Abstract
Objective
We assessed the efficacy of the Eat, Sleep, Console (ESC) model for neonatal abstinence syndrome at a regional referral center by examining non-pharmacological treatments, parental presence, length of stay (LOS), and pharmacological therapy.
Study design
We retrospectively reviewed medical records from 2018 to 2020 to compare neonatal outcomes between the 12 months prior to 12 months post ESC implementation.
Result
A total of 71 neonates pre-ESC and 64 neonates post-ESC implementation were included. There were no statistical differences between pre-ESC vs. ESC periods for pharmacological therapy (34% vs. 27%, p = 0.36) or LOS (median: 5.0 vs. 5.5 days, p = 0.54). During the ESC period, 41% of examined 4-h periods had no parent/caregiver presence. Decreased parental presence associated with pharmacological treatment (p < 0.001).
Conclusion
At our hospital which serves a geographically dispersed patient population, ESC model implementation did not decrease pharmacological therapy rates or LOS. Parental/caregiver presence may be a factor in the ESC model producing maximal benefits.
Similar content being viewed by others
Introduction
Neonatal abstinence syndrome (NAS) is a compilation of signs and symptoms of withdrawal exhibited by infants following in utero exposure to maternal substance use. The original assessment tools for NAS were developed for neonates exposed to opioids [1]. Polysubstance use is common and linked to NAS however opioid exposure remains the most studied contributor to NAS [1, 2]. The incidence and health care burden of NAS has dramatically increased over the past few decades due to the opioid epidemic; the proportion of pregnant women using opioids quadrupled from 1999 to 2014 [3]. Data collected across 23 hospitals in the USA from the Pediatric Health Information system showed a NAS incidence rate of 20/1,000 births in 2016 [4], with NAS incidence rates highest in areas most affected by the opioid epidemic. The opioid crisis disproportionately impacts Appalachia with West Virginia having the highest US rates of age-adjusted drug overdose deaths [5] and NAS diagnoses, with the reported incidence rate of NAS in 2017 at 53.5/1,000 births vs. the national average of 7.3/1000 births [6]. The increasing number of neonates with NAS is therefore also leading to increased health care costs. One of the main cost drivers is the increased length of stay (LOS), often 19 days or more, required for pharmacological management of NAS [7].
The Finnegan Neonatal Abstinence Scoring System (FNASS), often modified, is a popular tool for assessment of both opioid and non-opioid withdrawal [8,9,10]. The FNASS was designed to systematically assesses signs and symptoms associating with NAS [2, 8, 11]. The scoring system was developed in full term neonates [8], with prematurity associating with decreased withdrawal signs and symptoms, adding complexity to FNASS focused NAS management [11,12,13,14,15]. An FNASS-based cutoff has been historically used to identify neonates requiring NAS pharmacologic treatment with FNASS scoring also used to monitor, titrate, and terminate pharmacologic treatment [16].
To improve the care of neonates with NAS, a novel approach for assessing and managing infants with NAS was developed in 2017 by Grossman and colleagues at Yale-New Haven Children’s Hospital [17]. They developed the Eat, Sleep, and Console (ESC) model which is primarily focused on maintaining infant function and comfort, as opposed to reducing specific opioid withdrawal symptoms. The model’s emphasis is to encourage the parent-infant bond and maximize non-pharmacological therapies such as rooming-in, low stimulation environment, skin-to-skin contact, and swaddling prior to starting pharmacotherapy. Subsequently, Grossman et al. found that infants with NAS managed using the ESC approach had shorter LOS [17] and were treated with morphine significantly less frequently than if using the traditional FNASS indicator [18].
Our institution serves central Appalachia, an area known to have high rates of opioid use and NAS. The aim of this study was to assess the efficacy of the ESC approach in a regional hospital serving a rural, geographically dispersed patient population by examining the use of non-pharmacological treatments, parental presence, length of stay (LOS), and pharmacological therapy in neonates suspected of NAS.
Methods
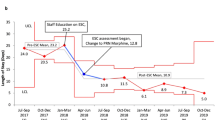
This retrospective review of neonates monitored for NAS symptoms in the newborn nursery was performed at Charleston Area Medical Center, Women and Children’s Hospital (Charleston, WV) between 9/4/2018 and 9/5/2020. Our hospital serves as a regional referral center in central Appalachia and provides care for more than 2000 newborn deliveries per year and has the only level IV NICU in the southern half of the state. The mother-baby department is comprised of a 52-crib nursery and 46 bed maternal post-care unit. In September 2019, the Mother-Baby unit transitioned from using a FNASS focused treatment protocol to the ESC model using a treatment algorithm based on that of Wachman and colleagues at Boston Medical Center, one of the earliest adopters of the ESC model [19].
Study inclusion criteria were (1) Full term neonates (gestational age from 37-42 weeks) born at our hospital between 9/4/2018 and 9/5/2020 and managed by the Mother-Baby Unit; (2) at least one documented Finnegan score greater than 0 during the birth admission or documented disruption to the infant’s ability to eat, sleep, or be consoled; and (3) documented intrauterine exposure to opioid substances including oxycodone, hydrocodone, morphine, buprenorphine, methadone, fentanyl, or heroin. Prenatal opioid exposure was identified by a positive maternal urine toxicology screen at any point during pregnancy or via neonatal cord toxicology. Our institution utilizes a universal urine drug screen for all women at time of admission for delivery. If maternal drug use is known or suspected, the neonate is further tested for intrauterine drug exposure by cord tissue toxicology, performed by United States Drug Testing Laboratories (Des Plaines, IL, USA) using a 15-drug panel.
Neonates were excluded from the study if they required transfer to the NICU, were premature (less than 37 weeks’ gestational age), had significant comorbidities (infections, asphyxia, congenital heart disease, pulmonary anomalies, transient tachypnea, spontaneous pneumothorax, lung pathology or maternal blood pressure abnormalities). Query of the hospital’s electronic medical records system for neonates having any recorded FNASS during the delivery admission generated the patient list for chart review. All aspects of the study including waiver of consent were approved by the Charleston Area Medical Center /West Virginia University-Charleston Institutional Review Board.
NAS management
At our institution, both pre and post-ESC implementation, neonates suspected of NAS were admitted to Mother-Baby Unit. Neonates were only transferred to the NICU if they had prematurity or additional comorbidities requiring intensive care. During the mothers’ admission, mothers had private rooms, and rooming-in with their infant was encouraged. Upon the mother’s discharge, the newborn was cared for in the well-infant nursery.
With ESC’s implementation, additional opportunities for infant-parental rooming-in after the mother’s discharge were made available. A room, within the Mother-Baby Unit was offered to the parent/caregiver during their visitation with the infant, unless the unit was at capacity. Rooms were not designated for NAS management and could be moved during the infant’s hospitalization. Additionally, as part of the ESC model, a NAS bundle of care was deployed and included encouraging breastfeeding (when eligible), skin-to-skin contact with parent, parental presence at the bedside, feeding on demand, swaddling, as well as decreased noise and light stimulation.
NAS assessments
Both pre and post-ESC implementation as part of standard care, FNASS scores were captured every 4 h in neonates evaluated for NAS for admission duration. In the pre-ESC period, methadone was started if a neonate scored on the FNASS three consecutive scores ≥8 or two consecutive scores ≥12 or at the physician’s discretion. After the implementation of ESC, FNASS were still obtained every 4 h but were not used for clinical decision-making, similar to other hospitals’ published procedures [20, 21]. In addition to the FNASS, neonates were assessed every 4 h by nursing staff to identify non-pharmacological therapies requiring reinforcement and performed ESC function-based assessments. Neonates were assessed every 4 h on their ability to perform three critical functions: (1) Eating: Can the newborn drink ½ to 1 oz of formula or breastfeed? (2) Sleeping: Can the newborn sleep undisturbed for an hour? and (3) Consolable: Can the newborn be consoled within 10 min? [17,18,19] If the infant was unable to eat, sleep, or be consoled due to withdrawal symptoms after all non-pharmacologic care was optimized, methadone was ordered following a meeting of the neonate’s care team. No other pharmacologic agents for NAS management in either the pre-ESC or ESC periods were used in the absence of methadone. Additionally, as part of the ESC care tool, parental/caregiver presence was recorded as the amount of time since last assessment that a parent (or other caregiver) spent in the room with infant.
Outcomes of interests
For this study, our primary outcome of interest was the rate of pharmacology therapy for NAS management. Our secondary outcomes included length of stay, rate of neonates with elevated FNASS values, length of pharmacotherapy, and need for 30-day readmission. Outcomes were compared between the 12 months preceding and 12 months following the implementation of ESC in the nursery (pre-ESC period: 9/4/2018–9/4/2019 and ESC period: 9/5/2019–9/5/2020). Additionally in the ESC cohort, we examined parental (or other caregiver) presence at the bedside to determine if it was inversely associated with pharmacotherapy usage.
Study variables
ESC assessments and FNASS scores were obtained from EMR records and included in analysis until pharmacological treatment for NAS was initiated, discharge, or 5 days post birth, whichever came first. Other variables collected included: sex, gestational age at birth, maternal race, parental presence, non-pharmacological therapies requiring reinforcement, maternal residential zip code, and distance to hospital (direct distance from center of the residential zip code to the study hospital in miles). Distance to hospital were dichotomized using the calculated median distance as the cut-point. In the ESC cohort, we also obtained data on the non-pharmacological therapies needing reinforcement which included parental/caregiver presence, rooming-in, skin-to-skin contact, holding by a caregiver, swaddling, optimal feeding at early hunger cues, non-nutritive sucking, quiet, low environment, limiting number of visitors, clustering care, safe-sleep/fall prevention, and parent/caregiver selfcare and rest.
Statistical analysis
We hypothesized we would experience a similar reduction of 40% in pharmacotherapy rates with ESC model adoption as reported by Wachman et al. [19]. As such, we needed a minimum of 24 infants per NAS management cohort to be able to reject the null hypothesis with a power of 0.95 and a Type I error probability of 0.05 using a two-sided chi-squared statistic (G*Power 3.1) [22]. Data was analyzed using SPSS 19 (IBM Corp., Armonk, NY, USA). Descriptive statistics, such as means and standard deviations for continuous variables and proportions and frequencies for categorical variables, were used to analyze infant characteristics. Variables of length of stays, length of pharmacological therapy, and distance to hospital were not normally distributed and were reported as medians with ranges (minimal to maximal value). Comparisons between groups for categorical variables were analyzed using Chi-square analysis, and when applicable, Fisher’s exact tests. Comparisons between groups for continuous variables were analyzed using two-sided t-test or Mann–Whitney U tests. Statistical significance was defined as p < 0.05.
Results
During the 12-month period prior to the implementation of ESC, records of 246 newborns having one or more recorded FNASS score were reviewed for study inclusion, of which 71 subjects met the inclusion criteria for the pre-ESC cohort. During the 12-month period following the implementation of ESC, 166 newborn records with a recorded FNASS score were reviewed, of which 64 subjects met the inclusion criteria and were included in the study. Figure 1 provides exclusion criteria frequencies, with majority of the neonates being excluded due to premature birth and/or need for neonatal intensive care.
Neonatal and maternal characteristics did not significantly differ between the pre-ESC and ESC cohorts (Table 1). The overall median distance from home residence to hospital was 29 miles (range: 0.8-141 miles). Mean FNASS values were not different between pre-ESC neonates (5.7 ± 1.7) versus the ESC cohort (5.8 ± 1.9), p = 0.83. FNASS-based and ESC-based NAS management strategies did not differ in the percentage of neonates receiving pharmacological therapy for the treatment of NAS (34% in pre-ESC vs 27% in ESC, p = 0.36) nor the median duration of pharmacotherapy (13 vs 12 days, p = 0.43). Among neonates receiving pharmacological therapy, LOS was similar between the two time periods (median: 17 (range: 8–32) days in pre-ESC versus 17 (10–30) days in ESC, p = 0.90). In neonates not receiving pharmacological therapy, the median LOS was 5 days in both cohorts, however the proportion of neonates having a LOS less than five days was greater in the pre-ESC cohort (19 of 71 had a LOS < 5 days) in comparison to the ESC group (8 of 64 with a LOS < 5 days), p = 0.04. No neonates from either cohort required NAS-related readmissions within 30 days. The rate of all cause 30-day readmission was low (≤ 7%) and did not differ between cohorts (p = 0.72). The toxicology profiles were similar between infants born during in the pre-ESC and ESC periods (Table 2). Buprenorphine was most the common exposure substance. Polysubstance was frequent (27% of cord specimens) as was cotinine exposure (54% of cord specimens).
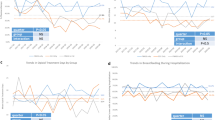
During ESC implementation, FNASS were obtained in conjunction with ESC measures as shown in Table 3. FNASS scores peaked and correlated with poor eating, poor sleeping, and inability to be consoled, at 48–96 h of life. Additionally, as part of the ESC care model, 12 non-pharmacological behaviors were evaluated every 4 h by the nursing staff and recorded when needing reinforcement. Figure 2 shows the percentage of assessments recorded as a specific non-pharmacological therapy requiring improvement or reinforcement. In the 64 neonates in the ESC period, non-pharmacological interventions were assessed a total of 948 times. The three most common non-pharmacological therapies requiring reinforcement were “increased parent/caregiver presence,” “rooming-in,” and “skin-to-skin”.
Parental/caregiver presence was documented at every ESC assessment, with the number of hours (0–4 h) with a parental/caregiver present recorded. A total of 41% of all evaluations were recorded as having no parent present for the entire 4-h period. Figure 3A demonstrates that parental/caregiver presence decreased during the initial 5 days of neonatal admission, with parental/caregiver presence dropping from 61% neonates having parental presence for three or more hours on Day 1 of life to 18% having the same level parental presence at Day 5. Parental presence was significantly decreased in the neonates that received pharmacotherapy in comparison to neonates receiving only non-pharmacotherapy (p < 0.001), with 58% of ESC assessments recorded no parental presence in neonates receiving NAS pharmacological therapy compared 39% of assessments having no parental presence in neonates not requiring pharmacotherapy (Fig. 3B). Parental presence was decreased in neonates whose recorded residence was more than median distance (29 miles) from the hospital (p = 0.02, Fig. 3C).
A Over the initial five days of newborn life, parent/caregiver presence steadily decreased (p < 0.001). B Parental presence was significantly less in newborns who received pharmacotherapy vs. the newborns than only received only non-pharmacological therapy (p < 0.001). C Distances from residence were stratified using the median distance (29 miles). Parental presence was significantly less in newborns with a residence greater than 29 miles in comparison to newborns with a recorded residence within 29 miles of the study hospital (p = 0.02).
Discussion
NAS care has become more centered on the infant-mother dyad with ESC model implementation. Although the FNASS has historically been used to quantify withdrawal symptoms severity and guide NAS treatment decisions, the ESC model shows high sensitivity in the detection of neonates requiring pharmacologic treatment [20]. Additionally, ESC scores correlate with FNASS scores shown both by us (Table 3) and others [21], thus suggesting that the ESC approach can be used as the primary method of guiding NAS treatment decisions, due its advantages of simplicity and patient-centered focus.
We examined the ESC model implementation for NAS management in a geographic region with high opioid use. We found with the ESC model fewer newborns received pharmacotherapy than predicted by historic FNASS-based cut-offs. Even though the decreased rate in methadone usage (34% pre-ESC to 27% during ESC) was not statistically significant, ESC model’s benefits remained including promoting non-pharmacologic therapies such as rooming-in, skin-to-skin contact, and providing a quiet environment [17,18,19, 23,24,25]. Our study findings deviated from those of Grossman et al. demonstrating the ESC approach reduced pharmacological treatment utilization and LOS [17]. Unlike many of the health care systems reporting their ESC implementation results [17,18,19, 23,24,25], at our institution infants with NAS are managed by the Mother-Baby unit which has limited private rooms for rooming-in post-maternal discharge. Dodds et al. noted that a major reason for the success of the ESC model at a community hospital was due to allowing caregivers to room-in with infants, since it created a quiet and nurturing environment, and allowed for a caregiver-focused model of care [24]. Furthermore, a systematic review reported that in newborns with NAS rooming-in compared to NICU significantly reduced pharmacotherapy use and LOS [26].
Given the ESC model’s strong focus on the infant-mother dyad and having a parent being the primary care provider to the infant during the hospital stay, the absence of the caregiver’s presence may prevent hospitals and patients from experiencing the full benefit of the ESC approach. A previous study of surveyed parents of newborns with NAS reported they valued the ESC model of care, as they felt they were a necessary and valued part of the care team in this holistic approach [27]. Further highlighting the importance of parental/caregiver involvement, we found that increased parental/caregiver presence associated with decreased need for pharmacotherapy. At our institution, we suspect that parental/caregiver participation was likely diminished by the limited availability of rooms for ESC as well as geographic distance from the parental/family residence as our institution is a tertiary care facility and has a large catchment area of approximately 12,000 square miles. Many patients drive two or more hours to have their child delivered at our hospital, and thus it may be difficult for them to return to the hospital after discharge to provide care for their admitted infant for extended lengths of time. Caring for other children in the household could also pose a significant barrier to parental/caregiver presence in the hospital. Additionally, a portion of the study was conducted during the COVID-19 pandemic when restricted visitation policies were enacted to reduce infection transmission, however, visitation of one or more parent/caregiver was allowed at all times. The limited visitation policies did not appear to affect parental presence as the percentage of assessments without any parental/caregiver presence were similar between pre-COVID (44% during September 2019-February 2020) and COVID periods (39% of assessments in March 2020–August 2020). Examination of specific barriers to parental presence was not conducted as part of the current study but is a topic of future research.
There are a number of limitations to our study. First, it was a retrospective medical record review, and we cannot account for missing data or limited documentation identified during chart review. Routine documentation in the medical record of caregiver presence and non-pharmacotherapies utilization only began in conjunction with ESC model implementation, thus we were unable to collect this information pre-ESC and to compare ESC to pre-ESC periods for those measures. Our strict inclusion criteria, including the exclusion of premature newborns and those needing intensive care which are common in those with NAS, may have reduced the study’s external validity and sample size. However, our sample size was larger than those reported in several previous studies [23,24,25]. Additionally, our hospital used a standardized protocol for methadone weaning if pharmacotherapy was initiated, with the weaning schedule not as rapid as prn morphine algorithms. Furthermore, during the study period FNASS measures were continued to be collected while using the ESC model of care. FNASS assessments could have possibly disrupted the infants, conflicting with ESC model’s goal to minimize interruptions, however clustering of care was utilized as part of the ESC model. While all clinicians and nursing staff were trained on the ESC model and agreed to not use FNASS for clinical decision-making, we cannot rule out they were influenced by FNASS scores. Lastly, this was a single site study and results may not be applicable to all hospitals, especially those in urban areas and/or abundant, designated ESC rooming-in facilities.
In our study, the absence of shorter LOS with ESC implementation may be due to our unique limitations as a tertiary care institution having limited rooming-in capacity while serving a mainly rural patient population. Ample rooming-in and parental presence may be some of the key drivers in the ESC model optimally reducing pharmacotherapy use and LOS. Further examination of the ESC model at similar institutions in the future may identify strategies to increase parental involvement and strengthen non-pharmacological interventions in NAS management as means to decrease LOS.
Data availability
Data not publicly available to maintain privacy in this vulnerable population.
References
McQueen K, Murphy-Oikonen J. Neonatal abstinence syndrome. N Engl J Med. 2016;375:2468–79.
Grossman M, Berkwitt A. Neonatal abstinence syndrome. Semin Perinatol. 2019;43:173–86.
Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization — United States, 1999–2014. MMWR Morbid Mortal Wkly Rep. 2018;67:845–9.
Milliren CE, Gupta M, Graham DA, Melvin P, Jorina M, Ozonoff A. Hospital variation in neonatal abstinence syndrome incidence, treatment modalities, resource use, and costs across pediatric hospitals in the United States, 2013 to 2016. Hosp Pediatr. 2018;8:15–20.
Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief. 2020;356:1–8.
Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA. 2021;325:146–55.
Patrick SW, Schumacher RE, Horbar JD, Buus-Frank ME, Edwards EM, Morrow KA, et al. Improving care for neonatal abstinence syndrome. Pediatrics. 2016;137:e20153835.
Finnegan LP, Connaughton JF Jr, Kron RE, Emich JP. Neonatal abstinence syndrome: assessment and management. Addict Dis. 1975;2:141–58.
Mehta A, Forbes KD, Kuppala VS. Neonatal abstinence syndrome management from prenatal counseling to a post discharge follow-up care: results of a national survey. Hosp Pediatr. 2013;3:317–23.
Byerley EM, Mohamed MW, Grindeland CJ, Muzzy Williamson JD. Neonatal abstinence syndrome practices in the United States. J Pediatr Pharm Ther. 2021;26:577–83. https://doi.org/10.5863/1551-6776-26.6.577
Jones HE, Harrow C, O’Grady KE, Crocetti M, Jansson LM, Kaltenbach K. Neonatal abstinence scores in opioid-exposed and nonexposed neonates: a blinded comparison. J Opioid Manag. 2010;6:409–13.
Lemon LS, Naimi A, Caritis SN, Platt RW, Venkataramanan R, Bodnar LM. The role of preterm birth in the association between opioid maintenance therapy and neonatal abstinence syndrome. Paediatr Perinat Epidemiol. 2018;32:213–22.
Gibson KS, Stark S, Kumar D, Bailit JL. The relationship between gestational age and the severity of neonatal abstinence syndrome. Addiction. 2017;112:711–6.
Ruwanpathirana R, Abdel-Latif ME, Burns L, Chen J, Craig F, Lui K, et al. Prematurity reduces the severity and need for treatment of neonatal abstinence syndrome. Acta Paediatr. 2015;104:e188–e194.
Allocco E, Melker M, Rojas-Miguez F, Bradley C, Hahn KA, Wachman EM. Comparison of neonatal abstinence syndrome manifestations in preterm versus term opioid-exposed infants. Adv Neonatal Care. 2016;16:329–36.
Sarkar S, Donn SM. Management of neonatal abstinence syndrome in neonatal intensive care units: a national survey. J Perinatol. 2006;26:15–17.
Grossman MR, Berkwitt AK, Osborn RR, Xu Y, Esserman DA, Shapiro ED, et al. An initiative to improve the quality of care of infants with neonatal abstinence syndrome. Pediatrics. 2017;139:e20163360.
Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr. 2018;8:1–6.
Wachman EM, Grossman M, Schiff DM, Philipp BL, Minear S, Hutton E, et al. Quality improvement initiative to improve inpatient outcomes for Neonatal abstinence syndrome. J Perinatol. 2018;38:1114–22.
Curran M, Holt C, Arciero M, Quinlan J, Cox D, Craig A. Proxy finnegan component scores for Eat, Sleep, Console in a cohort of opioid-exposed neonates. Hosp Pediatr. 2020;10:1053–8.
Ryan K, Moyer A, Glait M, Yan K, Dasgupta M, Saudek K, et al. Correlating scores but contrasting outcomes for eat sleep console versus modified finnegan. Hosp Pediatr. 2021;11:350–7.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91.
Blount T, Painter A, Freeman E, Grossman M, Sutton AG. Reduction in length of stay and morphine use for NAS with the “Eat, Sleep, Console” method. Hosp Pediatr. 2019;9:615–23.
Dodds D, Koch K, Buitrago-Mogollon T, Horstmann S. Successful implementation of the Eat Sleep Console model of care for infants with NAS in a community hospital. Hosp Pediatr. 2019;9:632–8.
Miller PA, Willier T. Baby STRENGTH: Eat, Sleep, Console for infants with neonatal abstinence syndrome. Adv Neonatal Care. 2021;21:99–106.
MacMillan KDL, Rendon CP, Verma K, Riblet N, Washer DB, Volpe Holmes A. Association of rooming-in with outcomes for neonatal abstinence syndrome: a systematic review and meta-analysis. JAMA Pediatr. 2018;172:345–51.
McRae K, Sebastian T, Grossman M, Loyal J. Parent perspectives on the Eat, Sleep, Console approach for the care of opioid-exposed infants. Hosp Pediatr. 2021;11:358–65.
Author information
Authors and Affiliations
Contributions
AA collected the data, drafted the initial manuscript, and reviewed and revised the manuscript for important intellectual content. MF collected data, reviewed, and revised the manuscript for important intellectual content. ST assisted in study design, performed data analyses, and reviewed and revised the manuscript for important intellectual content. AP conceptualized and designed the study, drafted the initial manuscript, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amin, A., Frazie, M., Thompson, S. et al. Assessing the Eat, Sleep, Console model for neonatal abstinence syndrome management at a regional referral center. J Perinatol 43, 916–922 (2023). https://doi.org/10.1038/s41372-023-01666-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01666-9