Abstract
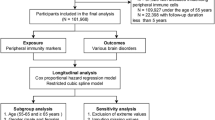
Central immunity components especially microglia in dementia have been well studied and corresponding immunotherapy gradually caught the attention. However, few studies focused on peripheral immunity and dementia. To address the issue, we examined the longitudinal association between incident dementia and peripheral immunity markers encompassing immune cell counts, and their derived ratios including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), systemic immune-inflammation index (SII), and lymphocyte-to-monocyte ratio (LMR), utilizing data of 361,653 participants from the UK Biobank (UKB). During a median follow-up of 8.99 years, 4239 participants developed dementia. The results revealed that increased innate immunity markers were associated with higher dementia risk (per SD increment hazard ratio [HR]; 95% confidence interval [CI] 1.14; 1.09–1.19 for neutrophils, 1.16; 1.11–1.20 for NLR and 1.11; 1.07–1.16 for SII), while increased adaptive immunity markers were associated with lower dementia risk (0.93; 0.90–0.97 for lymphocytes and 0.94; 0.90-0.98 for LMR). Our study pinpoints the differential role of innate and adaptive immunity in dementia incidence, which may provide some new perspectives in etiology and therapy of dementia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Nichols E, Szoeke CEI, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:88–106.
Patterson C. World Alzheimer report 2018. London: Alzheimer’s Disease International. 2018.
Alexander GC, Knopman DS, Emerson SS, Ovbiagele B, Kryscio RJ, Perlmutter JS, et al. Revisiting FDA approval of aducanumab. N Engl J Med. 2021;385:769–71.
Rabinovici GD. Controversy and progress in Alzheimer’s disease — FDA approval of aducanumab. N Engl J Med [Internet]. 2021;385:771–4. https://doi.org/10.1056/NEJMp2111320. Available from
Tisher A, Salardini A. A comprehensive update on treatment of dementia. Semin Neurol. 2019;39:167–78.
Bartels T, De Schepper S, Hong S. Microglia modulate neurodegeneration in Alzheimer’s and Parkinson’s diseases. Science. 2020;370:66–9.
Lall D, Baloh RH. Microglia and C9orf72 in neuroinflammation and ALS and frontotemporal dementia. J Clin Invest. 2017;127:3250–8.
Lewcock JW, Schlepckow K, Di Paolo G, Tahirovic S, Monroe KM, Haass C. Emerging microglia biology defines novel therapeutic approaches for Alzheimer’s disease. Neuron. 2020;108:801–21.
Arranz AM, De Strooper B. The role of astroglia in Alzheimer’s disease: pathophysiology and clinical implications. Lancet Neurol [Internet]. 2019;18:406–14. https://doi.org/10.1016/S1474-4422(18)30490-3. Available from
Butt AM, De La Rocha IC, Rivera A. Oligodendroglial cells in Alzheimer’s disease. Adv Exp Med Biol [Internet]. 2019 [accessed 4 Nov 2021];1175:325–33. https://pubmed.ncbi.nlm.nih.gov/31583593/
Erickson MA, Banks WA. Neuroimmune axes of the blood-brain barriers and blood-brain interfaces: Bases for physiological regulation, disease states, and pharmacological interventions. Pharm Rev. 2018;70:278–314.
Sweeney MD, Sagare AP, Zlokovic BV. Blood-brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol [Internet]. 2018;14:133–50. https://doi.org/10.1038/nrneurol.2017.188. Available from
Wu K-M, Zhang Y-R, Huang Y-Y, Dong Q, Tan L, Yu J-T. The role of the immune system in Alzheimer’s disease. Ageing Res Rev. 2021;70:101409.
Fani L, Ahmad S, Ikram MK, Ghanbari M, Ikram MA. Immunity and amyloid beta, total tau and neurofilament light chain: Findings from a community-based cohort study. Alzheimer’s Dement. 2021;17:446–56.
Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, et al. Innate lymphoid cells: 10 years on. Cell. 2018;174:1054–66.
Vivier E, Raulet DH, Moretta A, Caligiuri MA, Zitvogel L, Lanier LL, et al. Innate or adaptive immunity? The example of natural killer cells. Science (80-). 2011;331:44–9.
Nøst TH, Alcala K, Urbarova I, Byrne KS, Guida F, Sandanger TM, et al. Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol. 2021;36:841–8.
Kara SP, Altunan B, Unal A. Investigation of the peripheral inflammation (neutrophil–lymphocyte ratio) in two neurodegenerative diseases of the central nervous system. Neurol Sci. 2021:1–7. https://doi.org/10.1007/s10072-021-05507-5. Online ahead of print.
Van Der Willik KD, Fani L, Rizopoulos DI, Licher S, Fest J, Schagen SB, et al. Balance between innate versus adaptive immune system and the risk of dementia: a population-based cohort study. J Neuroinflammation. 2019;16:1–9.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open-access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:1–10.
Rembach A, Watt AD, Wilson WJ, Rainey-Smith S, Ellis KA, Rowe CC, et al. An increased neutrophil-lymphocyte ratio in Alzheimer’s disease is a function of age and is weakly correlated with neocortical amyloid accumulation. J Neuroimmunol. 2014;273:65–71.
Kuyumcu ME, Yesil Y, Oztürk ZA, Kizilarslanoǧlu C, Etgül S, Halil M, et al. The evaluation of neutrophil-lymphocyte ratio in Alzheimer’s disease. Dement Geriatr Cogn Disord. 2012;34:69–74.
Kalelioglu T, Yuruyen M, Gultekin G, Yavuzer H, Özturk Y, Kurt M, et al. Neutrophil and platelet to lymphocyte ratios in people with subjective, mild cognitive impairment and early Alzheimer’s disease. Psychogeriatrics. 2017;17:506–8.
Chen SH, Bu XLE, Jin WS, Shen LL, Wang J, Zhuang ZQ, et al. Altered peripheral profile of blood cells in Alzheimer disease. Medicine. 2017;96:1–7.
Cruz Hernández JC, Bracko O, Kersbergen CJ, Muse V, Haft-Javaherian M, Berg M, et al. Neutrophil adhesion in brain capillaries reduces cortical blood flow and impairs memory function in Alzheimer’s disease mouse models. Nat Neurosci. 2019;22:413–20.
Zenaro E, Pietronigro E, Bianca VDella, Piacentino G, Marongiu L, Budui S, et al. Neutrophils promote Alzheimer’s disease-like pathology and cognitive decline via LFA-1 integrin. Nat Med. 2015;21:880–6.
Marsh SE, Abud EM, Lakatos A, Karimzadeh A, Yeung ST, Davtyan H, et al. The adaptive immune system restrains Alzheimer’s disease pathogenesis by modulating microglial function. Proc Natl Acad Sci USA. 2016;113:E1316–25.
Saresella M, Calabrese E, Marventano I, Piancone F, Gatti A, Calvo MG, et al. PD1 negative and PD1 positive CD4+ T regulatory cells in mild cognitive impairment and Alzheimer’s disease. J Alzheimer’s Dis. 2010;21:927–38.
Baruch K, Rosenzweig N, Kertser A, Deczkowska A, Sharif AM, Spinrad A, et al. Breaking immune tolerance by targeting Foxp3+ regulatory T cells mitigates Alzheimer’s disease pathology. Nat Commun. 2015;6:7967.
Späni C, Suter T, Derungs R, Ferretti MT, Welt T, Wirth F, et al. Reduced β-amyloid pathology in an APP transgenic mouse model of Alzheimer’s disease lacking functional B and T cells. Acta Neuropathol Commun [Internet]. 2015;3:71 https://doi.org/10.1186/s40478-015-0251-x. Available from
Dansokho C, Ait Ahmed D, Aid S, Toly-Ndour C, Chaigneau T, Calle V, et al. Regulatory T cells delay disease progression in Alzheimer-like pathology. Brain. 2016;139:1237–51.
Acknowledgements
This study utilized the UK Biobank Resource under application number 19542. We would like to thank all the participants and researchers from the UK Biobank. This study was supported by grants from the National Natural Science Foundation of China (91849126), Shanghai Municipal Science and Technology Major Project (No.2018SHZDZX01) and ZHANGJIANG LAB, Tianqiao and Chrissy Chen Institute, and the State Key Laboratory of Neurobiology and Frontiers Center for Brain Science of Ministry of Education, Fudan University.
Author information
Authors and Affiliations
Contributions
JTY conceptualized the study and revised the manuscript. YRZ, YZL, YNO, and WC analyzed and interpreted the data. SFC, HFW, and SYH prepared all the figures and tables. YRZ, JJW, and SDC drafted and revised the manuscript. JFF and QD critically revised the manuscript. All authors contributed to the writing and revisions of the paper and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, YR., Wang, JJ., Chen, SF. et al. Peripheral immunity is associated with the risk of incident dementia. Mol Psychiatry 27, 1956–1962 (2022). https://doi.org/10.1038/s41380-022-01446-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-022-01446-5
This article is cited by
-
Adaptive immune changes associate with clinical progression of Alzheimer’s disease
Molecular Neurodegeneration (2024)
-
Systemic inflammation indicators and risk of incident arrhythmias in 478,524 individuals: evidence from the UK Biobank cohort
BMC Medicine (2023)
-
Digital oral health biomarkers for early detection of cognitive decline
BMC Public Health (2023)
-
Alzheimer’s disease: targeting the peripheral circulation
Molecular Neurodegeneration (2023)
-
Peripheral immune function and Alzheimer’s disease: a living systematic review and critical appraisal
Molecular Psychiatry (2023)