Abstract
Objectives
To assess the feasibility of drawing, processing, safety-testing, and banking term umbilical cord blood to meet the packed red blood cell transfusion (RBC Tx) needs of extremely-low-gestational-age neonates (ELGANs).
Design
(1) Retrospectively analyze all ELGANs RBC Tx over the past three years, (2) Estimate local cord blood availability, (3) Assess interest in this project, and implementation barriers, through stakeholder surveys.
Results
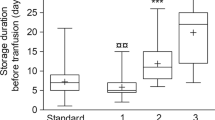
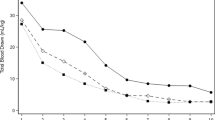
In three years we cared for 266 ELGANs; 165 (62%) received ≥1 RBC Tx. Annual RBC Tx averaged 197 (95% CI, 152–243). If 10% of our 10,353 annual term births had cord blood drawn and processed, and half of those tested were acceptable for Tx, collections would exceed the 95th % upper estimate for need by >four-fold. Interest exceeded 97%. Identified barriers included FDA approval, training to collect cord blood, and cost.
Conclusion
RBC Tx needs of ELGANS could be met by local cord blood collection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Deidentified data will be shared upon written request to the corresponding author.
References
Joseph RM, O’Shea TM, Allred EN, Heeren T, Hirtz D, et al. Neurocognitive and academic outcomes at age 10 years of extremely preterm newborns. Pediatrics. 2016;137:e20154343.
Bell EF, Hintz SR, Hansen NI, Bann CM, Wycoff MH, DeMauro SB, et al. Mortality, in-hospital morbidity, care practices, and 2-year outcomes for extremely Preterm infants in the US, 2013-2018. JAMA. 2022;327:248–63.
Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and neurodevelopmental outcomes among periviable infants. N. Engl J Med. 2017;376:617–28.
Del Vecchio A, Henry E, D’Amato G, Cannuscio A, Corriero L, Motta M, et al. Instituting a program to reduce the erythrocyte transfusion rate was accompanied by reductions in the incidence of bronchopulmonary dysplasia, retinopathy of prematurity and necrotizing enterocolitis. J Matern Fetal Neonatal Med. 2013;26:77–9.
Christensen RD, Baer VL, Lambert DK, Ilstrup SJ, Eggert LD, Henry E. Association, among very-low-birthweight neonates, between red blood cell transfusions in the week after birth and severe intraventricular hemorrhage. Transfusion. 2014;54:104–8.
Keir AK, New H, Robitaille N, Crighton GL, Wood EM, Stanworth SJ. Approaches to understanding and interpreting the risks of red blood cell transfusion in neonates. Transfus Med. 2019;29:231–8.
Song J, Dong H, Xu F, Wang Y, Li W, Jue Z, et al. The association of severe anemia, red blood cell transfusion and necrotizing enterocolitis in neonates. PLoS One. 2021;16:e0254810.
Khashu M, Dame C, Lavoie PM, De Plaen IG, Garg PM, Sampath V, et al. Current understanding of transfusion-associated necrotizing enterocolitis: review of clinical and experimental studies and a call for more definitive evidence. Newborn (Clarksville). 2022;1:201–8.
Odom TL, Eubanks J, Redpath N, Davenport E, Tumin D, Akpan US. Development of necrotizing enterocolitis after blood transfusion in very premature neonates. World J Pediatr. 2023;19:68–75.
Fontana C, Raffaeli G, Pesenti N, Boggini T, Cortesi V, Manzoni F, et al. Red blood cell transfusions in preterm newborns and neurodevelopmentaloutcomes at 2 and 5 years of age. Blood Transfus. 2022;20:40–49.
Vu PT, Ohls RK, Mayock DE, German KR, Comstock BA, Heagerty PJ, et al. Transfusions and neurodevelopmental outcomes in extremely low gestation neonates enrolled in the PENUT Trial: a randomized clinical trial. Pediatr Res. 2021;90:109–16.
D’Amato G, Faienza MF, Palladino V, Bianchi FP, Natale MP, Christensen RD, et al. Red blood cell transfusions and potentially related morbidities in neonates under 32 weeks’ gestation. Blood Transfus. 2021;19:113–9.
Bahr TM, Snow GL, Christensen TR, Davenport P, Henry E, Sarah M et al. Can transfusions have a pathogenic role in bronchopulmonary dysplasia? J Pediatr. 2023 (in press).
Stark CM, Juul SE. New frontiers in neonatal red blood cell transfusion research. J Perinatol. 2023;43:1349–56.
Puia-Dumitrescu M, Tanaka DT, Spears TG, Daniel CJ, Kumar KR, Athavale K, et al. Patterns of phlebotomy blood loss and transfusions in extremely low birth weight infants. J Perinatol. 2019;39:1670–5.
Ratanasopa K, Strader MB, Alayash AI, Bulow L. Dissection of the radical reactions linked to fetal hemoglobin reveals enhanced pseudoperoxidase activity. Front Physiol. 2015;6:39.
Perez M, Robbins ME, Revhaug C, Saugstad OD. Oxygen radical disease in the newborn, revisited: oxidative stress and disease in the newborn period. Free Radic Biol Med. 2019;142:61–72.
Arbell D, Bin-Nun A, Zugayar D, Eventov-Friedman S, Chepel N, Srebnik N, et al. Deformability of cord blood vs. newborns’ red blood cells: implication for blood transfusion. J Matern Fetal Neonatal Med. 2022;35:3270–5.
Wendelbo O, Hervig T, Haugen O, Seghatchian J, Reikvam H. Microcirculation, and red cell transfusion in patients with sepsis. Transfus Apher Sci. 2017;56:900–5.
Dani C, Poggi C, Gozzini E, Leonardi V, Sereni A, Abbate R, et al. Red blood cell transfusions can induce proinflammatory cytokines in preterm infants. Transfusion. 2017;57:1304–10.
Davenport P, Sola-Visner M. Immunologic effects of red blood cell and platelet transfusions in neonates. Curr Opin Hematol. 2022;29:297–305.
Eichler H, Schaible T, Richter E, Zieger W, Voller K, Leveringhaus A, et al. Cord blood as a source of autologous RBCs for transfusion to preterm infants. Transfusion. 2000;40:1111–7.
Brune T, Garritsen H, Witteler R, Schlake A, Wullenweber J, Louwen F, et al. Autologous placental blood transfusion for the therapy of anaemic neonates. Biol Neonate. 2002;81:236–43.
Garritsen HS, Brune T, Louwen F, Wullenweber J, Ahlke C, Cassens U, et al. Autologous red cells derived from cord blood: collection, preparation, storage, and quality controls with optimal additive storage medium (SAG-mannitol). Transfus Med. 2003;13:303–10.
Jansen M, Brand A, von Lindern JS, Scherjon S, Walther FJ. Potential use of autologous umbilical cord blood red blood cells for early transfusion needs of premature infants. Transfusion. 2006;46:1049–56.
Khodabux CM, von Lindern JS, van Hilten JA, Scherjon S, Walther FJ, Brand A. A clinical study on the feasibility of autologous cord blood transfusion for anemia of prematurity. Transfusion. 2008;48:1634–43.
Strauss RG, Widness JA. Is there a role for autologous/placental RBC transfusions in the anemia of prematurity? Transfus Med Rev. 2010;24:125–9.
Bianchi M, Teofili L, Giannantonio C, Landini A, Papacci P, Fioretti M, et al. Transfuse neonates with cord blood-derived red blood cells: a feasibility study to assess allogeneic cord blood unit fractionation and validation. Blood. 2012;122:275.
Bianchi M, Landini A, Giannatonio C, Papacci P, d’Onofrio G, Zini G. Allogeneic cord blood red cells for transfusion. Transfus Med Rev. 2012;26:90–1.
Bianchi M, Giannantonio C, Spartano S, Fioretti M, Landini A, Molisso A, et al. Allogenic umbilical cord blood red cell concentrates: an innovative blood product for transfusion therapy of preterm infants. Neonatology. 2015;107:81–6.
Teofili L, Papacci P, Orlando N, Bianchi M, Molisso A, Puracara V, et al. Allogeneic cord blood transfusions prevent fetal haemoglobin depletion in preterm neonates. Results of the CB-TrIP study. Br J Haematol. 2020;191:263–8.
Gavulic AE, Dougherty D, Li SH, Carver AR, Bermick JR, et al. Fetal hemoglobin levels in premature newborns. Should we reconsider transfusion of adult donor blood? J Pediatr Surg. 2021;56:1944–8.
Bianchi M, Orlando N, Barbagallo O, Sparnacci S, Balentini CG, Carducci B, et al. Allogenic cord blood red blood cells: assessing cord blood unit fractionation and validation. Blood Transfu. 2021;19:435–44.
Teofili L, Papacci P, Bartolo M, Molisso A, Orlando N, Pane L, et al. Transfusion-free survival predicts severe retinopathy in preterm neonates. Front Pediatr. 2022;10:814194.
Teofili L, Papacci P, Orlando N, Bianchi M, Pasciuto T, Mozzetta I, et al. BORN study: a multicenter randomized trial investigating cord blood red blood cell transfusions to reduce the severity of retinopathy of prematurity in extremely low gestational age neonates. Trials. 2022;23:1010.
Teofili L, Papacci P, Giannantonio C, Bianchi M, Valentini DG, Vento G. Allogenic cord blood transfusion in preterm infants. Clin Perinatol 2023 https://doi.org/10.1016/j.clp.2023.07.005.
Risso MA, Deffune E, Luzo ACM. Using umbilical cord blood as a source of paediatric packed red blood cells: processing and quality control. Vox Sang. 2023;118:637–46.
Lopriore E. Updates in red blood cell and platelet transfusions in preterm neonates. Am J Perinatol. 2019;36:S37–40.
Holzapfel LF, Rysavy MA, Bell EF. Red blood cell transfusion thresholds for anemia of prematurity. Neoreviews. 2023;24:e370–e6.
Bahr TM, Carroll PD. Cord blood sampling for neonatal admission laboratory testing-An evidence-based blood conservation strategy. Semin Perinatol. 2023;47:151786 https://doi.org/10.1016/j.semperi.2023.151786.
Carroll PD, Livingston E, Baer VL, Karkula K, Christensen RD. Evaluating otherwise-discarded umbilical cord blood as a source for a neonate’s complete blood cell count at various time points. Neonatology. 2018;114:82–6.
Henry E, Christensen RD, Sheffield MJ, Eggert LD, Carroll PD, Minton SD, et al. Why do four NICUs using identical RBC transfusion guidelines have different gestational age-adjusted RBC transfusion rates? J Perinatol. 2015;35:132–6.
Widness JA, Madan A, Grindeanu LA, Zimmerman MB, Wong DK, Stevenson DK. Reduction in red blood cell transfusions among preterm infants: results of a randomized trial with an in-line blood gas and chemistry monitor. Pediatrics. 2005;115:1299–306.
Ausbeck EB, Allman PH, Szychowski JM, Subramaniam A, Katheria A. Neonatal outcomes at extreme prematurity by gestational age versus birth weight in a contemporary cohort. Am J Perinatol. 2021;38:880–8.
Koo J, Kilicdag H, Katheria A. Umbilical cord milking-benefits and risks. Front Pediatr. 2023;11:1146057 https://doi.org/10.1055/s-0040-1722606
Mu TS, Prescott AC, Haischer-Rollo GD, Aden JK, Shapiro JB. Umbilical cord blood use for admission blood tests of VLBW preterm neonates: a randomized control trial. Am J Perinatol. 2023;40:1119–25.
Ohls RK, Lowe J, Yeo RA, Patel S, Winter S, Campbell RA, et al. Longitudinal assessment of preterm infants treated with erythropoiesis stimulating agents. Curr Pediatr Rev. 2023;19:417–24.
Bahr TM, Carr NR, Christensen TR, Wilkes J, O’Brien EA, German KR, et al. Early iron supplementation and iron sufficiency at one month of age in NICU patients at-risk for iron deficiency. Blood Cells Mol Dis. 2021;90:102575. Sep
Valieva OA, Strandjord TP, Mayock DE, Juul SE. Effects of transfusions in extremely low birth weight infants: a retrospective study. J Pediatr. 2009;155:331–37.
dos Santos AMN, Guinsburg R, de Almeida MF, Procianoy RS, Leone CR, Marba ST, et al. Red blood cell transfusions are independently associated with intra-hospital mortality in very low birth weight preterm infants. J Pediatr. 2011;159:371–6.
Baer VL, Lambert DK, Henry E, Snow GL, Christensen RD. Red blood cell transfusion of preterm neonates with a Grade 1 intraventricular hemorrhage is associated with extension to a Grade 3 or 4 hemorrhage. Transfusion. 2011;51:1933–9.
dos Santos AM, Guinsburg R, de Almeida MF, Procianoy RS, Marba ST, Ferri WA, et al. Factors associated with red blood cell transfusions in very-low-birth-weight preterm infants in Brazilian neonatal units. BMC Pediatr. 2015;15:113.
Ghirardello S, Dusi E, Cortinovis I, Villa S, Fumagalli M, Agosti M, et al. Effects of red blood cell transfusions on the risk of developing complications or death: an observational study of a cohort of very-low birth weight infants. Am J Perinatol. 2017;34:88–95.
Wang YC, Chan OW, Chiang MC, Yang PH, Chu SM, Hsu JF, et al. Red blood cell transfusion and clinical outcomes in extremely low birth weight preterm infants. Pediatr Neonatol. 2017;58:216–22.
Crawford TM, Andersen CC, Hodyl NA, Robertson SA, Stark MJ. The contribution of red blood cell transfusion to neonatal morbidity and mortality. J Paediatr Child Health. 2019;55:387–92.
MohanKumar K, Namachivayam K, Song T, Jake Cha B, Slate A, Hendrickson JE, et al. A murine neonatal model of necrotizing enterocolitis caused by anemia and red blood cell transfusions. Nat Commun. 2019;10:3494.
Bard H, Prosmanne J. Postnatal fetal and adult hemoglobin synthesis is preterm infants whose birth weight was less than 1,000 grams. J Clin Investig. 1982;70:50–2.
De Halleux V, Truttmann A, Gagnon C, Bard H. The effect of blood transfusion on the hemoglobin oxygen dissociation curve of very early preterm infants during the first week of life. Semin Perinatol. 2002;26:411–5.
Steinberg, MH, Thein SL. Fetal hemoglobin in health and disease. UpToDate 2023, June 13. www.uptodate.com/contents/fetal-hemoglobin-hb-f-in-health-and-disease.
Perrone B, Marchionni P, Bartoli A, Gidiucci C, Pasqualini M, D’Ascenzo R, et al. Fetal haemoglobin levels in preterm infants at 36 weeks postmenstrual age: effect of bronchopulmonary dysplasia, sepsis, and transfusions. Arch Dis Child. 2012;97:A75 https://doi.org/10.1136/archdischild-2012-302724.0258
Hellstrom W, Martinsson T, Hellstrom A, Morsing E, Ley D. Fetal haemoglobin, and bronchopulmonary dysplasia in neonates: an observational study. Arch Dis Child Fetal Neonatal Ed. 2021;106:88–92.
Guideline: delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. World Health Organization - 2014 - apps.who.int Untitled, pp 1 and 2. www.who.int/publications/i/item/97789241508209.
Surbek DV, Visca E, Steinmann C, Tichelli A, Schatt S, Hahn S, et al. Umbilical cord blood collection before placental delivery during cesarean delivery increases cord blood volume and nucleated cell number available for transplantation. Am J Obstet Gynecol. 2000;183:218–21.
Births, NVSS. Data for 2022. Vital Statistics Rapid Release, Number 28 (June 2023) (cdc.gov)
Free RJ, Sapiano MRP, Chavez Ortiz JL, Stewart P, Berger J, Basavaraju SV. Continued stabilization of blood collections and transfusions in the United States: Findings from the 2021 National Blood Collection and Utilization Survey. Transfusion 2023;18. https://doi.org/10.1111/trf.17360
Phillips AW, Reddy S, Durning SJ. Improving response rates and evaluating nonresponse bias in surveys: AMEE Guide No. 102. Med Teach. 2016;38:217–28.
Acknowledgements
The authors thank Dr. Luciana Teofili, Transfusion Medicine, and Dr. Giovanni Vento, Neonatology, Fondazione Policlinico Universitario A. Gemelli-Universita Cattolica del Sacro Cuore, Rome, Italy, Dr. Genny Raffaeli, Neonatology, Granada Ospedale Maggiore Policlinico, Milan, Italy, and Dr. Patrick D. Carroll, St. George Regional Hospital, for helpful discussions and manuscript review. We also thank Lindsey C. Carlson and Ashley Krueger of Intermountain Health Women and Newborns Research for their assistance with the survey and Jeni Walker, University of Utah Neonatology, for the illustration.
Author information
Authors and Affiliations
Contributions
RDC and TMB conceived the project. TRC, RKO, JK, LCC, EH, MJS, EG Assisted with data acquisition and analysis. RDC authored the initial draft of the manuscript. All authors reviewed and revised the manuscript, providing important content, and all authors approved the last version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Institutional Review Board of Intermountain Health reviewed the protocol and determined the project was exempt from the need for individual informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christensen, R.D., Bahr, T.M., Christensen, T.R. et al. Banked term umbilical cord blood to meet the packed red blood cell transfusion needs of extremely-low-gestational-age neonates: a feasibility analysis. J Perinatol (2023). https://doi.org/10.1038/s41372-023-01833-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-023-01833-y