Abstract
Tumor proportion score (TPS) and combined positive score ([CPS] includes immune cells), 2 methods for scoring programmed death ligand 1 (PD-L1) expression, have been used in clinical trials investigating the immune checkpoint inhibitor pembrolizumab in head and neck squamous cell carcinoma (HNSCC). These trials resulted in regulatory approval for pembrolizumab in the first- and second-line setting outside the United States. We performed a post hoc analysis of the KEYNOTE-040 study (NCT02252042) to determine whether CPS is a practical and suitable alternative scoring method to TPS. In KEYNOTE-040, patients with metastatic HNSCC received pembrolizumab or investigator choice of standard of care (SOC). The relative utility and equivalence of CPS ≥ 50 and TPS ≥ 50% for defining PD-L1 expression status in patients with HNSCC and comparability of scoring methods by tandem receiver operating characteristic (ROC) analysis were analyzed. The cutoff for each method was also evaluated. CPS ≥ 50 appeared equivalent to TPS ≥ 50% for predicting objective response rate (ORR), overall survival, and progression-free survival. ORR for pembrolizumab versus SOC was 26.2 versus 8.5% for TPS ≥ 50%, 28.1 versus 7.7% for CPS ≥ 50, 10.6 versus 11.6% for TPS < 50%, and 10.0 versus 12.0% for CPS < 50. Tandem ROC analysis showed that TPS 50% and CPS 50 maximized delta Youden index and suggested that CPS is more sensitive than TPS at lower cutoffs (i.e., CPS ≥ 1). In conclusion, CPS 50 can be used interchangeably with TPS 50% to determine PD-L1 status in patients with HNSCC. CPS may be more sensitive than TPS at lower cutoffs.
Similar content being viewed by others
Introduction
Programmed death ligand 1 (PD-L1) overexpression can promote immune evasion and has been reported in several tumor types, including colon adenocarcinoma, gastric carcinoma, glioblastoma, melanoma, nasopharyngeal cancer, non–small cell lung carcinoma (NSCLC), renal cell carcinoma, urothelial cancer, and head and neck squamous cell carcinoma (HNSCC) [1, 2]. Host immune cells expressing programmed death 1 (PD-1) receptor bind to its ligands, PD-L1 and PD-L2, on a variety of cell types, including tumor cells, and on cells within the tumor microenvironment, and are inactivated [3,4,5]. Anti–PD-1 and anti–PD-L1 agents, which block receptor-ligand binding, restore host immune cell activation and cytotoxicity. PD-L1 expression on tumor and/or immune cells is predictive of benefit from anti–PD-1 and anti–PD-L1 therapy in several tumor types [3].
NSCLC was one of the first tumor types for which PD-L1 was successfully implemented as a biomarker to predict response to immunotherapy [6,7,8,9,10]. PD-L1 expression was evaluated by immunohistochemistry (IHC) and determined by tumor proportion score (TPS), defined as the percentage of viable tumor cells with partial or complete membrane staining at any intensity [11]. PD-L1 expression assays have been labeled companion diagnostics for NSCLC. Data from patients with NSCLC and PD-L1 expression enrolled in phase 3 clinical trials with the immune checkpoint inhibitors nivolumab, pembrolizumab, and atezolizumab demonstrated higher response rates and favorable outcomes; however, different cutoffs for PD-L1 expression were used across these trials, as were different antibody clones and variability across patient populations [6]. For example, in the phase 3 CheckMate 057 trial, patients with non-squamous NSCLC that had progressed on or after platinum-based doublet chemotherapy were treated with nivolumab [6]. Objective response rate (ORR) was greater in patients with tumor PD-L1 expression ≥10% than in patients with PD-L1 expression <1% (37 vs. 9%). Progression-free survival (PFS) was 5.0 months versus 2.1 months; overall survival (OS) was 19.9 months versus 10.5 months. That study used the 28-8 monoclonal antibody to identify PD-L1 expression. In the KEYNOTE-010 trial, patients with previously treated NSCLC received pembrolizumab [12]. Patients receiving pembrolizumab 2 mg/kg with TPS ≥ 1% had an ORR of 18%, and patients with TPS ≥ 50% had an ORR of 30%; PFS was 3.9 months versus 5.0 months; OS was 10.4 months versus 14.9 months. This study used the 22C3 monoclonal antibody. Finally, in the phase 3 OAK trial, patients with previously treated NSCLC were treated with atezolizumab or docetaxel [13]. PD-L1 expression, identified using the SP142 PD-L1 IHC assay, was defined as follows: TC1/2/3 or IC1/2/3, PD-L1 expression on ≥1% of tumor cells or tumor-infiltrating immune cells, respectively; TC2/3 or IC2/3, PD-L1 expression on ≥5% of these cells; TC3, PD-L1 expression on ≥50% of tumor cells; IC3, expression on ≥10% of tumor-infiltrating immune cells; TC0 and IC0, PD-L1 expression on <1% of the respective cells. In that study, ORR was 8% in patients with TC0 and IC0 and 31% in those with TC3 or IC3. OS in patients receiving atezolizumab was 12.6 months in those with TC0 and IC0 and 20.5 months in those with TC3 or IC3 [13]. Despite the utility of TPS to measure PD-L1 expression in NSCLC, use of different staining platforms and antibodies, types of cells in which PD-L1 is assessed (tumor vs. immune cells), and thresholds used for PD-L1 positivity create challenges in the interpretation of PD-L1 expression across tumor types and therapeutic agents [11].
Based on emerging evidence, tumor PD-L1 expression alone may not be a suitable predictive biomarker for all tumor types [14]. Given that various mechanisms of immune evasion take place in many cancers, there is potential for immune cell PD-L1 expression to play a role in predicting checkpoint inhibitor response [14,15,16,17]. In fact, the presence of tumor-infiltrating lymphocytes has been shown to predict response of solid tumors to anti–PD-1 therapy [15, 18]. Thus, another scoring method, combined positive score (CPS), was developed to incorporate immune cell PD-L1 expression into a predictive biomarker [14, 19]; this has now been used across many tumor types. CPS is defined as the ratio of the number of PD-L1–expressing cells (tumor cells, lymphocytes, macrophages) to the number of all viable tumor cells multiplied by 100 and can be scored directly and reproducibly in one review by a pathologist [14, 19]. PD-L1 IHC 22C3 pharmDx (Agilent Technologies, Inc., Santa Clara, CA, USA) is a companion diagnostic test approved by the United States Food and Drug Administration (FDA) to evaluate PD-L1 expression in patients treated with pembrolizumab for NSCLC, gastric or gastroesophageal junction adenocarcinoma, esophageal squamous cell carcinoma, cervical cancer, or urothelial carcinoma [20, 21].
Pembrolizumab is also approved for patients with HNSCC, and PD-L1 IHC 22C3 pharmDx is a companion diagnostic in this setting as well. The FDA approved pembrolizumab for the treatment of patients with recurrent or metastatic (R/M) HNSCC with disease progression on or after platinum-containing chemotherapy based on single-arm clinical trial results from KEYNOTE-012, regardless of PD-L1 expression [21]. The randomized phase 3 KEYNOTE-040 trial, which investigated pembrolizumab versus standard of care (SOC) for patients with R/M HNSCC, stratified patients based on PD-L1 expression (TPS ≥ 50 vs. <50%) [22]. Pembrolizumab provided clinically meaningful prolongation of OS in the intention-to-treat population with fewer grade ≥3 treatment-related events compared with SOC (13 vs. 36%) [22]. Data from that trial led to European Medicines Agency (EMA) approval of pembrolizumab as monotherapy for the treatment of R/M HNSCC in adults whose tumors express PD-L1 with TPS ≥ 50% and who experienced disease progression on or after platinum-containing chemotherapy [23]. Notably, first-line pembrolizumab monotherapy has been approved by both the FDA and the EMA in HNSCC with CPS ≥ 1 based on data from the KEYNOTE-048 trial [21, 23].
A post hoc descriptive analysis of KEYNOTE-040 was performed to determine whether CPS is a practical and suitable alternative scoring method to TPS. This analysis aimed to reconcile the scoring methods used for patients with HNSCC treated with pembrolizumab. A secondary goal was to compare scoring methods by tandem receiver operating characteristic (ROC) analyses. Results from this analysis may provide further clarity to pathologists for measuring PD-L1 expression in this patient population. Of note, KEYNOTE-040 is a large randomized trial; thus, the available data set offers the unique opportunity to explore novel techniques to simultaneously evaluate the combined predictive and prognostic effect of the PD-L1 biomarker.
Methods
Details of the KEYNOTE-040 trial have been published [22]. Briefly, KEYNOTE-040 (ClinicalTrials.gov, NCT02252042) was a multi-site, phase 3 randomized trial comparing pembrolizumab (200 mg every 3 weeks intravenously) versus SOC (investigator choice of methotrexate [40 mg/m2 per week intravenously], docetaxel [75 mg/m2 every 3 weeks intravenously], or cetuximab [400 mg/m2 loading dose followed by 250 mg/m2 per week intravenously]) for R/M HNSCC that progressed after platinum therapy. Randomization was prospectively stratified by PD-L1 TPS (≥50 vs. <50%), p16 status in the oropharynx (positive vs. negative), and Eastern Cooperative Oncology Group performance status (0 vs. 1). The primary end point was OS. Secondary end points included ORR and PFS per Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 by independent central radiologic review in the intention-to-treat population and OS and ORR and PFS by RECIST v1.1 in patients whose tumor showed PD-L1–positive expression, defined as CPS ≥ 1. The trial protocol and all amendments were approved by the appropriate IRB/IEC consistent with local policies at each center. The study was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written informed consent before enrollment.
Tumor samples were evaluated by TPS with a pre-specified cutoff of 50% at the time of enrolment to support stratification. Samples were also evaluated by CPS subsequent to patient enrolment. The nominal pre-specified CPS cutoff was 1 at the time of scoring; pathologists were instructed to generate raw scores across the reportable range. The pathologists who evaluated CPS were not necessarily the same as those who evaluated TPS; however, pathologists evaluating CPS were blinded to patients’ TPS. All samples were scored at a contract research organization accredited by the College of American Pathologists and in the same manner by which testing is performed in routine clinical practice. All testing was performed using an investigational version of PD-L1 IHC 22C3 pharmDx [20]. Reagents were those currently approved by the FDA as a companion diagnostic for pembrolizumab and CE-marked in multiple indications. Assay precision (combined precision [inter-instrument, inter-operator, inter-day, and inter-lot], intra-run, and inter-/intra-observer) and reproducibility (inter-/intra-site, inter-/intra-observer) were previously tested using HNSCC tumor samples at CPS ≥ 20 and CPS ≥ 1 [20]. Additional details on the assay as well as scoring for TPS and CPS have been described [14]. Spearman rank-order correlation was used to determine patient correlation for TPS and CPS cutoffs.
The primary goal of this post hoc analysis was to determine whether CPS 50 was an equivalent predictor to TPS 50%. For this post hoc analysis, Kaplan–Meier curves were constructed for OS and PFS based on treatment group (pembrolizumab vs. SOC). Within each treatment group, separate curves were generated for TPS (≥50 vs. <50%) and CPS (≥50 vs. <50), leading to 16 curves grouped into 4 graphs: OS in PD-L1–positive tumors, OS in PD-L1–negative tumors, PFS in PD-L1–positive tumors, and PFS in PD-L1–negative tumors.
ORR for patients receiving pembrolizumab versus SOC were tabulated separately for tumors expressing PD-L1 determined by TPS (≥50 and <50%) and by CPS (≥50 and <50). The odds ratio (OR) was calculated as the odds of response to pembrolizumab divided by the odds of response to SOC. An OR > 1 favors pembrolizumab, whereas a ratio <1 favors SOC. To assess the incremental benefit of pembrolizumab versus SOC as a function of tumor PD-L1 expression in a granular fashion, difference in ORR (∆ORR) was analyzed. Patients were divided into 12 groups based on PD-L1 expression determined from TPS and CPS. ∆ORR for patients receiving pembrolizumab versus SOC was computed within each group, and results were plotted on a column graph. Total (weighted) treatment effect (TWTE) within each group, which considers the distribution of PD-L1 expression across tumors, is the ∆ORR multiplied by the total number of patients (receiving pembrolizumab or SOC) within that group. The interpretation of TWTE provided the incremental number of patients in each group who would have benefited if all patients in the study had received pembrolizumab. The 12 PD-L1 expression groups or categories for both TPS and CPS were defined as follows: 0, 1–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, 80–89, 90–99, and 100; the lower bound of each grouping indicates a practicable cutoff for TPS and CPS.
Standard ROC curves were plotted for TPS and CPS for patients receiving pembrolizumab versus SOC. In addition, ROC tables were constructed to demonstrate the relationship between pembrolizumab and SOC at each TPS or CPS cutoff as well as for true-positive rate (TPR), false-positive rate (FPR), and Youden index (YI; TPR minus FPR). The tables also include the ∆ Youden index (ΔYI), which is the YI for pembrolizumab minus the YI for SOC:
Results
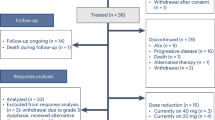
Of 495 patients randomly assigned in the intention-to-treat population, this post hoc analysis evaluated PD-L1 expression in 475 samples; 15 samples were removed because those patients were not treated and an additional 5 samples had no PD-L1 scoring. The data cutoff date for this analysis was May 15, 2017.
Good correlation was observed between TPS and CPS for each patient across the range of PD-L1 values (vs. 1); Spearman’s rho was 0.88 across all samples evaluated (Fig. 1a). Sixty-three of 475 patients (13.3%) had CPS < TPS; 39 patients were in the pembrolizumab group and 24 were in the SOC group, and 40 of them (pembrolizumab, n = 24; SOC, n = 16) had a difference ≤10. Measurement of OS based on PD-L1 using TPS ≥ 50% revealed a hazard ratio (HR) of 0.54 (95% CI, 0.36–0.82); with a median OS for pembrolizumab of 11.4 months (95%, CI 8.4–19.5) versus 6.6 months (95% CI, 4.8–10.0) with SOC (Fig. 2a). In patients with CPS ≥ 50, treatment with pembrolizumab versus SOC resulted in an HR of 0.60 (95% CI, 0.40–0.91) with a median OS of 11.6 months (95% CI, 8.2–20.1) versus 6.6 months (95% CI, 4.8–9.6), respectively (Fig. 2a). The OS curve for CPS ≥ 50 was highly congruent with that for TPS ≥ 50% in patients receiving pembrolizumab compared with those receiving SOC. In patients with TPS < 50%, HR was 0.93 (95% CI, 0.73–1.18) with a median OS of 7.0 months (95% CI, 5.8–9.1) with pembrolizumab versus 7.2 months (95% CI, 6.4–8.6) with SOC (Fig. 2b). In patients with CPS < 50, the HR was 0.89 (95% CI, 0.70–1.13) with a median OS of 7.3 months (95% CI, 5.9–9.1) with pembrolizumab versus 7.2 months (95% CI, 6.4–8.6) with SOC (Fig. 2b). Although the OS curve for CPS < 50 was highly congruent with that for TPS < 50% for patients receiving pembrolizumab, there was little separation between the pair of pembrolizumab curves and SOC curves.
OS in patients with (a) TPS ≥ 50% or CPS ≥ 50 or (b) TPS < 50% or CPS < 50. PFS in patients with (c) TPS ≥ 50% or CPS ≥ 50 or (d) TPS < 50% or CPS < 50. CPS combined positive score, OS overall survival, PD-L1 programmed death ligand 1, PFS progression-free survival, SOC standard of care, TPS tumor proportion score.
Measurement of PFS based on PD-L1 scoring method revealed an HR of 0.59 (95% CI, 0.40–0.87); median PFS was 3.5 months (95% CI, 2.1–7.6) with pembrolizumab versus 2.2 months (95% CI, 2.0–2.5) with SOC in patients with TPS ≥ 50% (Fig. 2c). For CPS ≥ 50, HR was 0.60 (95% CI 0.41–0.89) with a median PFS of 3.5 months (95% CI, 2.1–7.3) with pembrolizumab versus 2.1 months (95% CI, 2.0–2.5) with SOC (Fig. 2c). As with OS, there was high congruence between PFS curves for CPS ≥ 50 and TPS ≥ 50% in patients receiving pembrolizumab. Additionally, there was clear separation between the pair of pembrolizumab curves and SOC curves. HR for patients with TPS < 50% treated with pembrolizumab versus SOC was 1.13 (95% CI, 0.91–1.42) with a median PFS of 2.1 months (95% CI, 2.1–2.2) versus 2.6 months (95% CI, 2.1–3.6), respectively (Fig. 2d). In patients with CPS < 50, HR was 1.14 (95% CI, 0.91–1.43) with a median PFS of 2.1 months (95% CI, 2.1–2.2) with pembrolizumab versus 2.6 months (95% CI, 2.2–3.7) with SOC (Fig. 2d). Although the PFS curve for CPS < 50 was highly congruent with that for TPS < 50% for patients receiving pembrolizumab, there was little separation between the pair of pembrolizumab curves and SOC curves.
Among those with TPS ≥ 50%, 17 patients in the pembrolizumab arm and 5 in the SOC arm had confirmed or unconfirmed response, for ORRs of 26.2 and 8.5%, respectively (OR 3.83; 95% CI, 1.31–11.15) (Tables 1, 2). Among those with CPS ≥ 50, 18 patients receiving pembrolizumab and 5 receiving SOC had confirmed or unconfirmed responses, for ORRs of 28.1 and 7.7%, respectively (OR 4.70; 95%CI 1.62–13.59). For patients with TPS < 50%, 19 patients receiving pembrolizumab and 20 receiving SOC had confirmed or unconfirmed responses, for ORRs of 10.6 and 11.6%, respectively (OR 0.90; 95% CI, 0.46–1.76). For patients with CPS < 50, 18 patients receiving pembrolizumab and 20 receiving SOC had confirmed or unconfirmed responses, for ORRs of 10.0 and 12.0%, respectively (OR 0.81; 95% CI, 0.41–1.59). Taken together, treatment with pembrolizumab was favored in patients with high PD-L1 expression (TPS ≥ 50% or CPS ≥ 50), regardless of scoring method. Comparisons between pembrolizumab and SOC at various cutoffs are reported in Table 2. At low levels of PD-L1 expression, CPS maintained survival benefits similar to those of TPS.
To further analyze the incremental benefit of pembrolizumab as a function of tumor PD-L1 expression and scoring method, ∆ORR was measured. TWTE was also analyzed to determine the incremental number of patients in each group who might have benefited if all patients in the study had received pembrolizumab. For patients whose PD-L1 expression was scored using TPS, visual inspection of the graph suggests that differences begin to favor pembrolizumab at TPS 50% (Fig. 3a). TWTE suggests that pembrolizumab is favored at TPS 50%, although the TPS 0% bracket runs contrary to the overall trend (Fig. 3b). For patients whose PD-L1 expression was scored using CPS, visual inspection suggests that differences begin to favor pembrolizumab at CPS 50 (Fig. 3a). TWTE suggests that pembrolizumab is favored at CPS 50; the CPS 1-9 bracket runs contrary to the overall trend (Fig. 3b).
There were responders in both the >50 and ≤50 groups for both CPS and TPS. a The difference in response rate was analyzed based on PD-L1 scoring method using TPS and CPS. b The total (weighted) treatment effect was analyzed based on PD-L1 scoring method using TPS and CPS. CPS combined positive score, PD-L1 programmed death ligand 1, TPS tumor proportion score.
To determine the clinical utility of CPS, ROC curves (Fig. 4a) and YI plots (Fig. 4b) were generated. For the pembrolizumab group, the maximum vertical distance above the diagonal occurs at CPS 40, although the curve is relatively flat. As expected for an irrelevant biomarker, the curve for the SOC group runs mainly along the diagonal. The curve does dip below the diagonal at the lower left (corresponding to higher CPS), which is a tendency of a slightly negative prognostic indicator; the maximum vertical distance occurs at CPS 50. The YI plot emphasizes the relationship to the cutoff (Fig. 4b). Table 3 further supports the graphical findings. The maximum YI for the pembrolizumab group occurs at CPS 40. The minimum, or most negative, YI for SOC occurs at CPS 50. Thus, the maximum difference between the YIs occurs at CPS 50. Additional analysis of TPS also confirmed the cutoff at 50% (Fig. 4c, d; Table 4).
a ROC curve for CPS by treatment group. b YI plots for CPS by treatment group. c ROC curve for TPS by treatment group. d YI plots for TPS by treatment group. AUROC area under the receiver operating characteristics, CPS combined positive score, PD-L1 programmed death ligand 1, SOC standard of care, TPS tumor proportion score.
Discussion
In KEYNOTE-040, pembrolizumab provided a clinically meaningful survival benefit and favorable safety profile compared with SOC in patients with R/M HNSCC, regardless of PD-L1 status. PD-L1 is a dynamic and enriching biomarker, and there is a need to optimize the scoring method used to measure PD-L1 status in patients with R/M HNSCC. With the recent approval of pembrolizumab for the treatment of first-line R/M HNSCC for patients whose tumors express PD-L1, as measured by CPS ≥ 1 [21], and the development of 2 methods of assessing PD-L1 status, it will be useful for pathologists to understand the relationship between TPS and CPS. While acknowledging the caveats associated with post hoc analyses, the findings of this analysis from the KEYNOTE-040 trial demonstrate that CPS ≥ 50 is an equivalent predictor to TPS ≥ 50% for determining PD-L1 expression status in patients with HNSCC. This analysis further suggests that CPS may be more sensitive than TPS at lower cutoffs (CPS ≥ 1), supporting the importance of PD-L1–positive immune cells for a sensitive biomarker. Tandem analysis of the ROC curves (Fig. 4a, c) and ∆YI values (Tables 3 and 4) help account for subtle prognostic effects; the ∆YI also helps measure the advantage of pembrolizumab versus SOC over the PD-L1 expression range. At lower expression levels, CPS was more sensitive than TPS to objective response, detecting a larger fraction of responders while maintaining similar survival results (Fig. 2, Table 2). With the increasing number of anti–PD-1/–PD-L1 agents becoming available, determining tumor PD-L1 status at diagnosis may ultimately guide choice of first- or second-line therapy in some patients. To avoid an inconvenient situation for pathologists by using 2 methods of scoring in the same tumor type, this analysis demonstrates that CPS may offer a practical and suitable alternative method to TPS in patients with HNSCC.
Given that CPS measures tumor cells and immune cells expressing PD-L1, CPS ≥ 50 theoretically would capture all TPS ≥ 50% responders. Logically, there would be some concern that CPS ≥ 50 would capture too many additional non-responders such that treatment effect would be diluted. However, our post hoc re-examination of the cutoff confirmed that this was not the case. These findings are further supported by approval of CPS to measure PD-L1 expression in other tumor types. CPS is used to evaluate PD-L1 expression using multiple cutoffs to determine eligibility for treatment with pembrolizumab in patients with gastric or gastroesophageal junction adenocarcinoma (CPS ≥ 1), locally advanced or metastatic urothelial carcinoma (CPS ≥ 10), recurrent or metastatic cervical cancer (CPS ≥ 1), and recurrent locally advanced or metastatic squamous cell carcinoma of the esophagus (CPS ≥ 10) [21].
Scoring methods are typically compared in single-arm studies [24]. However, the opportunity to perform such a comparison with available control group data from KEYNOTE-040 presented new prospects and new challenges. Plotting ∆ORR (and TWTE) within each PD-L1 bracket proved to be informative and was possible because of the large sample size and adequate representation of PD-L1 values within each bracket. This type of approach can be challenging when data are limited in one or more of the pre-specified brackets, making it necessary to merge brackets. However, doing so objectively is difficult, and choice of brackets to merge may affect the outcome of the analysis.
Expansion of the familiar ROC analysis appears to be a viable solution to the limitations of the ∆ORR analysis. Separate ROC curves were plotted for pembrolizumab and SOC groups. Each individual ROC curve suggested a different cutoff, in which the maximum vertical distance from the diagonal (YI) occurred at a different CPS cutoff for each curve. Furthermore, the YI for the SOC curve by itself is not very impressive, but it does influence the ΔYI, which becomes a guide to help determine the proper cutoff. Of note, it is not possible to choose a cutoff by visual inspection or observation based on maximum vertical distance between the 2 ROC curves; a vertical line does not generally intersect both ROC curves at points corresponding to the same cutoff. Plots of the YI address this concern. In the present analysis, the cutoff chosen by the maximum ΔYI was the same cutoff suggested by the ∆ORR analysis. Thus, this “tandem ROC analysis” may be a useful technique for future applications.
Another noteworthy observation is that the ROC analysis (using maximum YI) for the pembrolizumab group produced a slightly different cutoff (CPS 40) than the ∆ORR analysis and the tandem ROC analysis (CPS 50). This is of interest primarily because it highlights one limitation of how biomarker cutoffs are typically derived. Deriving a cutoff from single-arm data assumes that the biomarker of interest has no effect on SOC. Another limitation of the typical cutoff derivation, one that even tandem ROC analysis does not solve, is the use of ORR as a clinical end point. ORR is typically used because it easily translates into dichotomized results (response vs. non-response), which is necessary for ROC analysis, and because ORR is available well before time-based end points such as PFS and OS. The truly appropriate cutoff, however, is one that predicts an advantage in OS; ORR may not always be the best surrogate end point, especially for immunotherapies.
The current findings from this post hoc analysis from KEYNOTE-040 support the use of measuring either tumor cells or a combination of tumor and immune cells in R/M HNSCC to appropriately identify PD-L1 status. These data also add to the growing body of evidence that emphasizes the importance of measuring PD-L1 in immune cells. In fact, several studies have demonstrated that the abundance of tumor-associated immune cells or tumor-infiltrating immune cells resulted in a greater likelihood of response to PD-1/PD-L1 inhibitors [25, 26]. In addition, use of CPS in the present analysis offered a robust measure to predict response to pembrolizumab in patients with R/M HNSCC receiving second-line therapy, offering a maximally sensitive biomarker. This is supported by more recent data from the KEYNOTE-048 trial, with CPS ≥ 1 selected as a companion diagnostic for the R/M HNSCC population receiving pembrolizumab monotherapy as first-line therapy [21, 27]. Taken together, these results suggest the utility of either TPS or CPS for R/M HNSCC and add to the growing body of evidence in support of its application, such as in earlier lines of treatment.
As previously mentioned, CPS seems to be more sensitive to clinical response than TPS. For example, CPS cutoffs of 1, 10, and 20 in the pembrolizumab group (Table 3 and Fig. 4a, b) demonstrate higher true-positive rates (sensitivities) and Youden indices (enrichment) than the corresponding TPS cutoffs (Table 4 and Fig. 4c, d). Furthermore, the PFS and OS advantages are maintained in a higher number of patients (Table 2). This may be of pathophysiologic significance and would be consistent with the notion that immune cell expression of PD-L1 is an earlier modulator of the adaptive immune response than tumor cell expression.
In summary, this post hoc analysis of data from the KEYNOTE-040 trial demonstrates that CPS can be a useful tool for evaluating PD-L1 expression in patients with HNSCC. This reproducible scoring method combines PD-L1 expression from tumor and immune cells to offer a single score that can identify tumors in which PD-L1 expression is driven by either cell type. Use of an FDA-approved and CE-marked diagnostic assay, PD-L1 IHC 22C3 pharmDx, and the success of CPS to determine PD-L1 expression in other tumor types further demonstrate the clinical utility of CPS in the HNSCC population as well as for earlier lines of therapy in this population, including first-line R/M HNSCC, where the impact of extending survival is greater.
References
Chen DS, Irving BA, Hodi FS. Molecular pathways: next-generation immunotherapy–inhibiting programmed death-ligand 1 and programmed death-1. Clin Cancer Res. 2012;18:6580–7.
Yang WF, Wong MCM, Thomson PJ, Li KY, Su YX. The prognostic role of PD-L1 expression for survival in head and neck squamous cell carcinoma: a systematic review and meta-analysis. Oral Oncol. 2018;86:81–90.
Caldwell C Jr., Johnson CE, Balaji VN, Balaji GA, Hammer RD, Kannan R. Identification and validation of a PD-L1 binding peptide for determination of PD-L1 expression in tumors. Sci Rep. 2017;7:13682.
Curiel TJ, Wei S, Dong H, Alvarez X, Cheng P, Mottram P, et al. Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat Med. 2003;9:562–7.
Yearly J, Gibson C, Yu N, Moon C, Murphy E, Juco J, et al. PD-L2 expression in human tumors: relevance to anti-PD-1 therapy in cancer. Clin Cancer Res. 2017;23:3158–67.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Carbognin L, Pilotto S, Milella M, Vaccaro V, Brunelli M, Calio A, et al. Differential activity of nivolumab, pembrolizumab and MPDL3280A according to the tumor expression of programmed death-ligand-1 (PD-L1): sensitivity analysis of trials in melanoma, lung and genitourinary cancers. PLoS One. 2015;10:e0130142.
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non–small-cell lung cancer. N Engl J Med. 2015;372:2018–28.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N Engl J Med. 2016;375:1823–33.
Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50.
Teixido C, Vilarino N, Reyes R, Reguart N. PD-L1 expression testing in non-small cell lung cancer. Ther Adv Med Oncol. 2018;10:1758835918763493.
Herbst RS, Baas P, Perez-Garcia JL, Felip E, Kim DW, Han JY, et al. Archival vs new tumor samples for assessing PD-L1 expression in the KEYNOTE-010 study of pembrolizumab (pembro) vs docetaxel (doce) for previously treated advanced NSCLC. J Clin Oncol. 2016;34:abstr. 3030.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65.
Kulangara K, Zhang N, Corigliano E, Guerrero L, Waldroup S, Jaiswal D, et al. Clinical utility of the combined positive score for programmed death ligand-1 expression and the approval of pembrolizumab for treatment of gastric cancer. Arch Pathol Lab Med. 2019;143:330–7.
Kim HR, Ha SJ, Hong MH, Heo SJ, Koh YW, Choi EC, et al. PD-L1 expression on immune cells, but not on tumor cells, is a favorable prognostic factor for head and neck cancer patients. Sci Rep. 2016;6:36956.
Muro K, Chung HC, Shankaran V, Geva R, Catenacci D, Gupta S, et al. Pembrolizumab for patients with PD-L1-positive advanced gastric cancer (KEYNOTE-012): a multicentre, open-label, phase 1b trial. Lancet Oncol. 2016;17:717–26.
Teng MW, Ngiow SF, Ribas A, Smyth MJ. Classifying cancers based on T-cell infiltration and PD-L1. Cancer Res. 2015;75:2139–45.
Ock CY, Keam B, Kim S, Lee JS, Kim M, Kim TM, et al. Pan-cancer immunogenomic perspective on the tumor microenvironment based on PD-L1 and CD8 T-cell infiltration. Clin Cancer Res. 2016;22:2261–70.
Kulangara K, Hanks DA, Waldroup S, Peltz L, Shah S, Roach C, et al. Development of the combined positive score (CPS) for the evaluation of PD-L1 in solid tumors with the immunohistochemistry assay PD-L1 IHC 22C3 pharmDx. J Clin Oncol. 2017;35:e14589.
PD-L1 IHC 22C3 pharmDx 50 tests for use with Autostainer Link 48. Carpinteria, CA: Dako North America, Inc; 2019. p. 37.
KEYTRUDA® (pembrolizumab) for injection, for intravenous use. Merck Sharp & Dohme Corp., Whitehouse Station, NJ, USA. 6/2020.
Cohen EEW, Soulieres D, Le Tourneau C, Dinis J, Licitra L, Ahn MJ, et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study. Lancet. 2019;393:156–67.
Keytruda (pembrolizumab) 50 mg powder for concentrate for solution for infusion (summary of product characteristics). Hoddesdon, UK: Merck Sharp & Dohme Limited; August 2020.
Dolled-Filhart M, Roach C, Toland G, Stanforth D, Jansson M, Lubiniecki GM, et al. Development of a companion diagnostic for pembrolizumab in non-small cell lung cancer using immunohistochemistry for programmed death ligand-1. Arch Pathol Lab Med. 2016;140:1243–49.
Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563–7.
Ferris RL, Blumenschein G, Harrington K, Fayette J, Guigay J, Colevas AD, et al. Tumor-associated immune cell PD-L1 expression and peripheral immune profiling: analyses from CheckMate 141. Cancer Res. 2017;77:CT021.
Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394:1915–28.
Acknowledgements
The authors thank the patients and their families and all investigators and site personnel. Medical writing and/or editorial assistance was provided by Holly C. Cappelli, PhD, CMPP, and Dana Francis, PhD, of ApotheCom (Yardley, PA, USA). This assistance was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. This study was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KE is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and a stockholder in Merck & Co., Inc., Kenilworth, NJ, USA; holds stock in Bayer AG and Johnson & Johnson; and has a patent for a Combined Positive Score pending. His spouse is an employee of and a stockholder in Bristol Myers Squibb. LH is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. DA-G is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. TB is a former employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. EEWC has received personal fees from ALX Oncology, Ascendis, Bayer, BiolineRx, BMS, Debio, Dynavax, MSD, Merck, Regeneron, and Sanofi. KH has received personal fees and grants paid to the research institution from MSD, AstraZeneca, and Boehringer-Ingelheim; and has received personal fees paid to his research institution from BMS, Merck-Serono, and Pfizer. DS has received grants for his institution from MSD; and has received fees for serving on advisory boards from MSD. CL has received personal fees and non-financial support from MSD, BMS, Amgen, Merck-Serono, Roche, Rakuten, AstraZeneca, Nanobiotix, and GSK. LL has received personal fees for consultancy/advisory and/or lectures from AstraZeneca, Bayer, BMS, Boehringer-Ingelheim, Debiopharm, Eisai, Merck-Serono, MSD, Novartis, Roche, Sobi, and Ipsen; for expert opinion/advisory boards for GSK, Health & Life srl, Doxa Pharma srl; and for public speaking/teaching at medical meetings from Immuno-Oncology Hub, Incyte Biosciences Italy srl, Amgen, and Nanobiotix SA; and has received grants for her institutions for clinical studies and research from Eisai, Merck-Serono, MSD, Novartis, and Roche. BB has received grants and personal fees from Merck. RS is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Emancipator, K., Huang, L., Aurora-Garg, D. et al. Comparing programmed death ligand 1 scores for predicting pembrolizumab efficacy in head and neck cancer. Mod Pathol 34, 532–541 (2021). https://doi.org/10.1038/s41379-020-00710-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00710-9
This article is cited by
-
Immunotherapy: The Fourth Domain in Oral Cancer Therapeutics
Indian Journal of Otolaryngology and Head & Neck Surgery (2024)
-
Significance of CD103+ tissue-resident memory T cells for predicting the effectiveness of immune checkpoint inhibitors in esophageal cancer
BMC Cancer (2023)
-
Programmed death-ligand 1 expression and overall survival in Thai patients with gastric cancer
Scientific Reports (2023)
-
A systematic review and meta-analysis of prognostic indicators in patients with head and neck malignancy treated with immune checkpoint inhibitors
Journal of Cancer Research and Clinical Oncology (2023)
-
Immunotherapy in HPV-Related Oropharyngeal Cancers
Current Treatment Options in Oncology (2023)