Abstract
It has been demonstrated that opioid agonists that preferentially act at μ-opioid receptors to activate G protein signaling over βarrestin2 recruitment produce antinociception with less respiratory suppression. However, most of the adverse effects associated with opioid therapeutics are realized after extended dosing. Therefore, we tested the onset of tolerance and dependence, and assessed for neurochemical changes associated with prolonged treatment with the biased agonist SR-17018. When chronically administered to mice, SR-17018 does not lead to hot plate antinociceptive tolerance, receptor desensitization in periaqueductal gray, nor a super-sensitization of adenylyl cyclase in the striatum, which are hallmarks of opioid neuronal adaptations that are seen with morphine. Interestingly, substitution with SR-17018 in morphine-tolerant mice restores morphine potency and efficacy, whereas the onset of opioid withdrawal is prevented. This is in contrast to buprenorphine, which can suppress withdrawal, but produces and maintains morphine antinociceptive tolerance. Biased agonists of this nature may therefore be useful for the treatment of opioid dependence while restoring opioid antinociceptive sensitivity.
Similar content being viewed by others
Introduction
There have been considerable efforts made toward developing safer μ-opioid receptor (MOR) agonists for the treatment of pain for over a century. In recent years, the concept of biased agonism, or functional selectivity, has emerged as a possible approach for refining pharmacological manipulation of this analgesic target. Biased agonism is a comparative term that refers to an agonist’s ability to preferentially signal in one pathway over another pathway relative to how a fully efficacious reference compound performs in both assays [1]. When the MOR, a G protein-coupled receptor, is activated by analgesics such as morphine, it interacts with multiple effectors, including heterotrimeric G proteins and scaffolding proteins, such as βarrestins [2, 3]. Interactions with these proximal effectors represent a pinnacle point at which MOR signaling divergence may originate. As such, assays determining agonism in these pathways are frequently explored to assess MOR signaling bias. MOR agonists that activate G protein signaling pathways to a greater extent than βarrestin2 recruitment in cellular assays have been shown to relieve pain with minimal respiratory suppression in mice [4,5,6].
There is evidence that βarrestin2 regulates the MOR in vivo, as βarrestin2 knockout (βarr2-KO) mice exhibit enhanced morphine antinociception and are resistant to developing morphine tolerance in a hot plate assay [7,8,9,10]. However, these mice do display morphine tolerance in a warm water tail immersion assay, suggesting that the regulation of the receptor is dynamic and may be neuronal population specific [11]. βarr2-KO mice display equivalent naloxone-precipitated withdrawal compared with wild-type mice when high doses of morphine are administered over time. However, when the dose of morphine is reduced over time, the display of withdrawal was less severe in the βarr2-KO mice [8, 9]. In addition to seeing benefits in alleviating pain and preventing severe withdrawal, βarr2-KO mice are protected from the respiratory suppression induced by morphine [12].
Together, these data support a role of βarrestin2 in the regulation of MOR in vivo; the extent to which this regulation is directly due to MOR-βarrestin2 interactions remains to be determined. Towards this question, agonists have been developed that promote MOR-G protein signaling while disfavoring βarrestin2 recruitment to the receptor. The first clinical compound developed, based on this principle, is oliceridine (TRV-130, Olinva®). Oliceridine was shown to have antinociceptive properties at doses that did not induce respiratory suppression in rodents [4]. However, in clinical studies, this benefit dissipates as the dosage increases, suggesting a more narrow therapeutic window than anticipated [13].
Recently, our laboratory developed a series of small molecule agonists that activate MOR-mediated G protein signaling to a similar degree as the enkephalin analog, DAMGO, but show a wide separation in potency for promoting recruitment of βarrestin2 to the receptor [6]. In this series, several compounds were compared, spanning a spectrum of biased agonism, in hope that improving the degree of bias beyond that obtained for oliceridine could improve the therapeutic window. In vivo, these compounds (the “SR series”) produce antinociception at doses consistent with their potency in the guanosine 5'-O-[gamma-thio]triphosphate (GTPγS) binding assay; however, their propensity to produce respiratory suppression directly correlates with their degree of bias (separation between GTPγS binding and βarrestin2 recruitment preference). The most biased compounds, although present at saturating levels in the brain, produced no significant respiratory suppression at doses sixfold higher than the antinociceptive ED50 in the hot plate assay, suggesting that this may be a viable strategy for improving opioid agonist safety. Questions remain regarding the impact of the chronic use of these compounds on the development of tolerance and physical dependence.
In this study, we investigate the impact of extended exposure to SR-17018, morphine, oxycodone, and buprenorphine. Parallel molecular pharmacology studies, focusing on G protein signaling in brain samples taken from the chronically treated mice, provide mechanistic insight into how SR-17018 differently effects receptor function relative to morphine. The interplay between SR-17018 or buprenorphine following chronic morphine administration is investigated as a paradigm of opioid substitution therapy.
Materials and methods
Compounds
SR-17018 was prepared as a mesylate salt in house and all dosing preparations reflect the base weight. Morphine sulfate pentahydrate (referred to as morphine) was from the NIDA Drug Supply Program and Sigma, and prepared according to the salt weight (as this makes the concentrations comparable to most published studies). Oxycodone HCl and buprenorphine HCl were from Sigma and were prepared according to salt weight. Compounds synthesized for this study were validated by nuclear magnetic resonance spectroscopy and purity was >95%. For all in vivo studies, the vehicle used is (1:1:8 dimethylsulfoxide (DMSO):Tween-80:sterile water) unless saline is indicated as for morphine. For chronic administration, morphine was dissolved in saline before loading into osmotic minipumps (o.m.p.). SR-17018, buprenorphine, and oxycodone were administered twice daily via oral gavage dissolved in vehicle (b.i.d. (half of the daily dose, every 12 h), p.o.) for chronic treatment studies. At the end of repeated dosing studies, all compounds were dissolved in vehicle and injected intraperitoneally, either as a single challenge dose or in a cumulative dosing procedure as indicated.
Animals
A total of 222 male and 16 female C57BL6 mice were used to complete these studies. Approximately 70% of mice used were acquired from Jackson Labs and the remaining 30% were bred in the lab vivarium space. Each individual experimental cohort contained both Jackson and Scripps Research-generated mice to control for effects of breeder source. All mice used were 10–20 weeks of age at the time of testing and were single housed prior to minipump implantation or twice daily oral gavage. In acute studies, mice were group housed prior to beginning the experiment. Mice were kept on 12 h light–dark cycle and had ad libitum access to standard rodent chow and water throughout testing procedures. Male and female mice were used separately and data are presented separately. In all biochemistry studies, an n = 1 represents tissue from one mouse. All mice were used in accordance with the National Institutes of Health Guidelines for the Care and Use of Laboratory Animals with the approval by The Scripps Research Institute Animal Care and Use Committee.
Blinding
For acute animal studies, individual aliquots of 50 μL of each compound prepared in DMSO at ten times the final concentration were dispensed into Eppendorf tubes by the experimenter. These tubes were given to another individual and treatment groups were randomized, and tubes individually labeled according to a key. The behavioral assay was then performed by the experimenter, and at the end of the study the key given to them.
To blind the experimenter in studies that used o.m.p., a second individual loaded the pumps and performed the surgeries. All postsurgical monitoring was done by the second individual such that the experimenter had no knowledge of treatment groups (compound or saline). This was done to ensure any common behaviors or physiological consequences associated with MOR agonists (e.g., hyperlocomotion, weight loss, Straub tail) could not be observed by the experimenter prior to the day of testing. In the dependence studies, where minipumps were explanted, compounds or vehicle were dispensed into Eppendorf tubes daily (as outlined above) by an individual not participating in observation of somatic signs of withdrawal or measurement of antinociception.
Blinding for p.o. dosing studies was performed similarly to acute blinding procedures, except that 8 ml injection top glass vials with 10× drug concentrations in DMSO were prepared each day, in the morning, for both AM and PM injections. In some cases, evening injections were performed by the eventual experimenter, although this was avoided when possible, and he or she remained blinded to treatment throughout dosing.
Osmotic minipump implantation in mice
Osmotic minipumps (Model 2001, 200 μL reservoir, 1 μL/h flow rate) were purchased from ALZET and implanted as described previously [9]. Prior to implantation, all mice were weighed and the concentration of morphine in 0.9% saline in each pump was normalized relative to the weight of the individual mouse (23–32 g at the time of surgery). No mouse weighing >32 g was included in these studies to stay beneath the limit of the solubility of morphine in 0.9% saline (morphine limit is 64 mg/mL). At 16–20 h prior to scheduled implantation, minipumps were filled with either saline or morphine adjusted to mouse body weight, to deliver 24 or 48 mg/kg/day, and primed overnight in 15 ml Falcon tubes, submerged in 4–5 ml of 0.9% saline at 37 °C. To implant the minipumps subcutaneously, anesthesia was induced via isoflurane inhalation. A small incision was made with surgical scissors above the shoulders. The pump was inserted with the opening facing the posterior of the mouse and the wound closed with one to two wound clips. Weight of the mouse and status of the surgical site was monitored daily until testing. For studies requiring the removal of the minipump, mice were anesthetized with isoflurane, the minipump was removed, and the wound was again closed with the clips.
Notes on compound solubility
SR-17018 is soluble up to a concentration of ~2.5 mg/mL when made in DMSO, Tween-80, and water (1:1:8 with DMSO first, then Tween-80, then water). We have found that efforts to improve solubility may work in solution, but upon repeated injections, the compound precipitates at the injection site. This especially proved true in pilot studies where, on the third day of daily i.p. or subcutaneous (s.c.) dosing, plasma levels dropped dramatically. Gross dissections revealed precipitation of compound at in the injection sites (s.c. or i.p.). We do not use higher concentrations of DMSO in i.p. or s.c. injections, as it can be dehydrating and have adverse effects on the mice. To use the o.m.p. (as described for morphine), concentrations would have to exceed 3 mg/mL, which exceeds the solubility of SR-17018 in 1:1:8 DMSO, Tween-80, water vehicle. Therefore, we tried to use a different vehicle to administer 12 mg/kg/day SR-17018 in 50% DMSO, 25% cremaphor, and 25% water; however, the plasma delivery ranged from19 to 38 ng/mL over 7 days (n = 3 mice), indicating that SR-17018 was not circulating at high levels. Similar results were obtained with using glycerol as a vehicle in the pumps (plasma levels between 16 and 46 ng/mL). Inspections of the pumps after 7 days revealed a precipitation encasing the pumps. For these reasons, we opted to move to oral delivery of SR-17018.
Twice daily dosing via gavage in mice with SR-17018 or oxycodone
To match housing conditions with mice implanted with minipumps, mice used for gavage experiments were single housed in home cages. After 1–2 days of acclimation, twice daily dosing began, with each injection spaced every 12 h for 6 days. Mice were dosed via oral gavage using flexible plastic feeding tubes mounted on the end of a 1 mL syringe at a volume of 10 μL/g of body weight. SR-17018 was dosed relative to the dose weight (24 or 48 mg/kg/day), whereas oxycodone was dosed relative to the salt weight (24 mg/kg/day). The doses administered per day were chosen to be approximately two to three times or four to six times the acute ED50 values determined from previous hot plate studies (separate groups per dose, i.p., ED50 calculated at 1 h post injection, [6]). After the addition of Tween-80, the solutions were vortexed until homogeneous, water added, then vortexed again. Solutions were prepared fresh in the morning in a single volume of the highest needed concentration and 10× DMSO stocks were distributed and diluted as needed among glass, injection top, 8 mL vials for both morning and evening injections.
Pharmacokinetic determination of morphine levels after minipump implantation
Following pump priming and implantation, mice were allowed to recover for 6 h. Blood samples were collected in EDTA-coated CapiJect tubes via cheek bleed, up to 150 μl, at which point bleeding was stopped via application of pressure with gauze. The blood samples were centrifuged at 12,000 × g to separate plasma and blood cells, and plasma was collected and frozen at −80 °C until quantification. On days 3 and 5, blood samples were again collected via cheek bleed. Sample collection was staggered such that blood was collected no more than twice from an individual mouse. On day 7, all mice were euthanized under isoflurane anesthesia, with trunk blood (plasma separated) and whole brain collected. As on day 1, all samples were preserved at −80 °C until quantification. Compound concentrations in the brain and plasma were evaluated using liquid chromatography (Shimadzu)–tandem mass spectrometry (AB Sciex) operated in a positive-ion mode using multiple reaction monitoring methods [6].
Pharmacokinetic determination of SR-17018 levels acutely during acute or twice daily oral dosing
To assess levels of SR-17018 throughout the chronic dosing paradigm, mice were orally treated with SR-17018 acutely (24 mg/kg, base weight) or chronically (48 mg/kg/day, or 24 mg/kg, b.i.d., p.o., in 1:1:8 DMSO:Tween-80:sterile water) for six days. Acutely, SR-17018 was delivered orally via gavage and 10 μL of blood samples were collected from the tail vein between 0.5 and 24 h. On days 1, 3, and 5, blood samples were collected via tail vein using 10 μL capillary tubes at 2 and 6 h after the morning injection, as well as immediately prior to the evening injection, or ~11.75 h after the morning injection. On the morning of the seventh day, ~15 h after the final injection mice were killed under isoflurane anesthesia, and trunk blood and whole brain collected. All blood samples were centrifuged at 12,000 × g and the plasma fraction collected and stored at −80 °C until quantification. Levels were determined in the same manner as for the morphine pump group. Oxycodone and its metabolites were measured in a similar manner following a single 12 mg/kg, p.o., dose at the times indicated up to 12 h.
Antinociception by hot plate test
For the hot plate assay, the assay was performed as previously described [6]. Mice were placed in a Plexiglass chamber (16” tall, 8” in diameter) on a ceramic plate heated to 52 °C and the timer started (Columbus Instruments). Paw licking, paw flicking, rapid stepping, and jumping were coded as positive responses, upon which the timer was stopped or up to a maximum of 20 s. Baseline measures were recorded in naive mice upon initial exposure to the hot plate (52 °C) and the latency to respond was recorded in seconds. A ceiling response latency was imposed at 20 s to avoid paw damage. In all studies, a tail flick response latency (49 °C) was recorded prior to assessing hot plate responses (data not presented here). Prior to analysis, raw antinociception data from hot plate measures were converted to percent maximal effect (%MPE) for each mouse to account for individual differences in baseline measures within the assay. The maximum effect ceiling was limited to 20 s. %MPE was calculated as: 100 × (test latency seconds − baseline latency seconds)/(20 s − baseline latency seconds).
Cumulative dosing procedure to assess tolerance to antinociception of MOR agonists
Mice were dosed cumulatively with morphine (6–48 mg/kg, i.p., salt weight) or SR-17018 (6–48 mg/kg, i.p., base weight) after the chronic treatments described above [9]. Immediately after recording baseline responses, mice were injected with the first dose. After 1 h, mice were again tested and injected with the next highest dose as indicated. For both morphine and SR-17018, doses were administered in the following order: 6, 6, 12, and 24 mg/kg, to yield cumulative doses of 6, 12, 24, and 48 mg/kg. For oxycodone, injections were 1, 2, 3, 6, and 12 mg/kg for cumulative doses of 1, 3, 6, 12, and 24 mg/kg. In all cases, the experimenter was blinded to chronic treatment.
ED50 values with 95% confidence limits were generated by nonlinear regression analysis with the top constrained to 100% and the bottom constrained to 0% as the data were normalized to baseline and the 20 s cutoff in the hot plate test. To facilitate comparisons, potency ratios were generated to compare shifts in potency relative to chronic saline or vehicle conditions. A shift in potency was considered significant if the confidence limits did not include 1. For reversal of morphine tolerance studies, all comparisons were made to morphine response curves obtained in saline-pump-implanted mice, followed by pump explant and 3 days of twice daily vehicle dosing. There was no statistical significant difference in morphine potency between mice treated with 6 days of 0.9% saline (ED50 (95% confidence interval (CI)) = 7.8 (6.1 to 9.4)) vs. mice treated for 6 days with 0.9% saline followed by explant and 3 days of vehicle (ED50 (95% CI) = 8.7 (7.5 to 10.1)) (Table 1), demonstrating no effect of prior treatment upon morphine potency under these conditions.
Tolerance reversal (daily)
Hot plate responses were measured once daily at 1, 24, and 48 h post minipump explant, 1 h after daily gavage (baseline measures were taken prior to start of chronic dosing) of SR-17018 (24 mg/kg, p.o.), buprenorphine (1 mg/kg, p.o.), or vehicle as indicated. Seventy-two hours after explant, prior to cumulative dosing, baseline measures were again assessed. This measure served as the baseline for each mouse in the subsequent cumulative dosing studies.
Assessment of somatic signs of opioid withdrawal
Following 6 days of SR-17018 (48 mg/kg/day b.i.d. p.o.), mice were assessed for somatic signs of withdrawal starting at 3 h after the final p.o. dose of 24 mg/kg. For morphine, mice were implanted with subcutaneous minipumps containing a concentration equivalent to 48 mg/kg/day, relative to the individual mouse’s weight. At 144 h after implantation, mice were again anesthetized with isoflurane and the minipump removed. In all groups, vehicle was administered (1:1:8 DMSO:Tween-80:water) by gavage every 12 h, except in cases where SR-17018 or buprenorphine was administered (in the same vehicle). Following minipump explant, mice were observed in 30 min periods at 1, 3, 5, 7, 11, 23.5, 47.5, and 71.5 h from the time the pump was removed. In a separate cohort, 30 min periods were observed at 1, 3, 25, 27, 49, 51, 73, and 75 h to assess the effect on ongoing administration of SR-17018. During each 30 min observation period, the number of paw tremors, wet dog shakes, and jumps were counted. Mastication was coded as absent (0) or present (1), and stools coded as solid (0), soft (1), or diarrhea (2). The global withdrawal scores were calculated as previously described [8, 9, 14] with the following weighting formula: [paw tremor × 0.35) + (wet dog shakes × 1) + (jumps × 0.8) + (diarrhea × 1.5) + (mastication × 1.5) = global withdrawal score]. All dosing and scoring of animals involved several individuals, blinded to dose and drug as described above.
Dissection of periaqueductal gray and striatum
Mice were euthanized via cervical dislocation. The brain was then removed and placed on filter paper wetted with phosphate-buffered saline atop a metal block placed in crushed ice. A coronal cut was made with a razor blade immediately rostral to the cerebellum, to expose the periaqueductal gray (PAG), and an additional cut made ~1 mm rostral to the first cut. The slice was placed on wetted filter paper and the area immediately surrounding the aqueduct was trimmed to leave a square with sides of ~1.5 mm. The remaining brain tissue rostral to the PAG was bisected with a razor between the two cortices. For each half, the cortex and midbrain were separated via blunt dissection to reveal the hippocampus, which was removed. The underlying striatum was cut away from the remaining tissue and any remaining cortex removed from the sample. Immediately following dissection, both PAG and striata were immediately placed in a conical tube and snap frozen in liquid nitrogen. Between each dissection, the filter paper was discarded to prevent cross-contamination and samples were stored at −80 °C prior to use in biochemical assays.
35S-GTPγS binding in PAG membranes
Frozen PAG were dissociated by glass-on-glass dounce homogenization on ice in homogenization buffer (50 mM Tris pH 7.4, 3 mM MgCl2, 1 mM EDTA) and centrifuged for 30 min at 20,000 × g. The supernatant was discarded and the pellet re-suspended two times. Membranes were re-suspended in assay buffer (50 mM Tris pH 7.4, 100 mM NaCl, 3 mM MgCl2, 0.2 mM EDTA, 10 µM GDP) and 0.1 nM 35S-GTPγS (1250 Ci/mmol), and plated at 2.5 µg/well in 96-well plates and incubated at room temperature for 30 min before rapid filtration through GF/B fiberglass filter plates on a 96-well Brandel cell harvester as described above for CHO-MOR membranes. To convert data to fold over basal for PAG studies, all data points were divided by the average counts measured in the absence of drug stimulation (basal). In all cases, assays were performed in duplicate or triplicate, and technical replicates were averaged into a single data point before combining assays between days to generate means with error. EC50 and Emax values were determined via nonlinear regression in GraphPad Prism software. Individual Emax values derived from the nonlinear regression from each PAG were averaged and presented with calculated 95% confidence limits for statistical comparison.
Radioligand binding in brainstem membranes
Assays were performed as previously described [6]. Briefly, brainstem was homogenized on ice by rotator tissue homogenization in buffer (10 mM Tris HCl pH 7.4, 100 mM NaCl, 1 mM EDTA); membranes were pelleted by centrifugation at 4 °C at 20,000 × g for 30 min. The supernatant was discarded, the pellet re-suspended by glass-on-glass dounce homogenization in buffer, pelleted via centrifugation as described above, and the supernatant discarded. The pellet was re-suspended in binding buffer (10 mM Tris HCl, pH 7.4) and plated at 20 µg/well protein. For 3H-DAMGO, concentration was determined based on radioactivity counts. Specific binding was determined by subtracting nonspecific binding (determined with 1 μM DAMGO) from total binding (4 nM 3H-DAMGO (53.7 Ci/mmol). Radioactivity was counted with Microscint on a TopCount NXT Scintillation Counter (PerkinElmer).
Assessment of forskolin-stimulated cyclic AMP production in striatal membranes
Striata were dissected from mice, snap frozen in liquid nitrogen, and stored at −80 °C until use. Both membrane buffer (50 mM HEPES, pH 7.4) and assay buffer (50 mM HEPES pH 7.4, 10 mM MgCl2, 0.2 mM ATP, 2% DMSO, 100 mM NaCl, 100 µM 3-isobutyl-1-methylxanthine, and 30 µM bovine serum albumin) were made fresh on the day of the assay. Samples were thawed on ice in membrane buffer and homogenized by glass-on-glass dounce homogenization. The homogenate was centrifuged at 500 × g for 5 min at 4 °C and the supernatant transferred to a new 1.5 mL Eppendorf tube. This process was repeated two to three times until there was no visible remaining pellet and the recovered supernatant was centrifuged for 10 min at 20,000 × g at 4 °C. The supernatant was discarded and then re-suspended in assay buffer, and protein standardized. For each sample, a protein concentration-effect curve in the absence of forskolin was run to determine basal cAMP levels and to assure that the detection of cAMP would be in the linear range (Supplementary Fig. 4 b). Prepared membranes (100 ng/well) were then stimulated by the indicated concentrations of forskolin for 30 min at room temperature. Levels of cAMP were determined using the homogenous time-resolved fluorescence resonance energy transfer (FRET) cAMP HiRange kit by Cisbio, according to the manufacturer’s instructions (Cisbio-62AM6PEC), using a 60 min incubation with detection reagents. A cAMP standard curve was included in each assay to determine the concentration of cAMP generated as presented. FRET was assessed as described for the cellular studies above.
Software and statistical analysis
In all cases, behavioral and molecular data analysis was performed in GraphPad Prism 7.0 (or higher versions). For pharmacokinetic studies, analysis was performed in WinNonLin software to determine pharmacokinetic parameters. Data are presented as the average of the mean ± SEM, or as mean with 95% confidence limits where indicated. For analysis of global withdrawal scores, a repeated-measures analysis of variance (ANOVA) was applied between drug and vehicle-treated groups followed by a Tukey’s post-hoc analysis. As a pilot study included animals to determine the time for onset of withdrawal at times 3 and 6 h post final dose in the SR-17018-treated cohort, the repeated-measures ANOVA only included the comparison after 12 h, for which there are time-matched repeated measures.
Results
Pharmacokinetic evaluation of chronic SR-17018 and morphine in vivo
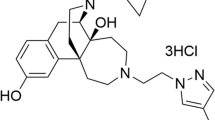
SR-17018 was used for chronic dosing in vivo, as it is equipotent and equi-efficacious to morphine in the mouse brainstem 35S-GTPγS-binding assay and the acute hot plate antinociception test; importantly, neither morphine or SR-17018 produced antinociception in the MOR-KO mice providing evidence that this effect is mediated by MOR [6]. SR-17018 is also highly biased for 35S-GTPγS binding over βarrestin2 recruitment (depending on the assay used, the calculated bias factor is 80–100 relative to DAMGO as per ref. [6]).
To evaluate SR-17018 in a chronic treatment paradigm, we first determined pharmacokinetic parameters for an oral route of dosing. This was necessary, as the poor solubility of the compound led to precipitation upon attempts at systemic repeated dosing or pump implantation. Orally administered SR-17018 is 69% bioavailable, has a half-life of ~6 h and can be detected in the brain at 15 h (Supplementary Fig. 1A) with antinociception comparable to that seen following i.p. dosing (Supplementary Fig. 1B) [6]). We therefore treated mice on a b.i.d. schedule in which a 48 mg/kg/day dose was given in a bolus gavage of 24 mg/kg every 12 h (Supplementary Fig. 1C, for schematic). Pharmacokinetic analysis of plasma levels taken at 2, 6, and 12 h after the gavage on days 1, 3, and 5 demonstrates that steady-sate delivery could be maintained (Fig. 1a). Another cohort of mice was treated with chronic morphine using an o.m.p. for steady-state delivery, as morphine is rapidly metabolized by mice [15]. As shown in Fig. 1, SR-17018 levels were maintained at higher levels than morphine during the course of the administration. At the end of the study, SR-17018 levels in brain were approximately five times that of morphine (Fig. 1a). To serve as a “route of administration” control, we orally administered oxycodone using the same dosing schedule as SR-17018. At 12 mg/kg, p.o., oxycodone and its major metabolites are present in the plasma at much lower concentrations than a SR-17018 dosed at 24 mg/kg, p.o. (Fig. 1b, graphed in comparison from day 1 of Fig. 1a). Under these conditions, we reasoned that SR-17018 should achieve sufficient levels to adequately facilitate MOR adaptations in the brain.
Chronic treatment with SR-17018 does not produce tolerance in the hot plate test, whereas morphine and oxycodone produce robust tolerance. a Pharmacokinetics of chronic morphine (48 mg/kg/day s.c. pump) and SR-17018 (48 mg/kg/day, p.o., b.i.d.) dosing over 147 h (~6 days). The morphine pump was implanted at time 0 and blood was sampled at 6 h after implant and every 48 h subsequently as indicated. SR-17018 (24 mg/kg p.o.) was administered at time 0 and at every 12 h (b.i.d) as indicated by the dotted lines; blood was then drawn at 2, 6, 12 h after each oral dose of SR-17018. Brain levels were measured at 147 h after morphine pump implantation or 15 h after the final dose of SR-17018. Shown are the mean ± SEM of concentrations measured by LC/MS at times indicated; n = 8 mice per group at each sampling. b Plasma levels of oxycodone (12 mg/kg, p.o.) and its metabolites were measured at the indicated time points over 12 h. A single dose of SR-17018 (24 mg/kg, p.o., from a) is shown here for comparison. c Morphine antinociceptive potency in the hot plate test (52 °C) was determined with cumulative dosing of morphine (i.p.) following saline, 24 or 48 mg/kg/day pump infusion over 6 days. d SR-17018 potency was determined by cumulative dosing of SR-17018 (i.p.) after vehicle (1:1:8, DMSO, Tween-80, water), or SR-17018 (24 or 48 mg/kg/day, p.o., b.i.d. every 12 h) for 6 days. e Oxycodone potency was determined by cumulative dosing of oxycodone (i.p.) following vehicle (1:1:8, DMSO, Tween-80, water) or oxycodone (24 mg/kg/day, p.o., b.i.d. every 12 h) for 6 days. Data are presented as the mean ± SEM %MPE; a 20 s cutoff was imposed; n = 8 in each chronic treatment group. Potencies (ED50) are presented in Table 1. f DAMGO-stimulated 35S-GTPγS binding in membranes from periaqueductal gray (PAG) from morphine (n = 9) or saline (n = 6) pump-treated and g SR-17018- (n = 12) or vehicle- (n = 10) treated mice (mean ± SEM). The baselines were not different between the drug- and vehicle-treated control groups (saline pump: 253 ± 29 compared with morphine pump: 250 ± 23 cpm and vehicle: 330 ± 37 compared with SR-17018: 348 ± 67 cpm). h Comparison of the mean EMAX calculated by nonlinear regression analysis shown with 95% CI. Supplementary Fig. 1. A table is included to show Pharmacokinetic parameters for SR-17018 and comparison of PO dosing to IP dosing in the hot plate test. A schematic is included to summarize chronic treatment paradigms for the tolerance and dependence studies. Supplementary Fig. 2 presents the data for females treated with SR-17018 (ED50 values are in the main text Table 1
Antinociceptive tolerance in the hot plate test
Male C57BL/6 mice treated for 6 days with morphine display tolerance as indicated by a twofold or fourfold shift in morphine potency following 24 or 48 mg/kg morphine, respectively, compared with the saline-pump-implanted controls (Fig. 1c and Table 1). SR-17018 produces no tolerance at 24 mg/kg/day, whereas a slight decrease in potency is observed when administered at 48 mg/kg/day (Fig. 1d and Table 1). Female mice, treated in the same manner with SR-17018 at 48 mg/kg/day, do not display tolerance (Supplementary Fig. 2 and Table 1). Mice treated for 6 days with oxycodone 24 mg/kg/day (b.i.d., p.o.) also develop robust tolerance to oxycodone (Fig. 1e and Table 1).
MOR-G protein signaling adaptations following chronic treatment in PAG
In a separate cohort of mice, brains were dissected following chronic treatment and G protein signaling was assessed in membranes from PAG, a center of MOR regulation of pain perception. A significant decrease in DAMGO-stimulated 35S-GTPγS binding was observed in the morphine-treated mice relative to saline-treated mice (Fig. 1f, h), whereas MOR activation was intact in SR-17018-treated mice compared with vehicle-treated mice (Fig. 1g, h). The PAG membranes did not provide sufficient protein to complete the radioligand binding; therefore, brainstem membranes were used to assess receptor binding. There was no change in 3H-DAMGO binding with respect to treatment (saline pump: 43 ± 7; morphine pump: 44 ± 5; vehicle: 42 ± 6; SR-17018: 35 ± 4 fmol/mg protein).
Abstinence-induced withdrawal following chronic opioid exposure
In a separate cohort of mice chronically treated in the same manner, we monitored abstinence-induced withdrawal signs following the morphine (48 mg/kg/day) or saline pump removal, or after the last oral dose of vehicle or SR-17018 (48 mg/kg, p.o., b.i.d.). Signs of abstinence-induced withdrawal were first evident at 1 h after morphine pump removal and were recorded over 3 days at the times indicated (Fig. 2a). For the SR-17018-treated group, no signs of withdrawal were observed at 3 and 6 h after the last 24 mg/kg, p.o. dose of SR-17018, which is consistent with the pharmacokinetic data supporting the presence of SR-17018 at 6 h (Fig. 2b, Fig. 1a, and Supplementary Fig. 1A,B). Withdrawal signs presented at 13 h after the last p.o. dose of SR-17018 and were recorded for 3 days at the time shown (Fig. 2b). A comparison of the sum of the withdrawal signs collected from the first signs of withdrawal over 3 days (from 1 to 72 h for morphine and from 13 to 84 h for SR-17018) to their respective controls demonstrates that chronic treatment with either compound produces significant withdrawal (morphine vs. saline; p < 0.05; SR-17018 vs. vehicle, p < 0.01, two-way ANOVA, Fig. 2a, b). The SR-17018-treated animals return to vehicle control levels by 48 h, whereas the morphine-treated group continue to show signs of withdrawal 3 days after the initial onset of withdrawal as compared with saline-treated mice.
Physical dependence following chronic administration and correlating biochemical signs of adaptation. Mice were treated in the same manner as in Fig. 1 with 48 mg/kg/day morphine or saline delivered by osmotic minipump, s.c., or by 48 mg/kg/day, p.o., b.i.d. dosing with SR-17018 or vehicle for 6 days. a Somatic signs of abstinence-induced withdrawal were recorded for 30 min starting after morphine or saline pump removal, or b following the last oral dose of SR-17018 (24 mg/kg/p.o.) or vehicle. The global signs of withdrawal are presented as the mean ± SEM in each group; both the SR-17018- and morphine-treated groups displayed signs of withdrawal that differed from their respective controls (morphine vs. saline pump, interaction, F(1,16) = 13.31, **p < 0.01; SR-17018 vs. vehicle, interaction, F(1,9) = 20.48, **p < 0.01, two-way repeated-measures ANOVA with Tukey’s multiple comparison test: ^^p < 0.01; ^p < 0.05 for morphine vs. saline; ##p < 0.01 SR-17018 vs. vehicle. The data are shown as the mean ± SEM (n = 4 vehicle or saline; n = 14 morphine; n = 8 SR-17018). c Forskolin-stimulated adenylyl cyclase activity in the striatum as shown by increased accumulation of cAMP. Morphine-treated mice show a significant increase in forskolin-stimulated cAMP production compared with saline pump-treated mice (interaction of forskolin concentration and opioid treatment, F(5,36) = 2.529, p = 0.0463, two-way ANOVA; Sidak multiple comparison test: ^^p < 0.01, ^p < 0.05 morphine vs. saline). SR-17018-treated animals did not differ from their vehicle-treated controls (p > 0.05). Data are shown as the mean ± SEM of n = 4–7 mice. Supplementary Data related to Fig. 2 and Supplementary Fig. 3A. Global and individual withdrawal scores (Supplementary Fig. 3B). Basal cAMP levels are presented as a function of protein to demonstrate that the assay was performed in the linear portion of sensitivity, and that basal levels of cAMP were equal
To determine whether neurochemical adaptations differed following these treatment paradigms, striata were collected at 3 h after morphine pump removal or 15 h after the last dose of SR-17018 from another cohort of mice treated in the same manner to correlate with the peak time of withdrawal responses. Although chronic morphine administration induces the classic overshoot in forskolin-stimulated cAMP accumulation in striatal membranes, SR-17018 does not induce this neurochemical adaptation (Fig. 2c and Supplementary Fig. 3B).
Cross-tolerance and restoration of MOR sensitivity
We then asked whether cross-tolerance would occur between morphine and SR-17018. Chronic morphine treatment produces cross-tolerance to SR-17018 to the same extent that it produces morphine tolerance, suggesting that SR-17018 is accessing the same population of receptors as morphine (Table 1 and Fig. 3a, c). However, chronic SR-17018-treated mice retain sensitivity to morphine (Fig. 3b, c) supporting a lack of SR-17018-induced desensitization of MOR.
Cross-tolerance is induced by morphine but not SR-17018 pretreatment, whereas SR-17018 treatment can reverse morphine tolerance in the hot plate test. a Chronic morphine treatment (24 mg/kg/day, pump, 6 days) leads to a shift in the SR-17018 (i.p.) dose–response curve relative to saline-treated (s.c. pump, 6 days) controls. b Chronic SR-17018 (24 mg/kg/day, p.o., b.i.d., 6 days) has no effect on morphine (i.p.) potency relative to vehicle-treated (p.o., b.i.d., 6 days) controls. a, b Data are the mean ± SEM, n = 6 per group. c The shift in potency relative to controls with 95% CI. d Morphine or saline-pump-treated mice were dosed with SR-17018 (48 mg/kg, p.o., b.i.d.) or vehicle (p.o., b.i.d) for 3 days and the hot plate response was measured 1 h after the dose of 24 mg/kg, p.o.). SR-17018 produced more antinociception than vehicle when compared within the respective chronic treatment group (p = 0.0003, F(6,78) = 4.864, two-way ANOVA, interaction, **p < 0.01, ****p < 0.0001 Tukey’s multiple comparison test). The chronic morphine group showed an improvement in SR-17018 efficacy upon repeated injections of SR-17018 (two-way repeated-measures ANOVA, interaction, p < 0.0001, F(6,86) = 5.355, ^^p < 0.01 vs. the 1 and 24 h time point within treatment group, Tukey’s multiple comparison test). Data are the mean ± SEM, n = 8 saline + SR-17018; 4 saline + vehicle; 11 morphine + vehicle; and 20 morphine + SR-17018. e Morphine- and saline pump-tolerant mice were treated with buprenorphine (2 mg/kg/day p.o., b.i.d.) as described for SR-17018. Buprenorphine (1 mg/kg, p.o.) does not produce significant antinociception compared with the vehicle-treated control in either chronic treatment group nor do the effects differ within treatment group with respect to time (two-way repeated-measures ANOVA, interaction, p = 0.1305, F(6,54) = 1.735). f Morphine (i.p.) potency is restored following 3 days of vehicle (p.o.) or SR-17018 (48 mg/kg/day, p.o., b.i.d.) treatment; however, the mice remain tolerant to morphine following buprenorphine (2 mg/kg/day p.o., b.i.d.). Data are the mean ± SEM, n = 8 saline + SR-17018; 4 saline + vehicle; 11 morphine + vehicle; and 20 morphine + SR-17018. Data are the mean ± SEM, n = 13 morphine + vehicle; 14 morphine + SR-17018; 8 morphine + buprenorphine. g Three days of buprenorphine (2 mg/kg/day, p.o. b.i.d.) administration induces robust morphine cross-tolerance compared with vehicle (p.o., b.i.d.) in mice implanted with the saline pump. Data are the mean ± SEM, n = 4 saline + vehicle; 8 saline + buprenorphine. All ED50 values are presented in Table 1 with 95% CI
As morphine-induced cross-tolerance to SR-17018, we asked whether mice would remain tolerant if dosing of SR-17018 were to continue. Surprisingly, we saw a significant improvement in SR-17018 efficacy upon repeated dosing over 2 days of SR-17018 (p < 0.0001, 48 vs. 24 h and 1 h post explant) (Fig. 3d). In another group of mice we looked at the effect of substituting a low dose of buprenorphine (1 mg/kg, p.o.) in morphine-tolerant mice. At this low dose, buprenorphine produces a weak antinociceptive response in both the morphine- and saline-pump-treated mice. After 2 days of treatment, buprenorphine (2 mg/kg/day, b.i.d., p.o) remains poorly efficacious in both the morphine- and saline-treated mice (Fig. 3e).
Following the third day of substitution dosing, we assessed the potency of morphine and found that the 3-day treatment with SR-17018 restores morphine potency in the morphine-tolerant cohort; however, buprenorphine treatment maintains morphine tolerance in these mice (Fig. 3f and Table 1). Vehicle treatment for 3 days also restores morphine potency similar to SR-17018 treatment (Fig. 3f and Table 1). Further, the low efficacy buprenorphine treatment for 3 days is sufficient to produce morphine cross-tolerance in the saline-pump implanted controls (Fig. 3g and Table 1).
Suppression of abstinence-induced morphine withdrawal
As buprenorphine is largely used for suppressing the signs of withdrawal in opioid-dependent patients [16], we tested whether the daily treatment with SR-17018 would similarly suppress signs of morphine withdrawal in comparison with buprenorphine (Fig. 4a). When administered upon morphine pump removal, both buprenorphine (2 mg/kg/day p.o., b.i.d.) and SR-17018 (48 mg/kg/day p.o., b.i.d) modestly suppress withdrawal signs relative to vehicle treatment over the 3 days observed (p < 0.0001, two-way ANOVA). SR-17018 has a pharmacokinetic half-life of ~6 h following p.o. dosing (Supplementary Fig. 1), which may account for the waning effect seen at 11 h after each dose. Therefore, we repeated the study monitoring withdrawal at 1 and 3 h after the oral dosing of SR-17018 or vehicle, and found that SR-17018 again significantly suppresses morphine withdrawal and retains efficacy over the 3 days administered (Fig. 4b).
Buprenorphine and SR-17018 can suppress withdrawal after cessation of morphine delivery (48 mg/kg/day, 6 days). a Mice were administered vehicle, SR-17018 (24 mg/kg, p.o.), or buprenorphine (1 mg/kg, p.o.) upon removal of the morphine pump and the signs of withdrawal were scored at 1, 3, 5, 7, and 11 h for 30 min. The same doses were continued every 12 h and the signs of withdrawal were monitored for 30 min at 23.5, 47.5, and 71.5 h. SR-17018 and buprenorphine suppressed the signs of withdrawal relative to vehicle for over time (p = 0.0002, interaction of time and treatment, two-way repeated-measures ANOVA, F(14,231) = 3.01, *p < 0.05 SR-17018 vs. vehicle, Sidak post-hoc test). b The study design is the same as in a, except withdrawal signs were scored at 1 and 3 h after each oral dose of vehicle or SR-17018 (24 mg/kg, p.o.) given every 12 h. SR-17018 significantly suppressed the signs of withdrawal compared with vehicle (p = 0.0387, interaction of time and treatment, two-way ANOVA, F(7,70) = 2.266, **p < 0.01 Sidak post-hoc test). Supplementary Data related to Fig. 4 and Supplementary Fig. 4: Individual withdrawal scores used to calculate the global withdrawal scores per day shown at all times collected
Discussion
In this study, we show that SR-17018, a compound that shows a strong preference for G protein signaling over βarrestin2 recruitment in cellular assays, produces less tolerance than morphine or oxycodone upon chronic administration in the mouse hot plate test. Moreover, we show that unlike morphine, chronic treatment with SR-17018 does not induce MOR desensitization in PAG or cyclase sensitization striatum following chronic treatment. Most interestingly, substitution of SR-17018 in morphine-tolerant mice restores morphine sensitivity within 3 days, in a manner similar to eliminating morphine, but can do so while suppressing the onset of withdrawal.
Substitution of one opioid for another has been a therapeutic approach for counteracting opioid tolerance and intolerable side effects for chronic pain patients; however, continued use of the replacement drug can promote subsequent tolerance, introducing the need to rotate to yet another agonist [17]. Morphine produces robust, dose-dependent tolerance, as well as cross-tolerance to SR-17018, suggesting that SR-17018 accesses the same pool of morphine-desensitized receptors to promote antinociception. Upon substitution of SR-17018 in morphine-tolerant mice, the efficacy of SR-17018 improves over 2 days of treatment. After 3 days of treatment, morphine potency is fully restored in these animals. Buprenorphine, which is clinically used in rotation therapy in humans, does not restore morphine potency in the tolerant mice. Rather, this 3-day dosing regimen of buprenorphine is sufficient to induce robust morphine cross-tolerance in the saline-pump-treated group. In this manner, SR-17018 is notably different from buprenorphine.
It is worth noting that treatment with vehicle for 3 days is sufficient to reverse morphine tolerance in the mice; however, without an opioid present, withdrawal symptoms persist during the 3-day period. Both buprenorphine and SR-17018 are effective at suppressing the signs of withdrawal during this treatment period, although buprenorphine substitution retains morphine cross-tolerance. Therefore, substitution with a compound such as SR-17018 may provide an opportunity to suppress withdrawal and restore morphine sensitivity simultaneously. Given that compounds chemically related to SR-17018 carry little threat of respiratory suppression [6], they may provide a safer approach to treating opioid dependence and maintaining pain therapeutic efficacy. This profile may meet an important clinical need, as patients maintained on buprenorphine to prevent withdrawal can experience tolerance to conventional opioid pain therapies [18] and report adverse effects of maintenance therapy [19]. It remains to be seen whether the return of morphine sensitivity observed in the pain pathways will manifest in other systems that adapt to chronic opioid exposure, such as the tolerance that develops to respiratory suppression and constipation or the adaptations that underlie drug-seeking and addiction.
It is somewhat surprising that a compound that would produce G protein signaling would not induce profound desensitization and downregulation of the MOR. However, in brainstem the number of receptors detected by radioligand binding does not change as a function of SR-17018 or morphine treatment. Studies in the βarr2-KO mice suggest that the desensitization of MOR in PAG following chronic morphine requires βarrestin2; however, the adaptive mechanisms in the striatum are less clear as forskolin induces a robust cAMP overshoot in both the wildtype and βarr2-KO mouse striatal membranes [8]. With lower doses of morphine, βarr2-KO mice showed less signs of withdrawal; however, cAMP levels were not measured in these animals [9]. Given that the SR-17018-treated animals (at 48 mg/kg/day, b.i.d.) still show signs of withdrawal, our findings, together with the observations made in the βarr2-KO mice, suggest that βarrestins may play a role in the onset or the severity of physical dependence but that this strategy may not eliminate the development of withdrawal signs following drug cessation.
SR-17018 is unusual for its ability to effectively suppress the signs of withdrawal, while restoring morphine responsiveness in the hot plate assay, which is in stark contrast to replacing morphine with buprenorphine. Taken together with the previously reported cellular studies, these data suggest that an agonist that can activate MOR-induced GTPγS binding in cell lines and in mouse brain with very little potency for stimulating recruitment of βarrestin2 [6] produces less antinociceptive tolerance in the hot plate test, and does not lead to MOR desensitization in PAG or enhanced forskolin sensitivity in striatum. We speculate that perhaps this compound may be able to stabilize the MOR in a manner that restores G protein signaling and may serve as a way to reinstate efficacy in a tolerant system, while preventing withdrawal when present. These findings are in agreement with evidence that the MOR is negatively regulated by βarrestin2 in processes governing hot plate nociceptive responses in the mouse. If an agonist can promote resensitization of a receptor, in this case by shifting from a βarrestin-desensitized state to a G protein-signaling state, it could be a means to restore function of the receptor. Further studies are forthcoming, investigating their efficacy across additional pain assays. We propose that SR-17018 has the characteristics of performing as a stabilizing agonist at MOR whereupon chronic treatment stabilizes a G protein coupling state and may represent a means to restore MOR responsiveness and analgesic efficacy in the opioid-dependent state, while lessening the severity of opiate withdrawal.
Funding and disclosure
The Scripps Research Institute has filed a patent application on the SR-17018 compound used herein (LMB, CLS, and TDB). The authors declare no competing interests.
References
Pasternak GW. Mu opioid pharmacology: 40 years to the promised land. Adv Pharmacol 2018;82:261–91.
Smith JS, Lefkowitz RJ, Rajagopal S. Biased signalling: from simple switches to allosteric microprocessors. Nat Rev Drug Discov 2018;17:243–60.
Gainetdinov RR, Premont RT, Bohn LM, Lefkowitz RJ, Caron MG. Desensitization of G protein-coupled receptors and neuronal functions. Annu Rev Neurosci 2004;27:107–44.
DeWire SM, Yamashita DS, Rominger DH, Liu G, Cowan CL, Graczyk TM, et al. A G protein-biased ligand at the mu-opioid receptor is potently analgesic with reduced gastrointestinal and respiratory dysfunction compared with morphine. J Pharm Exp Ther 2013;344:708–17.
Manglik A, Lin H, Aryal DK, McCorvy JD, Dengler D, Corder G, et al. Structure-based discovery of opioid analgesics with reduced side effects. Nature 2016;537:185–90.
Schmid CL, Kennedy NM, Ross NC, Lovell KM, Yue Z, Morgenweck J, et al. Bias factor and therapeutic window correlate to predict safer opioid analgesics. Cell 2017;171:1165–75 e13.
Bohn LM, Lefkowitz RJ, Gainetdinov RR, Peppel K, Caron MG, Lin FT. Enhanced morphine analgesia in mice lacking beta-arrestin 2. Science 1999;286:2495–8.
Bohn LM, Gainetdinov RR, Lin FT, Lefkowitz RJ, Caron MG. Mu-opioid receptor desensitization by beta-arrestin-2 determines morphine tolerance but not dependence. Nature 2000;408:720–3.
Raehal KM, Bohn LM. The role of beta-arrestin2 in the severity of antinociceptive tolerance and physical dependence induced by different opioid pain therapeutics. Neuropharmacology 2011;60:58–65.
Raehal KM, Schmid CL, Groer CE, Bohn LM. Functional selectivity at the mu-opioid receptor: implications for understanding opioid analgesia and tolerance. Pharm Rev 2011;63:1001–19.
Bohn LM, Lefkowitz RJ, Caron MG. Differential mechanisms of morphine antinociceptive tolerance revealed in (beta)arrestin-2 knock-out mice. J Neurosci 2002;22:10494–500.
Raehal KM, Walker JK, Bohn LM. Morphine side effects in beta-arrestin 2 knockout mice. J Pharm Exp Ther. 2005;314:1195–201.
Viscusi ER, Skobieranda F, Soergel DG, Cook E, Burt DA, Singla N. APOLLO-1: a randomized placebo and active-controlled phase III study investigating oliceridine (TRV130), a G protein-biased ligand at the micro-opioid receptor, for management of moderate-to-severe acute pain following bunionectomy. J Pain Res 2019;12:927–43.
Schulteis G, Markou A, Gold LH, Stinus L, Koob GF. Relative sensitivity to naloxone of multiple indices of opiate withdrawal: a quantitative dose-response analysis. J Pharm Exp Ther 1994;271:1391–8.
Handal M, Grung M, Skurtveit S, Ripel A, Morland J. Pharmacokinetic differences of morphine and morphine-glucuronides are reflected in locomotor activity. Pharm Biochem Behav 2002;73:883–92.
Gowing L, Ali R, White JM, Mbewe D. Buprenorphine for managing opioid withdrawal. Cochrane Database Syst Rev 2017;2:CD002025.
Smith HS, Peppin JF. Toward a systematic approach to opioid rotation. J Pain Res 2014;7:589–608.
Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med 2006;144:127–34.
Haber PS, Elsayed M, Espinoza D, Lintzeris N, Veillard AS, Hallinan R. Constipation and other common symptoms reported by women and men in methadone and buprenorphine maintenance treatment. Drug Alcohol Depend 2017;181:132–39.
Acknowledgements
Morphine was provided by the NIDA Drug Supply Program. We thank Ms. Nina McFague for additional assistance in blinded dosing and observations in the behavioral studies.
Author information
Authors and Affiliations
Contributions
TWG designed, performed, and analyzed the behavioral studies, and contributed to writing and editing. CLS designed, performed, and analyzed behavioral studies, and pilot brain signaling assays. ELS designed, performed, and analyzed biochemical studies in brain regions, and contributed to editing. FP and AAC blinding, drug preparation, surgeries, dosing, and scoring of the behavioral assays. J-HH performed cAMP studies in striatum, and editing. NMK performed synthesis of SR compounds, data preparation, and editing. MDC performed pharmacokinetic studies and analysis. TDB carried out chemical design and synthesis, funding, and contributed to writing and editing. LMB performed experimental design for cellular and PK, and behavioral studies, analysis, funding, and writing of the manuscript.
Corresponding author
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Grim, T.W., Schmid, C.L., Stahl, E.L. et al. A G protein signaling-biased agonist at the μ-opioid receptor reverses morphine tolerance while preventing morphine withdrawal. Neuropsychopharmacol. 45, 416–425 (2020). https://doi.org/10.1038/s41386-019-0491-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-019-0491-8
This article is cited by
-
Molecular mechanisms of morphine tolerance and dependence; novel insights and future perspectives
Molecular and Cellular Biochemistry (2023)
-
Glutathione ethyl ester reverses the deleterious effects of fentanyl on ventilation and arterial blood-gas chemistry while prolonging fentanyl-induced analgesia
Scientific Reports (2021)
-
Pharmacological and genetic manipulations at the µ-opioid receptor reveal arrestin-3 engagement limits analgesic tolerance and does not exacerbate respiratory depression in mice
Neuropsychopharmacology (2021)
-
Kratom Alkaloids, Natural and Semi-Synthetic, Show Less Physical Dependence and Ameliorate Opioid Withdrawal
Cellular and Molecular Neurobiology (2021)
-
Influence of G protein-biased agonists of μ-opioid receptor on addiction-related behaviors
Pharmacological Reports (2021)