Abstract
Intravenous leiomyomatosis (IVL) is an unusual uterine smooth muscle proliferation that can be associated with aggressive clinical behavior despite a histologically benign appearance. It has some overlapping molecular characteristics with both uterine leiomyoma and leiomyosarcoma based on limited genetic data. In this study, we assessed the clinical and morphological characteristics of 28 IVL and their correlation with molecular features and protein expression, using array comparative genomic hybridization (aCGH) and Cyclin D1, p16, phosphorylated-Rb, SMARCB1, SOX10, CAIX, SDHB and FH immunohistochemistry. The most common morphologies were cellular (n = 15), usual (n = 11), and vascular (n = 5; including 3 cellular IVL showing both vascular and cellular features). Among the immunohistochemical findings, the most striking was that all IVL showed differential expression of either p16 or Cyclin D1 in comparison to surrounding nonneoplastic tissue. Cytoplasmic phosphorylated-Rb was present in all but one IVL with hyalinization. SMARCB1, FH, and SDHB were retained; S0X10 and CAIX were not expressed. The most common genetic alterations involved 1p (39%), 22q (36%), 2q (29%), 1q (25%), 13q (21%), and 14q (21%). Hierarchical clustering analysis of recurrent aberrations revealed three molecular groups: Groups 1 (29%) and 2 (18%) with associated del(22q), and Group 3 (18%) with del(10q). The remaining IVL had nonspecific or no alterations by aCGH. Genomic index scores were calculated for all cases and showed no significant difference between the 14 IVL associated with aggressive clinical behavior (extrauterine extension or recurrence) and those without (median scores 5.15 vs 3.5). Among the 5 IVL associated with recurrence, 4 had a vascular morphology and 3 had alterations of 8q. Recurrent chromosome alterations detected herein overlap with those observed in the spectrum of uterine smooth muscle tumors and involve genes implicated in mesenchymal tumors at different sites with distinct morphological features.
Similar content being viewed by others
Introduction
Intravenous leiomyomatosis (IVL) is defined as an intravascular proliferation of benign smooth muscle cells in the absence or outside the confines of a uterine leiomyoma (UL) [1]. In most cases, it represents an incidental finding, but it can be grossly identified. IVL may occasionally grow into extrauterine vessels and rarely reach the right heart through the inferior vena cava leading to increased morbidity and mortality. Overall, the prognosis is generally favorable after surgery, even though recurrences have been reported [2,3,4,5].
The molecular knowledge on uterine smooth muscle neoplasms, particularly for UL and uterine leiomyosarcoma (ULMS), has significantly advanced in light of high throughput technologies over the last decade. t(12;14) with HMGA2-RAD51B fusion and del(7q) are the most common cytogenetic rearrangements in UL [6,7,8,9]. Whole-exome sequencing has revealed MED12 as the most frequently altered gene with mutations seen in ~70% of UL [10], while those without MED12 mutations are reported to have either HMGA2 rearrangements and/or complex chromosomal rearrangements [11,12,13]. MED12 and HMGA2 alterations together are present in 80–90% of UL [14]. Other recurrent chromosome rearrangements involve 6p21 (HMGA1), 1p, 1q (FH), 3q and rarely Xq (COL4A5-COL4A6) [15,16,17,18,19]. On the other hand, ULMS have much more complex alterations, including 1p, 2p, 6p, 9p, 10q, 13q, 14q, and 22q deletions and 8, 10, 12q, 17, X chromosome gains, and aneuploidy in addition to mutations and deletions in RB1, TP53, and PTEN, suggestive of genomic instability [20, 21].
In contrast to UL and ULMS, only three series have been reported to date focusing on the molecular aspects of IVL. In one study, recurrent 22q deletions (66%) and complex copy number alterations were detected using array comparative genomic hybridization (aCGH) [22]. None of these cases showed the most common MED12 mutation described in UL, highlighting the importance of structural chromosome rearrangements in the development of IVL. A second study described recurrent 12q14.3 rearrangements by FISH along with HMGA2 overexpression (58%, n = 12) and the loss of chromosome 22 in two out of three IVL analyzed by karyotyping [23]. Finally, a third study using RNA sequencing (n = 5) detected HOXA13 as a distinctly upregulated gene in UL when compared to IVL or myometrium [24]. These studies suggest that IVL has unique molecular characteristics that partially overlap with both UL and ULMS akin to their intermediate clinical behavior. Herein, we study genome-wide copy number alterations as well as potential correlation with clinical, histological, and immunohistochemical features in a large series of 28 IVL.
Materials and methods
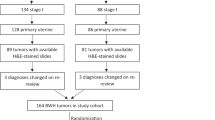
Following institutional IRB approval, 28 IVL from 26 patients (Cases 4 and 24 were recurrences of 3 and 17, respectively) were identified and available H&E slides (median: 1 slide, range: 1–17 slides) were reviewed by four pathologists (ZO, EO, PH and NB). The following microscopic characteristics were evaluated: cellularity (cellular or highly cellular), epithelioid morphology, hydropic change, hyalinization, hyaline plaques, vascularity, and presence of adipose tissue, nuclear atypia, mitotic activity (number per ten high power fields), and infarct-type necrosis. IVL with significantly more cellularity than the adjacent myometrium was described as “cellular”, while those with cellularity similar to that seen in endometrial stromal tumors were further characterized as “highly cellular”. IVL with features similar to those of uterine and extrauterine angioleiomyoma (numerous evenly distributed vasculature (capillary), venous (thick arteriole-like) or cavernous (widened) surrounded by smooth muscle cells) was classified as “vascular” [25, 26]. The vasculature was considered as “usual” type when vessels were variably sized with at least some prominent thick-walled large blood vessels. In addition, tumor vessels were assessed for hyalinization, myxoid change, and thrombi. The extent of morphological features was scored as minimal (<5%), focal (5–24%) or diffuse (>25%). For classification purposes, only when a specific morphology was at least focally present, the tumor was assigned to that category. Clinical and demographic information were retrieved from medical records or pathology reports. Aggressive clinical behavior was defined as the presence of tumor outside the uterus or recurrence.
Immunohistochemistry (IHC) was performed on the Leica Bond automated staining platform with appropriate positive and negative controls stained in parallel. Citrate or EDTA antigen retrievals were done using the Leica Biosystems Refine Detection Kit. The following antibodies were used: phosphorylated-Rb (Cell Signaling Technology, #9308 clone s807/811, 1:100, citrate retrieval, presence of cytoplasmic or nuclear staining), SOX10 (Cell Marque, #CM383A-76 Polyclonal,1:50, citrate retrieval, extent of nuclear staining), SDHB (Abcam, #14714 clone 21A11AE7,1:1000, EDTA retrieval, lack of cytoplasmic staining), p16 (Roche, #725-4713, 1:4, EDTA retrieval), Cyclin D1 (Leica, #PA0046, 1:1, EDTA retrieval, extent of nuclear staining), SMARCB1 (BD Bioscience, #612110, 1:100, EDTA retrieval, lack of nuclear staining), Carbonic Anhydrase IX (CAIX) (Cell Marque, #379R, 1:1, Citrate retrieval, extent of cytoplasmic/membranous staining) and FH (Thermo Scientific, #PA5-22091, EDTA retrieval, lack of cytoplasmic staining). When assessing extent of staining, a semiquantitative scoring method was used: 0 (no staining), 1 (<5%), 2 (5–24%), 3 (25–50%), and 4 (>50%) in IVL and surrounding non-neoplastic tissue (means between the two compared by Student’s t test).
DNA isolation and oligonucleotide aCGH assay were performed as previously described after manual dissection of tumor tissue from 5 μm unstained sections of formalin-fixed paraffin embedded tissue [22]. Briefly, DNA was extracted according to the manufacturer’s instructions using Qiagen tissue kit (Qiagen, Chatsworth, CA). Patient and control DNA labeling, oligonucleotide array hybridization (SurePrint G3 Human CGH 8 × 60 K Oligo Microarray Kit with 62,976 probes of 60-mer oligonucleotide per array; Agilent Technologies), post-hybridization wash, image capture, and extraction of signal feature were performed as previously described [27]. Genome-wide copy number variation was analyzed with a threshold value of 6, a cut-off value of 0.25, and a filter of 6 continuous probes in Agilent CytoGenomics 4.0. All nucleotide positions were designated according to the March 2006 Assembly (NCBI36/hg18) in the University of California Santa Cruz (UCSC) Human Genome browser (http://genome.ucsc.edu/). Genome-wide distribution and relative frequency of the chromosomal abnormalities were resulted from the raw data of copy number alterations in cases. Database of Genomic Variants (http://dgv.tcag.ca/dgv) was used to determine known copy number variants [28]. Cancer related genes in the recurrent copy number aberrations were detected using the Cancer Gene Census (https://cancer.sanger.ac.uk/cosmic/census?tier=all#cl_search) tool [29], including Tier 1 (documented activity in cancer with genomic alterations promoting oncogenic transformation) and tier 2 (recently emerging with strong indications of a role in cancer) genes, as well as literature search. Genomic index was calculated as A2/C (A = total number of alterations, C = number of involved chromosomes) [30,31,32]. Genomic index scores between IVL with aggressive clinical features and those without were compared by Mann–Whitney U test. Unsupervised hierarchical cluster analysis was performed based on the presence of recurrent aberrations within the indicated chromosome band detected in at least four cases (~15%). Of note, aCGH results from three cases (5, 6, and 22) had been previously reported [22].
Results
Clinical data
Twenty-eight IVL from 26 patients with a median age of 45.5 (34–82) years at diagnosis were analyzed. Tumors ranged in size from 0.2 (microscopic) to 17 (median 6) cm. Accompanying UL was noted in 18 IVL. At least 5 years follow-up was available for 23 patients with a median of 13 (up to 25) years. Fourteen IVL (12 patients) were associated with extrauterine extension, and 5 with recurrence (3 patients). In two instances IVL was incompletely resected due to anatomic extent of the tumor (Table 1).
Tumor morphology
The most common morphologies were cellular (n = 15, including 4 highly cellular), usual (n = 11), and vascular (n = 5, including 3 cellular IVL, showing both vascular and cellular features). There were two IVL with adipose tissue and two with epithelioid morphology, all of them cellular (Table 2). Hydropic change was detected in 11 (7 focal), hyalinization in 10 (4 focal), and both in 7 while hyaline plaques were present in 7 IVL (4 minimal, 1 focal) (Fig. 1). Twenty-three IVL had usual vasculature with prominent thick-walled large caliber vessels and cleft like spaces. Vascular IVL (n = 5) included capillary-predominant (n = 2) and arteriole-like (n = 3) vasculature (Fig. 2). Ten IVL had vascular hyalinization, which was focal in six cases. Myxoid change within vessel walls was seen in two cases, one with extensive thrombi, hemorrhage and hemosiderin deposition (Fig. 1). All associated UL available for review (15/18) had overlapping morphology with the accompanying IVL (seven usual, seven cellular including one epithelioid) except for one highly cellular IVL with usual UL (Table 2). Tumors were characterized by bland cytologic features and up to 2 mitoses/10 high power fields.
Note the hyaline plaques (Cases 14, 16, 18, and 24) and hyalinized vessels (Cases 14, 16, 17, and 24), adipose tissue (Cases 14 and 18), and large vessel with thrombosis, myxoid change and hemorrhage (Case 15). All these IVL are cellular except for Case 24, which is extensively hyalinized and cellularity is difficult to assess.
Immunohistochemistry
All IVL showed increased expression of either p16 or Cyclin D1 (mean scores 2.18 and 1.79) in comparison to surrounding nonneoplastic tissue (mean scores 0.58 and 0.88) (p < 0,0001 and p = 0.0032). Extensive (score ≥3) p16 or Cyclin D1 staining was detected in 10 (38%) and 6 (21%) IVL, respectively, with 3 (11%) showing positivity for both (Table 2). All but one IVL (Case 23), as well as their surrounding normal tissue displayed cytoplasmic phosphorylated-Rb staining with background nerve and endometrial cells showing nuclear localization. SMARCB1 and FH expression was preserved in all IVL while SOX10 or Carbonic Anhydrase IX were lacking in all.
Molecular alterations
The most frequently involved chromosome arms were 1p (39%), 22q (36%), 2q (29%), 1q (25%), 13q (21%), 14q (21%), 3q (18%) and 10q (18%) (Fig. 3, Table 3, Supplementary Figs. 1 and 2) with a median genomic index of 4.75 (0–19.3) (Table 2). Putative affected genes in these regions include MEAF6 (1p), SMARCB1 and DEPDC5 (22q), RB1 (13q), RAD51B (14q), KAT6B and FAM22B (10q), in addition to other genes of potential pathogenetic implications on chromosomes 8q (PLAG1), 17p (MYOCD) and Xq (COL4A5/6), among others (Table 3.)
Three molecular groups were identified based on unsupervised hierarchical clustering analysis of the recurrent copy number alterations, which were predominantly deletions: Group 1 (n = 8) and 2 (n = 5) with associated del(22q) (most common shared alteration) and Group 3 (n = 5) with del(10q) (Fig. 4, Supplementary Table 1). All three groups had alterations of 1p (n = 10) and 1q (n = 6). The remaining cases had either nonspecific aberrations (n = 4) or no alterations (n = 6) detected.
Groups 1 and 2 (n = 13) showed common alterations involving 22q (n = 8), 14q (n = 6), 8q (n = 2), 9q (n = 2), 15q (n = 2), 18q (n = 2) and Xp (n = 2), which were not detected in Group 3. Other specific alterations only present in Group 1 included 2q (n = 7), 13q (n = 6), 5q (n = 4). All IVL in Group 3 (n = 5) had del(10q). Nonspecific, but amplification-predominant alterations were seen in five IVL, including two cases with del(22q) that did not have the commonly accompanied alterations present in Groups 1 or 2. Median genomic index scores of Groups 1–3 and those with nonspecific and no alterations were 10.2, 3, 2, 7.15, and 0, respectively.
Integrated clinicopathological and molecular characteristics
Cellular appearance (n = 15, 54%) was the most frequent morphology and present in all molecular groups. Only one cellular (also epithelioid) IVL had no alterations detected. Chromosomal abnormalities in cellular IVL involved 1p (n = 9, 6 with 1q, 2 with 10q, 3 with 8q), 1q (n = 6), 10q (n = 5), 8q (n = 4) that were not seen in IVL with usual cellularity except for those with alterations in 1p (n = 3, none with accompanying 1q or 8q). Among these, three of the four highly cellular IVL had alterations of 1p and 1q (2 with del(10q)) and the other had amplifications of 1q and 8q. Two cellular IVL in Group 3 with del(10q) had adipose tissue (Fig. 1). There were no other unique aberrations associated with a specific morphology.
Among the three molecular IVL groups, only tumors in Group 3 had distinct morphological features. All five IVL in this group were cellular (two highly cellular), with hyaline plaques present in 4, adipose tissue in 2, focal to extensive hyalinized vessels with minimal to focal background hyalinization in 2 (Fig. 1 and Table 2). Three IVL outside Group 3 also had hyaline plaques, including one hypocellular IVL with extensively hyalinized vessels and no detectable copy number alterations (Case 24, recurrence of Case 17 in Group 3, Fig. 1)). The other two cases with hyaline plaques had nonspecific aberrations (1 highly cellular, 1 usual). The only IVL in Group 3 (Case 15) without hyaline plaques or hyalinized vessels had thrombi and myxoid change in large vessels with associated hemorrhage and hemosiderin deposition, a combination of features not found in any other IVL in our series. No clear correlation was observed between morphologic features and other molecular groups. Among the six IVL with no aberrations, three were hypocellular due to extensive hyalinization (two usual, one vascular) while the other three included one usual IVL with focal hyalinization, one cellular and epithelioid, and one vascular IVL.
Immunohistochemical stains were selected based on vasculotropism of IVL (CAIX) as well as recurrent molecular alterations (all the other immunostains). RB (13q), Cyclin D1 and p16 were analyzed given the frequent deletion of 13q (RB1) and regulatory pathway of RB. While cytoplasmic phosphorylated-Rb staining was detected in all but one IVL with hyalinization (Case 23), there was no correlation between p16 or Cyclin D1 expression and tumor morphology, molecular groups or genomic index scores. SMARCB1 (22q), SDHB (1p), and FH (1q) expression was retained. SOX10 (22q) and CAIX were negative in all IVL.
Aggressive clinical behavior was noted in 14 IVL (all with extrauterine extension and 5 associated with recurrences), with no significant differences in morphology, p16 and Cyclin D1 expression, molecular groups (Table 2), or genomic index scores (5.15 vs 3.5) compared to IVL without aggressive behavior.
The majority of IVL associated with recurrence showed vascular morphology (four out of five) (Fig. 2). The distribution of recurrences between molecular groups was as follows: Group 1 (n = 2), Group 2 (n = 1), Group 3 (n = 1) and no alterations (n = 1). Alterations in 8q were detected in three of the recurrent IVL. One patient (Cases three and four) had pelvic recurrence excised 5 years later. Morphologically both tumors showed hydropic change and were focally hyalinized. The recurrence had increased numbers of interspersed capillary lumens. The recurrence showed all the aberrations observed in primary tumor: deletions in 1p, 2p, 2q, 13q, 14q, 22q and amplifications in 8p and 8q and in addition, a new amplification in 2p (480 kb downstream to 2p deletion) and a deletion in 5q (Supplementary Table 1). Another recurrent IVL (Case 13, primary not available) had a deletion of 8q upstream to the aforementioned 8q amplification with deletions in 1p, 18q, 19q and 22q. Another patient had a recurrence 4 months later (cases 17 and 24). The primary tumor was hydropic with prominent hyalinized arteriole-like vessels and had del(10q) while the recurrence was highly vascular with arteriole-like hyalinized vessels, limited cellularity and no genomic alterations. Although not considered a recurrence, it is interesting to note that another patient (Case 15) with del(10q) showing large vessels with extensive thrombi, hemorrhage, myxoid change and hemosiderin deposition without prior treatment, presented 10 years later with a left palm mass that was histologically a thrombosed vein.
Pelvic lymph node involvement was noted in two IVL (Cases 14 and 20), both highly cellular. Case 14 also had adipose tissue and was found to have deletions in 1p, 1q, 3q, and 10q. Case 20 had parametrial and pelvic soft tissue extension and showed amplification of both 8p and 8q.
Discussion
IVL is a rare uterine neoplasm with less than 400 reports in the literature [33,34,35], and is defined as an intravenous endothelium-coated benign smooth muscle proliferation outside the confines of a leiomyoma. The histologic features of IVL overlap with those of typical leiomyoma and leiomyoma variants, including cellular, epithelioid, and hydropic variants, leiomyoma with bizarre nuclei, lipoleiomyoma, and other less common variants [1, 36]. The morphology of IVL may also overlap with other uterine mesenchymal tumors, most commonly hydropic leiomyoma, highly cellular leiomyoma with seedling leiomyomas, low-grade endometrial stromal sarcoma (ESS) and rarely with ULMS if the latter shows a prominent intravascular component [37,38,39]. However, the diagnosis in most cases is straightforward, as low-grade ESS typically presents as a multinodular mass involving the endo-myometrium with tongue-like pattern of myometrial invasion, and is histologically composed of relatively uniform endometrial stromal cells with spiral arterioles [40]. Leiomyosarcoma with prominent vascular involvement shows high-grade cytology, brisk mitotic activity and/or tumor cell necrosis, features that are lacking in IVL [39]. Leiomyoma with hydropic change and highly cellular leiomyoma with seedling leiomyomas may closely mimic the appearance of IVL at low power magnification [37, 41]. IVL may extend outside the uterus, into pelvic vessels, inferior vena cava, the right heart, or may even involve the pulmonary vessels, and it has a recurrence rate of ~10% [2,3,4,5]. Few studies have been conducted to investigate the molecular and immunohistochemical profile of IVL. In this study, we analyzed 28 such tumors by aCGH and immunohistochemistry to further understand their clinicopathologic and genomic characteristics.
Frequent molecular alterations in IVL
IVL has previously been characterized by der(14)t(12;14), a unique cytogenetic alteration detected by karyotyping [42]. This aberration is considered different than the balanced t(12;14) with HMGA2-RAD51B fusion seen in UL. Despite their identical breakpoints, der(14)t(12;14) cytogenetically corresponds to an unbalanced translocation which has two normal chromosome 12, and one normal and one derivative chromosome 14 with a deleted portion of 14q which is presumably replaced by 12q. Therefore, it has been proposed that the presence of an extra copy of 12q and/or loss of 14q may be critical genetic events leading to intravascular proliferation. There is only one reported IVL with a der(14)t(12;14) characterized by karyotyping and FISH that was subsequently analyzed by microarray [23]. It harbored complex chromosome alterations including del(14q) involving RAD51B, surprisingly without an increase in 12q copy number, as well as small deletions in 1p and 1q among others. Interestingly, presence of ring chromosome 1 (presumed to have copy number alterations in 1p, 1q or both) is reported to be a concurrent change in UL with a t(12;14) [43]. This observation parallels the findings in our IVL with del(14q) (n = 6, 5 involving RAD51B), 4 with an accompanying 1p deletion (1 tumor also had 1q gain) and none with 12q alterations. In addition to del(14q) (21%), other most common alterations involved 1p (39%), 22q (36%), 2q (29%), 1q (25%), 13q (21%), 3q (18%), and 10q (18%) (Fig. 3, Table 3), which is similar to a previously reported series [22].
Immunohistochemical characterization of IVL
Deregulation of the Rb/E2F pathway has been identified in a wide range of tumors by altering expression of genes involved in angiogenesis, epithelial-mesenchymal transition, invasion, and migration [44]. Hyperphosphorylation of Rb promotes tumorigenesis by blocking apoptosis and stimulating proliferation and invasion, which is regulated by Cyclin D1 and p16 proteins [45, 46]. In many cancer types alterations leading to increased Rb phosphorylation are more common than Rb mutations and therefore, targeted therapies are designed to inhibit the activity of cyclin dependent kinases toward Rb [47]. In this series, one of the most frequent alterations was del(13q) (RB1) (Table 3, Supplementary Table 1). Ser807 is a site phosphorylated by Cyclin D1/CDK4 that is shown to be important for hyperphosphorylation of Rb and its nuclear export resulting in its inactivation [48]. In this study, all but one IVL, which was hypocellular, displayed cytoplasmic phosphorylated-Rb localization, suggesting that nuclear export may be the mechanism for Rb inactivation.
IVL molecular groups vs UL subtypes
IVL were grouped by hierarchical clustering of recurrent aberrations to further correlate the concurrent alterations amongst each other as well as with clinicopathologic findings (Fig. 4 and Table 2). Three molecular groups were identified, while the rest had nonspecific/no alterations. The two most common characteristic changes in Groups 1 (n = 8, 29%) and 2 (n = 5, 18%) were del(22q) (n = 8) and del(14q) (n = 6), whereas all IVL in Group 3 had a distinct profile of del(10q) (n = 5, 18%). Alterations involving 1p (n = 10) and 1q (n = 6) were seen in all three groups. Based on these results, Group 1 can be considered the genomically unstable counterpart of Group 2 (median genomic index = 10.2 vs 3) given multiple unique alterations in Group 1, including changes in 2q, 13q, 5q, besides the common alterations seen in both groups. Four IVL (14%) had copy number changes that could not be categorized into any specific group, showing predominantly amplifications, in contrast to Groups 1–3 showing predominantly deletions. Six (21%) IVL had no alterations detected (three of them with limited tumor cellularity due to extensive hyalinization).
The three genomic groups described herein are comparable to the molecular subtypes described in UL, despite technical limitations related to detection of point mutations and balanced rearrangements by aCGH. In a study by Mehine et al. with selective enrichment of otherwise rare del(22q) UL (20/94), four UL subtypes were identified integrating both gene expression data and genomic alterations: HMGA2 (12q), MED12 (Xq), FH (1q), and COL4A5-COL4A6 (Xq)) [18]. Among these, HMGA2 UL usually had t(12;14) with RAD51B (14q) as the preferential translocation partner, whereas MED12 UL showed up-regulation of RAD51B expression. Nineteen out of 20 del(22q) UL clustered in either HMGA2 (12) or COL4A5/6 (7) subtypes. In our series, eight out of ten del(22q) IVL clustered together with IVL having del(14q) (n = 6, 5 involving RAD51B) and del (Xq) (n = 2, 1 involving COL4A5/6) in Groups 1 and 2 (Fig. 4, Supplementary Table 1). Although the number of cases is limited in both studies, it is worth noting that both IVL and UL with del(22q) appeared to have overlapping molecular features with tumors having genomic alterations in HMGA2/RAD51B or COL4A5/6 based on their preferential clustering with such tumors. In addition, UL with 22q alterations were further characterized by studying minimally deleted regions (27,111,559–33,871,686) and a UL with 22q translocation. DEPDC5 (with five UL showing a “second hit” mutation in this gene) and SMARCB1 were identified as the two putative target genes involved in 22q UL. Not only the minimally deleted 22q region reported in UL had a 4 Mb overlap with one reported herein (27,111,559–33,871,686 vs 25,351,942–31,211,236, respectively, Table 3), but also both DEPDC5 and SMARCB1 were either involved by or within 1 Mb of the altered region in nine out of ten IVL with del(22q). Taken together, IVL with del(22q) and del(14q) are common and tend to cluster together in same molecular groups, which appear to share similar molecular characteristics with their UL counterparts. Of note, none of the del(14q) IVL in our study had a del(10q), however, the aforementioned IVL described elsewhere [23] with der(14) with del(14q) also had a del(10q).
Group 3 IVL (18%) were characterized by del(10q). Alterations involving 10q have rarely been reported in UL (2%) [49], although specifically del(10q) are more commonly observed in ULMS than UL [50]. KAT6B, a rare tumor suppressor gene with homozygous deletions in multiple cancer types [51, 52], is described as the candidate 10q gene in UL in a study analyzing the rare t(10;17) event [53] and a similar t(10;17), resulting in a KAT6B-KANSL1 fusion detected in a retroperitoneal and more recently in a UL [54, 55]. This fusion is located at exon 3 (histone binding domain) of KAT6B without involvement of the downstream functional domains (histone acetylation and transcriptional activation), implicating KAT6B loss of function. Furthermore, germline mutations in both KAT6B and MED12 are associated with Ohdo Syndrome, a heterogenous group of disorders with intellectual disability and craniofacial anomalies [56]. Therefore, previous studies suggested that MED12 and KAT6B are functionally related, both encoding for chromatin-modifying enzymes and implicated in same diseases with mutations at germline and somatic levels [56, 57]. Interestingly, in our series all del(10q) IVL in Group 3 (5) involved KAT6B and none clustered together with del(22q), which may be parallel to UL groups with only 1 out of 20 del(22q) clustering with the MED12 subtype [18].
Overall, our IVL molecular groups had overlapping characteristics with UL subtypes, albeit the latter has been studied more comprehensively due to integration of RNA data. Commonly altered chromosome regions in IVL (Table 3) are less frequently involved in UL except for 14q (RAD51B). However, despite 14q being a frequently altered region in IVL and UL, the unbalanced nature of this aberration remains unique to IVL. The paucity of the common IVL alterations in UL may provide insight into the fact that only a very small subset of women with UL have accompanying IVL. Analysis of additional IVL along with RNA expression and fusion transcript data may help further characterize IVL molecular groups and their correlations with UL subtypes.
Alterations in IVL vs other UL variants with unusual clinical behavior and soft tissue LM
Benign metastasizing leiomyoma (BML) and disseminated peritoneal leiomyomatosis (DPL) are considered other unusual leiomyoma variants. Alterations involving 1p, 2q, 3q, 7p, 11q, 19q, 22q have been reported in BML [58,59,60]. A case report of a cellular DPL after morcellation of a hydropic and hyalinized UL showed r(1), del(3q), del(9q) and t(12;14) on karyotype with 1p, 1q, 2p 2q 3q, 14q loss, and 11p gain on microarray, in parallel to the aforementioned associations of IVL with der(14) and its relationship to r(1) and del(14q).In a study analyzing 8 soft tissue LM (all female patients with retroperitoneal/pelvic tumors), 3 had 12q alterations (inv(12); t(12;14); der(12) and del(14q) as well as −22), 3 had 8q (ins(8)(p23q12q22), t(8;14)(q13;q24), t(8;19)(q12;q13)), 1 had del(7) and del(14q), 1 had t(3;11) and add(11q). Tumors with 8q alterations showed PLAG1 involvement [61], which was also amplified in three IVL with aggressive behavior in our series. These rare subsets of leiomyomas occurring outside the uterus have recurrent alterations similar to those seen in IVL, which are rarely seen in UL.
Alterations in cellular IVL vs cellular UL and ESS
Cellular UL has been associated with del(1p) and t(10;17) [19, 53, 62]. In particular, a study analyzing 9 UL with del(1p) and other aberrations including loss of chromosomes 19 and/or 22, and less commonly 10q, 13q and 14, reported 6 of them being cellular [62]. In another study, gene expression analysis demonstrated clustering of IVL with ULMS and cellular/atypical UL with 1p deletion, rather than with myometrium, usual or plexiform UL [23]. In the current series, chromosomal abnormalities in cellular IVL involved 1p, 1q, 8q and 10q. Among these, 3 of the 4 highly cellular IVL had alterations of 1p and 1q (2 with del(10q)) and the other had amplifications of 8q and 8q. Although the copy number alterations reported herein are mostly Mb-sized larger genomic regions, it is interesting to note that some of the recurrent alterations in cellular IVL involve genes altered in ESS genomic rearrangements including MEAF6 (1p) and FAM22B (10q) (Table 3).
Vascular IVL vs angioleiomyoma
Angioleiomyoma (angiomyoma, vascular leiomyoma) is a benign soft tissue tumor with thick-walled vessels formed by proliferating smooth muscle cells, and vascular channels, which can rarely occur in the uterus [26]. Deletions in 6p [63] and 13q have been described in soft tissue tumors [64]. A microarray analysis of these tumors showed recurrent 22q loss as the most common alteration (22%) [65]. Cytogenetic analysis of a uterine angioleiomyoma showed a complex karyotype with abnormalities involving 2p, 2q, 5q, 11p, 20q and Xp including inv(2)(p15q13) [66]. None of these alterations are common in UL, however, they mostly overlap with IVL reported herein including those with vascular morphology, albeit not specific to this morphologic subtype.
IVL with del(22q) and del(14q) vs gastrointestinal stromal tumors (GIST)
The loss of 22q is one of the most frequent alterations in IVL, identified in 36% of tumors in our series and in two-thirds of tumors in a previously published smaller series [22]. In addition, we observed the loss of 14q in 21% of IVL. Interestingly, losses involving chromosomes 22q and 14q have also been frequently found in GIST [67,68,69,70], and it has been suggested that these alterations play an important role in early stages of GIST tumorigenesis [70]. In addition, allelic losses at 22q in GIST were found to be associated with high mitotic activity and disease recurrence [71]. We observed the loss of 22q in 6 of 14 IVL with extrauterine extension and in 3 of 5 recurrent tumors, suggesting the possibility of a similar association. From a potential diagnostic aspect, although karyotyping or array CGH are not typically performed as part of the routine diagnostic work-up, the overlap in tumor genomic profiles between GIST and IVL should also be taken into account when encountering spindle cell tumors at unusual peritoneal locations.
IVL vs smooth muscle tumors of uncertain malignant potential (STUMP)
Although IVL is histologically benign, our series shows molecular features that parallel those reported in STUMP [72]. An array genomic hybridization analysis of 29 STUMP showed alterations involving 22q (70%), 13q (50%), 11p (50%), 6q (50%), 3q (50%) and 1q (60%) [31]. In addition, a recent series by Croce et al. of 77 uterine smooth muscle tumors with a mean follow up of 63.6 months identified a genomic index cut-off score of 10 as a predictor of recurrence and a criterion for “molecular leiomyosarcoma” [32]. Among stage 1 “molecular leiomyosarcomas” in that study, poor prognostic markers included genomic index cut-off score of 35, 5p gain, 13q loss involving RB1 and 17p gain involving MYOCD, the latter promoting smooth muscle differentiation and cell migration [73]. Alterations of 22q (36%), 13q (21%), 6q (14%), 3q (18%) and 1q (25%) (Table 3) were overlapping recurrent aberrations detected in IVL in our series (predominantly in Group 1), although less frequent than those previously reported in STUMP. Six (21%) IVL had a genomic index of ≥10 (all < 35), also mostly in Group 1 (four of them). However, there was no association between genomic index (with or without specific cut-off of 10) and clinically aggressive behavior in IVL. It is interesting to note that Case 5 (Group 1) had the highest genomic index (19.3) and would have qualified as “molecular leiomyosarcoma” with two poor prognostic factors (5p gain and 13q loss) based on the aforementioned study. However, it had usual morphology, was confined to the uterus, and the patient had no recurrence after 6 years. Therefore, especially in the setting of leiomyoma variants, results of genomic analysis should be interpreted carefully in correlation with the pathologic findings. That said, the majority of the tumors in our series showed simple genomic profiles (genomic index ranging from 0 to 19.3; mean 5.9), significantly different from the previously reported genomic profiles of leiomyosarcomas (with genomic index up to 180, and mean 51.8) [32]. Future studies—using other techniques (mutation and gene expression analyses)—may uncover additional genomic alterations not detectable by aCGH (mutations or balanced rearrangements) that may be responsible for the intravascular tumor location and the resulting aggressive clinical behavior in some patients.
In summary, we describe three genomic groups of IVL, in which del(10q) and del(22q) were mutually exclusive with overlap in other aberrations including del(1p), comparable to molecular subtypes reported in UL. The described recurrent chromosome alterations included target genes reported in other uterine and extrauterine mesenchymal tumors with unique histologic characteristics particularly for cellular, vascular and Group 3 tumors with del(10q). The previously proposed genomic index for uterine smooth muscle tumors did not predict a malignant course in our series and there was no specific molecular alteration associated with aggressive behavior. Our molecular and immunohistochemical findings suggest involvement of the Rb pathway in the pathogenesis of a subset of IVL. Currently, this is the largest series correlating histological, immunohistochemical, and molecular characteristics of IVL. While our molecular analysis is limited to array CGH, these data may serve as a platform for future studies—including additional protein expression analysis and next generation sequencing—on IVL and paired adjacent leiomyomas to further explore their potential pathogenetic relationship and elucidate the critical steps of IVL tumorigenesis.
References
Clement PB, Young RH, Scully RE. Intravenous leiomyomatosis of the uterus. A clinicopathological analysis of 16 cases with unusual histologic features. Am J Surg Pathol. 1988;12:932–45.
Marshall JF, Morris DS. Intravenous leiomyomatosis of the uterus and pelvis: case report. Ann Surg 1959;149:126–34.
Valdes Devesa V, Conley CR, Stone WM, Collins JM, Magrina JF. Update on intravenous leiomyomatosis: report of five patients and literature review. Eur J Obstet Gynecol Reprod Biol. 2013;171:209–13.
Castagneto Gissey L, Mariano G, Musleh L, Lepiane P, Colasanti M, Meniconi RL, et al. Massive pelvic recurrence of uterine leiomyomatosis with intracaval-intracardiac extension: video case report and literature review. BMC Surg. 2017;17:118.
Carr RJ, Hui P, Buza N. Intravenous leiomyomatosis revisited: an experience of 14 cases at a single medical center. Int J Gynecol Pathol. 2015;34:169–76.
Ligon AH, Morton CC. Genetics of uterine leiomyomata. Genes Chromosomes Cancer. 2000;28:235–45.
Ordulu Z. Fibroids: genotype and phenotype. Clin Obstet Gynecol. 2016;59:25–29.
Pandis N, Heim S, Bardi G, Floderus UM, Willen H, Mandahl N, et al. Chromosome analysis of 96 uterine leiomyomas. Cancer Genet Cytogenet. 1991;55:11–18.
Xing YP, Powell WL, Morton CC. The del(7q) subgroup in uterine leiomyomata: genetic and biologic characteristics. Further evidence for the secondary nature of cytogenetic abnormalities in the pathobiology of uterine leiomyomata. Cancer Genet Cytogenet. 1997;98:69–74.
Makinen N, Mehine M, Tolvanen J, Kaasinen E, Li Y, Lehtonen HJ, et al. MED12, the mediator complex subunit 12 gene, is mutated at high frequency in uterine leiomyomas. Science. 2011;334:252–5.
Markowski DN, Bartnitzke S, Loning T, Drieschner N, Helmke BM, Bullerdiek J. MED12 mutations in uterine fibroids—their relationship to cytogenetic subgroups. Int J Cancer. 2012;131:1528–36.
Mehine M, Kaasinen E, Makinen N, Katainen R, Kampjarvi K, Pitkanen E, et al. Characterization of uterine leiomyomas by whole-genome sequencing. N. Engl J Med. 2013;369:43–53.
Hayden MA, Ordulu Z, Gallagher CS, Quade BJ, Anchan RM, Middleton NR, et al. Clinical, pathologic, cytogenetic, and molecular profiling in self-identified black women with uterine leiomyomata. Cancer Genet. 2018;222-223:1–8.
Mehine M, Makinen N, Heinonen HR, Aaltonen LA, Vahteristo P. Genomics of uterine leiomyomas: insights from high-throughput sequencing. Fertil Steril. 2014;102:621–9.
Gross KL, Panhuysen CI, Kleinman MS, Goldhammer H, Jones ES, Nassery N, et al. Involvement of fumarate hydratase in nonsyndromic uterine leiomyomas: genetic linkage analysis and FISH studies. Genes Chromosomes Cancer. 2004;41:183–90.
Nezhad MH, Drieschner N, Helms S, Meyer A, Tadayyon M, Klemke M, et al. 6p21 rearrangements in uterine leiomyomas targeting HMGA1. Cancer Genet Cytogenet. 2010;203:247–52.
Dal Cin P, Moerman P, Deprest J, Brosens I, Van, den Berghe H. A new cytogenetic subgroup in uterine leiomyoma is characterized by a deletion of the long arm of chromosome 3. Genes Chromosomes Cancer. 1995;13:219–20.
Mehine M, Kaasinen E, Heinonen HR, Makinen N, Kampjarvi K, Sarvilinna N, et al. Integrated data analysis reveals uterine leiomyoma subtypes with distinct driver pathways and biomarkers. Proc Natl Acad Sci USA. 2016;113:1315–20.
Hodge JC, Pearce KE, Clayton AC, Taran FA, Stewart EA. Uterine cellular leiomyomata with chromosome 1p deletions represent a distinct entity. Am J Obstet Gynecol. 2014;210:572 e571–577.
Cancer Genome Atlas Research Network. Electronic address edsc, Cancer Genome Atlas Research N. Comprehensive and integrated genomic characterization of adult soft tissue sarcomas. Cell. 2017;171:950–965 e928.
Raish M, Khurshid M, Ansari MA, Chaturvedi PK, Bae SM, Kim JH, et al. Analysis of molecular cytogenetic alterations in uterine leiomyosarcoma by array-based comparative genomic hybridization. J Cancer Res Clin Oncol. 2012;138:1173–86.
Buza N, Xu F, Wu W, Carr RJ, Li P, Hui P. Recurrent chromosomal aberrations in intravenous leiomyomatosis of the uterus: high-resolution array comparative genomic hybridization study. Hum Pathol. 2014;45:1885–92.
Ordulu Z, Nucci MR, Dal Cin P, Hollowell ML, Otis CN, Hornick JL, et al. Intravenous leiomyomatosis: an unusual intermediate between benign and malignant uterine smooth muscle tumors. Mod Pathol. 2016;29:500–10.
Zhang X, Wu L, Xu R, Zhu C, Ma G, Zhang C, et al. Identification of the molecular relationship between intravenous leiomyomatosis and uterine myoma using RNA sequencing. Sci Rep. 2019;9:1442.
Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer. 1984;54:126–30.
McCluggage WG, Boyde A. Uterine angioleiomyomas: a report of 3 cases of a distinctive benign leiomyoma variant. Int J Surg Pathol. 2007;15:262–5.
Bajaj R, Xu F, Xiang B, Wilcox K, Diadamo AJ, Kumar R, et al. Evidence-based genomic diagnosis characterized chromosomal and cryptic imbalances in 30 elderly patients with myelodysplastic syndrome and acute myeloid leukemia. Mol Cytogenet. 2011;4:3.
MacDonald JR, Ziman R, Yuen RK, Feuk L, Scherer SW. The Database of Genomic Variants: a curated collection of structural variation in the human genome. Nucleic Acids Res. 2014;42:D986–992.
Futreal PA, Coin L, Marshall M, Down T, Hubbard T, Wooster R, et al. A census of human cancer genes. Nat Rev Cancer. 2004;4:177–83.
Lagarde P, Perot G, Kauffmann A, Brulard C, Dapremont V, Hostein I, et al. Mitotic checkpoints and chromosome instability are strong predictors of clinical outcome in gastrointestinal stromal tumors. Clin Cancer Res. 2012;18:826–38.
Croce S, Ribeiro A, Brulard C, Noel JC, Amant F, Stoeckle E, et al. Uterine smooth muscle tumor analysis by comparative genomic hybridization: a useful diagnostic tool in challenging lesions. Mod Pathol. 2015;28:1001–10.
Croce S, Ducoulombier A, Ribeiro A, Lesluyes T, Noel JC, Amant F, et al. Genome profiling is an efficient tool to avoid the STUMP classification of uterine smooth muscle lesions: a comprehensive array-genomic hybridization analysis of 77 tumors. Mod Pathol. 2018;31:816–28.
Ip PP, Tse KY, Tam KF. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: a review of selected variants with emphasis on recent advances and unusual morphology that may cause concern for malignancy. Adv Anat Pathol. 2010;17:91–112.
Mahmoud MS, Desai K, Nezhat FR. Leiomyomas beyond the uterus; benign metastasizing leiomyomatosis with paraaortic metastasizing endometriosis and intravenous leiomyomatosis: a case series and review of the literature. Arch Gynecol Obstet. 2015;291:223–30.
Low HY, Zhao Y, Huang KS, Shen HP, Wu PJ, Tseng CJ. Intravenous leiomyomatosis of the uterus: A clinicopathological analysis of nine cases and literature review. Taiwan J Obstet Gynecol. 2017;56:362–5.
Clement PB. The pathology of uterine smooth muscle tumors and mixed endometrial stromal-smooth muscle tumors: a selective review with emphasis on recent advances. Int J Gynecol Pathol. 2000;19:39–55.
Oliva E, Young RH, Clement PB, Bhan AK, Scully RE. Cellular benign mesenchymal tumors of the uterus. A comparative morphologic and immunohistochemical analysis of 33 highly cellular leiomyomas and six endometrial stromal nodules, two frequently confused tumors. Am J Surg Pathol. 1995;19:757–68.
Oliva E. Cellular mesenchymal tumors of the uterus: a review emphasizing recent observations. Int J Gynecol Pathol. 2014;33:374–84.
Coard KC, Fletcher HM. Leiomyosarcoma of the uterus with a florid intravascular component (“intravenous leiomyosarcomatosis”). Int J Gynecol Pathol. 2002;21:182–5.
Chang KL, Crabtree GS, Lim-Tan SK, Kempson RL, Hendrickson MR. Primary uterine endometrial stromal neoplasms. A clinicopathologic study of 117 cases. Am J Surg Pathol. 1990;14:415–38.
Clement PB, Young RH, Scully RE. Diffuse, perinodular, and other patterns of hydropic degeneration within and adjacent to uterine leiomyomas. Problems in differential diagnosis. Am J Surg Pathol. 1992;16:26–32.
Dal Cin P, Quade BJ, Neskey DM, Kleinman MS, Weremowicz S, Morton CC. Intravenous leiomyomatosis is characterized by a der(14)t(12;14)(q15;q24). Genes Chromosomes Cancer. 2003;36:205–6.
Nilbert M, Heim S, Mandahl N, Floderus UM, Willen H, Akerman M, et al. Ring formation and structural rearrangements of chromosome 1 as secondary changes in uterine leiomyomas with t(12;14)(q14-15;q23-24). Cancer Genet Cytogenet. 1988;36:183–90.
Schaal C, Pillai S, Chellappan SP. The Rb-E2F transcriptional regulatory pathway in tumor angiogenesis and metastasis. Adv Cancer Res. 2014;121:147–82.
Mittnacht S. The retinoblastoma protein—from bench to bedside. Eur J Cell Biol. 2005;84:97–107.
Sherr CJ, McCormick F. The RB and p53 pathways in cancer. Cancer Cell. 2002;2:103–12.
Stone A, Sutherland RL, Musgrove EA. Inhibitors of cell cycle kinases: recent advances and future prospects as cancer therapeutics. Crit Rev Oncog. 2012;17:175–98.
Jiao W, Datta J, Lin HM, Dundr M, Rane SG. Nucleocytoplasmic shuttling of the retinoblastoma tumor suppressor protein via Cdk phosphorylation-dependent nuclear export. J Biol Chem. 2006;281:38098–108.
Ozisik YY, Meloni AM, Surti U, Sandberg AA. Involvement of 10q22 in leiomyoma. Cancer Genet Cytogenet. 1993;69:132–5.
Quade BJ, Pinto AP, Howard DR, Peters WA 3rd, Crum CP. Frequent loss of heterozygosity for chromosome 10 in uterine leiomyosarcoma in contrast to leiomyoma. Am J Pathol. 1999;154:945–50.
Cheng J, Demeulemeester J, Wedge DC, Vollan HKM, Pitt JJ, Russnes HG, et al. Pan-cancer analysis of homozygous deletions in primary tumours uncovers rare tumour suppressors. Nat Commun. 2017;8:1221.
Simo-Riudalbas L, Perez-Salvia M, Setien F, Villanueva A, Moutinho C, Martinez-Cardus A, et al. KAT6B is a tumor suppressor histone H3 lysine 23 acetyltransferase undergoing genomic loss in small cell lung cancer. Cancer Res. 2015;75:3936–45.
Moore SD, Herrick SR, Ince TA, Kleinman MS, Dal Cin P, Morton CC, et al. Uterine leiomyomata with t(10;17) disrupt the histone acetyltransferase MORF. Cancer Res. 2004;64:5570–7.
Panagopoulos I, Gorunova L, Bjerkehagen B, Heim S. Novel KAT6B-KANSL1 fusion gene identified by RNA sequencing in retroperitoneal leiomyoma with t(10;17)(q22;q21). PLoS One. 2015;10:e0117010.
Ainsworth AJ, Dashti NK, Mounajjed T, Fritchie KJ, Davila J, Mopuri R, et al. Leiomyoma with KAT6B-KANSL1 fusion: case report of a rapidly enlarging uterine mass in a postmenopausal woman. Diagn Pathol. 2019;14:32.
Vulto-van Silfhout AT, de Vries BB, van Bon BW, Hoischen A, Ruiterkamp-Versteeg M, Gilissen C, et al. Mutations in MED12 cause X-linked ohdo syndrome. Am J Hum Genet. 2013;92:401–6.
Ullah M, Pelletier N, Xiao L, Zhao SP, Wang K, Degerny C, et al. Molecular architecture of quartet MOZ/MORF histone acetyltransferase complexes. Mol Cell Biol. 2008;28:6828–43.
Wu RC, Chao AS, Lee LY, Lin G, Chen SJ, Lu YJ, et al. Massively parallel sequencing and genome-wide copy number analysis revealed a clonal relationship in benign metastasizing leiomyoma. Oncotarget. 2017;8:47547–54.
Soritsa D, Teder H, Roosipuu R, Tamm H, Laisk-Podar T, Soplepmann P, et al. Whole exome sequencing of benign pulmonary metastasizing leiomyoma reveals mutation in the BMP8B gene. BMC Med Genet. 2018;19:20.
Nucci MR, Drapkin R, Dal Cin P, Fletcher CD, Fletcher JA. Distinctive cytogenetic profile in benign metastasizing leiomyoma: pathogenetic implications. Am J Surg Pathol. 2007;31:737–43.
Panagopoulos I, Gorunova L, Brunetti M, Agostini A, Andersen HK, Lobmaier I, et al. Genetic heterogeneity in leiomyomas of deep soft tissue. Oncotarget. 2017;8:48769–81.
Christacos NC, Quade BJ, Dal Cin P, Morton CC. Uterine leiomyomata with deletions of Ip represent a distinct cytogenetic subgroup associated with unusual histologic features. Genes Chromosomes Cancer. 2006;45:304–12.
Heim S, Mandahl N, Kristoffersson U, Mitelman F, Rooser B, Rydholm A, et al. Structural chromosome aberrations in a case of angioleiomyoma. Cancer Genet Cytogenet. 1986;20:325–30.
Nilbert M, Mandahl N, Heim S, Rydholm A, Willen H, Mitelman F. Cytogenetic abnormalities in an angioleiomyoma. Cancer Genet Cytogenet. 1989;37:61–64.
Nishio J, Iwasaki H, Ohjimi Y, Ishiguro M, Kobayashi K, Nabeshima K, et al. Chromosomal imbalances in angioleiomyomas by comparative genomic hybridization. Int J Mol Med. 2004;13:13–16.
Hennig Y, Caselitz J, Stern C, Bartnitzke S, Bullerdiek J. Karyotype evolution in a case of uterine angioleiomyoma. Cancer Genet Cytogenet. 1999;108:79–80.
Breiner JA, Meis-Kindblom J, Kindblom LG, McComb E, Liu J, Nelson M, et al. Loss of 14q and 22q in gastrointestinal stromal tumors (pacemaker cell tumors). Cancer Genet Cytogenet. 2000;120:111–6.
Schoppmann SF, Vinatzer U, Popitsch N, Mittlbock M, Liebmann-Reindl S, Jomrich G, et al. Novel clinically relevant genes in gastrointestinal stromal tumors identified by exome sequencing. Clin Cancer Res. 2013;19:5329–39.
Yang J, Du X, Lazar AJ, Pollock R, Hunt K, Chen K, et al. Genetic aberrations of gastrointestinal stromal tumors. Cancer. 2008;113:1532–43.
Wozniak A, Sciot R, Guillou L, Pauwels P, Wasag B, Stul M, et al. Array CGH analysis in primary gastrointestinal stromal tumors: cytogenetic profile correlates with anatomic site and tumor aggressiveness, irrespective of mutational status. Genes Chromosomes Cancer. 2007;46:261–76.
Pylkkanen L, Sarlomo-Rikala M, Wessman M, Hamalainen E, Sainio M, Husgafvel-Pursiainen K, et al. Chromosome 22q alterations and expression of the NF2 gene product, merlin, in gastrointestinal stromal tumors. Hum Pathol. 2003;34:872–9.
Bell SW, Kempson RL, Hendrickson MR. Problematic uterine smooth muscle neoplasms. A clinicopathologic study of 213 cases. Am J Surg Pathol. 1994;18:535–58.
Perot G, Derre J, Coindre JM, Tirode F, Lucchesi C, Mariani O, et al. Strong smooth muscle differentiation is dependent on myocardin gene amplification in most human retroperitoneal leiomyosarcomas. Cancer Res. 2009;69:2269–78.
Acknowledgements
We thank Massachusetts General Hospital immunohistochemistry Laboratory and Dana-Farber/Harvard Cancer Center in Boston, MA, for the use of the Specialized Histopathology Core, which provided histology and immunohistochemistry service. Dana-Farber/Harvard Cancer Center is supported in part by an NCI Cancer Center Support Grant # NIH 5 P30 CA06516. This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ordulu, Z., Chai, H., Peng, G. et al. Molecular and clinicopathologic characterization of intravenous leiomyomatosis. Mod Pathol 33, 1844–1860 (2020). https://doi.org/10.1038/s41379-020-0546-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-0546-8
This article is cited by
-
Safety and efficacy of sirolimus in recurrent intravenous leiomyomatosis, pulmonary benign metastatic leiomyomatosis, and leiomyomatosis peritonealis disseminata: a pilot study
BMC Medicine (2024)
-
MR imaging findings of stage I intravenous leiomyomatosis: a retrospective single-center study in 19 cases
Abdominal Radiology (2024)
-
Correlating genomic copy number alterations with clinicopathologic findings in 75 cases of hepatocellular carcinoma
BMC Medical Genomics (2021)
-
Retroperitoneal angioleiomyomatosis
The Journal of Obstetrics and Gynecology of India (2021)