019;205:107639.
Hasin DS, Fenton MC, Beseler C, Park JY, Wall MM. Analyses related to the development of DSM-5 criteria for substance use related disorders: 2. Proposed DSM-5 criteria for alcohol, cannabis, cocaine and heroin disorders in 663 substance abuse patients. Drug Alcohol Depend. 2012;122:28–37.
Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies-tackling the opioid-overdose epidemic. N. Engl J Med. 2014;370:2063–6.
Konova AB, Louie K, Glimcher PW. The computational form of craving is a selective multiplication of economic value. Proc Natl Acad Sci USA. 2018;115:4122–7.
Acuff SF, Amlung M, Dennhardt AA, MacKillop J, Murphy JG. Experimental manipulations of behavioral economic demand for addictive commodities: a meta-analysis. Addiction 2020;115:817–31.
Amlung MT, McCarty KN, Morris DH, Tsai CL, McCarthy DM. Increased behavioral economic demand and craving for alcohol following a laboratory alcohol challenge. Addiction 2015;110:1421–28.
Amlung M, MacKillop J. Understanding the effects of stress and alcohol cues on motivation for alcohol via behavioral economics. Alcohol Clin Exp Res. 2014;38:1780–9.
Amlung MT, Acker J, Stojek MK, Murphy JG, MacKillop J. Is talk “cheap”? An initial investigation of the equivalence of alcohol purchase task performance for hypothetical and actual rewards. Alcohol Clin Exp Res. 2012;36:716–24.
MacKillop J, O’Hagen S, Lisman SA, Murphy JG, Ray LA, Tidey JW, et al. Behavioral economic analysis of cue-elicited craving for alcohol. Addiction 2010;105:1599–607.
MacKillop J, Brown CL, Stojek MK, Murphy CM, Sweet LH, Niaura RS. Behavioral economic analysis of withdrawal- and cue-elicited craving for tobacco: An initial investigation. Nicotine Tob Res. 2012;14:1426–34.
Acker J, MacKillop J. Behavioral economic analysis of cue-elicited craving for tobacco: A virtual reality study. Nicotine Tob Res. 2013;15:1409–16.
Badger GJ, Bickel WK, Giordano LA, Jacobs EA, Loewenstein G, Marsch L. Altered states: The impact of immediate craving on the valuation of current and future opioids. J Health Econ. 2007;26:865–76.
Giordano LA, Bickel WK, Loewenstein G, Jacobs EA, Marsch L, Badger GJ. Mild opioid deprivation increases the degree that opioid-dependent outpatients discount delayed heroin and money. Psychopharmacol (Berl). 2002;163:174–82.
Yi R, Landes RD. Temporal and probability discounting by cigarette smokers following acute smoking abstinence. Nicotine Tob Res. 2012;14:547–58.
Roewer I, Wiehler A, Peters J. Nicotine deprivation, temporal discounting and choice consistency in heavy smokers. J Exp Anal Behav. 2015;103:62–76.
Field M, Rush M, Cole J, Goudie A. The smoking Stroop and delay discounting in smokers: effects of environmental smoking cues. J Psychopharmacol. 2007;21:603–10.
Mackillop J, Menges DP, McGeary JE, Lisman SA. Effects of craving and DRD4 VNTR genotype on the relative value of alcohol: an initial human laboratory study. Behav Brain Funct. 2007;3:11.
Preston KL, Epstein DH. Stress in the daily lives of cocaine and heroin users: relationship to mood, craving, relapse triggers, and cocaine use. Psychopharmacology 2011;218:29–37.
Hyman SM, Fox H, Hong KIA, Doebrick C, Sinha R. Stress and drug-cue-induced craving in opioid-dependent individuals in naltrexone treatment. Exp Clin Psychopharmacol. 2007;15:134–43.
Schlauch RC, Gwynn-Shapiro D, Stasiewicz PR, Molnar DS, Lang AR. Affect and craving: Positive and negative affect are differentially associated with approach and avoidance inclinations. Addictive Behav. 2013;38:1970–9.
Pantazis CB, Gonzalez LA, Tunstall BJ, Carmack SA, Koob GF, Vendruscolo LF. Cues conditioned to withdrawal and negative reinforcement: Neglected but key motivational elements driving opioid addiction. Sci Adv. 2021;7:1:13.
Koob GF. Neurobiology of opioid addiction: Opponent process, hyperkatifeia, and negative reinforcement. Biol Psychiatry. 2020;87:44–53.
Koob GF. Neurobiological substrates for the dark side of compulsivity in addiction. Neuropharmacology 2009;56:18–31.
Phelps EA, Lempert KM, Sokol-Hessner P. Emotion and Decision Making: Multiple Modulatory Neural Circuits. Annu Rev Neurosci. 2014;37:263–87.
Lempert KM, Phelps EA Neuroeconomics of emotion and decision making In: Glimcher PW, Fehr E, editors. Neuroeconomics: Decision making and the brain. New York, NY: Academic Press; 2013.
Hogarth L, Hardy L, Bakou A, Mahlberg J, Weidemann G, Cashel S, et al. Negative mood induction increases choice of heroin versus food pictures in opiate-dependent individuals: Correlation with self-medication coping motives and subjective reactivity. Front Psychiatry. 2019;10:274.
Langleben DD, Ruparel K, Elman I, Busch-Winokur S, Pratiwadi R, Loughead J, et al. Acute effect of methadone maintenance dose on brain FMRI response to heroin-related cues. Am J Psychiatry. 2008;165:390–4.
McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the addiction severity index. J Subst Abus Treat. 1992;9:199–213.
Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2 ed. The Psychological Corporation: San Antonio; 1996.
Beck AT, Steer RA. Beck Anxiety Inventory Manual. Harcourt Brace and Company: San Antonio; 1993.
McHugh RK, Fulciniti F, Mashhoon Y, Weiss RD. Cue-induced craving to paraphernalia and drug images in opioid dependence. Am J Addictions. 2016;25:105–9.
McHugh RK, Park S, Weiss RD. Cue-induced craving in dependence upon prescription opioids and heroin. Am J Addictions. 2014;23:453–8.
Wang LP, Maxwell SE. On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychol Methods. 2015;20:63–83.
Lenoir M, Ahmed SH. Supply of a nondrug substitute reduces escalated heroin consumption. Neuropsychopharmacology 2008;33:2272–82.
Greenwald MK, Steinmiller CL. Behavioral economic analysis of opioid consumption in heroin-dependent individuals: Effects of alternative reinforcer magnitude and post-session drug supply. Drug Alcohol Depend. 2009;104:84–93.
Pickover AM, Messina BG, Correia CJ, Garza KB, Murphy JG. A behavioral economic analysis of the nonmedical use of prescription drugs among young adults. Exp Clin Psychopharmacol. 2016;24:38–47.
Strickland JC, Lile JA, Stoops WW. Evaluating non-medical prescription opioid demand using commodity purchase tasks: Test-retest reliability and incremental validity. Psychopharmacol (Berl). 2019;236:2641–52.
Schwartz LP, Blank L, Hursh SR. Behavioral economic demand in opioid treatment: Predictive validity of hypothetical purchase tasks for heroin, cocaine, and benzodiazepines. Drug Alcohol Depend. 2021;221:108562.
Bickel WK, Snider SE, Quisenberry AJ, Stein JS. Reinforcer pathology: The behavioral economics of abuse liability testing. Clin Pharm Ther. 2017;101:185–7.
MacKillop J. The behavioral economics and neuroeconomics of alcohol use disorders. Alcohol Clin Exp Res. 2016;40:672–85.
Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annu Rev Clin Psychol. 2014;10:641–77.
Strickland JC, Campbell EM, Lile JA, Stoops WW. Utilizing the commodity purchase task to evaluate behavioral economic demand for illicit substances: a review and meta-analysis. Addiction 2020;115:393–406.
Gonzalez-Roz A, Jackson J, Murphy C, Rohsenow DJ, MacKillop J. Behavioral economic tobacco demand in relation to cigarette consumption and nicotine dependence: A meta-analysis of cross-sectional relationships. Addiction 2019;114:1926–40.
Martinez-Loredo V, Gonzalez-Roz A, Secades-Villa R, Fernandez-Hermida JR, MacKillop J. Concurrent validity of the alcohol purchase task for measuring the reinforcing efficacy of alcohol: an updated systematic review and meta-analysis. Addiction. 2020.
Versace F, Engelmann JM, Deweese MM, Robinson JD, Green CE, Lam CY, et al. Beyond cue reactivity: Non-drug-related motivationally relevant stimuli are necessary to understand reactivity to drug-related Cues. Nicotine Tob Res. 2017;19:663–9.
Hogarth L, Field M. Relative expected value of drugs versus competing rewards underpins vulnerability to and recovery from addiction. Behav Brain Res. 2020;394:112815.
Moeller SJ, Hanley AW, Garland EL Behavioral preference for viewing drug v. pleasant images predicts current and future opioid misuse among chronic pain patients. Psychol Med. 2020;50:1–9.
Venniro M, Caprioli D, Shaham Y. Animal models of drug relapse and craving: From drug priming-induced reinstatement to incubation of craving after voluntary abstinence. Prog Brain Res. 2016;224:25–52.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev. 1993;18:247–91.
Bartra O, McGuire JT, Kable JW. The valuation system: a coordinate-based meta-analysis of BOLD fMRI experiments examining neural correlates of subjective value. Neuroimage 2013;76:412–27.
Clithero JA, Rangel A. Informatic parcellation of the network involved in the computation of subjective value. Soc Cogn Affect Neurosci. 2014;9:1289–302.
Zijlstra F, Booij J, van den Brink W, Franken IH. Striatal dopamine D2 receptor binding and dopamine release during cue-elicited craving in recently abstinent opiate-dependent males. Eur Neuropsychopharmacol: J Eur Coll Neuropsychopharmacol. 2008;18:262–70.
Volkow ND, Wang GJ, Telang F, Fowler JS, Logan J, Childress AR, et al. Cocaine cues and dopamine in dorsal striatum: mechanism of craving in cocaine addiction. J Neurosci. 2006;26:6583–8.
Servan-Schreiber D, Printz H, Cohen JD. A network model of catecholamine effects: gain, signal-to-noise ratio, and behavior. Science 1990;249:892.
Montague PR, Hyman SE, Cohen JD. Computational roles for dopamine in behavioural control. Nature 2004;431:760–7.
Howard JD, Gottfried JA, Tobler PN, Kahnt T. Identity-specific coding of future rewards in the human orbitofrontal cortex. Proc Natl Acad Sci USA. 2015;112:5195–200.
Kahnt T. A decade of decoding reward-related fMRI signals and where we go from here. Neuroimage 2018;180:324–33.
McNamee D, Rangel A, O’Doherty JP. Category-dependent and category-independent goal-value codes in human ventromedial prefrontal cortex. Nat Neurosci. 2013;16:479–85.
Stalnaker TA, Cooch NK, McDannald MA, Liu TL, Wied H, Schoenbaum G. Orbitofrontal neurons infer the value and identity of predicted outcomes. Nat Commun. 2014;5:3926.
Howard JD, Kahnt T. Identity-specific reward representations in orbitofrontal cortex are modulated by selective devaluation. J Neurosci. 2017;37:2627–38.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neuro. 2005;8:1481–9.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: Role of automatic and nonautomatic processes. 1990;97:147–68.
Vandaele Y, Ahmed SH. Habit, choice, and addiction. Neuropsychopharmacology 2021;46:689–98.
Hogarth L. Addiction is driven by excessive goal-directed drug choice under negative affect: translational critique of habit and compulsion theory. Neuropsychopharmacology 2020;45:720–35.
Hill AJ. The psychology of food craving. Proc Nutr Soc. 2007;66:277–85.
Kleykamp BA, Weiss RD, Strain EC. Time to reconsider the role of craving in opioid use disorder. JAMA Psychiatry. 2019;76:1113–14.
McHugh RK, Votaw VR, Sugarman DE, Greenfield SF. Sex and gender differences in substance use disorders. Clin Psychol Rev. 2018;66:12–23.
Kennedy AP, Epstein DH, Phillips KA, Preston KL. Sex differences in cocaine/heroin users: drug-use triggers and craving in daily life. Drug Alcohol Depend. 2013;132:29–37.
Acknowledgements
We would like to thank Adelya Urmanche, Lewis Leone, and Andrea Bell for help with data collection, David Lydon-Staley, and the Rutgers University Biostatics & Epidemiology Services (RUBIES) for statistical consulting, and all the patients and staff at the Bellevue Hospital Outpatient Treatment Program.
Funding
This work was supported by grants from the Brain & Behavior Research Foundation (Grant #25387 to A.B.K.), the National Institute on Drug Abuse (R01DA043676 to P.W.G. and J.R. and F32DA039648, R01DA053282, and R01DA054201 to A.B.K.), and the U.S. Fulbright Commission and the Colombian government (to S.L-G.).
Author information
Authors and Affiliations
Contributions
ABK and SLG designed the experiment with support from PWG and JR. JM and NVB collected the data. KB and ABK analyzed the data and wrote the first draft of the paper. All authors provided comments on the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biernacki, K., Lopez-Guzman, S., Messinger, J.C. et al. A neuroeconomic signature of opioid craving: How fluctuations in craving bias drug-related and nondrug-related value. Neuropsychopharmacol. 47, 1440–1448 (2022). https://doi.org/10.1038/s41386-021-01248-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-021-01248-3