Abstract
Histologic features of idiopathic noncirrhotic portal hypertension (INCPH), loosely termed as obliterative portal venopathy (OPV), are heterogenous, often subtle, and overlap with other entities. To this date, no consensus histopathologic diagnostic criteria have been established for INCPH. For these reasons, rendering a reproducible consensus histologic diagnosis of OPV on a liver biopsy may often be challenging even for experienced hepatopathologists. We report herein a two-phase interobserver agreement study on the diagnosis of OPV and assessed the relative value of histologic features in 104 liver biopsies in distinguishing between INCPH and non-INCPH with the goal to obtain a consensus on specific practical diagnostic criteria. Six hepatopathologists blinded to clinical information and original pathologic diagnosis reviewed internet-based case study sets with high-resolution whole-slide images. The initial interobserver agreement on OPV was expectedly low, but significantly improved (moderate agreement in most categories) upon adopting a consensus view recognizing portal vein sclerosis as the only strong independent histologic predictor for INCPH, and that contrary to the conventional view, aberrant portal/periportal vessels does not significantly contribute to the positive assignment of OPV status. We propose a three-tiered classification with diagnostic criteria to facilitate the histologic assignment of OPV status for the evaluation of INCPH. Furthermore, we have validated the performance of the proposed criteria either based on histology alone or coupled with clinicopathologic correlation. This classification may aid in practical histologic assessment of liver biopsies with or without portal hypertension and help to improve diagnostic consistency and accuracy.
Similar content being viewed by others
Introduction
A liver biopsy is the key component of the diagnostic workup of an individual with unexplained portal hypertension (PH) to exclude cirrhosis as the cause and to establish an etiology of noncirrhotic portal hypertension (NCPH) [1, 2]. Common causes of NCPH include extrahepatic portal vein or splenic vein obstruction, chronic hepatic parenchymal diseases, and post hepatic venous obstruction such as Budd–Chiari syndrome [3, 4]. Idiopathic noncirrhotic portal hypertension (INCPH), defined as PH without a known cause and without portal vein thrombosis, is a nebulous clinicopathologic entity in which liver biopsy may be helpful, especially in excluding cirrhosis [1]. Historically, several terms have been used to refer to the histologic changes in INCPH, including hepatoportal sclerosis [5], noncirrhotic portal fibrosis [6], nodular regenerative hyperplasia (NRH) [7], obliterative portal venopathy (OPV) [8], and porto-sinusoidal vascular disease [9]. We adopted the term OPV for the purpose of this study.
The interpretation of liver biopsies in INCPH is challenging, as the histologic features that reportedly characterize OPV in patients with INCPH are heterogeneous, frequently subtle with a patchy distribution, vary with disease stage, and appear to exist not uncommonly in other conditions with or without PH. A number of studies have attempted to characterize these histologic features in patients with INCPH. They are mostly based on autopsy, explant livers with end-stage diseases, or biopsies with relatively small number of cases, while lacking adequate controls for comparison and based on histologic interpretation by only one or two pathologists potentially biased by knowledge of clinical and pathologic information of the cases [10,11,12,13,14,15,16,17,18,19,20,21]. No consensus histologic diagnostic criteria for OPV or INCPH has been established. While a broad spectrum of histologic features has been described, no single or combination of features are considered pathognomonic for diagnosis. Abnormalities of the portal vein branches are generally regarded as the characteristic change, which encompasses variable degree of sclerosis, luminal narrowing, obliteration, increase in number, dilation, and herniation into the lobule [4, 5, 22,23,24,25,26]. On a biopsy, however, these features are often subtle and patchy. A diagnosis of OPV for patients with INCPH may be easily missed when the pathologist is not sufficiently familiar with the entity, or the clinical information of PH is not available to the pathologist. In practice, a history of PH may often serve as the only clue for the pathologist to search for subtle histologic features of OPV on biopsies. On the other hand, the absence of PH does not exclude OPV, as studies showed up to 35% of cases with OPV lack PH [13] and OPV can be found in up to ~20% of patients without PH [27], rendering the diagnosis of OPV on biopsies more challenging.
In this study, we carried out a two-phase analysis of the interobserver agreement for reporting the histologic diagnosis of OPV on liver biopsies among six pathologists with varying degree of experience and expertise in hepatobiliary pathology. We sought to answer the following questions: (1) what (or how low) is the interobserver agreement for diagnosing OPV and recognizing related individual histologic features; (2) which histologic feature(s), alone or in combination, are key predictor(s) for INCPH; (3) can interobserver agreement for reporting OPV on liver biopsies be improved; (4) can we establish practical histologic diagnostic criteria that would be reproducible among observers. We attempted to answer these questions by using a digital library of liver biopsies consisting of confirmed cases of INCPH, clinicopathologic mimics of INCPH with PH and/or OPV, and controls lacking PH with minimal or mild histologic changes.
Materials and methods
Case selection and construction of digital case study sets
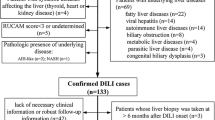
This study was approved by the Institutional Review Board at Vanderbilt University Medical Center. Fifty-two liver biopsies with original pathologic diagnosis of OPV were identified by searching the Vanderbilt University Medical Center pathology database and the electronic medical record. These included 41 and 11 biopsies with original pathologic assignment of “consistent with OPV” and “possible OPV” between 2000 and 2018, respectively. Case inclusion criteria included needle core (≥1 cm in length and contain ≥ 5 portal tracts) or wedge biopsies with both hematoxylin and eosin (H&E) and either trichrome or reticulin stains for review, and the availability of clinical information for clinicopathologic correlation and follow-up. A total of 34 INCPH biopsies were confirmed using clinical follow-up information (see details in “Data collection and final clinicopathologic diagnosis”). The remaining 18 cases were classified as non-INCPH because plausible etiology for PH was identified in eight and no PH was detected in ten during follow-up. Fifty-two age-matched liver biopsies from patients without history of PH between 2016 and 2018 were selected as non-INCPH controls. The original pathologic assignment of these 52 biopsies included no or minimal changes in 35, mild changes (mild inflammation, mild macrovesicular steatosis, and/or mild fibrosis) in 16, and steatohepatitis in 1 (Table 1). To compare with the INCPH group (n = 34), two non-INCPH control groups were used for analysis: Control 1 (n = 70) consisting of 18 clinicopathologic mimics with original pathologic assignment of OPV and 52 with no more than mild pathologic changes, and Control 2 (n = 52) consisting of only the latter. All slides were scanned into high-resolution whole-slide images using a Leica SCN400 Slide Scanner (400× Brightfield scanning). Digital images for all 104 biopsies were pooled together and randomized twice by computer programming to generate two separate digital study sets (Set A and Set B created after each randomization and comprised of the same 104 whole-slide digital images). In each study set, every digital file was labeled with a unique computer-generated code. There were five wedge biopsies in the INCPH and four in the non-INCPH samples to minimize the bias perceived by pathologists toward the type of biopsy. Similarly, a comparable number of reticulin stains were included in each group to minimize bias toward the type of special stains. The non-INCPH cases in control group 2 (n = 52) had overall low percentage of macrovesicular steatosis (<5% in 42, 5% in 8, and 10% in 2 biopsies) to reduce the bias toward the degree of steatosis, as INCPH biopsies generally exhibit no or minimal degree (<5%) of macrovesicular steatosis. The two phases of interobserver study were separated by 11 months, which further reduced the effect of participants’ memory of individual biopsies on their observations.
Data collection and final clinicopathologic diagnosis
Baseline data including demographics, medical history, laboratory, and radiographic studies were collected. A final diagnosis based on clinical, radiographic, and pathologic findings at diagnosis and follow-up was made in each biopsy. In this study, the criteria for the diagnosis of INCPH is defined as a combination of (1) clinical evidence of PH, (2) no identifiable cause for PH, (3) no hepatic or portal vein obstruction at the time of diagnosis (portal vein thrombosis may occur late in the disease course as a result or complication of INCPH, however), and (4) lack of cirrhosis on liver biopsy [1]. The diagnosis of PH was based on clinical manifestations (varices, splenomegaly with or without thrombocytopenia, and ascites) in 40 (95%, 40/42) and elevated hepatic venous pressure gradient in two cases (5%, 2/42). Esophageal varices were present in 32 cases.
Histologic study
In each biopsy, H&E and Masson-trichrome-stained slides were examined. In samples when Masson-trichrome-stained slides were not available, reticulin stains were used. Using the digital sets, the pathologists were blinded to clinical information, independently completed an evaluation of histologic features related to INCPH, and provided an overall assignment of OPV status (positive, indeterminate, or negative) for each biopsy. Clinical information was withheld because we believed that it may bias the pathologists. For the purpose of the study, four groups of histologic features were scored (positive or negative for each group):
-
(1)
We used the term “portal vein sclerosis” to include a spectrum of histologic features ranging from reduced luminal caliber to complete obliteration or even disappearance of portal vein branches. These changes are often associated with thickened, sometimes arterialized walls, and are thought by many to be the initial lesions in INCPH.
-
(2)
Aberrant portal/periportal vessels include herniated portal vein(s) (one or multiple thin-walled vessels directly extend into and abut the periportal parenchyma without any intervening connective tissue separating the vein wall from the lobule), paraportal shunt formation (characterized by aberrant venous structures, frequently with marked dilation and irregular contours, surrounding the portal tract in which the native portal vein is often absent), and the so-called pseudo-angiomatosis (characterized by multiple thin-walled vessels within the portal tract, creating a sieve-like appearance). As paraportal shunt formation and pseudo-angiomatosis frequently co-existed with herniated portal veins and rarely appeared as isolated findings, we considered that these histologic features may represent a spectrum of abnormally dilated portal vein branches (as opposed to portal vein sclerosis with diminished lumens) associated with abnormal shape, number, and/or location.
-
(3)
Increased portal fibrous tissue was characterized by expansion of portal tract by stromal fibrosis, often rendering a rounded or nodular appearance.
-
(4)
NRH was characterized by distinct hepatocellular nodule(s) less than 3 mm in diameter consisting of central enlarged hepatocytes and/or thickened liver cell plates, surrounded by a rim of smaller hepatocytes and/or thinner liver cell plates [28].
Consensus from more than half of the participating pathologists was used to determine the pathologic assignment of OPV status and whether any of the four groups of histologic features were positive in each biopsy. After the first-phase of the study, one author (JL) scored the total number of portal tracts, the number of portal tracts showing portal vein sclerosis, and the number of portal tracts showing aberrant portal/periportal vessels in each biopsy, generating an initial distribution analysis of histologic features and a cut-off value for portal vein sclerosis to guide the second phase of the study. Two additional authors (WJH and HC) independently repeated the scoring after the second phase of the study. A final distribution analysis and cut-off point were derived by combining the scoring data from three authors (JL, WJH, and HC). All authors were blinded to clinical and pathologic information during scoring.
Interobserver agreement study
Six subspecialist pathologists with experience in hepatobiliary pathology independently reviewed the study Set A online and scored specific histologic features that contributed to the histopathologic diagnosis of OPV. All participants were familiar with these histologic features before the onset of the study. All participants were aware that both INCPH and non-INCPH biopsies were included in the study sets.
After independent examination of the study Set A (first phase), all participants attended two consensus meetings to review the interobserver agreement analysis data and develop practical diagnostic criteria for OPV. Portal vein sclerosis as a significant independent predictor for INCPH and the poor performance of aberrant portal/periportal vessels as a histologic predictor were noted to all participants. A second phase of study was conducted with five of the six original participating pathologists evaluating the study Set B. Receiver operating characteristics (ROCs) curves for the performance of portal vein sclerosis alone or in combination with aberrant portal/periportal vessels in diagnosing INCPH were generated. An optimal threshold for the percentage of portal tracts with portal vein sclerosis was derived. We subsequently obtained a consensus and proposed practical classification criteria for OPV in order to assess INCPH on biopsies.
Statistical analysis
Interobserver concordance was quantified using Fleiss’ κ statistic, with interpretations as previously described [29], which is, ≤0.00, poor agreement; 0.01–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.00, almost perfect agreement. For comparisons between individual pathologists and the rest of the group, we used a weighted κ statistics [30]. When all pathologists were evaluated together, we rated agreement using the method of Landis and Koch [29]. Univariate and multivariable logistic regression were used to assess the relationship between histologic features and INCPH. Sensitivity, specificity, and positive and negative predictive values were calculated with histologic assignment of OPV as the test condition and the clinical diagnosis (INCPH or non-INCPH) considered as the true disease state of each patient. Diagnostic accuracy was calculated as the sum of true positive and true negative biopsies over the total number of biopsies.
Results
Interobserver agreement study
The first phase of the study demonstrated the overall interobserver agreement was only slight (κ = 0.15), while interobserver agreement on positive, indeterminate, and negative for OPV was fair (κ = 0.21), poor (κ < 0), and slight (κ = 0.19), respectively (Table 2). Agreement between individual pathologists and the group ranged from 71% (κ = 0.40, fair) to 59% (κ = 0.18, slight) (Table 3). The overall interobserver agreement for histologic features were fair (κ = 0.25) for portal vein sclerosis, slight (κ = 0.15) for aberrant portal/periportal vessels, fair (κ = 0.30) for increase in portal fibrous tissue, and slight (κ = 0.17) for NRH. While portal vein sclerosis (odds ratio [OR] = 13.22; 95% confidence interval [CI]: 4.33, 40.36, p < 0.001, Fig. 1a–e), increase in portal fibrous tissue (OR = 7.43; 95% CI: 2.68, 20.56, p < 0.001) and NRH (OR = 24.60; 95% CI: 1.33, 456.08, p = 0.032, Fig. 1f), but not aberrant portal/periportal veins (OR = 1.36; 95% CI: 0.56, 3.30, p = 0.499, Fig. 2), were found to be significant predictors of OPV by univariate logistic regression analysis, only portal vein sclerosis remained significant by multivariate analysis (OR = 7.32; 95% CI: 1.45, 36.78, p = 0.016).
a A portal tract with diminished portal vein and increase in portal stromal fibrous tissue. Note that a markedly dilated thin-walled vessel is present in the periportal area directly abutting the liver parenchyma. b A fibrotic portal tract with a nodular contour and complete obliteration of portal vein. Note that several minute, slit-like vascular channels and a scant chronic inflammatory infiltrate are present within the portal tract. c Two closely approximated portal tracts with nodular contours and diminished portal veins, suggestive of possible parenchymal atrophy. d A rounded portal tract expanded by dense stromal fibrosis (Masson trichrome). Note that a normal, centrally located portal vein is absent. A venous structure with a caliber comparable to the portal arterioles is present at the periphery of the portal tract. e A nodular, large-sized portal tract with stromal fibrosis and muscularized portal venous wall (Masson trichrome). A few thin-walled vessels were present. Only a portion of this portal tract was sampled in the biopsy. f Nodular regenerative hyperplasia with central widened hepatocyte plates surrounded by peripheral atrophic hepatocyte plates and compressed sinusoidal spaces (reticulin stain).
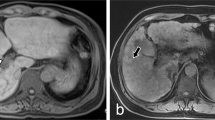
a Liver biopsy from a patient with abnormal liver function tests and no history of PH showing multiple herniated venous structures. A few thin-walled vessels are present (to the upper right of the portal tract), creating a sieve-like appearance. b Liver biopsy from another non-INCPH patient showing paraportal shunt formation. c A portal tract with a herniated venous structure without any intervening connective tissue separating the herniated vein wall from the lobule. We note that the portal tracts containing herniated venous structures in non-INCPH biopsies tend to have no or minimal portal fibrosis and rarely exhibit rounded contours.
To explore the underlying causes of low interobserver agreement for individual histologic features and the overall assignment of OPV status, a small subset of cases (n = 20, 19%) was re-assessed by all participants at consensus sessions with emphasis on developing diagnostic criteria reproducible among pathologists. The resulting consensus recognized that: (1) aberrant portal/periportal vessels were frequently present in non-INCPH biopsies and should not be regarded as a reliable predictor of INCPH; (2) portal vein sclerosis combined with increase in portal fibrous tissue served as key diagnostic requirement for OPV and strong predictors for INCPH; (3) recognition of NRH on core needle biopsies was challenging, but the presence of NRH strongly correlated with INCPH. The consensus was further supported by the distribution analysis of the percentage of portal tracts showing individual histologic features (Figs. 3a, b), demonstrating significant association of portal vein sclerosis, but not aberrant portal/periportal vessels, with INCPH. Based on the initial analysis (scored by one pathologist), an optimal cut-off point of 14% (corresponding to ≥1 per 7 portal tracts) for portal vein sclerosis alone was derived by ROC analysis with good performance (area under the curve = 0.8664).
Distribution of the percentage of portal tracts (PTs) with features of portal vein sclerosis (PVS) (a) or aberrant portal/periportal vessels (APV) (b) in idiopathic noncirrhotic portal hypertension (INCPH) and non-INCPH biopsies, showing significant association of PVS, but not APV, with INCPH. Box-and-whisker plots overlay the data. The central box represents the values from the lower to upper quartile (25th to 75th percentile). The middle line represents the median. The vertical line extends from the minimum to the maximum value, excluding outside and far out values which are displayed as separate points. Univariate logistic regression was performed to calculate p values. Receiver operating characteristic analysis was used to evaluate the performance of the percentage of PTs with PVS alone (c) or combined with the percentage of PTs with APV (d) in discriminating INCPH from non-INCPH. The former demonstrated a good performance (area under the curve = 0.8880) with an optimal cut-off point (maximal sum of sensitivity and specificity) of 8.3% when control group 2 was used, while addition of APV did not improve the performance. The performance was comparable when control group 1 was used (area under the curve = 0.8151 for PVS alone). Three pathologists independently performed the scoring of individual biopsies blinded to clinical and pathologic information.
The updated consensus was subjected to validation by five pathologists during the second phase of interobserver agreement study, resulting in a significantly improved overall interobserver agreement (κ = 0.35, fair) compared to previous (κ = 0.15, slight). Agreement on positive, indeterminate, and negative for OPV was moderate (κ=0.43), slight (κ = 0.10), and fair (κ = 0.37), respectively (Table 2). Agreement between individual pathologists and the group also significantly improved, achieving a moderate level of agreement in all five pathologists, ranging from 79% (κ = 0.55) to 72% (κ = 0.42) (Table 3).
Next, we evaluated the performance of using the updated consensus in distinguishing INCPH from non-INCPH biopsies including mimics. Portal vein sclerosis (76.5%) was the most prevalent histologic feature in biopsies from patients with INCPH, while NRH (5.9%) was the least (Table 4). By univariate logistic regression analysis, portal vein sclerosis (OR = 8.13; 95% CI: 3.15, 20.95, p < 0.001) and increase in portal fibrous tissue (OR = 3.93; 95% CI: 1.60, 9.64, p = 0.003) were significant predictors of INCPH compared to control group 1. However, only portal vein sclerosis remained significant by multivariate analysis (OR = 12.89; 95% CI: 2.42, 68.59, p = 0.003). The same pattern was observed when control group 2 was used for analysis (Table 5). Of note, among the 26 INCPH cases with portal vein sclerosis, 24 (92.3%) were also positive for increase in portal fibrous tissue. For pathologic assignment of OPV status, a slight majority of INCPH cases (56%) were classified by consensus as positive, 6% as indeterminate, 26% as negative, and 12% with no consensus. For comparison, majority of the non-INCPH controls (73% and 81% for control 1 and 2, respectively) were classified as negative, while a significant small subset (19% and 12% for control 1 and 2, respectively) was deemed positive by consensus (Table 6). To determine the accuracy of liver biopsy in reaching a confident assignment of OPV status for assessment of INCPH, only biopsies receiving a consensus diagnosis of either positive or negative were used. The sensitivity of liver biopsy for a diagnosis of INCPH was 67.9% (95% CI: 49.3-82.1%), the specificity was 79.7% (95% CI: 68.3–87.7%), and the diagnostic accuracy was 76.1% (95% CI: 66.4–83.6%).
Proposal of histologic criteria for OPV to assess INCPH
All participants agreed on the general concept that no single histologic feature was specific for OPV and that the findings may be subtle and focal on a biopsy. Regarding individual histologic features, all participants recognized that portal vein sclerosis was significantly associated with INCPH and almost always accompanied by increase in portal fibrous tissue, that aberrant portal/periportal vessels was a poor predictor for INCPH, either alone or in combination with portal vein sclerosis, and that NRH was rare but strongly associated with INCPH. Taking these into consideration, we establish the consensus diagnostic criteria for OPV to assess INCPH on biopsies, as shown in Table 7. We defined three pathologic diagnostic categories (consistent with, indeterminate, and not consistent with OPV) and outlined histopathologic features for each group. A final cut-off point of 8.3% (corresponding to ≥1 per 12 portal tracts) for portal tracts exhibiting portal vein sclerosis was determined by ROC analysis scored by 3 pathologists (Fig. 3c), while addition of aberrant portal/periportal vessels did not significantly improve the performance (Fig. 3d).
To facilitate the integration of pathologic diagnostic category with clinical information to assess INCPH in practice, we summarized in Table 8 the correlations for each OPV category with clinical diagnosis based on the presence or absence of PH and, if present, with or without probable underlying etiology. Of note, as emerging evidence suggests that some patients with features of OPV on biopsies may not show PH until years later [2, 27], we cautioned the interpretation of “consistent with OPV” category when PH is lacking. While the clinical criteria for INCPH is not met, the possibility of “subclinical” INCPH remains.
Finally, we further assessed the performance of the proposed diagnostic criteria in providing clinicopathologic correlations in this cohort using the consensus regarding individual histologic features in each biopsy (Table 9). Among the 34 INCPH cases, 24 (71%) were classified as “consistent” and 10 (29%) as “not consistent with OPV”. This differed from the subjective assignment of OPV status (positive, indeterminate, and negative) during interobserver agreement study in that the latter was concluded without specific criteria. When clinical diagnosis was incorporated, this resulted in 71% of INCPH cases being classified as “positive” and 29% as “cannot exclude INCPH”. Among the 70 non-INCPH controls, 19 (27%), 6 (9%) and 45 (64%) were classified as “consistent with”, “indeterminate”, and “not consistent with OPV”, respectively. Upon clinicopathologic correlation, 51 (73%) non-INCPH controls were classified as “negative INCPH”, 14 (20%) as “possible subclinical INCPH”, and 5 (7%) as “NCPH with OPV features”.
Discussion
In this study, we examined the interobserver agreement on the pathologic diagnosis of OPV and sought to identify which histologic features in liver biopsies best characterize INCPH and optimally discriminate between INCPH and non-INCPH. As consensus diagnostic criteria for OPV has not been established in the literature, we used well-characterized histologic features in patients with INCPH described in previous studies as tentative guidelines. After the first phase of the interobserver agreement study which demonstrated expectant low concordance, we analyzed the agreement on individual histologic features and their performance on correlating with OPV status, which collectively resulted in an adapted consensus for classifying OPV status. This consensus view recognized extensive variability in the severity of the histologic changes in INCPH. For example, portal vein sclerosis, generally regarded as a main feature of OPV, was considered absent in as many as 23.5% of INCPH cases. Features seen in INCPH also overlapped with non-INCPH controls, as 28.6% of the latter exhibited portal vein sclerosis, and aberrant portal/periportal vessels were present in 54.3%. However, we did find that portal vein sclerosis was the only strong independent histologic predictor of INCPH. The utility of the new consensus view was validated by the second phase of the interobserver agreement study with significant improvement in all agreement categories, prompting us to further establish practical diagnostic criteria for OPV on liver biopsies intended for evaluation of INCPH. The key components in our proposed three-tiered classification concern the absence of both cirrhosis and conditions known to cause PH, as well as the presence of portal vein sclerosis or NRH. Increase in portal fibrous tissue almost always accompanied portal vein sclerosis. A major deviation from the conventional view was that aberrant portal/periportal vessels does not significantly contribute to the assignment of OPV status.
The cause for low interobserver agreement during the first phase of the study was likely multifactorial. The rarity of INCPH cases in the United States, lack of well-established diagnostic criteria for OPV, and varied training background and experience among participants may have contributed to the initial low interobserver agreement. In addition, all participants were blinded to clinical information in the current study while the status of PH was almost always available to pathologists during routine sign-out. The knowledge of PH served as a critical, frequently the sole clue to searching for subtle histologic changes in liver biopsies. In fact, the study was designed to minimize any possible source of bias and facilitate participants to make judgment based only on histology. Therefore, the low interobserver agreement may stem from habitual dependence on clinical information and the lack of objective morphologic anchor points for the diagnosis of OPV in our routine practice. Lastly, the interobserver agreement of “indeterminate” (κ < 0) was much lower than those of “positive” (κ = 0.21) and “negative” for OPV (κ = 0.19), contributing to a low overall agreement. This pattern remained during the second phase of the study (κ = 0.10 for indeterminate, 0.43 for positive, and 0.37 for negative). Although indeterminate or intermediate groups of three-tiered systems generally tend to suffer from low levels of agreement, we opted to include the indeterminate category rather than using a two-tiered system (positive or negative) in order to account for a small subset of biopsies with subtle changes that are difficult to determine as positive or negative in practice.
After adopting the new consensus view on the predictability of individual histologic features for INCPH, the interobserver agreement in all categories had improved significantly. In particular, the agreement between individual pathologist and the group exhibited uniform improvement (from one pathologist with slight and four with fair in the first phase to all five with moderate agreement in the second). These results were encouraging as it was the first time for all participants to apply the updated consensus. Although no additional interobserver agreement analysis was carried out after we further established the diagnostic criteria, routine usage of the proposed criteria is expected to further improve the diagnostic agreement.
If omitting cases from the “indeterminate” category, we estimated the diagnostic accuracy of biopsy blinded to clinical information to be 76.1%, and the sensitivity and specificity for a diagnosis of INCPH were 67.9% and 79.7%, respectively. We believe this low diagnostic accuracy is reflective of the subtle nature and extensive variability of the histologic features associated with INCPH. Also, we observed that most of the well-described histologic features of INCPH substantially overlap with non-INCPH in our study. The low sensitivity may also have resulted from the withholding of clinical information. For example, nine clinically confirmed INCPH cases (26%) were considered by consensus to be negative for OPV, and 2 (6%) were thought to be indeterminate, while an original pathologic diagnosis of OPV was made prior to the study for all 11 cases. In practice, when clinical information of PH or suspicion of INCPH is available to pathologists, a positive assignment of OPV appears to be more readily rendered, even though the histologic findings in the biopsies were, at best, subtle. These nine cases were characterized by lack of portal vein sclerosis in eight cases, lack of aberrant portal/periportal vessels in eight, and the absence of NRH in all nine. One case demonstrated both portal vein sclerosis and aberrant portal/periportal vessels associated with advanced portal fibrosis, the latter finding deterring most participants from assigning this case to the positive category.
Among the 70 non-INCPH controls, 13 (19%) were thought by consensus during interobserver agreement study to be positive for OPV, and 5 (7%) were left without consensus assignment. If the proposed criteria were applied, 19 (27%) would be classified as consistent with OPV. All of these biopsies were characterized by portal vein sclerosis associated with increase in portal fibrous tissue. Five cases were clinically confirmed to have PH with plausible underlying etiology, highlighting the overlap of OPV features in INCPH with those in NCPH with known etiology as well as the challenges of separating INCPH from NCPH by histology alone. Interestingly, 14 biopsies (20%) without evidence of PH would be classified as consistent with OPV. These include five with original histologic diagnosis of OPV, and nine with original histologic diagnosis of minimal to mild steatosis, inflammation, and/or fibrosis. The follow-up time for these 14 patients ranged from 2 months to 11 years (median = 2 years) and no evidence of PH was found during follow-up. These findings were similar to previous studies in which OPV were found in approximately 20–30% of patients without PH [20, 27]. Whether the findings of histologic features of OPV in patients without PH represent a preclinical state of INCPH requires further study. A significantly longer follow-up period may be necessary for this purpose, since another study suggested that only 64% of patients with OPV initially presented with PH, but subsequently increased to 88% after a mean follow-up of 8.6 years [13].
Our study reinforced the view that it is challenging, and probably impractical, to use individual or combination of histologic features alone for reliable prediction of INCPH [2, 3, 10, 18, 25, 26]. Using the proposed criteria, we could only predict 71% of INCPH cases while assigning 27% of non-INCPH controls as consistent with OPV based on histology alone. However, when clinical information was incorporated, the 29% of histologically negative INCPH cases would be classified as “cannot exclude INCPH”; thus, a repeat biopsy and/or close follow-up would be triggered and the clinical management would not be compromised. The 27% histologically positive non-INCPH biopsies would also be appropriately classified as “possible subclinical INCPH” for 20% and “NCPH with OPV features” for 7%. OPV without PH has been increasingly recognized as a potential cause of unexplained abnormal liver function tests and may precede INCPH [24, 27].
In summary, this interobserver agreement study showed initial low agreement on OPV was significantly improved upon recognition of portal vein sclerosis as the only strong independent histologic predictor for INCPH, and a cut-off point of ≥1 per 12 portal tracts was optimal. Histologic features in INCPH cases exhibited wide variation in severity and overlapped with non-INCPH biopsies. We proposed a three-tiered classification with diagnostic criteria to facilitate the histologic assignment of OPV status. This system may aid in practical histologic assessment of liver biopsies with or without PH and help to improve diagnostic consistency and accuracy.
References
Schouten JN, Garcia-Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011;54:1071–81.
Hernandez-Gea V, Baiges A, Turon F, Garcia-Pagan JC. Idiopathic portal hypertension. Hepatology. 2018;68:2413–23.
Khanna R, Sarin SK. Non-cirrhotic portal hypertension—diagnosis and management. J Hepatol. 2014;60:421–41.
Fiel MI, Schiano TD. Idiopathic noncirrhotic portal hypertension. Semin Diagn Pathol. 2019;36:395–403.
Bioulac-Sage P, Le Bail B, Bernard PH, Balabaud C. Hepatoportal sclerosis. Semin Liver Dis. 1995;15:329–39.
Sama SK, Bhargava S, Nath NG, Talwar JR, Nayak NC, Tandon BN, et al. Noncirrhotic portal fibrosis. Am J Med. 1971;51:160–9.
Steiner PE. Nodular regenerative hyperplasia of the liver. Am J Pathol. 1959;35:943–53.
Nayak NC, Ramalingaswami V. Obliterative portal venopathy of the liver. Associated with so-called idiopathic portal hypertension or tropical splenomegaly. Arch Pathol. 1969;87:359–69.
De Gottardi A, Rautou PE, Schouten J, Rubbia-Brandt L, Leebeek F, Trebicka J, et al. Porto-sinusoidal vascular disease: proposal and description of a novel entity. Lancet Gastroenterol Hepatol. 2019;4:399–411.
Verheij J, Schouten JN, Komuta M, Nevens F, Hansen BE, Janssen HL, et al. Histological features in western patients with idiopathic non-cirrhotic portal hypertension. Histopathology. 2013;62:1083–91.
Nayak NC, Jain D, Saigal S, Soin AS. Non-cirrhotic portal fibrosis: one disease with many names? An analysis from morphological study of native explant livers with end stage chronic liver disease. J Clin Pathol. 2011;64:592–8.
Hillaire S, Bonte E, Denninger MH, Casadevall N, Cadranel JF, Lebrec D, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension in the West: a re-evaluation in 28 patients. Gut. 2002;51:275–80.
Cazals-Hatem D, Hillaire S, Rudler M, Plessier A, Paradis V, Condat B, et al. Obliterative portal venopathy: portal hypertension is not always present at diagnosis. J Hepatol. 2011;54:455–61.
Chougule A, Rastogi A, Maiwall R, Bihari C, Sood V, Sarin SK. Spectrum of histopathological changes in patients with non-cirrhotic portal fibrosis. Hepatol Int. 2018;12:158–66.
Ludwig J, Hashimoto E, Obata H, Baldus WP. Idiopathic portal hypertension; a histopathological study of 26 Japanese cases. Histopathology. 1993;22:227–34.
Isabel Fiel M, Thung SN, Hytiroglou P, Emre S, Schiano TD. Liver failure and need for liver transplantation in patients with advanced hepatoportal sclerosis. Am J Surg Pathol. 2007;31:607–14.
Franchi-Abella S, Fabre M, Mselati E, De Marsillac ME, Bayari M, Pariente D, et al. Obliterative portal venopathy: a study of 48 children. J Pediatr. 2014;165:190–3.e2.
Nakanuma Y, Hoso M, Sasaki M, Terada T, Katayanagi K, Nonomura A, et al. Histopathology of the liver in non-cirrhotic portal hypertension of unknown aetiology. Histopathology. 1996;28:195–204.
Abramowsky C, Romero R, Heffron T. Pathology of noncirrhotic portal hypertension: clinicopathologic study in pediatric patients. Pediatr Dev Pathol. 2003;6:421–6.
Zuo C, Chumbalkar V, Ells PF, Bonville DJ, Lee H. Prevalence of histological features of idiopathic noncirrhotic portal hypertension in general population: a retrospective study of incidental liver biopsies. Hepatol Int. 2017;11:452–60.
Wanless IR, Bernier V, Seger M. Intrahepatic portal vein sclerosis in patients without a history of liver disease. Autops Study Am J Pathol. 1982;106:63–70.
Guido M, Alves VAF, Balabaud C, Bathal PS, Bioulac-Sage P, Colombari R, et al. Histology of portal vascular changes associated with idiopathic non-cirrhotic portal hypertension: nomenclature and definition. Histopathology. 2019;74:219–26.
Okudaira M, Ohbu M, Okuda K. Idiopathic portal hypertension and its pathology. Semin Liver Dis. 2002;22:59–72.
Guido M, Sarcognato S, Sacchi D, Colloredo G. Pathology of idiopathic non-cirrhotic portal hypertension. Virchows Arch. 2018;473:23–31.
Lee H, Rehman AU, Fiel MI. Idiopathic noncirrhotic portal hypertension: an appraisal. J Pathol Transl Med. 2016;50:17–25.
Schouten JN, Verheij J, Seijo S. Idiopathic non-cirrhotic portal hypertension: a review. Orphanet J Rare Dis. 2015;10:67.
Guido M, Sarcognato S, Sonzogni A, Luca MG, Senzolo M, Fagiuoli S, et al. Obliterative portal venopathy without portal hypertension: an underestimated condition. Liver Int. 2016;36:454–60.
Jharap B, van Asseldonk DP, de Boer NK, Bedossa P, Diebold J, Jonker AM, et al. Diagnosing nodular regenerative hyperplasia of the liver is thwarted by low interobserver agreement. PLoS ONE. 2015;10:e0120299.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70:213–20.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, J., Shi, C., Dupont, W.D. et al. Key histopathologic features in idiopathic noncirrhotic portal hypertension: an interobserver agreement study and proposal for diagnostic criteria. Mod Pathol 34, 592–602 (2021). https://doi.org/10.1038/s41379-020-00676-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00676-8
This article is cited by
-
Evaluation of the histologic and immunohistochemical (CD34, glutamine synthetase) findings in idiopathic non-cirrhotic portal hypertension (INCPH)
Hepatology International (2024)
-
Obliterative Portal Venopathy
Current Hepatology Reports (2023)